Abstract
Background
Total leukocyte and differential Leukocyte counts are prognostic indictors in patients with coronary artery disease (CAD). However, there is no data available regarding their prognostic utility in very old patients with acute myocardial infarction (AMI). The aim of this study is to investigate the potential role of different leukocyte parameters in predicting the mortality among very old patients with AMI.
Methods
A total of 523 patients aged over 80 years with AMI were consecutively enrolled into this study. Leukocyte and its subtypes were obtained at admission in each patient. The primary study endpoint was cardiovascular mortality. Patients were followed up for an average of 2.2 years and 153 patients died. The associations of leukocyte parameters with mortality were assessed using Cox regression analyses. The concordance index was calculated to test the model efficiency.
Results
In multivariable regression analysis, neutrophils-plus-monocytes-to-lymphocytes ratio (NMLR) and neutrophils-to-lymphocytes ratio (NLR) were two most significant predictors of mortality among all the leukocyte parameters (HR = 3.21, 95% CI 1.75–5.35; HR = 2.79, 95% CI 1.59–4.88, respectively, all p < 0.001, adjusted for age, male gender, body mass index, family history of CAD, smoking, hypertension, diabetes mellitus, high-density lipoprotein cholesterol (HDL-C), non-HDL-C, high sensitivity C-reactive protein, creatinine, left ventricular ejection fraction, troponin I, use of statin, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, and percutaneous coronary intervention). Furthermore, adding NMLR and NLR into the Cox model increased the C-statistic by 0.038 and 0.037 respectively, which were more significant than that of other leukocyte parameters. Besides, addition of NMLR and NLR to the Canada Acute Coronary Syndrome Risk Score model also increased the C-statistic by 0.079 and 0.077 respectively.
Conclusion
Our data firstly indicated that most leukocyte subtypes were independent markers for the mortality in very old patients with AMI, while NMLR and NLR appeared to be more effective.
Similar content being viewed by others
Background
Acute myocardial infarction (AMI) is a major cause of mortality worldwide, especially in geriatric patients [1]. Previous studies suggested that elderly patients with AMI had higher in-hospital, short- and long-term mortality rates compared with that of the young adults [2,3,4,5]. Moreover, the prevalence of AMI was much higher in very old patients [6]. Thus, finding new markers for precise cardiovascular risk stratification in very old patients may be crucial. In fact, several biomarkers including C-reactive protein and brain natriuretic peptide were proved to be predictive of adverse outcomes in AMI patients [7]. However, measurements of these markers are costly in current clinical practice. It may be of great value to find a simple and easy to access biomarker for predicting mortality in very old patients with AMI.
It was previously demonstrated that leukocyte count was a simple and low-cost marker which had a key role in the pathophysiology and prognosis of cardiovascular disease. Previous studies showed that leukocyte count was associated with a higher risk of coronary artery disease (CAD) [8,9,10]. Moreover, leukocyte count was also related to the severity of coronary artery stenosis, as well as the extent of infarct size in patients with AMI [11,12,13]. Furthermore, elevated leukocyte count was correlated with higher short- and long-term mortality in stable CAD patients with previous MI, unstable angina pectoris or acute coronary syndrome (ACS) [14,15,16,17,18].
As it is well known, the leukocytes subpopulations have different impacts in the development of atherosclerosis. Several studies had indicated that leukocytes and its subtypes were related to mortality in patients with ACS. However, the results were controversial [19, 20]. Previous studies about prognostic value of leukocytes were with several limitations as heterogeneous study population and limited subtypes of leukocyte. More importantly, to the best of our knowledge, data about leukocyte and its subtypes predicting mortality of AMI in very old patients with AMI is currently unavailable. Besides, no study investigated the relationship between neutrophil-plus-monocyte-to-lymphocyte ratio (NMLR) and clinical outcome in very old patients with AMI. In the current study, we aim to assess the association between leukocyte and its subpopulations with mortality and identify which leukocyte subtype is the best marker for predicting mortality in very old patients with AMI.
Methods
Study population
The study was complied with the Declaration of Helsinki and was approved by the hospital ethical review board (FuWai Hospital and National Center for Cardiovascular Diseases, Beijing, China). All patients provided written informed consent before enrolling in our study.
As described in Fig. 1, From January 2012 to December 2018, we consecutively enrolled 1313 hospitalized patients ≥ 80 years with CAD at our center. Patients were excluded from our study for the following criteria: stable CAD, unstable angina (UA), active infection, chronic inflammatory, immunologic disease, malignancy, severe liver disease, chronic obstructive pulmonary disease, hematologic disease, history of glucocorticoid therapy within the past 3 months. Finally, a total of 523 patients over 80 years with AMI were included in the present study. The medical history was recorded, and the electrocardiogram, clinical, laboratory examinations of each patient were carried out by experienced nurses and physicians.
The diagnosis of AMI was made by clinical presentation, electrocardiography and increment in cardiac troponins. Dyslipidemia was defined in subjects with fasting total cholesterol (TC) concentration ≥ 200 mg/dL, and triglyceride (TG) concentration ≥ 150 mg/dL. Diabetes mellitus (DM) was diagnosed as fasting plasma glucose (FPG) ≥ 7.0 mmol/L, the haemoglobin A1c (HbA1c) ≥ 6.5% or the current use of insulin or oral hypoglycemic drugs. Hypertension was diagnosed if a patient had blood pressure ≥ 140/90 mmHg three or more consecutive times or had been receiving anti-hypertensive medications.
Laboratory tests
Venous blood samples were drawn from patients at admission. We measured the level of white blood cells, neutrophils, monocytes and lymphocytes using an automated hematology analyzer Counter LH780 (Beckman Coulter Ireland Inc, Mervue, Galway, Ireland). Neutrophil-to-lymphocyte ratio (NLR), monocyte-to-lymphocyte ratio (MLR), eosinophil-to-leukocyte ratio (ELR) and NMLR were calculated. Lipid biomarkers including plasma TC, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), TG were assayed by automatic biochemistry analyser (Hitachi 7150, Tokyo, Japan). The level of non-HDL-C was calculated from the TC subtracted by HDL-C. The level of high sensitivity C-reactive protein (hsCRP) was determined using immunoturbidimetry (Beckmann Assay 360; Bera, CA, USA). Cardiac troponin I (cTnI) was measured by an immunochemiluminometric assay (Access AccuTnI, Beckman Coulter, CA). The rest of biochemical parameters were analyzed with standard laboratory techniques. The left ventricular ejection fraction (LVEF), which was evaluated by experienced specialists who performed the transthoracic echocardiography in a standard manner, was calculated using either Teichholz or Simpson’s biplane method at admission. The Canada Acute Coronary Syndrome Risk Score (C-ACS), included 4 variables and ranged from 0 to 4, was calculated as follows: 1 point was given for age ≥ 75 years, Killip > 1, systolic blood pressure < 100 mmHg, and heart rate > 100 beats/min, respectively [21].
Study endpoints
Follow-up data were acquired by interviewing each patient face to face or by telephone. The primary endpoint used for the analysis was cardiovascular mortality mainly including death caused by AMI, congestive heart failure, stroke, malignant arrhythmia and other structural or functional cardiac diseases as our previous studies [22]. Mortality data were obtained from interviewing and medical records.
Statistical analysis
Research data were analyzed using SPSS version 22.0 software (Chicago, IL, USA) and R language version 3.6.0 (Feather Spray). The Kolmogorov–Smirnov test was used to test the normality distribution. Data were shown as mean ± standard deviations (SD) or median with interquartile range for continuous variables and as numbers and percentages for categorical variables. Comparisons were made using Student’s t test, Mann–Whitney U test, Kruskal–Wallis test, chi-square test, or Fisher’s exact test when appropriate. Kaplan–Meier analysis was performed to illustrate mortality differences by tertiles of NMLR and NLR and Log-rank test was carried out to assess significance. Univariable and multivariable Cox regression analyses were used to calculate the hazard ratios (HRs). The adjusted Cox models included traditional cardiovascular risk factors as follows: age, male gender, body mass index (BMI), family history of CAD, smoking, hypertension, DM, HDL-C, non-HDL-C, hsCRP, creatinine, LVEF, troponin I, percutaneous coronary intervention (PCI), use of statin and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers (ACE-I/ARB). Besides, the predictive values of original model, C-ACS model, and either original model or C-ACS model plus leukocyte subtypes on mortality were also analyzed by receiver-operating characteristic curve (ROC). Moreover, the concordance index (C-Statistic) was calculated to assess the predictive efficiency. The incremental values of adding leukocyte and its subtypes to traditional risk model and C-ACS model were evaluated by △C-statistic. A p value of less than 0.05 was considered statistically significant.
Results
Baseline characteristics between deceased and survived group
The study cohort consisted of 523 patients with AMI. The mean age of study population was 82.75 ± 2.74 years (median = 82 years; ranged from 80 to 93 years). The median duration of follow up was 803 days (interquartile range 323–1158 days). 153/523 (29%) died over the course of the study.
The clinical characteristics and laboratory data of all patients were shown in Table 1. In brief, the deceased group had higher mean age, hsCRP, creatinine, prevalence of DM, but lower LVEF. In addition, the deceased group had significantly higher leukocytes, neutrophils, monocytes, NMLR, NLR, MLR levels but lower lymphocytes, eosinophils, basophils, ELR when compared with the survived group (all p < 0.05).
Predictive value of leukocyte and its subtypes for mortality
As shown in Fig. 2, Kaplan–Meier analyses suggested that subjects in the T2 and T3 of NMLR and NLR had lower survival rate than that in the T1 of NMLR and NLR. As was shown in Additional file 1: Table S1, patients with older age, DM, elevated hsCRP, creatinine and Troponin I or decreased LVEF and BMI were with higher risk of cardiovascular mortality. The relationship of leukocyte and its subtypes to the cardiovascular mortality of AMI was also evaluated using Cox proportional hazard regression analyses. In univariate models, both NMLR and NLR T3 were associated with higher risk of cardiovascular mortality [NMLR: Hazard Ratio (HR): 4.05, 95% CI 2.64–6.22; NLR: HR: 3.74, 95% CI 2.44–5.71, all p < 0.05, Table 2]. Adjustment of confounding variables did not change the association (HR = 3.21, 95% CI 1.75–5.35; and HR = 2.79, 95% CI 1.59–4.88, respectively, all p < 0.001).
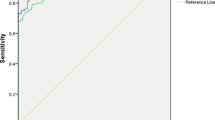
The ROC analyses of adding NMLR and NLR into C-ACS model and original model (included age, male gender, BMI, family history of CAD, smoking, hypertension, DM, HDL-C, non-HDL-C, hsCRP, creatinine, LVEF, troponin I, use of statin, ACE-I/ARB, and PCI) were shown in Figs. 3 and 4 and Table 3. The C-ACS model and original model were with the AUC of 0.636 (95% CI 0.583–0.688, p < 0.001) and 0.763 (95% CI 0.714–0.812, p < 0.001). Moreover, C-ACS model plus NMLR and NLR had the AUC of 0.705 (95% CI 0.654–0.756) and 0.703 (95% CI 0.651–0.754) respectively. Original model plus NMLR and NLR had the AUC of 0.803 (95% CI 0.759–0.847) and 0.802 (95% CI 0.757–0.846) respectively.
The original model was with the C-statistic of 0.728. Among all the leukocyte parameters, adding NMLR and NLR to the original model increased the C-statistic (0.766 and 0.765, △C-statistic 0.038 and 0.037 respectively, all p < 0.05, Table 4). As shown in Table 5, the C-statistic value of C-ACS model was 0.643. Addition of NMLR and NLR to the C-ACS model significantly improved the C-statistic to 0.722 and 0.720, respectively.
Discussion
The current prospective study investigated the predictive value of leukocyte parameters for cardiovascular mortality in very old patients with AMI. Cox regression analyses revealed that leukocyte subtypes including neutrophils, lymphocytes, eosinophils, basophils, NMLR, NLR, MLR and ELR were independently associated with cardiovascular mortality in very old patients. However, of all leukocyte parameters, NMLR and NLR were the better predictors of mortality. Moreover, adding NMLR and NLR to both original model and C-ACS model significantly improved the model efficiency. Thus, the present study provided novel information regarding the better performance of NMLR and NLR in predicting cardiovascular mortality in very old patients with AMI.
Previous studies suggested that older patients had not only more severe clinical manifestations but also worse outcomes than younger adult when they are suffered from AMI [23]. In a study of AMI patients, Marrugat, et al. [3] found that the MI mortality, incidence, and case-fatality dramatically increased among patients older than 64 years. Besides, the mortality rate of patients aged 75 to 84 years and 85 to 94 years was higher than that in the 34–64 years age group. They concluded that AMI had a greater impact in the elderly than that in those younger than 65 years old. Similar findings were reported in other studies [24]. Moreover, the problems of the elderly were attracting increasing attention not only in Western countries, but also in Asia. For elderly patients with MI, early risk assessment may help improve the clinical outcome. Thus, it is important to find a simple marker to identify the high-risk elderly population after MI.
Inflammation plays an important role in the occurrence and development of atherosclerotic cardiovascular diseases. Although previous studies have demonstrated that CRP, interleukin-6 and tumor necrosis factor-α were typical biomarkers of inflammation, measuring those markers was expensive and time consuming. Circulating leukocyte is a simple and inexpensive marker from the regular laboratory measurements. A large number of epidemiologic studies have indicated the positive relationship between leukocyte counts and risk of CAD [8,9,10]. In previous studies, leukocytes were also associated with the severity of CAD [11, 12]. Moreover, accumulating data indicated that leukocytes were predictive of mortality in patients with stable CAD, ACS and AMI [14,15,16,17,18].
However, few studies evaluated which leukocyte subpopulation was the most valuable one in predicting mortality in AMI patients. In 1037 patients with AMI, Dragu et al. [19] found that elevated neutrophil count was most significantly associated with mortality. In another study by Azab et al. [25], it was suggested that NLR was the best predictor of mortality in 1345 patients with non-ST-segment elevation MI. Yet a study by Shiyovich et al. [20] showed that lymphocytes had the strongest association with long-term risk of mortality in patients with AMI. However, these studies did not include all the leukocyte subtypes. Thus, it is still unclear which leukocyte parameter is the best for predicting mortality. In addition, data on the predictive utility of leukocyte and its subpopulations for mortality in very old patients with AMI is not currently available. Also, no study investigated the relation of NMLR and clinical outcome in very old patients with AMI. In our current study, in elderly patients with AMI, we found that most of leukocytes parameters including neutrophils, lymphocytes, eosinophils, basophils, NMLR, NLR, MLR and ELR were significantly and independently associated with mortality after adjustment for confounding variables, among which NMLR and NLR had better predictive performance than the other leukocytes parameters. Thus, the present study firstly reported that NMLR and NLR appeared to be more effective than other leukocytes parameters in predicting mortality in patients over 80 years with AMI.
The use of risk score models for indentifying high-risk patients in AMI is considered as a common method in current clinical guidelines [26, 27]. As one of the risk score models, the C-ACS was a simple model which was previously reported to predict both short- and long-term mortality of patients with ACS [21]. In accordance with previous study [21], our study showed that the C-ACS could independently predict mortality in elderly patients with AMI. As shown in our study, adding NMLR and NLR into the C-ACS model significantly improved the predictive efficiency in mortality. More importantly, adding NMLR and NLR to traditional risk model including age, male gender, BMI, family history of CAD, smoking, hypertension, DM, HDL-C, non-HDL-C, hsCRP, creatinine, LVEF, troponin I, use of statin, ACE-I/ARB, and PCI also significantly improved the model efficiency. Thus, it is necessary to take NMLR and NLR into consideration in the risk stratification for elderly patients with AMI.
As is the main findings of our study, both NMLR and NLR were independent markers and more powerful than other leukocyte parameters in predicting mortality in very old patients with AMI. However, the underlying mechanisms remained unclear. We speculate that the association between NMLR and NLR with mortality may due to their inflammatory and thrombotic activity. In fact, neutrophils could infiltrate vascular wall and result in plaque instability by secretion of superoxide radicals, cytokines, and a variety of proteolytic enzymes [28]. In addition, inflammatory monocytes, which are the earliest responders in AMI, contain many inflammatory cytokines including proteases. These inflammatory cytokines can cause necrosis of myocardium. Lymphocytes, on the other side, could induce the expression of interleukin-10 and promote tissue repairment [29]. Nevertheless, during AMI, subjects often present lower plasma lymphocytes count due to elevated cortisol levels, which may be associated with increased risk of death [30, 31]. Based on above mentioned mechanisms, neutrophils and monocytes play a key role in the inflammatory response while the lymphocytes are involved in the regulation of the immune system. Thereby, NMLR and NLR may reflect the balance between two opposite immune pathways and act as a more powerful predictor for mortality than single differential leukocyte count.
There are several limitations in the current study. First, the sample size of the current study is relatively small, and all patients were recruited from single center. Further studies in larger cohort may be in need to reveal our findings. Second, we only measured the baseline level of leukocytes and its subtypes. Multiple measurements over time may provide more valuable information for predicting mortality. Finally, even if the study only enrolled very old population at baseline, variation for age composition of the study population may affect our findings. Additional analysis of the relationship between white blood cells and outcome for different age subgroups in a larger cohort may also be in need.
Conclusion
Our data firstly indicated the multiple leukocyte subtypes were independent markers for the mortality in very old patients with AMI, while NMLR and NLR appeared to be more effective, suggesting the necessity to pay more attention to the levels of NMLR and NLR in such patients. In summary, increased NMLR and NLR may serve as simple indicators to identify high-risk patients and help determine appropriate treatment strategies.
Availability of data and materials
The technical appendix, statistical code and data set are available from the corresponding author.
Abbreviations
- CAD:
-
Coronary artery disease
- AMI:
-
Acute myocardial infarction
- NMLR:
-
Neutrophil-plus-monocyte-to-lymphocyte
- NLR:
-
Neutrophil-to-lymphocyte ratio
- MLR:
-
Monocyte-to-lymphocyte ratio
- ELR:
-
Eosinophil-to-leukocyte ratio
- ACS:
-
Acute coronary syndrome
- TC:
-
Total cholesterol
- DM:
-
Diabetes mellitus
- TG:
-
Triglyceride
- FPG:
-
Fasting plasma glucose
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- hsCRP:
-
High sensitivity C-reactive protein
- LVEF:
-
Left ventricular ejection fraction
References
Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord. 2017;17(1):53.
Shiraki T, Saito D. Clinical features of acute myocardial infarction in elderly patients. Acta Med Okayama. 2011;65(6):379–85.
Marrugat J, Sala J, Manresa JM, Gil M, Elosua R, Perez G, Albert X, Pena A, Masia R. Acute myocardial infarction population incidence and in-hospital management factors associated to 28-day case-fatality in the 65 year and older. Eur J Epidemiol. 2004;19(3):231–7.
Kanic V, Vollrath M, Tapajner A, Sinkovic A. Sex-related 30-day and long-term mortality in acute myocardial infarction patients treated with percutaneous coronary intervention. J Womens Health (Larchmt). 2017;26(4):374–9.
Haller PM, Jager B, Farhan S, Christ G, Schreiber W, Weidinger F, Stefenelli T, Delle-Karth G, Kaff A, Maurer G, et al. Impact of age on short- and long-term mortality of patients with ST-elevation myocardial infarction in the VIENNA STEMI network. Wien Klin Wochenschr. 2018;130(5–6):172–81.
Cui Y, Hao K, Takahashi J, Miyata S, Shindo T, Nishimiya K, Kikuchi Y, Tsuburaya R, Matsumoto Y, Ito K, et al. Age-specific trends in the incidence and in-hospital mortality of acute myocardial infarction over 30 years in Japan-report from the Miyagi AMI Registry Study. Circ J. 2017;81(4):520–8.
Sabatine MS, Morrow DA, de Lemos JA, Gibson CM, Murphy SA, Rifai N, McCabe C, Antman EM, Cannon CP, Braunwald E. Multimarker approach to risk stratification in non-ST elevation acute coronary syndromes: simultaneous assessment of troponin I, C-reactive protein, and B-type natriuretic peptide. Circulation. 2002;105(15):1760–3.
Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA. 1998;279(18):1477–82.
Rana JS, Boekholdt SM, Ridker PM, Jukema JW, Luben R, Bingham SA, Day NE, Wareham NJ, Kastelein JJ, Khaw KT. Differential leucocyte count and the risk of future coronary artery disease in healthy men and women: the EPIC-Norfolk Prospective Population Study. J Intern Med. 2007;262(6):678–89.
Margolis KL, Manson JE, Greenland P, Rodabough RJ, Bray PF, Safford M, Grimm RH Jr, Howard BV, Assaf AR, Prentice R. Leukocyte count as a predictor of cardiovascular events and mortality in postmenopausal women: the Women’s Health Initiative Observational Study. Arch Intern Med. 2005;165(5):500–8.
Amaro A, Gonzalez-Juanatey JR, Iglesias C, Martinez-Sande L, Trillo R, Garcia-Acuna J, Gil de la Pena M. Leukocyte count as a predictor of the severity ischaemic heart disease as evaluated by coronary angiography. Rev Port Cardiol. 1993;12(11):913–7.
Hong LF, Li XL, Luo SH, Guo YL, Liu J, Zhu CG, Qing P, Xu RX, Wu NQ, Jiang LX, et al. Relation of leukocytes and its subsets counts with the severity of stable coronary artery disease in patients with diabetic mellitus. PLoS ONE. 2014;9(3):e90663.
Chia S, Nagurney JT, Brown DF, Raffel OC, Bamberg F, Senatore F, Wackers FJ, Jang IK. Association of leukocyte and neutrophil counts with infarct size, left ventricular function and outcomes after percutaneous coronary intervention for ST-elevation myocardial infarction. Am J Cardiol. 2009;103(3):333–7.
Sabatine MS, Morrow DA, Cannon CP, Murphy SA, Demopoulos LA, DiBattiste PM, McCabe CH, Braunwald E, Gibson CM. Relationship between baseline white blood cell count and degree of coronary artery disease and mortality in patients with acute coronary syndromes: a TACTICS-TIMI 18 (Treat Angina with Aggrastat and determine Cost of Therapy with an Invasive or Conservative Strategy-Thrombolysis in Myocardial Infarction 18 trial) substudy. J Am Coll Cardiol. 2002;40(10):1761–8.
Cannon CP, McCabe CH, Wilcox RG, Bentley JH, Braunwald E. Association of white blood cell count with increased mortality in acute myocardial infarction and unstable angina pectoris, OPUS-TIMI 16 Investigators. Am J Cardiol. 2001;87(5):636–9.
Menon V, Lessard D, Yarzebski J, Furman MI, Gore JM, Goldberg RJ. Leukocytosis and adverse hospital outcomes after acute myocardial infarction. Am J Cardiol. 2003;92(4):368–72.
Mueller C, Neumann FJ, Perruchoud AP, Buettner HJ. White blood cell count and long term mortality after non-ST elevation acute coronary syndrome treated with very early revascularisation. Heart. 2003;89(4):389–92.
Hajj-Ali R, Zareba W, Ezzeddine R, Moss AJ. Relation of the leukocyte count to recurrent cardiac events in stable patients after acute myocardial infarction. Am J Cardiol. 2001;88(11):1221–4.
Dragu R, Khoury S, Zuckerman R, Suleiman M, Mutlak D, Agmon Y, Kapeliovich M, Beyar R, Markiewicz W, Hammerman H, et al. Predictive value of white blood cell subtypes for long-term outcome following myocardial infarction. Atherosclerosis. 2008;196(1):405–12.
Shiyovich A, Gilutz H, Plakht Y. White blood cell subtypes are associated with a greater long-term risk of death after acute myocardial infarction. Tex Heart Inst J. 2017;44(3):176–88.
Huynh T, Kouz S, Yan AT, Danchin N, O’Loughlin J, Schampaert E, Yan RT, Rinfret S, Tardif JC, Eisenberg MJ, et al. Canada Acute Coronary Syndrome Risk Score: a new risk score for early prognostication in acute coronary syndromes. Am Heart J. 2013;166(1):58–63.
Zhou BY, Guo YL, Wu NQ, Zhu CG, Gao Y, Qing P, Li XL, Wang Y, Dong Q, Liu G, et al. Plasma big endothelin-1 levels at admission and future cardiovascular outcomes: a cohort study in patients with stable coronary artery disease. Int J Cardiol. 2017;230:76–9.
Thiemann DR, Coresh J, Oetgen WJ, Powe NR. The association between hospital volume and survival after acute myocardial infarction in elderly patients. N Engl J Med. 1999;340(21):1640–8.
Vazquez-Oliva G, Zamora A, Ramos R, Marti R, Subirana I, Grau M, Degano IR, Marrugat J, Elosua R. Acute myocardial infarction population incidence and mortality rates, and 28-day case-fatality in older adults. REGICOR Study Rev Esp Cardiol (Engl Ed). 2018;71(9):718–25.
Azab B, Zaher M, Weiserbs KF, Torbey E, Lacossiere K, Gaddam S, Gobunsuy R, Jadonath S, Baldari D, McCord D, et al. Usefulness of neutrophil to lymphocyte ratio in predicting short- and long-term mortality after non-ST-elevation myocardial infarction. Am J Cardiol. 2010;106(4):470–6.
O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78–140.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Baldus S, Heeschen C, Meinertz T, Zeiher AM, Eiserich JP, Munzel T, Simoons ML, Hamm CW. Myeloperoxidase serum levels predict risk in patients with acute coronary syndromes. Circulation. 2003;108(12):1440–5.
Frangogiannis NG, Smith CW, Entman ML. The inflammatory response in myocardial infarction. Cardiovasc Res. 2002;53(1):31–47.
Bain RJ, Fox JP, Jagger J, Davies MK, Littler WA, Murray RG. Serum cortisol levels predict infarct size and patient mortality. Int J Cardiol. 1992;37(2):145–50.
Horne BD, Anderson JL, John JM, Weaver A, Bair TL, Jensen KR, Renlund DG, Muhlestein JB. Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol. 2005;45(10):1638–43.
Acknowledgements
The authors thank all the staff and participants of this study for their important contributions.
Funding
This work was partially supported by the Capital Health Development Fund (201614035) and CAMS Major Collaborative Innovation Project (2016-I2M-1-011).
Author information
Authors and Affiliations
Contributions
NQW and YLG conceived of the study design. XNY and JLJ wrote the manuscript. LFH and CGZ revised the manuscript. QD and MZ contributed to data collection and analysis of data. JJL contributed to the study design and data management. XNY and JLJ contributed to this work equally. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed according to the Declaration of Helsinki, and the hospital ethics review board (Fuwai Hospital and National Center for Cardiovascular Diseases, Beijing, China) approved the protocol. All patients provided written informed consent for the study.
Consent for publication
Not applicable.
Competing interests
No conflicts of interest in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Unadjusted cox proportional hazards regression analysis of cardiovascular mortality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yan, XN., Jin, JL., Zhang, M. et al. Differential leukocyte counts and cardiovascular mortality in very old patients with acute myocardial infarction: a Chinese cohort study. BMC Cardiovasc Disord 20, 465 (2020). https://doi.org/10.1186/s12872-020-01743-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-020-01743-3