Abstract
Background
While single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) is a well-established noninvasive procedure for the evaluation of patients with coronary artery disease (CAD), it is unable to detect the presence of, or underestimates the extent of CAD in certain patients. We aimed to show that a bio-impedance device can detect early post-stress changes in several hemodynamic parameters, thereby serving as a potential marker for the presence of significant ischemia.
Methods
Prospectively enrolled patients, referred to our Medical Center for clinically-indicated MPI, underwent testing using a Non-Invasive Cardiac System (NICaS) before and immediately after exercise. The differences between rest and stress hemodynamic parameters were compared with the severity and extent of myocardial ischemia by MPI. The study included 198 patients; mean age was 62 years, 26% were women, 54% had hypertension, and 29% diabetes mellitus. Of them, 188 patients had ≤10%, and 10 had > 10% of myocardial ischemia.
Results
In the first group, there was a significantly greater increase in post-exercise stroke index, stroke work index, cardiac index and cardiac power index (19.2, 29.1, 90.5 and 107%, respectively) compared with the second group (− 2.7, 3.8, 43.7 and 53.5%, respectively), as well as a significantly greater decrease in total peripheral resistance index (− 38.7% compared with − 16.3%), with corresponding p values of 0.015, 0.017, 0.040, 0.016, and < 0.001, respectively.
Conclusions
Our data suggest that immediate post-stress changes in several hemodynamic parameters, detected by the NICaS, can be used as an important adjunct to SPECT MPI for the early detection of myocardial ischemia.
Similar content being viewed by others
Background
Single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) is a well-established noninvasive procedure for the evaluation and risk stratification of patients with coronary artery disease (CAD) [1]. However, it has been recognized that in certain patients SPECT MPI is unable to detect the presence of, or underestimates the extent of CAD. The fact that moderate to severe perfusion defects are noted in less than half of the patients with significant left main disease [2] has stimulated studies to improve the diagnostic accuracy of SPECT MPI. Such studies have analyzed post-stress parameters such as left ventricular ejection fraction [3, 4], wall motion abnormalities [5] and transient left ventricular dilation [6] with images acquired on conventional Anger cameras as long as 60 min after the stress tracer injection. Such delayed assessment may miss early ischemic stunning as a result of its transient nature.
The Non-Invasive Cardiac System (NICaS, NI Medical, Israel) is a whole-body bio-impedance device capable of measuring various hemodynamic parameters [7,8,9,10,11]. We hypothesized that the non-invasive detection of an early post-stress decrease in cardiac performance may serve as a potential marker for the presence of significant or extensive ischemia. We therefore aimed to test for an early post-stress change in several hemodynamic parameters by the NICaS, and its relationship to the severity and extent of myocardial ischemia in patients undergoing exercise stress MPI using a novel cadmium-zinc-telluride SPECT camera.
Methods
Study population
We prospectively enrolled 198 patients who were referred to the Nuclear Cardiology Center at the Sheba Medical Center, Tel Hashomer, Israel, for a clinically-indicated exercise stress MPI study. Exclusion criteria included patients with: unstable angina, decompensated heart failure, systolic blood pressure > 200 mmHg or diastolic blood pressure > 110 mmHg, uncontrolled arrhythmias, severe aortic stenosis, acute pulmonary embolism, acute myocarditis or pericarditis, acute aortic dissection, intra- and extra-cardiac shunts, hemodialysis and those aged < 18 or > 80 years of age. The study was approved by the hospital’s Institutional Review Board and all patients provided written informed consent.
Exercise stress protocol and image acquisition sequence
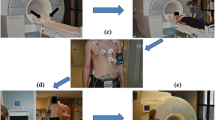
Beta blockers and calcium-channel antagonists were terminated at least 24 h before testing, and nitrates at least 6 h before testing. During the pre-imaging stress-lab evaluation and procedures, standard 12 leads for ECG monitoring and leads for image gating were applied, and a venous catheter was inserted into an antecubital vein. The imaging room was equipped with an ECG monitor, emergency cart and oxygen source.
A “stress-first-rest-second” protocol was used, as previously described [12,13,14,15,16,17,18,19,20,21]. Briefly, after obtaining baseline heart rate, blood pressure, and a 12 lead ECG, a symptom-limited treadmill-exercise (Bruce protocol) was performed. At peak exercise, an IV bolus of 6-11 mCi 99mTc-sestamibi, according to a body mass index-related dose schedule, was injected. The first imaging was started at least 20 min after the IV tracer injection. The patient was placed in the supine position of the cadmium-zinc-telluride-SPECT camera (Discovery NM 530c, General Electric Healthcare, Israel). The detector was positioned to include the entire heart image, as well as to isolate the heart from extra-cardiac activity. Acquisitions utilized a 20% energy window centered around the 140 KeV peak of 99mTc-sestamibi, and a16-bin ECG-gating was performed using a 50% acceptance window. Subsequently, the patient was placed in a prone position and imaging was repeated. After at least 1.5 h, the patient returned to the lab for rest injection and acquisition using 16-31 mCi of 99mTc-sestamibi, according to a body mass index-related dose schedule. Images were reoriented into short-axis and vertical and horizontal long-axis slices using standard software (QPS/QGS, Cedars-Sinai Medical Center, Los Angeles, CA, USA). All image contours were reviewed by experienced technologists and nuclear cardiologists on a case-by-case basis and were individually adjusted if necessary [12,13,14,15,16,17,18,19,20,21].
Automated quantification of perfusion
The QPS software computed the total perfusion deficit score by integrating the hypo-perfusion severities below normal limits in polar map coordinates [14]. Normal limit thresholds were defined as 3.0 mean absolute deviations (approximately equivalent to 2.5 standard deviations) for each polar map sample. Ischemic total perfusion deficit was calculated as an absolute difference between stress and rest total perfusion deficit [15, 16, 18], and was expressed as a percentage.
The non-invasive cardiac system
The NICaS calculates the stroke volume by measuring impedance cardiography in a tetra-polar mode, derived from electrodes placed on one wrist and the contra-lateral ankle [7, 8]. During transmission of an electrical current through the body, resistivity to its conduction (bio-impedance) is measured. The resistivity of blood and plasma is the lowest in the body, 150 and 63 Ω/cm, respectively, while resistivity of cardiac muscle, lungs and fat is 750, 1275 and 2500 Ω/cm, respectively. Thus, when an alternating current of 32.5 kHz, 1.4 mA is delivered through the two electrodes, it is primarily distributed via the extracellular fluid and the blood, and the changes in body resistivity are therefore related to the dynamic changes of the blood and plasma volume. Therefore, the measured bio-impedance and its fluctuations over time are proportional to the stroke volume. Consequently, each systolic increase in the aortic blood volume is associated with a proportional increase in the measurable conductance of the whole body. In addition, a standard three-lead ECG connection is made for measuring the pulse rate. Patient age, gender, weight, height, hematocrit and electrolytes are entered into the NICaS when the monitoring is started and are used for the stroke volume calculation. Cardiac output is calculated by multiplying stroke volume by the heart rate.
Measurements are adjusted to the body surface area to yield stroke index (SI) and cardiac index (CI). Mean arterial pressure (MAP), calculated from standard blood pressure measurements, together with SI and CI allows the calculation of stroke work index (SWI = MAP*SI/7500.8 J/m2), cardiac power index (CPI=MAP*CI/451 W/m2) and total peripheral index (TPRI = MAP/CI*80 Dyn*Sec/cm5*m2).
This simple to operate, non-invasive technique has been validated in several studies as a reliable estimation of resting CO, compared with traditional, invasive techniques in different settings including healthy subjects, patients with heart failure and ischemia [7,8,9,10,11]. Evaluation of impedance was performed both before and immediately after exercise. Given that the patient needs to be motionless during the measurement to avoid motion artifacts, data acquisition was carried out about 1 min after completion of exercise. The differences between rest and stress hemodynamic parameters were compared with the severity and extent of myocardial ischemia by MPI.
Statistics
Statistical analyses were performed using SPSS software (version 2b, IBM Corporation). All baseline variables are described as mean ± SD. Rest, stress and changes of hemodynamic parameters are described as mean and 95% confidence interval. A one-way ANOVA was used to compare differences for continuous variables. A chi-square test was used to compare differences across subgroups for categorical variables. A 2-tailed p < 0.05 as a cut-off was considered statistically significant. Receiver operator characteristic (ROC) curve was used to calculate sensitivity and specificity.
Results
Patient baseline clinical characteristics and medications are presented in Table 1. Mean age was 62 (±9) years and 74% were males. A sizeable percentage of patients had CAD, with a previous myocardial infarction in 22%, previous percutaneous transluminal coronary angioplasty in 18%, and previous coronary artery bypass grafting in 5%. Notably, the characteristics of those patients with myocardial ischemia ≤10% were similar to those with myocardial ischemia > 10%, with no significant differences in any of the baseline parameters. Patient baseline (resting) hemodynamic parameters are presented in Table 2. Once again, there were no statistically significant differences between patients with myocardial ischemia ≤10% and those with myocardial ischemia > 10%.
The hemodynamic changes between rest and stress in patients with myocardial ischemia ≤10% and in those with myocardial ischemia > 10% are presented in Table 3. In the first group, there was a significantly greater increase in post-exercise SI, SWI, CI and CPI (19.2, 29.1, 90.5 and 107%, respectively) compared with the second group (− 2.7, 3.8, 43.7 and 53.5%, respectively), as well as a significantly greater decrease in TPRI (− 38.7%) compared with the second group (− 16.3%), with corresponding p values of 0.015, 0.017, 0.040, 0.016, and < 0.001, respectively.
Fig. 1 provides a visual presentation of the change in cardiac function in patients with myocardial ischemia ≤10% and in those with myocardial ischemia > 10%. As may be clearly seen, the SI in the first group increased as expected with an associated marked increase in the CI; however, the SI in the second group actually decreased and thus only a mild increase was noted in the CI, mediated only by the increased heart rate.
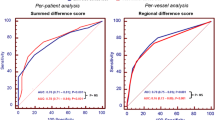
Fig. 2 demonstrates the ROC curve for myocardial ischemia > 10% vs. change in the SI (cut off = 0) from rest to stress. Noteworthy, are the areas under the curve with 95% confidence interval, sensitivity, and specificity. As may be seen, a change in SI of < 0 from rest to stress has 70.0% sensitivity and 73.1% specificity for detecting myocardial ischemia of > 10%.
Discussion
While SPECT MPI is an excellent noninvasive procedure for the detection and risk stratification of patients with CAD, it may be unable to detect the presence of disease in certain patients and may underestimate its severity in others. As a result, several studies have attempted to tackle this issue using various approaches [3,4,5,6]. In this prospective study we demonstrate that the non-invasive detection of an early post-stress decrease in cardiac performance may serve as a potential marker for the presence of significant or extensive ischemia.
As already shown in multiple prior studies, the NICaS whole-body bio-impedance device is capable of reliably measuring various hemodynamic parameters [7,8,9,10,11]. In this study we used the NICaS to examine the hemodynamic changes between rest and stress in patients with myocardial ischemia ≤10% and in those with myocardial ischemia > 10%. As seen in Table 3, the patients with ischemia were unable to increase their SWI, CI, and CPI to the same extent as those without significant ischemia, and were unable to decrease TPRI to the same extent as those without significant ischemia.
Most notably, the SI actually decreased in those patients with myocardial ischemia > 10% (Table 3, Fig. 1). While the SI in patients without significant ischemia increased as expected with an associated marked increase in their CI, it actually decreased in those with ischemia, and therefore only a mild increase was noted in the CI, mediated only by the increased heart rate (Fig. 1). Indeed, any decrease in SI may be used to detect myocardial ischemia > 10% with 70.0% sensitivity and 73.1% specificity (Fig. 2). The novel NICaS technology consistently identifies this pattern and therefore may be an important tool in the detection of ischemia.
The current study certainly has some limitations. Beta-blocker therapy was discontinued at least 24 h prior to testing and no information was available regarding the use of other medications. In addition, our findings are applicable only to the present study population, comprising patients with an intermediate pretest probability for the presence of CAD without significant comorbidities. Moreover, the small number of patients with myocardial ischemia > 10% limits certainly impacts the strength of the data. Of note, the reproducibility of the measured hemodynamic parameters may be somewhat limited by the patients’ physical fitness and performance on the particular test day. Finally, it may also have been useful to have had echocardiographic data to look for valvular comorbidity and to have had additional validation of the stroke volume at rest. We intend to address these limitations in future work as well as to obtain correlation with true anatomy by coronary angiography.
Conclusions
The results of the present study suggest that the immediate post-stress changes in several hemodynamic parameters as detected by the NICaS can be used as an important adjunct to the diagnostic approach for the early detection of myocardial ischemia. These findings can be used to improve risk assessment prior to a decision regarding the need to proceed with more complex and costly imaging modalities for the detection of myocardial ischemia. Moreover, future research should explore the potential use of the NICaS generated parameters as prognostic markers in the development and evolution of CAD.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- SPECT:
-
Single photon emission computed tomography
- MPI:
-
Myocardial perfusion imaging
- CAD:
-
Coronary artery disease
- NICaS:
-
Non-invasive cardiac system
- SI:
-
Stroke index
- CI:
-
Cardiac index
- MAP:
-
Mean arterial pressure
- CPI:
-
Cardiac power index
- TPRI:
-
Total peripheral resistance index
- SWI:
-
Stroke work index
- ROC:
-
Receiver operator characteristic
References
Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, et al. Single photon-emission computed tomography. J Nucl Cardiol. 2010;5:941–73.
Berman DS, Kang X, Slomka PJ, Gerlach J, de Yang L, Hayes SW, et al. Underestimation of extent of ischemia by gated SPECT myocardial perfusion imaging in patients with left main coronary artery disease. J Nucl Cardiol. 2007;4:521–8.
Lima RS, Watson DD, Goode AR, Lima RS, Watson DD, Goode AR, et al. Incremental value of combined perfusion and function over perfusion alone by gated SPECT myocardial perfusion imaging for detection of severe three-vessel coronary artery disease. J Am Coll Cardiol. 2003;1:64–70.
Sharir T, Germano G, Kavanagh PB, Lai S, Cohen I, Lewin HC, et al. Incremental prognostic value of post-stress left ventricular ejection fraction and volume by gated myocardial perfusion single photon emission computed tomography. Circulation. 1999;10:1035–42.
Sharir T, Bacher-Stier C, Dhar S, Lewin HC, Miranda R, Friedman JD, et al. Identification of severe and extensive coronary artery disease by postexercise regional wall motion abnormalities in Tc-99m sestamibi gated single-photon emission computed tomography. Am J Cardiol. 2000;11:1171–5.
Abidov A, Bax JJ, Hayes SW, Cohen I, Nishina H, Yoda S, et al. Integration of automatically measured transient ischemic dilation ratio into interpretation of adenosine stress myocardial perfusion SPECT for detection of severe and extensive CAD. J Nucl Med. 2004;12:1999–2007.
Cohen AJ, Arnaudov D, Zabeeda D, Schulthesis L, Lashinger J, Schachner A, et al. Non invasive measurement of cardiac output during coronary bypass grafting. Eur J Cardiothorac Surg. 1998;14:64–9.
Cotter G, Moshkovitz Y, Kaluski E, Cohen AJ, Miller H, Goor D, et al. Accurate, non-invasive, continuous monitoring of cardiac output by whole body electrical bio-impedance. Chest. 2004;125:1431–40.
Paredes OL, Shite J, Shinke T, Watanabe S, Otake H, Matsumoto D, et al. Impedance cardiography for cardiac output estimation - reliability of wrist-to-ankle electrode configuration. Circ J. 2006;70:1164–8.
Leitman M, Sucher E, Kaluski E, Wolf R, Peleg E, Moshkovitz Y, et al. Non-invasive measurement of cardiac output by whole-body bio-impedance during dobutamine stress echocardiography: clinical implications in patients with left ventricular dysfunction and ischaemia. Eur J Heart Fail. 2006;8:136–40.
Tanino Y, Shite J, Paredes OL, Shinke T, Ogasawara D, Sawada T, et al. Whole body bioimpedance monitoring for outpatient chronic heart failure follow up. Circ J. 2009;73:1074–9.
Imbert L, Poussier S, Franken PR, Songy B, Verger A, Morel O, et al. Compared performance of high-sensitivity cameras dedicated to myocardial perfusion SPECT: a comprehensive analysis of phantom and human images. J Nucl Med. 2012;12:1897–903.
Sharir T, Slomka PJ, Hayes SW, DiCarli MF, Ziffer JA, Martin WH, et al. Multicenter trial of high-speed versus conventional single-photon emission computed tomography imaging: quantitative results of myocardial perfusion and left ventricular function. J Am Coll Cardiol. 2010;18:1965–74.
Erlandsson K, Kacperski K, van Gramberg D, Hutton BF. Performance evaluation of D-SPECT: a novel SPECT system for nuclear cardiology. Phys Med Biol. 2009;9:2635–49.
Iskandrian AE, Bateman TM, Belardinelli L, Blackburn B, Cerqueira MD, Hendel RC, et al. ADVANCE MPI investigators. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: results of the ADVANCE phase 3 multicenter international trials. J Nucl Cardiol. 2007;5:645–58.
Sharir T, Ben-Haim S, Merzon K, Prochorov V, Dickman D, Ben-Haim S, et al. High-speed myocardial perfusion imaging. Initial clinical comparison with conventional dual detector anger camera imaging. J Am Coll Cardiol Img. 2008;1:156–63.
Patton J, Berman DS, Slomka P. Recent technological advances in nuclear cardiology. J Nucl Cardiol. 2007;14:433–54.
Slomka PJ, Nishina H, Berman DS, Akincioglu C, Abidov A, Friedman JD, et al. Automated quantification of myocardial perfusion SPECT using simplified normal limits. J Nucl Cardiol. 2005;1:66–77.
Xu Y, Kavanagh P, Fish M, Gerlach J, Ramesh A, Lemley M, et al. Automated quality control for segmentation of myocardial perfusion SPECT. J Nucl Med. 2009;9:1418–26.
Nishina H, Slomka PJ, Abidov A, Yoda S, Akincioglu C, Kang X, et al. Combined supine and prone quantitative myocardial perfusion SPECT: method development and clinical validation in patients with no known coronary artery disease. J Nucl Med. 2006;1:51–8.
Brodov Y, Fish M, Rubeaux M, Yuka O, Gransar H, Lemley M, et al. Quantitation of left ventricular ejection fraction reserve from early gated regadenoson stress Tc-99m high efficiency SPECT. J Nucl Cardiol. 2016;23:1251–61.
Acknowledgements
Poster presentation:
Goldkorn, R., Naimushin, A., Rozen, E., and D. Freimark. Early Post-Stress Decrease in Cardiac Performance by Impedance Cardiography and its Relation to the Severity and Extent of Ischemia by Myocardial Perfusion Imaging. European Society of Cardiology International Conference on Nuclear Cardiology and Cardiac CT, Lisbon, Portugal 2019. https://academic.oup.com/ehjcimaging/article/20/Supplement_3/jez149.003/5512782
Funding
This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
RG, made substantial contributions to the conception and design of the work, the acquisition, analysis, and interpretation of data, and drafted the work. AN, made substantial contributions to the conception and design of the work, the acquisition, analysis, and interpretation of data. ER, made substantial contributions to the the acquisition, analysis, and interpretation of data. DF, made substantial contributions to the conception and design of the work, the acquisition, analysis, and interpretation of data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Sheba Medical Center Institutional Review Board (reference number 2900–16-SMC) and all patients provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Goldkorn, R., Naimushin, A., Rozen, E. et al. Early post-stress decrease in cardiac performance by impedance cardiography and its relationship to the severity and extent of ischemia by myocardial perfusion imaging. BMC Cardiovasc Disord 20, 354 (2020). https://doi.org/10.1186/s12872-020-01639-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-020-01639-2