Abstract
Background
Trials of aspiration thrombectomy (AT) prior to primary percutaneous intervention (PCI) in patients with ST-segment elevation MI (STEMI) have shown apparently inconsistent results and therefore generated uncertainty and controversy. To summarize the effects of AT prior to PCI versus conventional PCI in STEMI patients.
Methods
Searches of MEDLINE, EMBASE and CENTRAL to June 2015 and review of reference lists of previous reviews. We included randomized controlled trials (RCTs) comparing AT prior to PCI with conventional PCI alone. Pairs of reviewers independently screened eligible articles; extracted data; and assessed risk of bias. We used the GRADE approach to rate overall certainty of the evidence.
Results
Among 73 potential articles identified, 20 trials including 21,660 patients were eligible; data were complete for 20,866 patients. Moderate-certainty evidence suggested a non statistically significant decrease in overall mortality (risk ratio (RR) 0.89, 95 % confidence interval, 0.78 to 1.01, risk difference (RD) 4/1,000 over 6 months), no impact on recurrent MI (RR 0.94, 95 % CI, 0.79 to 1.12) or major bleeding (RR 1.02, 95 % CI, 0.78 to 1.35), and an increase in stroke (RR 1.56, 95 % CI, 1.09 to 2.24, RD 3/1,000 over 6 months).
Conclusions
Moderate certainty evidence suggests aspiration thrombectomy is associated with a possible small decrease in mortality (4 less deaths/1000 over 6 months) and a small increase in stroke (3 more strokes/1000 over 6 months). Because absolute effects are very small and closely balanced, thrombectomy prior to primary PCI should not be used as a routine strategy.
Similar content being viewed by others
Background
In patients with ST-segment elevation myocardial infarction (STEMI), primary percutaneous coronary intervention (PCI) rapidly restores myocardial flow resulting in decreased infarct size and decreased mortality compared to thrombolysis or conservative medical management [1]. Some patients may, however, experience distal embolization of thrombus and plaque debris with failure to adequately restore distal microcirculatory flow. This “no reflow” phenomenon is associated with an increase in infarct size and lower survival [2].
Randomized clinical trials (RCTs) comparing aspiration or mechanical thrombectomy prior to primary PCI to PCI alone have shown improvement in markers of myocardial reperfusion (e.g. “myocardial blush”, ST-segment resolution post procedure) [3]. A recent meta-analysis of 20 RCTs addressing patient-important outcomes and including over 11,000 patients reported that aspiration thrombectomy prior to primary PCI was associated with a reduction in major coronary adverse events and 1-year mortality [4]. A more recent meta-analysis including 26 RCTs, reported a different conclusion: aspiration thrombectomy did not improve clinical outcomes [5]. Neither of these meta-analyses included the recently published Trial of Routine Aspiration Thrombectomy with PCI versus PCI Alone in Patients with STEMI (TOTAL), which randomized over 10,000 patients [6].
We therefore undertook a systematic review of all RCTs comparing aspiration thrombectomy prior to PCI versus PCI alone in patients with STEMI, focusing on patient-important outcomes. As composite endpoints varied between trials and can produce misleading results [7, 8], we focused on individual endpoints of overall mortality, recurrent MI, stroke, and major bleeding.
Methods
This review adheres to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Statement [9]; the Quality of Reporting of Meta-analyses QUOROM [10]; and the Cochrane Handbook for Systematic Reviews of Interventions [11].
Eligibility criteria
We included RCTs that compared aspiration thrombectomy prior to PCI with conventional PCI in patients with STEMI, included any one of the following patient-important outcomes: overall mortality, cardiovascular (CV) mortality, myocardial infarction (MI), stroke (including ischemic and hemorrhagic stroke) and, non-fatal extracranial major bleeding, and followed patients for at least 30 days. We excluded studies reported only as conference abstracts.
Data source and searches
A previous review with similar inclusion criteria identified studies up to December 2013 [5]. Using Medical Subject Headings (MeSH) based on the terms “thrombectomy,” “thrombus aspiration,” “thromboaspiration,” “infarction,” and “myocardial infarction” (Appendix Table 1) we replicated the search strategy of that review [5] for Medline, EMBASE, and Cochrane Controlled Trials Register (CENTRAL) from January 1, 2014 to June 26, 2015. We also reviewed reference lists of relevant review articles [4, 5, 12] and primary studies.
Selection of studies
Teams of two reviewers independently screened all titles and abstracts identified by the literature search, obtained full-text articles of all potentially eligible studies, and evaluated these studies for eligibility criteria.
Data extraction and risk of bias assessment
Three pairs of reviewers independently extracted the following data using a pre-standardized data extraction form: characteristics of the study design; participants; interventions; outcomes event rates and follow-up.
Reviewers independently assessed risk of bias by using a modified version of the Cochrane Collaboration’s tool for assessing risk for bias tool [13] (http:/distillercer.com/resources/) [14] that includes nine domains: adequacy of sequence generation, allocation sequence concealment, blinding of participants and caregivers, blinding of data collectors, blinding for outcome assessors, blinding of data analysts, incomplete outcome data, selective outcome reporting, and the presence of other potential sources of bias not accounted for in the previously cited domains [14]. For incomplete outcome data we stipulated as low risk of bias loss to follow-up of less than 10 % and a difference of less than 5 % in missing data in intervention and control groups.
Certainty of evidence
The reviewers used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology to rate certainty of the evidence for each outcome as high, moderate, low, or very low [15]. Detailed GRADE guidance was used to assess overall risk of bias [16], imprecision [17], inconsistency [18], indirectness [19] and publication bias [20], and summarized results in an evidence profile. We assessed publication bias through visual inspection of funnel plots for 10 or more studies.
For decisions regarding eligibility, risk of bias assessment, and data abstraction, reviewers resolved disagreement through discussion with third party adjudication if necessary.
Data synthesis and statistical analysis
We chose six months as a follow-up time that represented duration important to patients, sufficient to include most events that would likely be influenced by thrombectomy, and would include relatively few events that would not be potentially influenced by thrombectomy. For meta-analyses we used six months data if available; and otherwise we chose the time point closest to six months, but preferring 1-year over 30 days.
We calculated pooled risk ratios (RRs) and associated 95 % confidential intervals (CIs) using random-effects models with statistical method of Mantel-Haenszel. Absolute effects and 95 % CI were calculated by multiplying pooled RRs and 95 % CI by baseline risk estimates derived from the TOTAL study (the most recent and largest of the included RCTs) [6]. We addressed variability in results across studies by using I2 statistic and the P value obtained from the Cochran chi square test. Our primary analyses were based on eligible patients who had reported outcomes for each study (complete case analysis). For overall mortality we used all-cause mortality when available. For studies that did not present all-cause mortality we used cardiovascular mortality. We assessed publication bias through visual inspection of funnel plots for outcomes addressed in 10 or more studies. Review Manager (RevMan) provided the software for all analyses (version 5.3; Nordic Cochrane Centre, Cochrane) [21].
We also performed a meta-regression with a fixed-effect model using restricted estimated maximum likelihood with an observed log-odds ratio to predict whether mortality and recurrent myocardial infarction rates changed significantly by mean age. Meta-regression analysis was performed using Stata-13 (StataCorp LP, College Station, TX).
Results
Selection of titles
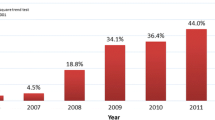
Our search strategy focusing on publications since the last review identified 103 unique citations (Fig. 1). After title and abstract screening, we assessed the full-text version of 38 relevant citations. In addition, we identified 42 potentially eligible publications included in previous systematic reviews, six [6, 22–26] of which were also identified in our search strategy. Thereafter, we assessed eligibility of 74 unique publications and excluded 49 studies (Fig. 1). As a result, we included 25 publications documenting 20 randomized controlled trials [6, 25–48] involving 21,660 participants. Two studies [28, 35] and one updated follow-up [46] were not included in any of the previous reviews.
Study characteristics
Ten studies [26, 27, 29, 31–34, 39–41, 43–46] were conducted largely in Europe (Table 1). Sample size ranged from 56 [35] to 10,732 [6] patients of whom a majority were males with mean ages typically in the early 60s. Studies included adult STEMI patients typically with symptoms lasting >30 min but <12 hours, and cumulative ST-segment elevation of >0.1 mV in ≥2 leads. Some studies excluded life expectancy < 6 months [6, 28, 29]; cardiogenic shock [28, 29, 32, 33, 35–38, 45–47]; previous CABG or MI or significant left main coronary lesion [6, 25, 29–33, 35–37, 39, 40, 42, 45–47]; pre-catheterization therapy with lytic agents [34]; severe asthma or bradycardia precluding use of adenosine [35]; dialysis; platelet count <100,000 or >700,000 cells/mm3; hemoglobin <10 g/dL [36, 37]; severe HF treated with intra-aortic balloon pump [39]; contraindication or prior use of platelet glycoprotein IIb/IIIa inhibitors [32–34, 40, 42]; rescue or facilitated PCI [42–44]; need for emergency CABG [26, 27]; pregnancy [45, 46]; and major planned surgery requiring discontinuation of antiplatelets agents [45, 46]. Follow-up time ranged from 30 to 360 days.
Twelve studies [25, 28–30, 34, 35, 38–44] used aspirin and clopidogrel as a preprocedure antithrombotic therapy; some of them [6, 25–30, 32–35, 38, 39, 41–47] also used intravenous heparin; seven of them had all patients were treated with abciximab [25, 31, 35, 39, 40, 41, 43, 44] and; one of them [42] also used nitroglycerin (Table 2).
The choice of medication during the procedure such as aspirin, heparin, clopidogrel, and glycoprotein IIb/IIIa inhibitors was at the investigator’s discretion in one of the included studies [34]. The patients in one further trial [26, 27] received the following procedure-related medication: bivalirudin, clopidogrel or ticlopidine, acetylsalicylic acid, ticagrelor, prasugrel, heparin, low-molecular-weight heparin, and glycoprotein IIb/IIIa blocker, while in other one [6] patients received unfractionated heparin; bivalirudin; enoxaparin and; glycoprotein IIb/IIa inhibitor (Table 2). Patients in TROFI trial [45, 46] received only heparin in ambulance and, in VAMPIRE trial [47] aspirin and intravenous heparin boluses were administered during the procedure to maintain an activated clotting time ≥ 300 s.
Risk of bias assessment
A possibly important limitation with respect to risk of bias was lack of blinding for caregivers. A number of studies, including the larger ones, blinded the adjudicators of outcome. Follow-up was largely satisfactory: 14 trials lost less than 10 % of patients to follow-up (Table 3 and Fig. 2).
Outcomes
Appendix Table 2 presents the mortality data by individual study and Appendix Table 3 presents individual study outcome data for recurrent MI, stroke, and bleeding.
Overall mortality
In 20 trials [6, 25–48] that addressed overall mortality, 457 of 10,433 (4.4 %) patients died in the control arm compared to 403 of 10,433 (3.9 %) in the aspiration PCI arm (relative risk (RR) 0.89, 95 % CI 0.78 to 1.01; I2 = 0 %; risk difference (RD) 4/1,000 over 6 months; moderate certainty) (Fig. 3). Certainty in evidence was rated down to moderate because of imprecision and unblinding of caregivers in all included studies (Table 4).
Recurrent myocardial infarction
In 17 trials [6, 25–29, 31–34, 36–41, 43–48], 246 of 10,331 (2.4 %) patients suffered a recurrent MI in the control arm compared to 229 of 10,331 (2.2 %) in the aspiration PCI arm (RR 0.94, 95 % CI 0.79 to 1.12; I2 = 0 %; RD 1/1,000 over 6 months; moderate certainty) (Fig. 4). Certainty in evidence was rated down to moderate because of imprecision, lack of blinding of caregivers in all included studies and inadequate or unreported blinding of outcome adjudicators in some studies [26, 27, 29, 31, 39, 41, 48] (Table 4).
Stroke
In 8 trials [6, 26, 27, 29, 36–39, 41, 45, 46], 77 of 9,185 (0.8 %) patients that underwent aspiration PCI use had a stroke compared to 48 of 9,162 (0.5 %) in the PCI alone (RR 1.56, 1.09 to 2.24; I2 = 0 %; RD 3/1,000 over 6 months; moderate certainty) (Fig. 5). Certainty in evidence was rated down to moderate because of imprecision, lack of blinding of caregivers in all included studies and inadequate or unreported blinding of outcome adjudicators in some studies [26, 27, 29, 39, 41] (Table 4). We intended to evaluate non-fatal stroke, but data was not available in sufficient number of studies to provide a useful comparison.
Major bleeding
In 4 trials [6, 36–38, 43, 44], 99 of 5823 (1.7 %) patients presented major bleeding in the control arm compared to 101 of 5,832 (1.7 %) in the aspiration PCI arm (RR 1.02, 0.78 to 1.35; I2 = 0 %; RD 0/1,000 over 6 months; moderate certainty) (Fig. 6). Certainty in evidence was rated down to moderate because of imprecision and lack of blinding of caregivers in all included studies (Table 4).
More than 10 studies addressed overall mortality and recurrent MI; for both, funnel plots did not suggest publication bias (Appendix: Figures 1 and 2).
Meta-Regression analysis
Data from studies assessed in a meta-regression showed that the relationship between mortality rates decreased with increasing mean age; however was not significant (slope: −0.011; 95 % confidence interval: −.0980 to .0765; P = 0.784; Fig. 7). Similarly, the relationship between recurrent myocardial infarction rates decreased with increasing mean age; however was not significant (slope: −0.011; 95 % confidence interval: −.1175 to .0944; P = 0.811; Fig. 8).
Meta-regression of recurrent myocardial infarction rates by mean age. Each circle represents a study highlighted by its weight in the analysis. The relationship between recurrent myocardial infarction and mean age in both groups was not significant (slope: -0.011; 95 % confidence interval: -.1175 to .0944; P = 0.811)
Discussion
Main findings
Based on pooled data from 20 randomized trials with more than 20,000 patients, we found moderate quality evidence for a non-statistically significant reduction in overall mortality (4 fewer deaths/1000 treated over 6 months) (Table 4) and a small potential increase in stroke (3 additional strokes/1000 treated over 6 months) (Table 4) in patients treated with thrombectomy. Moderate quality evidence suggests no impact of thrombectomy on either recurrent MI or major bleeding (Table 4).
A number of factors decreased our certainty in the estimates for overall mortality. In particular, the confidence interval included both no reduction in deaths and a mortality reduction that although small (8 fewer deaths in 1,000 over six months), many would consider important. Similarly with stroke: the confidence interval includes no increase in stroke and an increase of 6 more strokes in 1,000 patients over 6 months with thrombectomy, which many would consider an important risk. Other issues decreasing confidence in our estimates included potential risk of bias imposed by lack of blinding of patients and health care providers in all studies, and lack of blinding of outcome adjudicators in some studies.
The meta-regression analyses showed that both mortality and recurrent myocardial infarction rates decreased with increasing mean age. However, there was a non-significant difference between these two variables and the mean age of participants in both studied groups. A study [49] evaluated through a meta-regression whether there is an association between age, gender, diabetes mellitus, previous myocardial infarction and ejection fraction, and the choice of revascularization, focusing on death, myocardial infarction, repeat revascularization and stroke. The authors found that the reduction in stroke was significantly higher in females, and that women and patients with diabetes mellitus were at increased risk of subsequent revascularization after PCI [49].
Strengths and limitations
Strengths of our review include a comprehensive search; assessment of eligibility, risk of bias, and data abstraction independently and in duplicate; use of the GRADE approach in rating the quality of evidence for each outcome; and focus on absolute as well as relative effects of the intervention on patient-important outcomes. In this case, the small and more or less equivalent number of possible deaths prevented and strokes caused by thrombectomy, and the uncertainty consequent on the imprecision and risk of bias issues, are crucial in considering patient management (Table 4).
Potential limitations are related to the available data. Trials often suffered from incomplete outcome reporting, and lack of blinding consequent on the nature of the intervention, but for some studies also avoidable lack of blinding (outcome adjudication).
Relation to prior work
Recently published results from another meta-analysis [50] as well as data from a limited meta-analysis conducted as part of an evaluation of the outcome of stroke in the TOTAL study [12] are in general consistent with our findings. Results from all three analyses are in general consistent with our findings. Our systematic review and meta-analysis nevertheless adds important information as a result of our comprehensive assessment of risk of bias issues, our use of a complete case analysis that avoids assumptions regarding patients lost to follow-up, our use of the GRADE approach to rate quality of evidence, and our focus on absolute effects of thrombectomy required for optimal decision-making.
Furthermore, another review compared the effects of thrombectomy as an adjunct to PCI in the management of acute myocardial infarction in 20,853 patients [51]. The authors concluded that mortality; reinfarction and; stent thrombosis rates did not differ significantly between patients treated with or without AT; but stroke rates were increased with AT [51].
Implications
The possible magnitude of benefit with respect to mortality and magnitude of harm with respect to stroke are small – some might say very small – and similar both with respect to magnitude and likelihood that the effects are real. With respect to mortality, the most likely mechanism of benefit would be a reduction in recurrent MI; the data, however, provide no support for an impact of thrombectomy on MI.
Similarly the mechanism of an increase in stroke is not immediately apparent. In a recent analysis of data from the TOTAL study, thrombectomy was associated with a small increase in procedure time as well as increased use of larger catheters (99.2 % vs. 97.5 % > 5 French) [12]. One could postulate this could lead to an increase in embolization of aortic atherosclerotic plaque leading to increased early ischemic events. More frequent development of subsequent atrial fibrillation would constitute another possible mechanism; no study reported this outcome.
Initial enthusiasm for thrombectomy was motivated by evidence of improvement in markers of myocardial tissue reperfusion. Our findings emphasize the need for caution with respect to surrogates, and the desirability of focus on outcomes important to patients. While it is not routinely justified there may be individual cases in which an operator may feel the potential benefit of the procedure outweighs potential risks.
The absolute effects of thrombectomy prior to primary PCI are very small and still associated with uncertainty. Given the best estimates of effect and associated quality of evidence, fully informed risk adverse patients - and particularly those who are highly stroke risk averse - would likely decline thrombectomy. Patients who place high value on an uncertain mortality reduction and have limited concern regarding a possible stroke increase would be more likely to choose to undergo the procedure. Given current concerns regarding overtreatment and efficient use of health care resources, a policy decision to not use thrombectomy in a particular catheterization laboratory is defensible.
Conclusions
Moderate certainty evidence suggests aspiration thrombectomy is associated with a possible small decrease in mortality (4 less deaths/1000 over 6 months) and a small increase in stroke (3 more strokes/1000 over 6 months). Because absolute effects are very small and closely balanced, thrombectomy prior to primary PCI should not be used as a routine strategy.
Abbreviations
AT: aspiration thrombectomy; CV: cardiovascular; CENTRAL: cochrane controlled trials register; CIs: confidential intervals; GRADE: grading of recommendations assessment, development and evaluation; MeSH: medical subject headings; MI: myocardial infarction; PRISMA: preferred reporting items for systematic reviews and meta-analyses statement; PCI: primary percutaneous intervention; RCTs: randomized controlled trials; RevMan: review manager; RRs: risk ratios; STEMI: ST-segment elevation MI; TOTAL: Trial of Routine Aspiration Thrombectomy with PCI versus PCI Alone in Patients with STEMI
References
Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13–20.
Stone GW, Peterson MA, Lansky AJ, Dangas G, Mehran R, Leon MB. Impact of normalized myocardial perfusion after successful angioplasty in acute myocardial infarction. J Am Coll Cardiol. 2002;39(4):591–7.
Kumbhani DJ, Bavry AA, Desai MY, Bangalore S, Bhatt DL. Role of aspiration and mechanical thrombectomy in patients with acute myocardial infarction undergoing primary angioplasty: an updated meta-analysis of randomized trials. J Am Coll Cardiol. 2013;62(16):1409–18.
Kumbhani DJ, Bavry AA, Desai MY, Bangalore S, Byrne RA, Jneid H, et al. Aspiration thrombectomy in patients undergoing primary angioplasty: totality of data to 2013. Catheter Cardiovasc Interv. 2014;84(6):973–7.
Spitzer E, Heg D, Stefanini GG, Stortecky S, Rutjes AW, Räber L, Blöchlinger S, Pilgrim T, Jüni P, Windecker S. Aspiration Thrombectomy for Treatment of ST-segment Elevation Myocardial Infarction: a Meta-analysis of 26 Randomized Trials in 11 943 Patients. Rev Esp Cardiol (Engl Ed). 2015;68(9):746–52.
Jolly SS, Cairns JA, Yusuf S, Meeks B, Pogue J, Rokoss MJ, Kedev S, Thabane L, Stankovic G, Moreno R, Gershlick A, Chowdhary S, Lavi S, Niemelä K, Steg PG, Bernat I, Xu Y, Cantor WJ, Overgaard CB, Naber CK, Cheema AN, Welsh RC, Bertrand OF, Avezum A, Bhindi R, Pancholy S, Rao SV, Natarajan MK, ten Berg JM, Shestakovska O, Gao P, Widimsky P, Džavík V. Randomized trial of primary PCI with or without routine manual thrombectomy. N Engl J Med. 2015;372(15):1389–98.
Ferreira-Gonzalez I, Busse JW, Heels-Ansdell D, Montori VM, Akl EA, Bryant DM, Alonso-Coello P, Alonso J, Worster A, Upadhye S, Jaeschke R, Schünemann HJ, Permanyer-Miralda G, Pacheco-Huergo V, Domingo-Salvany A, Wu P, Mills EJ, Guyatt GH. Problems with use of composite end points in cardiovascular trials: systematic review of randomised controlled trials. BMJ. 2007;334(7597):786.
Lim E, Brown A, Helmy A, Mussa S, Altman DG. Composite outcomes in cardiovascular research: a survey of randomized trials. Ann Intern Med. 2008;149(9):612–7.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:b2535.
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354(9193):1896–900.
Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org
Jolly SS, Cairns JA, Yusuf S, Meeks B, Gao P, Hart RG, Kedev S, Stankovic G, Moreno R, Horak D, Kassam S, Rokoss MJ, Leung RC, El-Omar M, Romppanen HO, Alazzoni A, Alak A, Fung A, Alexopoulos D, Schwalm JD, Valettas N, Džavík V. Stroke in the TOTAL trial: a randomized trial of routine thrombectomy vs. percutaneous coronary intervention alone in ST elevation myocardial infarction. Eur Heart J. 2015;36(35):2364–72.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Guyatt GH, Busse JW. Modification of Cochrane Tool to assess risk of bias in randomized trials. http://distillercer.com/resources/.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y, Norris SL, Williams JW Jr, Atkins D, Meerpohl J, Schünemann HJ. GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). J Clin Epidemiol. 2011;64:407–15.
Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, Devereaux PJ, Montori VM, Freyschuss B, Vist G, Jaeschke R, Williams JW Jr, Murad MH, Sinclair D, Falck-Ytter Y, Meerpohl J, Whittington C, Thorlund K, Andrews J, Schünemann HJ. GRADE guidelines 6. Rating the quality of evidence—imprecision. J Clin Epidemiol. 2011;64:1283–93.
Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA, Norris S, Vist G, Dahm P, Shukla VK, Higgins J, Falck-Ytter Y, Schünemann HJ. GRADE guidelines: 7. Rating the quality of evidence—inconsistency. J Clin Epidemiol. 2011;64:1294–302.
Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA, Norris S, Vist G, Dahm P, Shukla VK, Higgins J, Falck-Ytter Y, Schünemann HJ. GRADE guidelines: 8. Rating the quality of evidence—indirectness. J Clin Epidemiol. 2011;64:1303–10.
Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, Alonso-Coello P, Djulbegovic B, Atkins D, Falck-Ytter Y, Williams JW Jr, Meerpohl J, Norris SL, Akl EA, Schünemann HJ. GRADE guidelines: 5. Rating the quality of evidence—publication bias. J Clin Epidemiol. 2011;64:1277–82.
The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). 5.3. Copenhagen: The NordicCochrane Centre, The Cochrane Collaboration; 2011.
Orlic D, Ostojic M, Beleslin B, Borovic M, Tesic M, Milasinovic D, et al. The randomized physiologic assessment of thrombus aspiration in patients with ST-segment elevation acute myocardial infarction trial (PATA STEMI) [abstract]. Eur Heart J. 2014;35:Abstract Supplement, 45.
Woo SI, Park SD, Kim DH, Kwan J, Shin SH, Park KS, Kim SH, Ko KY, Hwang TH, Yoon GS, Choi WG, Kim SH. Thrombus aspiration during primary percutaneous coronary intervention for preserving the index of microcirculatory resistance: A randomised study. EuroIntervention. 2014;9(9):1057–62.
Shehata M. Impact of successful manual thrombus aspiration during primary PCI in diabetic patients: Angiographic and clinical follow-up [abstract]. Catheter Cardiovasc Interv. 2014;83:S3.
Shehata M. Angiographic and clinical impact of successful manual thrombus aspiration in diabetic patients undergoing primary PCI. Int J Vasc Med 2014b; 263926 doi:10.1155/2014/263926.
Lagerqvist B, Fröbert O, Olivecrona GK, Gudnason T, Maeng M, Alström P, Andersson J, Calais F, Carlsson J, Collste O, Götberg M, Hårdhammar P, Ioanes D, Kallryd A, Linder R, Lundin A, Odenstedt J, Omerovic E, Puskar V, Tödt T, Zelleroth E, Östlund O, James SK.. Outcomes 1 year after thrombus aspiration for myocardial infarction. N Engl J Med. 2014;371(12):1111–20.
Frobert O, Lagerqvist B, Olivecrona GK, Omerovic E, Gudnason T, Maeng M, Aasa M, Angerås O, Calais F, Danielewicz M, Erlinge D, Hellsten L, Jensen U, Johansson AC, Kåregren A, Nilsson J, Robertson L, Sandhall L, Sjögren I, Ostlund O, Harnek J, James SK. Thrombus aspiration during st-segment elevation myocardial infarction. N Engl J Med. 2013;369:1587–97.
Turgeman Y, Bushari LI, Antonelli D, Feldman A, Yahalom M, Bloch L, Suleiman K. Catheter Aspiration after Every Stage during Primary Percutaneous Angioplasty, ADMIT Trial. Intl J Angiol. 2014;23(1):29–40.
Bulum J, Ernst A, Strozzi M. The impact of successful manual thrombus aspiration on in-stent restenosis after primary PCI: Angiographic and clinical follow-up. Coron Artery Dis. 2012;23:487–91.
Chao CL, Hung CS, Lin YH, Lin MS, Lin LC, Ho YL, Liu CP, Chiang CH, Kao HL. Time-dependent benefit of initial thrombosuction on myocardial reperfusion in primary percutaneous coronary intervention. Int J Clin Pract. 2008;62:555–61.
De Luca L, Sardella G, Davidson CJ, De Persio G, Beraldi M, Tommasone T, Mancone M, Nguyen BL, Agati L, Gheorghiade M, Fedele F. Impact of intracoronary aspiration thrombectomy during primary angioplasty on left ventricular remodeling in patients with anterior ST elevation myocardial infarction. Heart. 2006;92:951–7.
Sardella G, Mancone M, Bucciarelli-Ducci C, Agati L, Scardala R, Carbone I, et al. Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size: The EXPIRA (thrombectomy with export catheter in infarct-related artery during primary percutaneous coronary intervention) prospective, randomized trial. J Am Coll Cardiol. 2009;53:309–15.
Sardella G, Mancone M, Canali E, Di Roma A, Benedetti G, Stio R, Badagliacca R, Lucisano L, Agati L, Fedele F. Impact of thrombectomy with export catheter in infarct-related artery during primary percutaneous coronary intervention (EXPIRA trial) on cardiac death. Am J Cardiol. 2010;106:624–9.
Chevalier B, Gilard M, Lang I, Commeau P, Roosen J, Hanssen M, Lefevre T, Carrié D, Bartorelli A, Montalescot G, Parikh K. Systematic primary aspiration in acute myocardial percutaneous intervention: A multicentre randomised controlled trial of the Export aspiration catheter. EuroIntervention. 2008;4:222–8.
Hoole SP, Jaworski C, Brown AJ, McCormick LM, Agrawal B, Clarke SC, West NE. Serial assessment of the index of microcirculatory resistance during primary percutaneous coronary intervention comparing manual aspiration catheter thrombectomy with balloon angioplasty (IMPACT study): a randomised controlled pilot study. Open Heart. 2015;2(1):e000238.
Stone GW, Maehara A, Witzenbichler B, Godlewski J, Parise H, Dambrink JH, Ochala A, Carlton TW, Cristea E, Wolff SD, Brener SJ, Chowdhary S, El-Omar M, Neunteufl T, Metzger DC, Karwoski T, Dizon JM, Mehran R, Gibson CM. Intracoronary abciximab and aspiration thrombectomy in patients with large anterior myocardial infarction: The INFUSE-AMI randomized trial. JAMA. 2012;307:1817–26.
Stone GW, Witzenbichler B, Godlewski J, Dambrink JH, Ochala A, Chowdhary S, et al. Intralesional abciximab and thrombus aspiration in patients with large anterior myocardial infarction: One-year results from the INFUSE-AMI trial. Circ Cardiovasc Interv. 2013;6:527–34.
Liu CP, Lin MS, Chiu YW, Lee JK, Hsu CN, Hung CS, Kao HL. Additive benefit of glycoprotein IIb/IIIa inhibition and adjunctive thrombus aspiration during primary coronary intervention: results of the Initial Thrombosuction and Tirofiban Infusion (ITTI) trial. Int J Cardiol. 2012;156(2):174–9.
Kaltoft A, Bøttcher M, Nielsen SS, Hansen HH, Terkelsen C, Maeng M, Kristensen J, Thuesen L, Krusell LR, Kristensen SD, Andersen HR, Lassen JF, Rasmussen K, Rehling M, Nielsen TT, Bøtker HE. Routine thrombectomy in percutaneous coronary intervention for acute ST-segment-elevation myocardial infarction: A randomized, controlled trial. Circulation. 2006;114:40–7.
Liistro F, Grotti S, Angioli P, Falsini G, Ducci K, Baldassarre S, Sabini A, Brandini R, Capati E, Bolognese L. Impact of thrombus aspiration on myocardial tissue reperfusion and left ventricular functional recovery and remodeling after primary angioplasty. Circ Cardiovasc Interv. 2009;2:376–83.
Burzotta F, Trani C, Romagnoli E, Mazzari MA, Rebuzzi AG, De Vita M, Garramone B, Giannico F, Niccoli G, Biondi-Zoccai GG, Schiavoni G, Mongiardo R, Crea F. Manual thrombus-aspiration improves myocardial reperfusion: The randomized evaluation of the effect of mechanical reduction of distal embolization by thrombus-aspiration in primary and rescue angioplasty (REMEDIA) trial. J Am Coll Cardiol. 2005;46:371–6.
Sim DS, Ahn Y, Kim YH, Lee D, Seon HJ, Park KH, Yoon HJ, Yoon NS, Kim KH, Hong YJ, Park HW, Kim JH, Jeong MH, Cho JG, Park JC. Effect of manual thrombus aspiration during primary percutaneous coronary intervention on infarct size: Evaluation with cardiac computed tomography. Int J Cardio. 2013;168:4328–30.
Svilaas T, Vlaar PJ, van der Horst IC, Diercks GF, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008;358:557–67.
Vlaar PJ, Svilaas T, van der Horst IC, Diercks GF, Fokkema ML, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Cardiac death and reinfarction after 1 year in the thrombus aspiration during percutaneous coronary intervention in acute myocardial infarction study (tapas): A 1-year follow-up study. Lancet. 2008;371:1915–20.
Onuma Y, Thuesen L, van Geuns RJ, van der Ent M, Desch S, Fajadet J, Christiansen E, Smits P, Holm NR, Regar E, van Mieghem N, Borovicanin V, Paunovic D, Senshu K, van Es GA, Muramatsu T, Lee IS, Schuler G, Zijlstra F, Garcia-Garcia HM, Serruys PW. Randomized study to assess the effect of thrombus aspiration on flow area in patients with ST-elevation myocardial infarction: an optical frequency domain imaging study—TROFI trial. European Heart J. 2013;34:1050–60.
Garcia-Garcia HM, Muramatsu T, Nakatani S, Lee IS, Holm NR, Thuesen L, van Geuns RJ, van der Ent M, Borovicanin V, Paunovic D, Onuma Y, Serruys PW. Serial optical frequency domain imaging in STEMI patients: the follow-up report of TROFI study. European Heart J – Cardiovascular Imaging. 2014;15(9):987–95.
Ikari Y, Sakurada M, Kozuma K, Kawano S, Katsuki T, Kimura K, Suzuki T, Yamashita T, Takizawa A, Misumi K, Hashimoto H, Isshiki T. Upfront thrombus aspiration in primary coronary intervention for patients with ST-segment elevation acute myocardial infarction: Report of the VAMPIRE (vacuum aspiration thrombus removal) trial. JACC Cardiovasc Interv. 2008;1:424–31.
Yin D, Zhu H, Zhou X, Huang R, Wang J, Zheng Z. Thrombus aspiration before angiography during percutaneous coronary intervention in acute myocardial infarction. J Dalian Med Univ. 2011;33:235–9.
D'Ascenzo F, Barbero U, Moretti C, Palmerini T, Della Riva D, Mariani A, Omedè P, DiNicolantonio JJ, Biondi-Zoccai G, Gaita F. Percutaneous coronary intervention versus coronary artery bypass graft for stable angina: meta-regression of randomized trials. Contemp Clin Trials. 2014;38(1):51–8.
Elgendy IY, Huo T, Bhatt DL, Bavry AA. Is Aspiration Thrombectomy Beneficial in Patients Undergoing Primary Percutaneous Coronary Intervention? Meta-Analysis of Randomized Trials. Circ Cardiovasc Interv. 2015;8(7).
Barkagan M, Steinvil A, Berchenko Y, Finkelstein A, Keren G, Banai S, Halkin A. Impact of routine manual aspiration thrombectomy on outcomes of patients undergoing primary percutaneous coronary intervention for acute myocardial infarction: A meta-analysis. Int J Cardiol. 2016;204:189–95.
ᅟ
ᅟ
Funding
R El Dib received a Brazilian Research Council (CNPq) scholarship (CNPq 310953/2015-4).
Authors’ contributions
Conceiving the review: GHG, FAS, POV and RED. Undertaking searches: JK. Screening search results: RED, EAS, HG, JK, POV. Organizing retrieval of papers: RED and EAS. Screening retrieved papers against inclusion criteria: RED, EAS, HG, JK and POV. Appraising quality of papers: RED, EAS, HG, JK and POV. Extracting data from papers: RED, EAS, HG, JK and POV. Writing to authors of papers for additional information: RED. Providing additional data about papers: RED. Obtaining and screening data on unpublished studies: RED and EAS. Managing data for the review: RED. Entering data into Review Manager (RevMan): RED. Analyzing RevMan statistical data: RED, FAS, GHG, POV. Interpreting data: RED, FAS, GHG, POV. Making statistical inferences: RED, FAS, GHG, POV. Writing the review: RED, FAS, GHG, POV. Taking responsibility for reading and checking the review before submission: RED, FAS, EAS, HG, JK, GHG, POV. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
El Dib, R., Spencer, F.A., Suzumura, E.A. et al. Aspiration thrombectomy prior to percutaneous coronary intervention in ST-elevation myocardial infarction: a systematic review and meta-analysis. BMC Cardiovasc Disord 16, 121 (2016). https://doi.org/10.1186/s12872-016-0285-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-016-0285-4