Abstract
Background
Esketamine is commonly used as a premedication for its sedation effect. However, the proper dosage for intranasal use in children with congenital heart disease (CHD) has not been determined. This study aimed to estimate the median effective dose (ED50) of esketamine for intranasal premedication in children with CHD.
Methods
Thirty-four children with CHD who needed premedication in March 2021 were enrolled. Intranasal esketamine was initiated at a dose of 1 mg/kg. Based on the outcome of sedation in the previous patient, the dose for the subsequent patient was either increased or reduced by 0.1 mg/kg, which was adjusted between each child. Successful sedation was defined as a Ramsay Sedation Scale score ≥ 3 and Parental Separation Anxiety Scale score ≤ 2. The required ED50 of esketamine was calculated using the modified sequential method. Non-invasive blood pressure, heart rate, saturation of peripheral oxygen, sedation onset time, and adverse reactions were recorded at 5 min intervals after drug administration.
Results
The 34 children enrolled had a mean age of 22.5 ± 16.4 (4–54) months and a mean weight of 11.2 ± 3.6 (5.5–20.5) kg; American Society of Anesthesiologists classification I–III. The ED50 of intranasal S(+)-ketamine (esketamine) required for preoperative sedation in pediatric patients with CHD was 0.7 (95% confidence interval: 0.54–0.86) mg/kg, and the mean sedation onset time was 16.39 ± 7.24 min. No serious adverse events, such as respiratory distress, nausea, and vomiting were observed.
Conclusions
The ED50 of intranasal esketamine was 0.7 mg/kg, which was safe and effective for preoperative sedation in pediatric patients with CHD.
Trial registration
: The trial was registered in the Chinese Clinical Trial Registry Network (ChiCTR2100044551) on 24/03/2021.
Similar content being viewed by others
Background
Preoperative pediatric anxiety occurs in approximately 50–60% of children, especially those aged 1–5 years. This may have a negative psychological impact on children undergoing surgery [1, 2].
Preoperative sedation can alleviate perioperative anxiety of young children, thus creating a good condition for parental separation and anesthesia induction [3, 4]. Currently, various methods can be used to alleviate preoperative anxiety. In recent years large numbers of studies have focused on the effectiveness of non-pharmaceutical methods to achieve preoperative sedation in pediatric patients, although pharmaceutical sedation remains the general clinical practice.
Intranasal premedication is simple and minimally invasive compared with intramuscular or intravenous injections. Absorption is more complete, avoiding first-pass metabolism, and provides anesthesiologists with an alternative route for preoperative sedation. Midazolam, dexmedetomidine, and ketamine are sedatives for preoperative sedation in children, among which dexmedetomidine is more commonly used. However, dexmedetomidine will likely slow the heart rate [5,6,7,8]. The results of our previous study on preoperative medication in children with congenital heart disease (CHD) suggested that an intranasal drip of 2 mg/kg ketamine can be safely and effectively used for preoperative sedation in pediatric patients with CHD [9]. Esketamine is a new-type N-methyl-D-aspartate receptor inhibitor with the advantages of fast-acting and good sedative and analgesic effects; its sedative efficacy is 2-fold higher than that of ketamine, with minimal mental symptoms. In Europe, racemic ketamine has been replaced by its enantiomer S(+)-ketamine (esketamine), which has the advantage of anesthetic potency, minimal psychiatric adverse effects, little saliva secretion, fast action, and quick recovery [10,11,12].
Esketamine is also effective for pain relief because of ease of use and minimal effect on respiration. In addition, it has the feature of sympathetic activity, can increase systemic vascular resistance, and reduce intracardiac right-to-left shunting in children with cyanotic CHD, thus relieving hypoxia.
To the best of our knowledge, there is a lack of research on the median effective dose (ED50) of esketamine for intranasal premedication, especially in children with CHD, who are an exceptional cohort, and rational preoperative sedation can keep them in a quiet state and reduce vigorous hemodynamic fluctuations due to stress and anxiety.
Our pilot experiments suggested that a dose of 0.5–1.5 mg/kg could achieve an expected sedative effect in most children, and no evident inhibition of breathing and circulation was observed. Adverse reactions such as allergy, nausea, and vomiting have not been recorded. At present, the dosage of esketamine has not been clearly determined. To rationally apply esketamine to clinical practice, we designed this experiment to determine the ED50 of esketamine for intranasal premedication in children with CHD, and evaluated its safety, hoping that the results obtained in this study can provide useful references for the clinical application of the medication.
Methods
Participants
This prospective, randomized, single-blind study was approved by the ethics committee of by the Medical Ethics Committee of Shanghai Children’s Medical Center (SCMCIRB-K2020058-2) and registered in the Chinese Clinical Trial Registry Network (ChiCTR2100044551) on 24/03/2021. Inclusion of children with CHD was decided by the randomized number generated by computer simulation without sex limitation. Before signing the informed consent form, the guardians were informed of the possible risks associated with sedation and the precautions for care and monitoring.
Included in this prospective study were 34 children with CHD, aged from 4 to 54 months and weighing from 5.5 to 20.5 kg, who underwent elective surgery for CHD in March 2021. The exclusion criteria were: American Society of Anesthesiologists (ASA) classification ≥ IV; allergy to the drug to be tested; severe liver/kidney dysfunction; increased intracranial pressure; inability to separate from parents/guardians; history of intranasal surgery; front facial deformity; airway abnormality; and the presence of obstructive sleep apnea syndrome. According to the requirements for the research design of the sequential method, 6–8 crossover points were expected to be included [12], and the crossover point was defined as “the turning point for 2 adjacent cases from failure to achieve the expected effect” and “success in achieving the expected effect.“ Therefore, the inclusion of approximately 30 cases in the experiment would satisfy the statistical requirements.
Methods
Before surgery, the parents/guardians of the participants were advised to routinely fast their children for 6 h, avoid breastfeeding for 4 h and feed them with light food for 2 h. The patients and their guardians were escorted to the operating room 60 min before surgery. The patient’s preoperative status was assessed by the anesthesiologist in a single-blind manner, including ASA classification, heart rate monitoring, non-invasive blood pressure, saturation of peripheral oxygen (SpO2), and other baseline parameters. Esketamine (Jiangsu Hengrui Pharmaceuticals Co., Ltd., Lianyungang, China; batch no.: 200325BL) in a sterile hypodermic syringe (1 ml) was administered intranasally with the patient in the supine position in the guardian’s arms; the nasal mucosa absorbed it. Based on the pilot experiment results, the dose of esketamine was set as 1.0 mg/kg for the first patient, and the dose for the subsequent patient was determined by the extent of the expected effect achieved in the previous patient; if the expected effect was achieved, the dose gradient would be reduced, and if it failed to reach the expected effect, the dose gradient would be increased. Each nasal cavity was administered a half dose of esketamine, during which the child was in a supine position for 2 min and have the bilateral nasal wings pressed gently. Five min after drug administration, the patient’s heart rate and SpO2 were monitored. The depth of sedation was assessed by the Ramsay Sedation Scale score (Table 1), and at the same time, the nurse blinded to the study recorded the depth of sedation at the time of parental/guardian separation. In the present study, “success in reaching the expected effect” was defined using a ≥ 3 Ramsay Sedation Scale score 30 min after drug administration and a Parental Separation Anxiety Scale score (PSAS) (Table 2) ≤ 2 simultaneously. A dose gradient was defined as 0.1 mg/kg. The “effect onset time” was defined as the time from successful sedation to the time of reaching the Ramsay Sedation Scale score of ≥ 3. The sedation onset time and the occurrence of any adverse events such as nausea and vomiting, increased secretion, tachycardia or bradycardia, blood pressure abnormality, hypoxia, respiratory distress, and respiratory tract obstruction were recorded.
We confirmed that all methods were performed following the relevant guidelines and regulations.
Research Parameters
The primary endpoint of the present study was the ED50 of esketamine for intranasal premedication in children with CHD. The secondary endpoints were the sedation onset time after drug administration and changes in respiratory and circulating functions at the designated observational time points.
Statistical analysis
Statistical data were analyzed by SPSS 20.0 (IBM Corp., Armonk, NY, USA) and Excel Software (Microsoft Corporation, Redmond, WA, USA). The normality test of measurement data was performed using the Kolmogorov-Smirnov method, and data for normal distribution are expressed as the mean ± standard deviation. Under homogeneity of variance, a paired t-test was used for data analysis between groups. Measurement data for abnormal distribution or with uneven variance were tested using the Kruskal-Wallis method. P < 0.05 was considered statistically significant. Probit regression was used to calculate ED50 of esketamine and a 95% confidence interval (CI).
Results
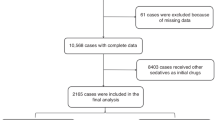
Thirty-four patients were included in the study,, ASAI–III,21 boys and 13 girls, with a mean age of 22.5 ± 16.4 (4–54) months and a mean weight of 11.2 ± 3.6 (5.5–20.5) kg. The mean weight for successful and failed sedation was 11.0 ± 4.0 kg and 11.5 ± 3.1 kg, respectively. The CHD of the patients included ventricular septal defect in 17, atrial septal defect in 9, pulmonary valve stenosis (PVS) in 2, Tetralogy of Fallot (TOF) in 2, and aortic stenosis in 1, patent ductus arteriosus in 1, and coronary right ventricular fistula in 1. The flow chart of the research process is indicated in Fig. 1.
Nineteen (55.9%) of the 34 patients who achieved successful sedation with intranasal esketamine were first included for analysis, in whom the effect onset time (min) was 20.5 ± 5.3 min, the quickest sedation onset time was 11.5 min, and the slowest was 28 min with a mean of 20.5 min. The other 15 patients who failed to achieve sedation were also included for analysis, including 9 cases of parental separation failure (4 children were unsuccessful in separating from their parents/guardians and sedation failure)and 6 cases of loss of sedation. After including the drug dose covariate and the dependent variable of response success, the optimal solution was obtained after 12 iterations. Using the probability regression method, the ED50 of esketamine was calculated as 0.7 (95% confidence interval [CI]: 0.54–0.86) mg/kg. Details of the actual response curves and drug doses of esketamine in the 2 groups are shown in Fig. 2.
Heart rate, SpO2, and mean arterial pressure at all designated time points were collected and analyzed for all patients (Table 3). No significant change was observed between the vital signs at baseline and those after drug administration. The Ramsay Sedation Scale scores obtained at the designated time points are shown in Table 4. The depth of sedation reached peak at 15–20 min after drug administration and remained till the end of the experiment. No significant adverse reactions were observed.
Discussion
We determined that the preoperative ED50 of esketamine was 0.7 (95% CI: 0.54–0.86) mg/kg for the pediatric patients in the series of this study; and no significant adverse events were observed throughout the experimental period. A 0.7 mg/kg dose was able to provide a safe and satisfactory effect against preoperative anxiety and an appropriate sedation effect in the children, as represented by the decreased anxiety, emotional stability, good cooperation, success in falling asleep, no bodily resistance, and smooth separation from their patients/guardians.
Midazolam, dexmedetomidine, and Ketamine are commonly used for preoperative sedation in children. An early in vitro animal experiment suggested that ketamine may be able to exert a potent diastolic effect on the intima of the pulmonary artery, thus reducing pulmonary circulation resistance [13, 14]. However, subsequent clinical studies demonstrated that the inductive dose of ketamine had no significant effect on the pulmonary arterial pressure of children with CHD and pulmonary vascular pressure of children with pulmonary hypertension [15, 16]. Esketamine is a new-type N-methyl-D-aspartate receptor inhibitor with the advantages of fasting action and evident sedative and analgesic effects. There have been many studies on esketamine administration for sedation and analgesia in children through an intravenous, intramuscular, or rectal route alone or in combination with other narcotics [17, 18]. Some studies reported that 2 mg/kg intranasal administration of esketamine can be absorbed quickly and effectively, reaching peak plasma concentration within a mean of 18 ± 13 min [19, 20]. Our study found Ramsay’s Sedation Scale score ≥ 3 occurred approximately 20.5 min in our cohort of children with CHD, which is consistent with the result reported in a previous study.
Unlike the previously reported studies, our study is one of the few studies that confirmed the ED50 within 95% CI after intranasal esketamine administration. We chose the modified sequential method to estimate the results because it is simple and requires a smaller sample size. Additionally, this method is suitable for obtaining quick results, and any effective dose can be determined using PROBIT regression analysis, such as ED90 and ED95. Many previous studies of oral or anorectal medication administration were concerned with pharmacodynamics and safety; and indicated 3–8 mg/kg as a maximum tolerable dose for oral medications. The common sedative effect of 1.5 mg/kg rectal administration was attributed to the high liver first-pass effect, produced after administration, and the bioavailability is only approximately 16%. Esketamine is relatively weak in young children, and its effect is not high as that of rectal administration of midazolam alone. In addition, the incidence of adverse effects is also relatively high [21] For this reason, some researchers have wondered whether it is possible to use larger doses and proposed to conduct further research on the relationship between pharmacodynamics and dosage. Considering that intranasal drug administration quickly acts on the brain due to bypassing the first-pass metabolism, high bioavailability, and loss of drug due to swallowing [22,23,24], esketamine is not added with any preservative. Therefore, it has little simulation on children, and the titer of esketamine is approximately 2-fold that of ketamine. In our pilot experiment, we selected 1 mg/kg of esketamine as the initial dose for intranasal premedication in our cohort of children with CHD to explore the ED50 and safety of intranasal esketamine.
Earlier studies on preoperative medication in children with CHD suggested that both intranasal administrations of 2 mg/kg ketamine and oral administration of 5 mg/kg ketamine were safe and effective for preoperative medication in children with TOF [9]. The sedation onset time of the intranasal medication group was faster than that of the oral medication group. The reason for the discrepancy of our ED50 value from other studies may be that: (1) the criteria for sedation assessment were different, we used the Ramsay Sedation Scale score ≥ 3 and PSAS ≥ 2 as the criteria for successful sedation; (2) we provided the parents/guardians of the participants with complete preoperative information and created a quiet preoperative waiting zone by separating them from other people unconcerned, and the waiting zone was equipped with cartoons and toys appropriate for the psychological features of children; and (3) we provided opportunities for family members to accompany the children and participate in their care. In addition few investigators had used intranasal administration for esketamine rather than ketamine for premedication in pediatrics, thus fewer results can be compared.
Our study found that the ED50 value of intranasal esketamine obtained in our patients was close to the result reported by Weber et al. [8]. Likewise, our patient cohort had no significant cardiovascular and respiratory adverse reactions, suggesting that an intranasal dose is not significantly different from a rectal dose. Weber et al. reported that compared with midazolam alone, combination use of 1–2 mg/kg esketamine could substantially increase the sedation score by 2.5 min after drug administration. Nausea and vomiting are common adverse reactions after intranasal administration of ketamine. The replacement of syringe drug administration by atomizer administration can reduce the incidence of nausea and vomiting by 50%. However we did not observe nausea and vomiting in our cohort of patients, possibly because the dose we used was relatively small and the observation time after sedation was relatively short.
Most researchers also define “cooperation without anxiety” as the criterion of successful sedation without considering the presence or absence of deep sleeping. Intranasal administration of 6 mg/kg ketamine created an appropriate depth of sedation in approximately 92% of cases, with a mean onset time of 5.79 ± 1.42 min. As the dose of ketamine is relatively large, some researchers recommended using the high-concentration of 100 mg/ml [25]. In our opinion, the main purpose of preoperative sedation is to relieve the anxiety of sick children and separate them from their parents peacefully. A deeper sleeping state not only requires a considerably larger amount of medication but will defer the resuscitation time for the children.
Although many studies believe that most children cannot comply with intranasal drug administration, only 1 child in our study had obvious non-compliance and resistance to intranasal premedication and needed physical restraint with the help of the parents for drug administration. The volume of drug administration in this study was less than 0.15 ml, and no child exhibited significant symptoms of pharmacochemical stimulation, suggesting that esketamine has minimal intranasal stimulation and the intranasal route is appropriate for drug administration. The intranasal stimulation symptoms observed in 36.1% of patients administered midazolam differed in several ways from those observed in this study [26], indicating that the pharmacochemical stimulation effect of midazolam is significantly higher than that of esketamine. Due to the concentration ratio of esketamine and data indicating a higher dose requires a higher volume for intranasal administration, which increases the discomfort of the patient and drug proportion passing through the throat and the amount absorbed by the gastrointestinal tract mucosa, we restrained the total amount of intranasal medication of esketamine to less than 0.3 ml, and the intranasal optimal volume dosage to less than 0.15 ml (the maximum amount for each nostril was 0.2 ml) to avoid oral administration of the excessive portion of the drug, which may have reduced bioavailability.
This study has several limitations. Firstly, we failed to make precise discriminations of the pediatric patient personality characteristics before the initiation of the study, knowing that different personalities may affect the sedative outcome on the day of surgery. In addition, we could not stratify the disease type and age because of the relatively small number of included patients. Therefore, we could not include patients of the same age group and the same kind of CHD for analysis. Thirdly, we did not use the atomizer. While atomizers offer a convenient means of administering nasal medication, their use is limited by the financial constraints faced by many caregivers who may require assistance in procuring the relatively expensive nasal atomizers. Finally, we did not further observe the sedative or analgesic effects after the patients entered the operating room.
Conclusions
To our knowledge,this was the first study to report the ED50 of intranasal esketamine before cardiovascular surgery in young children with CHD. Our finding concerning the drug dosage differs from the results reported by most other studies, suggesting that drug administration should be implemented with caution and the target sedation protocol for children should be assessed individually. Other than the complex hemodynamic changes commonly induced by narcotics and sedatives, more attention should be paid to potential neurotoxicities arising from these agents and their interactions with subsequent anesthesia.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- CHD:
-
congenital heart disease
- CI:
-
confidence interval
- ED50 :
-
effective dose
- PSAS:
-
Parental Separation Anxiety Scale
- SpO2 :
-
saturation of peripheral oxygen
- TOF:
-
Tetralogy of Fallot
References
Ahmed MI, Farrell MA, Parrish K, Karla A. Preoperative anxiety in children risk factors and non-pharmacological management. Middle East J Anaesthesiol. 2011;21(2):153–64.
Jung MJ, Libaw JS, Ma K, Whitlock EL, Feiner JR, Sinskey JL. Pediatric distraction on induction of Anesthesia with virtual reality and perioperative anxiolysis: a Randomized Controlled Trial. Anesth Analg. 2021;132(3):798–806.
Mason KP. Paediatric emergence delirium: a comprehensive review and interpretation of the literature. Br J Anaesth. 2017;118(3):335–43.
Li HP, Liu KP, Yao L. Dexmedetomidine in combination with ketamine for pediatric procedural sedation or premedication: a meta-analysis. Am J Emerg Med. 2021;50:442–8.
Lei H, Chao L, Miao T, Ya Jun L, Shen Ling L, Yan Ying P, et al. Incidence and risk factors of bradycardia in pediatric patients undergoing intranasal dexmedetomidine sedation. Acta Anaesthesiol Scand. 2020;64(4):464–71.
van Hoorn CE, Flint RB, Skowno J, Davies P, Engelhardt T, Lalwani K, et al. Off-label use of dexmedetomidine in paediatric anaesthesiology: an international survey of 791 (paediatric) anaesthesiologists. Eur J Clin Pharmacol. 2021;77(4):625–35.
Tervonen M, Pokka T, Kallio M, Peltoniemi O. Systematic review and meta-analysis found that intranasal dexmedetomidine was a safe and effective sedative drug during paediatric procedural sedation. Acta Paediatr. 2020;109(10):2008–16.
Salman S, Tang EKY, Cheung LC, Nguyen MN, Sommerfield D, Slevin L, et al. A novel, palatable paediatric oral formulation of Midazolam: pharmacokinetics, tolerability, efficacy and safety. Anaesthesia. 2018;73(12):1469–77.
Li M, Wang YT, Zhang MZ. Clinical observation of oral administration of Midazolam, ketamine and dexmedetomidine in children with tetralogy of Fallot. J Shanghai Jiaotong Univ. 2017;37(1):71–4.
Weber F, Wulf H, el Saeidi G. Premedication with nasal s-ketamine and midazolam provides good conditions for induction of anesthesia in preschool children. Can J Anaesth. 2003;50(5):470–5.
Lu X, Tang L, Lan H, Li C, Lin H. A comparison of Intranasal Dexmedetomidine, Esketamine or a dexmedetomidine-esketamine combination for induction of Anaesthesia in Children: a randomized controlled double-blind trial. Front Pharmacol. 2021;12:808930.
Pace NL, Stylianou MP. Advances in and limitations of up-and-down methodology: a précis of clinical use, study design, and dose estimation in anesthesia research. Anesthesiology. 2007;107(1):144–52.
Lee TS, Hou X. Vasoactive effects of ketamine on isolated rabbit pulmonary arteries. Chest. 1995;107(4):1152–5.
Oklü E, Bulutcu FS, Yalçin Y, Ozbek U, Cakali E, Bayindir O. Which anesthetic agent alters the hemodynamic status during pediatric catheterization? Comparison of propofol versus ketamine. J Cardiothorac Vasc Anesth. 2003;17(6):686–90.
Williams GD, Maan H, Ramamoorthy C, Kamra K, Bratton SL, Bair E, et al. Perioperative complications in children with pulmonary hypertension undergoing general anesthesia with ketamine. Paediatr Anaesth. 2010;20(1):28–37.
Williams GD, Philip BM, Chu LF, Boltz MG, Kamra K, Terwey H, et al. Ketamine does not increase pulmonary vascular resistance in children with pulmonary hypertension undergoing sevoflurane anesthesia and spontaneous ventilation. Anesth Analg. 2007;105(6):1578–84. table of contents.
Koinig H, Marhofer P. S(+)-ketamine in paediatric anaesthesia. Paediatr Anaesth. 2003;13(3):185–7.
Zheng XS, Shen Y, Yang YY, He P, Wang YT, Tao YY, et al. E.D. (50) and E.D. (95) of propofol combined with different doses of esketamine for children undergoing upper gastrointestinal endoscopy: a prospective dose-finding study using up-and-down sequential allocation method. J Clin Pharm Ther. 2022;47(7):1002–9.
Weber F, Wulf H, Gruber M, Biallas R. S-ketamine and s-norketamine plasma concentrations after nasal and i.v. administration in anesthetized children. Paediatr Anaesth. 2004;14(12):983–8.
Flint RB, Brouwer CNM, Kränzlin ASC, Lie AHL, Bos AP, Mathôt RAA. Pharmacokinetics of S-ketamine during prolonged sedation at the pediatric intensive care unit. Paediatr Anaesth. 2017;27(11):1098–107.
Marhofer P, Freitag H, Hochtl A, Greher M, Erlacher W, Semsroth M. S(+)-ketamine for rectal premedication in children. Anesth Analg. 2001;92(1):62–5.
Boddu SHS, Kumari S. A Short Review on the Intranasal Delivery of Diazepam for Treating Acute Repetitive Seizures.Pharmaceutics. 2020;12(12).
Keller LA, Merkel O, Popp A. Intranasal drug delivery: opportunities and toxicologic challenges during drug development. Drug Deliv Transl Res. 2022;12(4):735–57.
Knoester PD, Jonker DM, Van Der Hoeven RT, Vermeij TA, Edelbroek PM, Brekelmans GJ, et al. Pharmacokinetics and pharmacodynamics of Midazolam administered as a concentrated intranasal spray. A study in healthy volunteers. Br J Clin Pharmacol. 2002;53(5):501–7.
Bahetwar SK, Pandey RK, Saksena AK, Chandra G. A comparative evaluation of intranasal midazolam, ketamine and their combination for sedation of young uncooperative pediatric dental patients: a triple blind randomized crossover trial. J Clin Pediatr Dent. 2011;35(4):415–20.
Sheta SA, Al-Sarheed MA, Abdelhalim AA. Intranasal dexmedetomidine vs midazolam for premedication in children undergoing complete dental rehabilitation: a double-blinded randomized controlled trial. Paediatr Anaesth. 2014;24(2):181–9.
Acknowledgements
We thank all colleagues in the Department of Anesthesiology, Fujian Children’s Hospital, Shanghai Children’s Medical Center for their support in analyzing and collecting data for the paper, and for correcting the language and grammatical structure of the manuscript. We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
H.B. G and J.J. H were the major contributors to the drafting of the manuscript. J.B. and D.Q. L were responsible for contacting the hospitals. D.Q. L analyzed and interpreted the data. The questionnaire was designed by H.B. G, J.J. H, J B, and D.Q. L. All authors read and approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of Shanghai Children’s Medical Center. Written informed consent to participate in this study was provided by the participant’s legal guardian/next of kin. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, J., Liu, D., Bai, J. et al. Median effective dose of esketamine for intranasal premedication in children with congenital heart disease. BMC Anesthesiol 23, 129 (2023). https://doi.org/10.1186/s12871-023-02077-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-02077-1