Abstract
Background
Spontaneous breathing potentially injures lungs and diaphragm when spontaneous effort is vigorous in acute respiratory distress syndrome (ARDS) while immobility also has risks of Intensive Care Unit (ICU) acquired weakness and diaphragm atrophy. Thus, ventilatory strategy to mitigate strong spontaneous effort should be promptly established without a systemic use of neuromuscular blocking agent. Here, we investigated the impacts of positive end-expiratory pressure (PEEP) and body position on the capacity of force generation from diaphragm following bilateral phrenic nerve stimulations in a rabbit ARDS model.
Methods
Using lung-injured rabbits, we measured 1) transdiaphragmatic pressure by bilateral phrenic nerve stimulation and 2) end-expiratory lung volume using computed tomography, under two different levels of PEEP (high, low) and body positions (supine, prone).
Results
Overall, transdiaphragmatic pressure was the highest at low PEEP in supine position and the lowest at high PEEP in prone position. Compared to values in low PEEP + supine, transdiaphragmatic pressure was significantly reduced by either prone alone (the same PEEP) or increasing PEEP alone (the same position) or both combinations. End-expiratory lung volume was significantly increased with increasing PEEP in both positions, but it was not altered by body position.
Interpretation
The capacity of force generation from diaphragm was modulated by PEEP and body position during mechanical ventilation in ARDS. Higher PEEP or prone position per se or both was effective to decrease the force generation from diaphragm.
Similar content being viewed by others
Introduction
Spontaneous breathing potentially injures lungs and diaphragm when spontaneous effort is vigorous in acute respiratory distress syndrome (ARDS) [1,2,3,4,5]. The key mechanism whereby spontaneous breathing may injure lungs and (potentially) diaphragm is the large excursion of diaphragm (e.g., large tidal volume, high transpulmonary pressure, large pendelluft, high transvascular pressure) [6]. Silence of respiratory muscles by the systemic use of neuromuscular blockade improved survival in severe ARDS[7], but it may have a risk of ICU-acquired weakness and diaphragm atrophy[2]. Thus, a promising strategy to maintain modest level of spontaneous breathing effort (without paralyzing patients) should be established promptly [8].
Several factors increase the strength -and injury potential- of spontaneous breathing effort, including respiratory drive from cortical stimuli, chemoreceptive stimuli, and mechanical stimuli, as well as capacity of force generation from diaphragm [8,9,10]. Previous studies reported that higher positive end-expiratory pressure (PEEP) or prone position decreased spontaneous breathing effort in ARDS[1, 11,12,13], but distinct mechanism has been still unidentified, e.g., decreased respiratory drive or altered capacity of force generation from diaphragm. PEEP and prone position are known to have similar effects of restoring lung volume and thus potentially may change the force–length relationship of the diaphragm, which leads to decrease spontaneous breathing effort, independent of respiratory drive.
Therefore, we investigated the impacts of PEEP and body position on the capacity of force generation from diaphragm following bilateral phrenic nerve stimulations in a rabbit ARDS model.
Methods
The study was approved by the Laboratory Investigation Committee, Osaka University Medical School (#03,033,000). Animals were cared for in accordance with the University’s standards for care and use of laboratory animals, and all procedures were performed in accordance with the National Institutes of Health ‘Guidelines for the Care and Use of Laboratory Animals’. This study was carried out in compliance with the ARRIVE guidelines.
The schematic of study protocol is presented in Fig. 1. Ten New Zealand white rabbits (adult, male, 3.6 ± 0.2 kg; five in each series) were anesthetized with ketamine (20–30 mg.kg−1.h−1) and dexmedetomidine (2 μg.kg−1.h−1) and tracheostomized. Then, animals were ventilated in supine position with tidal volume (VT) 8 ~ 10 mL kg−1; respiratory rate 30–50 breaths.min−1 (targeted for PaCO2 ≈40 mmHg); and PEEP 3cmH2O, using Servo 300 ventilator (Siemens-Elema AB, Solna, Sweden) or with Puritan Bennett™ 840 (Covidien, Mansfield, MA, USA), either of which is available. An esophageal and gastric balloon (CareFusion, San Diego, USA) was inserted to estimate transdiaphragmatic pressure (Pdi), filled with air (0.3 mL as minimal non-stress volume for esophageal balloon; 2.0 mL for gastric balloon) and its position of esophageal balloon was verified as above[14].
Lung injury
Lung injury was established by repeated saline lavage (targeted PaO2/FiO2 ratio ≈200 mmHg) at PEEP of 3cmH2O. All animals were temporarily paralyzed with a bolus of rocuronium bromide during establishment of lung injury. No residual effect of neuromuscular blocking agent to affect respiratory muscles was confirmed by the same amount of maximal transdiaphragmatic pressure generated with supramaximal stimuli of bilateral phrenic nerves as observed at baseline, i.e., before the induction of lung injury.
Experimental protocol
AnimalS were randomly assigned to all of four conditions as follows:
-
Low PEEP, Supine;
-
High PEEP, Supine;
-
Low PEEP, Prone;
-
High PEEP, Prone;
Measurements in each condition were performed approximately in an hour. Lungs were fully recruited by stepwise increases of airway pressure among each sequence, and then we waited for at least 30 min before starting the measurements. The animals were ventilated with volume-controlled ventilation: targeting tidal volume of ≈7 mL kg−1, respiratory rate between 60 to 120 min−1(targeted to PaCO2 < 50 mmHg) and FIO2 of 1.0. In our pilot study, decremental PEEP steps from 18 to 0 cmH2O showed that oxygenation started to decrease below PEEP of ≈10 cmH2O. Based on this finding, high PEEP and low PEEP was defined as 10 and 3cmH2O respectively.
Series 1- Bilateral phrenic nerve stimulation
Bilateral phrenic nerves were exposed and identified by electrical stimulation with bipolar nerve block needles (Hakko, Nagano, Japan). The intensity of voltage was gradually increased until maximal value of Pdi was obtained at end-expiration (maintained lung volume by tube clamp), by stimulating bilaterally phrenic nerves with 500 ms train duration with square-wave pulse of 0.15 ms duration at 75 Hz[15]. Supramaximal phrenic nerve stimuli were defined as × 1.25 of the voltage where maximal value of Pdi was obtained[16]. The force generation from diaphragm at end-expiration (maintained lung volume by tube clamp) was evaluated by measuring Pdi for 2 s train duration with square-wave pulse of 0.15 ms duration at frequencies of 10, 30, 50, 80 and 100 Hz during bilateral supramaximal voltage phrenic nerve stimulation. Transdiaphragmatic pressure reduction was expressed with averaging how much Pdi was reduced, taken from all stimulation frequencies in each condition, compared with low PEEP, Supine.
Series 2- End-expiratory lung volume
Computed tomography (CT) scans were performed (SOMATOM Emotion 16; Siemens Medical Solutions, Erlangen, Germany). Unenhanced helical CT scans (matrix: 512 rows × 512 columns; slices 1.5 mm; voltage 130 kV; tube current 240 mA) were performed during an end-expiratory pause with tube clumping. The images were analyzed using Osirix MD image viewer and analysis software program (version 12.5.1; Pixmeo, Geneva, Switzerland) for segmentation and volumetric measurements. The heart and diaphragm were excluded from the regions of interest. The volume of hyperinflation, normal aeration, poor aeration, and non-aeration was calculated in end-expiratory images. We identified each lung compartment according to their densities in Hounsfield Units: non-aeration (+ 100 to -200 HU), poor aeration (-201 to -500 HU), normal aeration (-501 to -900 HU), and hyperinflation (-901 to -1000 HU)[20]. The end-expiratory lung volume was calculated based on densities expressed in Hounsfield units of -1000 to -201 (excluding non-aeration), modified from previous CT study[17].
Definitions
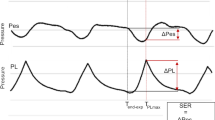
Definitions of pulmonary pressures was as follows.
-
Peak (inspiratory) transpulmonary pressure, Peak transpulmonary pressure = maximal value of [airway pressure – esophageal pressure] cmH2O.
-
Plateau (inspiratory) transpulmonary pressure, Plateau transpulmonary pressure = [Plateau airway pressure – end-inspiratory esophageal pressure] cmH2O
-
Plateau pressure, airway pressure measured during a short inspiratory hold (i.e. zero flow phase)
-
Driving Pressure = [Plateau airway pressure – PEEP] cmH2O
-
Compliance of the respiratory system = [VT/(Driving Pressure)] mL·cmH2O.−1
-
Compliance of the lung = [VT/(Driving transpulmonary pressure)] mL·cmH2O.−1
-
Transdiaphragmatic pressure = [the sum of change in esophageal pressure and change in gastric pressure] This is because the absolute value of abdominal pressure was changed by body position.
Statistical analysis
Statistical analysis were performed using SPSS 24.0.0.0 for Windows (SPSS, Chicago, IL, USA). 1-way analysis of variance (ANOVA) with repeated measures evaluated the impacts of frequency on Pdi and 1-way ANOVA evaluated the effects of condition on Pdi, respiratory parameters, and CT measures. In the post hoc analysis, a Dunnett’s test was used to compare repeated values with the value at the start of the stimulation (i.e. 10 Hz), and Tukey’s pair-wise multiple comparison test was used to determine condition differences. All tests were 2-tailed, and differences were considered significant when p < 0.05.
Results
Respiratory and hemodynamics parameters are summarized in Table 1. VT was low and similar (volume-controlled ventilation: ≈7 mL/kg) in all of four conditions. PEEP (and thus expiratory transpulmonary pressure) was significantly higher in High PEEP conditions, as anticipated. PaO2/FIO2 was the lowest in Low PEEP, Supine (80 ± 46 mmHg) and was significantly improved by increasing PEEP or changing position or both combinations. Driving pressure, respiratory system compliance and lung compliance did not significantly differ among four conditions (Table 1).
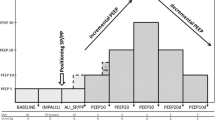
Transdiaphragmatic pressure was greater as stimulation frequency was higher in all conditions (Fig. 2). Overall, transdiaphragmatic pressure was the highest at low PEEP in supine position and the lowest at high PEEP in prone position (Fig. 2). Compared to values in low PEEP + supine, transdiaphragmatic pressure was significantly reduced by either changing position to prone alone (Low PEEP, Prone: -27.9 ± 30.9%) or increasing PEEP alone (High PEEP, Supine: -51.7 ± 16.6%) or both combinations (High PEEP, Prone: -62.0 ± 14.6%) (Fig. 3B).
Transdiaphragmatic pressure-frequency curve in all conditions. Data represent mean ± SD. Transdiaphragmatic pressure was greater as stimulation frequency was higher in all conditions (p < 0.01 at 50, 80 and 100 Hz vs. 10 Hz). Overall, transdiaphragmatic pressure was the highest at low PEEP in supine position and the lowest at high PEEP in prone position. Compared to values in low PEEP + supine, transdiaphragmatic pressure was significantly reduced by either changing position to prone alone (the same PEEP) or increasing PEEP alone (the same position) or both combinations. * p < 0.05 vs. all conditions; + p < 0.05 vs. high PEEP conditions; † p < 0.05 vs. low PEEP + prone. Abbreviations: PEEP positive end-expiratory pressure; SD standard deviation
End-expiratory lung volume and transdiaphragmatic pressure reduction in all conditions. Data represent mean ± SD. End-expiratory lung volume calculated using CT was presented in all conditions (A). End-expiratory lung volume was higher in high PEEP conditions vs. low PEEP conditions. Body position did not affect end-expiratory lung volume. Representative CT images from the same subject are shown in (A). Representative CT images are presented. Aerated lung regions are reduced because of lung collapse predominant in dependent (dorsal in supine position, ventral in prone position) lung regions in low PEEP conditions. Transdiaphragmatic pressure reduction (vs. low PEEP + supine) is shown in (B). Transdiaphragmatic pressure is reduced by higher PEEP (regardless of body position) and prone position (regardless of PEEP levels). * p < 0.01 vs. all conditions; + p < 0.05 vs. low PEEP conditions. Abbreviations: CT computed tomography; HU Hounsfield unit; PEEP positive end-expiratory pressure; SD standard deviation
CT analysis found that high PEEP in both positions decreased the amount of non-aeration (Table) and thus end-expiratory lung volume was significantly increased with increasing PEEP in both positions (Fig. 3A). Regardless of PEEP levels, however, end-expiratory lung volume was not altered by body position (Fig. 3A).
Discussion
The current study found that in a rabbit ARDS model, the capacity of force generation from diaphragm was altered by PEEP and body position- transdiaphragmatic pressure following bilateral phrenic nerve stimulation was decreased by increasing PEEP (regardless of body position) and changing position from supine to prone (regardless of PEEP levels).
Two potential strategies were revealed to modulate the force generated by diaphragmatic contraction and thereby to mitigate effort-dependent lung injury in ARDS. First, higher PEEP was associated with less spontaneous breathing effort (reflected by esophageal pressure) during mechanical ventilation in ARDS[1, 11, 12, 18] although its distinct mechanism has been unknown. Here, we confirmed that PEEP was an independent mechanistic determinant of force generation from diaphragm by altering end-expiratory lung volume (evidenced by CT). A recent clinical study using healthy volunteer also showed higher PEEP decreased neuromechanical efficiency of the diaphragm [19]. Of course, higher lung volume is known to shorten diaphragm length, resulting in less force generation from diaphragm[9, 10].
Second, body position per se modulated the capacity of force generation from diaphragm. Transdiaphragmatic pressure was increased in supine position and decreased in prone position. This effect was independent of PEEP levels or end-expiratory lung volume. This is probably because prone position per se shorten diaphragm length even with the same end-expiratory lung volume due to altered chest wall configuration and diaphragm geometry[20, 21]. Our findings partially explain recent clinical observations. Prone position was associated with less spontaneous effort (estimated by esophageal pressure), resulting in less systemic inflammation in severe ARDS[13]. Further, awake prone position decreased respiratory rate and decreased the need of intubation[22]. Thus, the current study may reveal a protective mechanism of prone position to mitigate effort-dependent lung injury in ARDS.
The model studied here is well known to be a model of ‘recruitable’ lung and rabbits are naturally prone. Lung recruitment was calculated as the proportion of the total lung weight accounted for by nonaerated lung tissue (expressed in HU between + 100 and -200) in which aeration was restored by PEEP of 10 cmH2O and 3 cmH2O in supine position[23]. Indeed, lung recruitment calculated between PEEP of 3 and 10 cmH2O was 23 ± 15%, confirming that our surfactant-depleted rabbit ARDS model was very recruitable. In contrast, human ARDS usually has heterogeneous etiology, variable lung recruitability and the far longer usual time-course. Although the model studied here has been successfully used to illustrate key mechanism of the capacity of force generation from diaphragm, caution is necessary in extrapolating the current data to the clinical context. Further study would be necessary to investigate the impacts of PEEP and body position on the capacity of force generation from diaphragm in a model of ‘non-recruitable’ lung. In this study, prone position had no impact on end-expiratory lung volume. Previous review reported the impacts of prone position on end-expiratory lung volume were conflicting (probably depending on lung recruitablity, shape of chest wall, the presence of abdominal hypertension and the presence of support)[24].The long-term effect of strategy to alter the capacity of force generation from diaphragm is unknown and of note, a previous animal study showed that prolonged application of higher PEEP caused longitudinal muscle fiber atrophy[25].
Conclusions
The capacity of force generation from diaphragm was modulated by PEEP and body position during mechanical ventilation in ARDS. Higher PEEP or prone position per se or both was effective to decrease the force generation from diaphragm.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute Respiratory Distress Syndrome
- PEEP:
-
Positive End-Expiratory Pressure
- CT:
-
Computed Tomography
References
Morais CCA, Koyama Y, Yoshida T, Plens GM, Gomes S, Lima CAS, Ramos OPS, Pereira SM, Kawaguchi N, Yamamoto H, et al. High Positive End-Expiratory Pressure Renders Spontaneous Effort Noninjurious. Am J Respir Crit Care Med. 2018;197(10):1285–96.
Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, Vorona S, Sklar MC, Rittayamai N, Lanys A, et al. Mechanical Ventilation-induced Diaphragm Atrophy Strongly Impacts Clinical Outcomes. Am J Respir Crit Care Med. 2018;197(2):204–13.
Hurtado DE, Erranz B, Lillo F, Sarabia-Vallejos M, Iturrieta P, Morales F, Blaha K, Medina T, Diaz F, Cruces P. Progression of regional lung strain and heterogeneity in lung injury: assessing the evolution under spontaneous breathing and mechanical ventilation. Ann Intensive Care. 2020;10(1):107.
Tonelli R, Fantini R, Tabbi L, Castaniere I, Pisani L, Pellegrino MR, Della Casa G, D’Amico R, Girardis M, Nava S, et al. Early Inspiratory Effort Assessment by Esophageal Manometry Predicts Noninvasive Ventilation Outcome in De Novo Respiratory Failure. A Pilot Study. Am J Respir Crit Care Med. 2020;202(4):558–67.
Goligher EC, Dres M, Patel BK, Sahetya SK, Beitler JR, Telias I, Yoshida T, Vaporidi K, Grieco DL, Schepens T, et al. Lung and Diaphragm-Protective Ventilation. Am J Respir Crit Care Med. 2020;202(7):950–61.
Yoshida T, Fujino Y, Amato MB, Kavanagh BP. Fifty Years of Research in ARDS. Spontaneous Breathing during Mechanical Ventilation. Risks, Mechanisms, and Management. Am J Respir Crit Care Med. 2017;195(8):985–92.
Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363(12):1107–16.
Goligher EC, Jonkman AH, Dianti J, Vaporidi K, Beitler JR, Patel BK, Yoshida T, Jaber S, Dres M, Mauri T, et al. Clinical strategies for implementing lung and diaphragm-protective ventilation: avoiding insufficient and excessive effort. Intensive Care Med. 2020;46(12):2314–26.
Pengelly LD, Alderson AM, Milic-Emili J. Mechanics of the diaphragm. J Appl Physiol. 1971;30(6):797–805.
Laghi F, Harrison MJ, Tobin MJ. Comparison of magnetic and electrical phrenic nerve stimulation in assessment of diaphragmatic contractility. J Appl Physiol (Bethesda, Md : 1985). 1996;80(5):1731–42.
Teggia Droghi M, De Santis Santiago RR, Pinciroli R, Marrazzo F, Bittner EA, Amato MBP, Kacmarek RM, Berra L. High Positive End-Expiratory Pressure Allows Extubation of an Obese Patient. Am J Respir Crit Care Med. 2018;198(4):524–5.
Rossi FS, Costa ELV, Iope D, Pacce PHD, Cestaro C, Braz L, Bousso A, Amato MBP. Pendelluft detection using Electrical Impedance Tomography in an infant. Keep those images in mind! Am J Respir Crit Care Med. 2019;200(11):1427–9.
Yoshida T, Tanaka A, Roldan R, Quispe R, Taenaka H, Uchiyama A, Fujino Y. Prone Position Reduces Spontaneous Inspiratory Effort in Patients with Acute Respiratory Distress Syndrome: A Bicenter Study. Am J Respir Crit Care Med. 2021;203(11):1437–40.
Baydur A, Behrakis PK, Zin WA, Jaeger M, Milic-Emili J. A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis. 1982;126(5):788–91.
Jiang TX, Reid WD, Road JD. Delayed diaphragm injury and diaphragm force production. Am J Respir Crit Care Med. 1998;157(3 Pt 1):736–42.
Sassoon CS, Caiozzo VJ, Manka A, Sieck GC. Altered diaphragm contractile properties with controlled mechanical ventilation. J Appl Physiol (Bethesda, Md : 1985. 2002;92(6):2585–95.
Wrigge H, Zinserling J, Neumann P, Muders T, Magnusson A, Putensen C, Hedenstierna G. Spontaneous breathing with airway pressure release ventilation favors ventilation in dependent lung regions and counters cyclic alveolar collapse in oleic-acid-induced lung injury: a randomized controlled computed tomography trial. Crit Care (London, England). 2005;9(6):R780-789.
Yoshida T, Roldan R, Beraldo MA, Torsani V, Gomes S, De Santis RR, Costa EL, Tucci MR, Lima RG, Kavanagh BP, et al. Spontaneous Effort During Mechanical Ventilation: Maximal Injury With Less Positive End-Expiratory Pressure. Crit Care Med. 2016;44(8):e678-688.
Jansen D, Jonkman AH, Vries HJ, Wennen M, Elshof J, Hoofs MA, van den Berg M, Man AME, Keijzer C, Scheffer GJ, et al. Positive end-expiratory pressure affects geometry and function of the human diaphragm. J Appl Physiol (Bethesda, Md : 1985. 2021;131(4):1328–39.
Sprung J, Deschamps C, Margulies SS, Hubmayr RD, Rodarte JR. Effect of body position on regional diaphragm function in dogs. J Appl Physiol (Bethesda, Md : 1985). 1990;69(6):2296–302.
Rehan VK, Nakashima JM, Gutman A, Rubin LP, McCool FD. Effects of the supine and prone position on diaphragm thickness in healthy term infants. Arch Dis Child. 2000;83(3):234–8.
Ehrmann S, Li J, Ibarra-Estrada M, Perez Y, Pavlov I, McNicholas B, Roca O, Mirza S, Vines D, Garcia-Salcido R, et al. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med. 2021;9(12):1387–95.
Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354(17):1775–86.
Gattinoni L, Taccone P, Carlesso E, Marini JJ. Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am J Respir Crit Care Med. 2013;188(11):1286–93.
Lindqvist J, van den Berg M, van der Pijl R, Hooijman PE, Beishuizen A, Elshof J, de Waard M, Girbes A, Spoelstra-de Man A, Shi ZH, et al. Positive End-Expiratory Pressure Ventilation Induces Longitudinal Atrophy in Diaphragm Fibers. Am J Respir Crit Care Med. 2018;198(4):472–85.
Acknowledgements
N.A.
Funding
Grant-in-Aid for Young Scientists (#19K18294), the Ministry of Education, Culture, Sports, Science and Technology, Japan (TY), Grant for the Promotion of Joint Research, Fukuda Foundation for Medical Technology, Japan (TY).
Author information
Authors and Affiliations
Contributions
AMFF conducted the study, collected the data, analyzed the data, and wrote the manuscript. TY designed the study, analyzed the data, wrote the manuscript, revised manuscript, and supervised the study. HH conducted the study and collected the data. HI conducted the study and collected the data. YF interpreted all data and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Laboratory Investigation Committee, Osaka University Medical School (#03033000). Animals were cared for in accordance with the University’s standards for care and use of laboratory animals, and all procedures were performed in accordance with the National Institutes of Health ‘Guidelines for the Care and Use of Laboratory Animals’. This study was carried out in compliance with the ARRIVE guidelines.
Consent for publication
N.A.
Competing interests
The Authors declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Firstiogusran, A.M.F., Yoshida, T., Hashimoto, H. et al. Positive end-expiratory pressure and prone position alter the capacity of force generation from diaphragm in acute respiratory distress syndrome: an animal experiment. BMC Anesthesiol 22, 373 (2022). https://doi.org/10.1186/s12871-022-01921-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-022-01921-0