Abstract
Background
To evaluate the usefulness of mean platelet volume (MPV), a marker of inflammation and stress, for predicting weaning failure in patients undergoing invasive mechanical ventilation (IMV) compared to traditional inflammation markers.
Methods
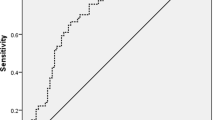
The retrospective observational study including patients who received IMV and underwent spontaneous breathing trial (SBT) was conducted in ICU at Beijing Chao-Yang hospital in China from January, 2013 to December, 2019. According to the weaning outcome, MPV, leukocyte count and C-reaction protein(CRP) were compared between weaning failure and weaning success group. Receiver-operating characteristics (ROC) curves and multivariate logistical regression analysis were constructed to analyze the value of these inflammatory markers for predicting weaning failure.
Results
A total of 261 patients were enrolled in the study and 54 patients (20.7%) experienced weaning failure (45 SBT failure and 9 extubation failure after successful SBT). MPV was a better predictor for weaning failure (AUC 0.777;95%CI, 0.722–0.826) than leukocyte count (AUC 0.6;95%CI,0.538–0.66) and CRP (0.627;95%CI,0.565–0.685). The cutoff value of MPV for predicting weaning failure was 11.3 fl with sensitivity 55.56%, specificity 87.92%, and diagnostic accuracy 81.22%. According to multivariate logistic regression analyses, MPV > 11.3 fl was an independent risk factor for predicting weaning failure.
Conclusions
MPV could be a more valuable marker for predicting weaning failure. and the patients with MPV > 11.3 fl should be attentively evaluated before weaning since they are at high risk of weaning failure, and it would be auspicable for those patients to undergo a noninvasive ventilation or high-flow nasal cannula oxygen therapy after extubation or even an early tracheostomy.
Similar content being viewed by others
Background
Invasive mechanical ventilation (IMV) is a procedure widely used for life support in intensive care unit (ICU), however, liberating from IMV is an challenging problem to critical care physicians [1]. The weaning process may account for a significant proportion of total ventilation time, which can delay extubation and lead to complications and/or death [2, 3]. Although a spontaneous breathing trial (SBT) is the major diagnostic test to determine whether patients can be successfully extubated, about 19% of critically ill patients with successful SBT still need reintubation, which is associated with high morbidity and mortality [4]. Hence, it is critical to improve the accuracy of methods predicting weaning outcome.
It has been reported that platelet plays an important role in the procedure of inflammation and immunity [5].Mean platelet volume (MPV) is an simple, easy available and accurate indicator of platelet size and function, and is considered to be a crucial inflammatory marker [6]. In some inflammatory clinical conditions, increasing MPV has been regard as a poor prognostic indicator for patients in respiratory ICU [7]. Among sepsis patients, an increase in mean platelet volume from baseline is associated with mortality in patients with severe sepsis or septic shock [8]. Among influenza pneumonia patients, the change of MVP strongly predicts acute respiratory distress syndrome [9]. It was also reported that higher MPV was an independent risk factors for the poor prognosis of patients with acute pulmonary embolism [10]. Among some patients with surgery, MPV values were significantly higher in the non-survivors following acute abdominal surgery [11], and patients with increased MPV showed lower rates of 1-year survival following undergoing cytoreductive surgery with hyperthermic intraperitoneal chemotherapy [12]. In addition, MPV also has been shown to be a valuable prognostic marker for pulmonary hypertension in chronic obstructive pulmonary disease (COPD) patients [13], coronary artery disease [14], type 2 diabetes mellitus [15].
Critically ill patients are generally in a high state of inflammation, and patients undergoing endotracheal intubation and subsequent IMV show a robust pulmonary inflammation response [16]. Moreover, mechanical ventilation augments preexisting lung injury and inflammation [17]. Besides that, weaning process entails an higher pulmonary and cardiovascular stress among patients who fail to wean than those who are successfully weaned [18]. Hence, weaning failure patients suffer more inflammatory response and stress. However, there were few studies focusing on the relationships between the inflammation or stress and weaning outcome.
Accordingly, we assumed that MPV would be higher in weaning failure patients than in weaning success patients. And we evaluated the effectiveness of MPV for predicting weaning failure in patients receiving IMV, compared to traditional inflammatory markers such as leukocyte counts, levels of C-reactive protein (CRP).
Methods
Study design
The retrospective observational study involving 261 patients receiving IMV admitted to ICU of Beijing Chao-Yang Hospital was conducted from January, 2013 to December, 2019. The weaning outcome flowing chart was shown in Fig. 1.
The ethics committee of the Beijing Chao-Yang Hospital, Capital Medical University approved this study (NO.2020-KE-94). Because of retrospective study, written informed consent was waived by the ethics committee of the Beijing Chao-Yang Hospital, Capital Medical University which gave approval to the verbal consent. All patients were informed by telephone about this research and their consents were obtained, and we keep patient clinical data confidential. All procedures were in accordance with Helsinki Declaration.
Inclusion criteria
All patients intubated and mechanically ventilated for not less than 48 h were considered eligible for the study if they fulfilled the following: resolution of causes of acute respiratory failure; adequate cough reflex; absence of excessive tracheobronchial secretion; adequate oxygenation (e.g., arterial oxygen saturation > 90% or arterial oxygen tension/fraction of inspired oxygen [PaO2/FiO2] ≥ 150 mmHg, both on the FiO2 of ≤ 0.4 and the positive end-expiratory pressure of ≤ 8 cmH2O); adequate ventilatory status (e.g., respiratory rate [RR] ≤ 35 breaths/min with tidal volume ≥ 5 mL/kg of predicted body weight and no significant respiratory acidosis); stable hemodynamics (e.g., heart rate [HR] < 120 beats/min; systolic blood pressure [SBP], 90–160 mmHg; and no or minimal vasopressor use); adequate mentation (e.g., arousable or glasgow coma scale ≥ 13 with no continuous sedative infusions); body temperature < 38 ℃; hemoglobinemia ≥ 80 g/L; and acceptable electrolytes.
Exclusion criteria
Age < 18 years; pregnancy; tracheotomy or other upper airway disorders; mechanically ventilated less than 48 h; intubated before admission; abandoned before extubation; neuromuscular disease; lack of cooperation; decision to limit active treatment; and refusal of research authorization; incomplete data.
Weaning protocol
A 2 h-SBT was performed in all eligible patients, which allowed the patients to breathe spontaneously through a T-tube circuit with the FiO2 set at the same level used during IMV while the patients were in a semi-recumbent position (45°). The SBT was the first trial for every patient. During the trial, basic vital signs were detected, such as respiratory rate (RR), systolic blood pressure (SBP), heart rate (HR), peripheral oxygen saturation (SpO2), five-lead electrocardiographic tracing. Arterial blood gases were analyzed at the beginning and the end of the SBT.
A criteria for SBT failure were: (1)arterial pH < 7.32 with arterial carbon dioxide tension (PaCO2) ≥ 10 mmHg higher than baseline; (2)RR > 35 breaths/min or ≥ 50% higher than baseline; (3)peripheral oxygen saturation (SpO2) < 90% or PaO2 ≤ 60 mmHg at FiO2 ≥ 0.4; (4)HR > 140 beats/min or ≥ 20% higher/lower than baseline;(5) SBP > 180 or < 90 mmHg or ≥ 20% higher/lower than baseline; (6)use of accessory respiratory muscles, or thoracic-abdominal paradoxical movement; decreased consciousness, agitation, or diaphoresis. Patients free of these features at the end of SBT were considered to succeed the SBT and subsequently extubated.
Weaning failure was defined as SBT failure or reintubation within 48 h following extubation [20]. Weaning success was defined as extubation successfully and the absence of reintubation for more than 48 h following extubation. We share the same weaning protocol in our department, and this was described in our previous research [19].
Data collection
Patients’ demographic and baseline characteristics were recorded at enrollment, including age, sex, body mass index (BMI), acute physiology and chronic health evaluation II (APACHE II) score, IMV duration before weaning, comorbidities and acute causes of IMV. Basic vital signs and arterial blood gas were recorded. After extubation, the following was recorded: success or failure of weaning, length of stay (LOS)in ICU, LOS in hospital, ICU mortality, and hospital morality, 28-day survival rate. For patients discharged within 28 days, we followed up their survival status after discharge by telephone.
Complete blood cell counts and CRP at initiation of the SBT were measured. Complete blood cell counts were measured by automatic blood analyzer. CRP concentrations were measured using immunoscatter turbidimetry by Goldsite Aristo (Goldsite, Ltd., China), and the normal value of CRP ranges from 0 to 5 mg/L.
Statistics
For comparing categorical data, described as frequencies and percentages, Chi square (χ2) test was performed. For Continuous variables, the normal distribution was tested by the Kolmogorov–Smirnov test. Student’s t test was employed for normally distributed data and expressed as mean ± standard deviation. The Mann–Whitney U-test was used for non-normally distributed data and expressed by median (25th-75th percentile). Spearman correlation were used for correlation analysis between MPV and other variables, and the results were displayed as rho and P values. We utilized the receiver-operating characteristic (ROC) analysis to evaluate the sensitivity and specificity of inflammatory markers for predicting weaning failure and to determine the optimum cutoff value for the studied diagnostic markers. Finally, to determine the significant predicting marker of weaning failure, the univariate analysis was used first and then the logistic regression analysis was used to perform a multivariate analysis by a conditional backward stepwise regression model, which resulted in adjusted odds ratios (OR, 95%CI). All analyses were two-tailed, and probability value (p value) less than 0.05 was considered statistically significant. All data were done using SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) version 22 for Microsoft Windows.
Results
Patients’ characteristics and weaning outcome
A total of 261 patients were included in the study, as shown in Fig. 1. Of these, 54 failed the weaning process (45 failed the SBT and 9 extubation failure after successful SBT), 207 succussed the weaning finally. Table 1 shows the baseline characteristics of the patients. Compared to weaning success patients, the failure group had longer IMV duration prior to weaning, higher APACHE II score, lower rates of postoperation. There were significant differences between the two groups in RR, SpO2, SBP, PaCO2, PaO2, FiO2, PaO2/FiO2 (Table 2).
Pre-weaning platelet indices, leukocyte count and CRP
As shown in Table 2 and Fig. 2, leukocyte count(P = 0.023), MPV(P = 0.000), and CRP(P = 0.004) were statistically higher in the weaning failure group than that in the success group. Platelet count was lower in weaning failure group (P = 0.031). Platelet large cell ratio tended to be higher in the failure patients, but the p-value did not reach the significance level(P = 0.056). There was not significant difference in platelet distribution width (PDW) between the groups. By correlation analysis, MPV was positively correlated with CRP (rho = 0.2, P = 0.001) and APACHE II score (rho = 0.197, P = 0.001), while it was negatively related with platelet count (rho = -0.246, P = 0.000) and PaO2/FIO2(rho = -0.15P = 0.015). However, there was not significant correlation between MPV and leukocyte count (Table 3).
Predicting ability of MPV, leukocyte count, and CRP level for weaning failure
The ROC curves of the MPV, leukocyte count, and CRP were shown in Fig. 3. Table 4 showed that the AUC of MPV (0.777;95%CI,0.722–0.826) was higher than that of leukocyte count (0.6;95%CI,0.538–0.66), and CRP (0.627;95%CI,0.565–0.685). The diagnostic accuracy of MPV is highest among the three inflammatory markers.
The cutoff value for predicting weaning failure was MPV > 11.3 fl, leukocyte count > 8.9 × 109/L, and CRP > 67 mg/L.
According to multivariate logistic regression analyses, both MPV > 11.3 fl and leukocyte count > 8.9 × 109/L were independent factors for predicting weaning failure(Table 5).Multivariate logistic regression was performed with the covariates which showed the P < 0.02 by univariate analysis, including APACHE II score, IMV duration prior to SBT, postoperation, pre-weaning PaCO2, PaO2/FiO2, SPO2, SBP. Age, sex, and BMI were also included since they often effect prognosis of various diseases [21,22,23].
Patients’ outcome grouped by MPV cutoff value
Table 6 shows the baseline data, vital signs, arterial blood gas and traditional inflammation markers according to MPV cutoff value. Compared to patients with MPV ≤ 11.3 fl, patients in the group of MPV > 11.3 fl had higher APACHE II score, longer ICU LOS, increased frequency of patients with immunosuppression. Moreover, patients with MPV > 11.3 fl exhibited lower SPO2, lower platelet count, higher PDW, higher larger platelet ratio and higher CRP level. The weaning failure rate was higher in patients with MPV > 11.3 fl than in those with MPV ≤ 11.3 fl (Table 5, 30/55(54.5%) vs. 24/206(11.7%), OR = 9.1, P = 0.000).
Patient outcome
The weaning failure group had higher ICU mortality [11/54(20.4%) vs. 4/207(2%); P = 0.000], higher hospital mortality [14/54(25.9%) vs. 7/207(3%); P = 0.000], and longer LOS in ICU [18(13–34) vs 10(2–18); P = 0.000] compared to successful weaning group. There was not significant difference in LOS in hospital [21(15–34) vs. 19(13–28); P = 0.085]. The 28-day survival rate was lower in weaning failure group (P = 0.000) and in MPV > 11.3 fl group(P = 0.01) by log-rank test, while Leukocyte count (P = 0.233) and CRP level (P = 0.19) did not significantly affect 28-day survival rate (Fig. 4).
Discussion
In the current study, we found that MPV > 11.3 fl with the highest AUC of ROC (AUC = 0.777;95%CI,0.722–0.826) was a more valuable marker for predicting weaning failure when compared to traditional inflammatory makers in critically ill patients, and MPV > 11.3 fl was an independent predictor for weaning failure. The odds ratio of MPV > 11.3 fl to predict weaning failure is 8.101, indicating that the risk of weaning failure of patients with MPV > 11.3 fl is much higher than patients with MPV ≤ 11.3 fl.
The underlying mechanisms of rising MPV with weaning failure in critically ill patients remain unclever. The findings may be explained by several possible reasons below. Patients with critical illness often experience more serious status and stronger inflammatory response [16]. Mechanical ventilation can trigger an inflammatory reaction in the lung and subsequent ventilation associated pneumonia or lung injury further enhanced this reaction [17, 24, 25].Moreover, weaning failure patients experienced more pulmonary inflammation response and stress [18].
Hence, the main potential mechanism for higher MPV in patients with weaning failure is severe inflammation and stress caused by unresolved inflammatory diseases and mechanical ventilation. Some studies suggested that system or local infection could increase release of thrombopoietin and different inflammatory cytokines, such as IL-1, IL3 and IL6 and tumor necrosis factor-α, result in increasing thrombopoiesis and lead to the production of younger large platelets in blood circulation [26]. However, the larger platelets function poorly competent, inducing thrombogenic activity and adverse clinical outcomes [26]. In this study, weaning failure patients had higher APACHEII score, longer IMV duration prior to weaning, longer LOS during ICU, higher leukocyte count, CRP level than those in weaning success group, suggesting that the patients of weaning failure were in more serious condition and have a robust inflammatory and stress. Besides that, severe inflammatory status could induce thrombocyte consumption in the peripheral tissue, which finally resulted in the higher MPV [27]. In our study, patients with MPV > 11.3 fl had the lower platelet count than that in patients with MPV ≤ 11.3 fl. Moreover, MPV was inversely related with platelet count among these patients, which was in line with previous study [28]. Hypoxemia may increase the consumption of platelet and promote bone marrow proliferation, which is a possible explanation for increased MPV with lower platelet count in critical patients [7]. Our result suggested that the weaning failure patients had much lower PaO2 and PaO2/FIO2, which could partially explain why MPV was higher in weaning failure group. Taken together, more severe inflammatory, stress and hypoxemia would result in a higher MPV. All of these factors could possibly lead to weaning failure [1]. According, we believe that there was an association between inflammation and stress and weaning failure, and thus MPV might be a more valuable predictor for weaning failure.
Leukocyte level was also an independent predictor of weaning failure in this study, however, by comparing the AUC between MPV and leukocyte count, we concluded that leukocyte was an inferior predictive marker of weaning failure. It is known that sepsis or severe infection could cause either leukocytosis or leukopenia [29]. Many patients presented a normal leukocyte count. Hence, the leukocyte is not likely to reflect disease severity sometimes, thus it may be less valuable to predict weaning failure.
CRP is also the most commonly used metric to investigate inflammation. Nevertheless, we found that MPV outmatched CRP in predicting weaning failure. In line with previous study, CRP was poor for predicting sepsis in children compared to MPV [30].We suggested that CRP is not superior to using MPV for predicting weaning failure.
Limitations
This study had a few limitations. First, this is a retrospective study in a single center with the relatively small sample, the results of this study ought to be generalized with caution. Second, we did not investigate the medication treatment such as anti-platelet agents and smoking status, which are known to affect MPV [31].Third, certain co-morbidities, nutritional status and anti-inflammatory would affect the inflammatory responses of blood circulation and weaning outcome, but the relevant data were absent since it is difficult to obtain all data in ICU. Fourth, due to the lack of the data, we did not evaluate the correlation of MPV with other more classic parameters related with weaning such as rapid shallow breathing index or the negative inspiratory force, so MPV should be considered together with other traditional clinical and non-clinical parameters to optimize weaning outcome. Fifth, there were a proportion of postsurgical patients who tended to wean successfully, and this possibly cause a bias in the interpretations of the results. Finally, the specific mechanisms of MPV predicting weaning failure cannot be elucidated.
Conclusions
The ability of MPV to predict weaning failure has not been studied before.
This study indicates that MPV is a preferable marker for predicting weaning failure than traditional inflammatory ones, and MPV > 11.3 fl is an independent predictor for weaning failure. We reveal that patient with MPV > 11.3 fl should be more attentively evaluated before weaning from IMV, and it would be auspicable for those patients to undergo a noninvasive ventilation or high-flow nasal cannula after extubation or even an early tracheostomy. However, further study with a larger sample size is required to confirm this preliminary study.
Availability of data and materials
The data sets supporting the results of this article are included within the article.
Abbreviations
- MPV:
-
Mean platelet volume
- IMV:
-
Invasive mechanical ventilation
- ICU:
-
Intensive care unit
- SBT:
-
Spontaneous breathing trial
- CRP:
-
C-reaction protein
- ROC:
-
Receiver-operating characteristics
- COPD:
-
Chronic obstructive pulmonary disease
- BMI:
-
Body mass index
- LOS:
-
Length of stay
- APACHE II:
-
Acute physiology and chronic health evaluation II
- RR:
-
Respiratory rate
- HR:
-
Heart rate
- SBP:
-
Systolic blood pressure
- SPO2,:
-
Peripheral oxygen saturation
- PaCO2:
-
Arterial carbon dioxide tension
- PaO2:
-
Arterial oxygen tension
- FiO2:
-
Fraction of inspired oxygen
- MPV:
-
Mean platelet volume
- PDW:
-
Platelet distribution width
- CRP:
-
C-reactive protein
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
References
Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, Pearl R, Silverman H, Stanchina M, Vieillard-Baron A, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29(5):1033–56.
Vallverdu I, Calaf N, Subirana M, Net A, Benito S, Mancebo J. Clinical characteristics, respiratory functional parameters, and outcome of a two-hour T-piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med. 1998;158(6):1855–62.
Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguia C, Nightingale P, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287(3):345–55.
Miu T, Joffe AM, Yanez ND, Khandelwal N, Dagal AH, Deem S, Treggiari MM. Predictors of reintubation in critically ill patients. Respir Care. 2014;59(2):178–85.
Vieira-de-Abreu A, Campbell RA, Weyrich AS, Zimmerman GA. Platelets: versatile effector cells in hemostasis, inflammation, and the immune continuum. Semin Immunopathol. 2012;34(1):5–30.
Korniluk A, Koper-Lenkiewicz OM, Kaminska J, Kemona H, Dymicka-Piekarska V. Mean Platelet Volume (MPV): new perspectives for an old marker in the course and prognosis of inflammatory conditions. Mediators Inflamm. 2019;2019:9213074.
Sezgi C, Taylan M, Kaya H, SelimogluSen H, Abakay O, Demir M, Abakay A, Tanrikulu AC. Alterations in platelet count and mean platelet volume as predictors of patient outcome in the respiratory intensive care unit. Clin Respir J. 2015;9(4):403–8.
Kim CH, Kim SJ, Lee MJ, Kwon YE, Kim YL, Park KS, Ryu HJ, Park JT, Han SH, Yoo TH, et al. An increase in mean platelet volume from baseline is associated with mortality in patients with severe sepsis or septic shock. PLoS ONE. 2015;10(3):e0119437.
Reangvilaikul T, Udompongpaiboon P, Vattanavanit V. Predicting acute respiratory distress syndrome in influenza pneumonia patients using delta mean platelet volume. BMC Pulm Med. 2021;21(1):405.
Wang J, Wang L, Jin L, Rong X, Tang X, Guo H, Liu X, Shi L, Tao G. Predictive value of MPV and plasma NT-ProBNP combined with the simplified geneva scale for the prognosis of acute pulmonary embolism. Evid Based Complement Alternat Med. 2021;2021:1292921.
Colakoglu SM, GencMoralar D, Cekmecelioglu BT, Hergunsel GO. Relationship of mortality with neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, and mean platelet volume in patients undergoing acute abdominal surgery. Ulus Travma Acil Cerrahi Derg. 2020;26(5):735–41.
Kim NY, Chun DH, Kim SY, Kim NK, Baik SH, Hong JH, Kim KS, Shin CS. Prognostic value of systemic inflammatory indices, NLR, PLR, and MPV, for predicting 1-year survival of patients undergoing cytoreductive surgery with HIPEC. J Clin Med. 2019;8(5):589.
Mohamed MF, Ali A, Abbas A, Awad MS, Gouda M, Sediq AM. Mean platelet volume as a predictor of pulmonary hypertension in patients with stable COPD. Int J Chron Obstruct Pulmon Dis. 2019;14:1099–108.
Pafili K, Penlioglou T, Mikhailidis DP, Papanas N. Mean platelet volume and coronary artery disease. Curr Opin Cardiol. 2019;34(4):390–8.
Karim F, Akter QS, Khanom A, Haque S, Nahar S. Mean platelet volume in Type 2 diabetes male. Mymensingh medical journal : MMJ. 2020;29(3):659–63.
Zahorec R. Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001;102(1):5–14.
Hennus MP, van Vught AJ, Brabander M, Brus F, Jansen NJ, Bont LJ. Mechanical ventilation drives inflammation in severe viral bronchiolitis. PLoS ONE. 2013;8(12):e83035.
Jubran A, Tobin MJ. Pathophysiologic basis of acute respiratory distress in patients who fail a trial of weaning from mechanical ventilation. Am J Respir Crit Care Med. 1997;155(3):906–15.
Luo Z, Zheng Y, Yang L, Liu S, Zhu J, Zhao N, Pang B, Cao Z, Ma Y. Neutrophil/lymphocyte ratio is helpful for predicting weaning failure: a prospective, observational cohort study. J Thorac Dis. 2018;10(9):5232–45.
Esteban A, Frutos F, Tobin MJ, Alia I, Solsona JF, Valverdu I, Fernandez R, de la Cal MA, Benito S, Tomas R, et al. A comparison of four methods of weaning patients from mechanical ventilation. Spanish lung failure collaborative group. N Engl J Med. 1995;332(6):345–50.
Fowler RA, Filate W, Hartleib M, Frost DW, Lazongas C, Hladunewich M. Sex and critical illness. Curr Opin Crit Care. 2009;15(5):442–9.
Bunch TJ, May HT, Bair TL, Jacobs V, Crandall BG, Cutler M, Weiss JP, Mallender C, Osborn JS, Anderson JL, et al. The impact of age on 5-year outcomes after atrial fibrillation catheter ablation. J Cardiovasc Electrophysiol. 2016;27(2):141–6.
Alsio A, Nasic S, Ljungstrom L, Jacobsson G. Impact of obesity on outcome of severe bacterial infections. PLoS ONE. 2021;16(5):e0251887.
Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126–36.
Sellares J, Loureiro H, Ferrer M, Amaro R, Farre R, Torres A. The effect of spontaneous breathing on systemic interleukin-6 during ventilator weaning. Eur Respir J. 2012;39(3):654–60.
Machlus KR, Thon JN, Italiano JE Jr. Interpreting the developmental dance of the megakaryocyte: a review of the cellular and molecular processes mediating platelet formation. Br J Haematol. 2014;165(2):227–36.
Becchi C, Al Malyan M, Fabbri LP, Marsili M, Boddi V, Boncinelli S. Mean platelet volume trend in sepsis: is it a useful parameter? Minerva Anestesiol. 2006;72(9):749–56.
Butkiewicz AM, Kemona H, Dymicka-Piekarska V, Matowicka-Karna J, Radziwon P, Lipska A. Platelet count, mean platelet volume and thrombocytopoietic indices in healthy women and men. Thromb Res. 2006;118(2):199–204.
Belok SH, Bosch NA, Klings ES, Walkey AJ. Evaluation of leukopenia during sepsis as a marker of sepsis-defining organ dysfunction. PLoS ONE. 2021;16(6):e0252206.
Dursun A, Ozsoylu S, Akyildiz BN. Neutrophil-to-lymphocyte ratio and mean platelet volume can be useful markers to predict sepsis in children. Pak J Med Sci. 2018;34(4):918–22.
Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des. 2011;17(1):47–58.
Acknowledgements
Not applicable
Funding
This study was supported by the Nation Natural Science Foundation of China (No.81570070).
Author information
Authors and Affiliations
Contributions
Yingying Zheng and Zujin Luo designed the research; Zhixin Cao conducted the research; Yingying Zheng and Zujin Luo collected and analyzed the data; all authors wrote the paper; and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of the Beijing Chao-Yang Hospital, Capital Medical University approved this study (NO.2020-KE-94). Because of retrospective study, written informed consent was waived by the ethics committee of the Beijing Chao-Yang Hospital, Capital Medical University which gave approval to the verbal consent. All patients were informed by telephone about this research and their consents were obtained, and we keep patient clinical data confidential. All procedures were in accordance with Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, Y., Luo, Z. & Cao, Z. Mean platelet volume is useful for predicting weaning failure: a retrospective, observational study. BMC Anesthesiol 22, 160 (2022). https://doi.org/10.1186/s12871-022-01701-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-022-01701-w