Abstract
Background
Malnutrition in intensive care unit (ICU) patients is associated with adverse clinical outcomes. The modified nutrition risk in the critically ill score (mNUTRIC) was proposed as an appropriate nutritional assessment tool in critically ill patients, but it has not been fully demonstrated and widely used. Our study was conducted to identify the nutritional risk in ICU patients using the mNUTRIC score and explore the relationship between 28-day mortality and high mNUTRIC scores.
Methods
This study is a secondary analysis, the data were extracted from The Beijing Acute Kidney Injury Trial (BAKIT). In total, 9049 patients were admitted consecutively, and 3107 patients with complete clinical data were included in this study. We divided the study population into high nutritional risk (mNUTRIC score ≥ 5 points) and low nutritional risk (mNUTRIC score < 5 points) groups. The predictive capacity of the mNUTRIC score was studied by receiver operating characteristic (ROC) curve analysis, appropriate cut-off was identified by highest combined sensitivity and specificity using Youden’s index. The significance level was set at 5%.
Results
Among the 3107 patients, the 28-day mortality rate was 17.4% (540 patients died). Nearly 28.2% of patients admitted to the ICU were at risk of malnutrition, high nutritional risk patients were older (P < 0.001), with higher illness severity scores than low nutritional risk patients. Multivariate analysis revealed that the mNUTRIC score was an independent risk factor for 28-day mortality and mortality increased with increasing scores (p = 0.000). The calculated area under curve (AUC) for the mNUTRIC score was 0.763 (CI 0.740–0.786). According to Youden’s index, we found a suitable cut-off > 4 for the mNUTRIC score to predict the 28-day mortality.
Conclusions
Patients admitted to the ICU were at high risk of malnutrition, and a high mNUTRIC score was associated with increased ICU length of stay and higher mortality. More large prospective studies are needed to demonstrate the validity of this score.
Trial registration
This study was registered at www.chictr.org.cn (registration number Chi CTR-ONC-11001875). Registered on 14 December 2011.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Malnutrition is common in intensive care unit (ICU) patients, it is associated with a variety of adverse outcomes, including higher complication rates, prolonged mechanical ventilation, prolonged hospitalization, and higher mortality [1, 2]. For critically ill patients, we should evaluate their nutritional status and provide adequate nutritional support [3], so effective tools are needed to assess the nutritional risk of ICU patients. However, traditional methods of nutrition assessment are limited in the hospital setting. Recently, Heyland et al. [4] published the first nutritional risk assessment tool specifically designed for critically ill patients: the NUTRIC score.
The NUTRIC score includes age, the Acute Physiology and Chronic Health Evaluation II (APACHE II) score [5], the Sequential Organ Failure Assessment (SOFA) score [6], comorbidities, days from hospitalization to ICU admission, and the interleukin-6 (IL-6) level, which was developed to link starvation, inflammation, and clinical outcomes. Patients are scored from 0 to 10, a score of 6 or greater indicates a high nutritional risk [4].
The NUTRIC score can predict 28-day mortality in a medical-surgical ICU population [4] and in postoperative surgical patients [7]. But the use of original NUTRIC score is limited by the availability of IL-6, which is not readily available in many institutions, and Heyland et al. stated that IL-6 only increased the C-index by 0.007 (from 0.776 to 0.783), with no statistical difference. Therefore, they suggested that in settings in which IL-6 is not available, it could be omitted from the NUTRIC score [4]. This adjusted score is called the modified NUTRIC score (mNUTRIC) [8]. Rahman et al. evaluated this modified NUTRIC score and found that mortality increased by 1.4% (95% CI, 1.3–1.5) for every point increase in the mNUTRIC score [8].
Some studies are available on the validity of the mNUTRIC score, however, most of them are small samples [9,10,11,12] or retrospective studies [13,14,15], and there are few prospective studies with large samples at present [8, 16, 17]. The mNUTRIC score has not been widely used in China, where has been no large sample studies. Moreover, there is a debate about the cutoff value of the mNUTRIC score [13, 14, 18]. Our main objective was to validate the mNUTRIC score in a surgical-medical ICU population in China, we also aimed to identify the cut-off point obtained in the mNUTRIC score that presented the best validity parameters for predicting mortality in this population.
Methods
Study design and data collection
This study used a database from a prospective, multi-centre, observational study that investigated the epidemiology of acute kidney injury (AKI) in critically ill patients in 30 ICUs at 28 tertiary hospitals in Beijing, China, from March 1 to August 31, 2012 (the Beijing Acute Kidney Injury Trial (BAKIT) [19] (for a complete list of these hospitals and the persons responsible for the data acquisition, see Additional file 1). Study subjects included all adult patients (age ≥ 18 years) admitted consecutively to the ICU. Only the initial ICU admission was considered in this study. The following patients were excluded: patients with preexisting end-stage chronic kidney disease, patients already receiving renal replacement therapy (RRT) before admission to the ICU, and patients who had received kidney transplantation in the previous 3 months [20]. Pre-existing comorbidities were diagnosed based on the International Classification of Diseases (ICD-10) codes. Patients were followed up until death, until hospital discharge, or for 28 days. Among the 9079 patients who were admitted consecutively, 3107 patients were included in our study (Fig. 1).
Thorough follow-up of all patients included in the study was conducted in the first 10 days after ICU admission. The collected data included demographics, anthropometrics, admission diagnosis, comorbidities, daily vital signs and laboratory data, which were used to automatically calculate the APACHE II score, the Simplified Acute Physiology Score II (SAPS II) score [21] and the SOFA score, days from hospital to ICU admission, ICU length of stay (LOS), hospital LOS, use of vasoactive drugs, and length of mechanical ventilation. RRT data were also reported.
Mortality data were collected up to 28 days after ICU discharge from hospital records, including records from hospital admissions and visits to outpatient clinics.
Outcomes
The primary outcome was 28-day mortality, and the secondary outcome was the occurrence of the AKI.
Nutritional support
Nutritional support methods were based on the guidelines for enteral and parenteral nutrition issued by the European and American Society of Enteroprotective Nutrition [22], combined with our accumulated clinical experience, individualized nutritional support was given to all patients. The patients began enteral nutrition (EN) 20–25 kcal/(kg.d) and a protein requirement of 1.2–2.0 g/(kg.d) within 24–48 h of admission to the ICU (on average). If the patient was intolerant of EN or had contraindications to EN, parenteral nutrition (PN) support was given within 24—48 h. If EN could not fully meet the nutritional needs of patients, appropriate intravenous supplementation with glucose, amino acids, or fat emulsion was given, that is, the combination of EN and PN.
Definitions
We used the modified 9-point scale of the NUTRIC score, the mNUTRIC score [8]. We defined the scores from 0 to 4 as “low scores”, which indicated a low level of risk of malnutrition, and the scores from 5 to 9 as “high scores”, which were associated with worse clinical outcomes [8]. Because the mNUTRIC score includes APACHE II score, it was calculated only once at ICU admission.
AKI severity was classified according to the KDIGO guidelines [23]. AKI occurring within 10 days is defined as AKI, and more than 10 days is defined as non-AKI.
Statistical analysis
Non-normally distributed continuous variables were expressed as the medians with interquartile ranges (IQRs) and were compared using the Mann–Whitney U test or Kruskal–Wallis analysis of variance with Bonferroni correction. Categorical variables were expressed as the number of cases and proportions and were compared using the Mantel–Haenszel Chi-square test.
A multivariate Cox regression analysis was performed using a backward stepwise selection method, with P value < 0.05 as the entry criterion, and P value ≥ 0.10 as the removal criterion. The assumption of proportional hazards was checked graphically using log (-log (survival probability)) plots and was found to be appropriate. Because the mNUTRIC score includes APACHE II and SOFA score, to avoid the duplicates, we did a collinearity analysis on the mNUTRIC score, APACHEII and SOFA, and found that there was no collinearity between them. Variables considered for multivariable analysis included age, sex, body mass index (BMI), APACHE II score, SAPS II, SOFA score, mNUTRIC score, use of vasoactive drugs, mechanical ventilation, AKI, RRT and underlying diseases. We tested for collinearity among all variables using a Cox regression analysis to generate hazard ratios (HR) and 95% confidence intervals (CIs).
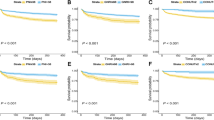
The receiver operating characteristic (ROC) curve was drawn according to the sensitivity and specificity of the mNUTRIC score in predicting the 28-day mortality risk of patients and the best cut-off value was determined by the maximum of the Youden index (i.e., sensitivity plus specificity minus one) calculated from the ROC analysis. Using Hosmer- lemeshow goodness of fit to test the calibration of the scoring system. The 28-day survival stratified by low and high mNUTRIC scores was additionally evaluated graphically using the Kaplan–Meier product limit survival plot, we used Log-rank (Mantel–Cox) test for the comparison of survival curves. To verify the predictive effect of the mNUTRIC score on 28-day mortality in different populations, subgroup analysis was performed, we divided the study population into mechanical ventilation, medical mechanical ventilation (Because surgical patients are intubated for surgery, unlike medical patients who are intubated for serious medical conditions, we separately list medical patients who require intubation), sepsis, AKI and RRT patients, respectively.
All statistical analyses were performed using SPSS software (IBM Corp., Statistics for Windows, version 22.0, Armonk, NY, USA), with a two-sided P value < 0.05 considered statistically significant.
Results
Study population
Among the 9049 patients enrolled in the BAKIT study, 5942 were excluded for the reasons shown in Fig. 1, leaving 3107 patients for analysis. The characteristics of the entire cohort are shown in Table 1. The median age was 64 (IQR: 51–77) years, and 61.5% were men. The all-cause 28-day mortality rate was 17.4% and the median ICU LOS was 4 (IQR: 2–9) days. Among the included patients, the median BMI was 24 (IQR: 21–26) kg/m2, the median APACHE II score was 14 (IQR:10–20), the median SAPSII was 34 (IQR: 26–45), the median SOFA score was 6 (IQR: 3- 8), the median mNUTRIC score was 3 (IQR: 2–5), and the median number of comorbidities was 1 (IQR: 0—2). Mechanical ventilation was used in 2021 (65.0%) patients, 1307 patients (42.1%) received vasopressors, 1584 patients developed AKI and 281 patients (9.0%) underwent RRT. A total of 876 patients (28.2%) had high mNUTRIC scores.
Characteristics of high nutritional risk patients
From Table 1, we can see high nutritional risk patients were older (P < 0.001), with higher illness severity scores than low nutritional risk patients. High nutritional risk patients were more likely to present with sepsis on ICU admission, were more likely to develop AKI, and had longer durations of ICU and hospital stays when compared to the low nutritional risk group. Furthermore, mechanical ventilation was more commonly used in high nutritional risk patients (76.1% vs 60.7%; P < 0.001). The 28-day mortality and in-hospital mortality rates were higher among high nutritional risk patients than low nutritional risk patients (P < 0.001).
28-Day mortality according to score
Our analysis showed that the 28-day mortality increased with higher mNUTRIC scores (Fig. 2), and the 28-day mortality for the maximum mNUTRIC score was 67.4%.
High mNUTRIC score and the 28-day mortality
In multivariate Cox regression analysis (Table 2), after adjusting for age, sex, BMI, sepsis, APACHE II score, SAPS II, SOFA score, mNUTRIC score, use of vasoactive drugs, mechanical ventilation, AKI, RRT and underlying diseases, the mNUTRIC score, APACHE II score, SAPS II, sepsis, mechanical ventilation, AKI and RRT were independent predictors of 28-day mortality, and the 28-day mortality increased by 8.5% for every point increase in the mNUTRIC score (p = 0.012, HR = 1.085). Kaplan–Meier analysis also showed that the presence of high mNUTRIC scores was associated with a higher risk of mortality (p < 0.001) (Fig. 3).
Area under the curve of scores for predicting 28-day mortality
We divided the study population into mechanical ventilation, medical mechanical ventilation, sepsis, AKI and RRT patients, respectively. We can see that in this cohort and each subgroup, the areas under the curve (AUCs) of the mNUTRIC score for predicting 28-day mortality indicated good predictive performance of the score (Fig. 4). In the ROC curve for the mNUTRIC score, the best cut-off value was at 4 (sensitivity 61.48% and specificity 78.81%) in this cohort, and the Youden index was 0.4029.
Discussion
This study was a secondary analysis of a prospective observational study in surgical-medical ICUs. We used a validated nutrition assessment tool in an attempt to demonstrate an association between malnutrition and 28-day mortality. We found a high incidence of malnutrition in ICU patients, and malnutrition was associated with a poor prognosis.
In the present study, 28.2% of the critically ill patients admitted to the ICU were at high nutritional risk (mNUTRIC scores ≥ 5). These findings were similar to the results of a study conducted in Turkey [7], in which 22.4% patients were evaluated as having high scores (between 5 and 9). Lew et al. [24] also demonstrated that the prevalence of malnutrition in the ICU was 28% using the 7-point Subjective Global Assessment (7-point SGA) to determine patients’ nutritional status. Recently, a study [10] reported that 45% of mechanically ventilated patients admitted to the ICU were at high nutritional risk. Similarly, Kalaiselvan et al. [25] reported that 42.5% of mechanically ventilated patients had NUTRIC scores ≥ 5. Our study is more generalizable because of the inclusion of both medical and surgical patients. The aforementioned studies included only patients on mechanical ventilation, and patients on mechanical ventilation were more seriously ill than those not on mechanical ventilation. The differences among studies are mainly the result of different populations and nutrition screening tools.
In our study, the 28-day mortality associated with the maximum mNUTRIC score was 67.7%, which is similar to the finding in the study by Jeong [13], in which this rate was 62.5%. Compared with patients with a low NUTRIC score, patients with high NUTRIC score had a higher mortality rate and longer ICU LOS, similar results were reported by other studies [4, 16].
The mortality rate in our study was 17.4%, which was lower than the rate reported in the second validation study of the NUTRIC score (29%) by Rahman et al. [8]. This difference may be because our study included many postoperative care patients. In this study, we found that the mNUTRIC score was a good prognostic predictor in critically ill patients and that high mNUTRIC scores were associated with an elevated risk of death at 28 days (HR = 1.085, 95% CI = 1.018 to 1.157, P = 0.012). This finding is consistent with those of prior studies [9, 13, 16].
The mNUTRIC score was found to have a fair predictive performance for 28-day mortality in this cohort (AUC 0.763; 95% CI 0.740—0.786) and each subgroup. These results are in line with those of the initial validation study by Heyland et al. (AUC: 0.783) [4] and a recently published validation study of the mNUTRIC score by Mukhopadhyay et al. (AUC 0.71) [26]. Recently, a study [13] showed that the AUC of the NUTRIC score for the prediction of 28-day mortality was 0.762 (95% CI: 0.718–0.806), while that of the mNUTRIC score was 0.757 (95% CI: 0.713–0.801). There was no significant difference between the two scores (p = 0.45). The mNUTRIC score is a good nutritional risk assessment tool for critically ill patients.
We found that the best cut-off value for the mNUTRIC score was > 4 (sensitivity 61.48% and specificity 78.81%) in this cohort, and the Youden index was 0.4029, which is consistent with previous work by de Vries et al. [14]. However, in another study, the best cut-off value was at 6 (sensitivity 75% and specificity 65%), and the Youden index was 0.401[13]. Jung et al. reported that patients were considered to be at high risk of malnutrition when their mNUTRIC score was ≥ 5[27]. Our study included patients with various diseases, while Jung’s study population was limited to patients with sepsis. Further investigation is needed to find the best cut-off value of the mNUTRIC score to define the high-risk group.
The limitations of our study stem mainly from the fact that it is a secondary analysis of an original database that lacked data on inflammation indicators such as IL-6. Therefore, we could not calculate the NUTRIC score to verify the difference between the NUTRIC and mNUTRIC score. Second, nutrition history and feeding parameters were not available in our cohort, so the associations among nutritional adequacy, mNUTRIC score and mortality could not be confirmed by our results. Third, we did not perform dynamic nutritional risk assessments, which may provide more information for patient outcomes.
Conclusion
Patients were considered to be at high risk of malnutrition when their mNUTRIC score was > 4. The mNUTRIC score is a practical, easy-to-use tool based on variables that are easy to obtain in the critical care setting.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request. Corresponding author: Xiuming Xi, email: xixiuming2937@sina.com.
Abbreviations
- ICU:
-
Intensive care unit
- NUTRIC:
-
the nutrition risk in the critically ill score
- IL-6:
-
Interleukin-6
- mNUTRIC:
-
The modified nutrition risk in the critically ill score
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under curve
- AKI:
-
Acute kidney injury
- BAKIT:
-
The Beijing Acute Kidney Injury Trial
- BMI:
-
Body mass index
- RRT:
-
Renal replacement therapy
- APACHE II:
-
Acute physiology and chronic health evaluation II
- SAPS II:
-
The simplified acute physiology score II
- SOFA:
-
Sequential organ failure assessment
- LOS:
-
Length of stay
- EN:
-
Enteral nutrition
- PN:
-
Parenteral nutrition
- IQR:
-
Interquartile range
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
References
Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22(3):235–9.
Heyland DK, Cahill N, Day AG. Optimal amount of calories for critically ill patients: depends on how you slice the cake! Crit Care Med. 2011;39(12):2619–26.
Al-Dorzi HM, Albarrak A, Ferwana M, et al. Lower versus higher dose of enteral caloric intake in adult critically ill patients: a systematic review and meta-analysis. Crit Care. 2016;20(1):358.
Heyland DK, Dhaliwal R, Jiang X, et al. Identifying critically ill patients who benefit the most from nutrition therapy: the development and initial validation of a novel risk assessment tool. Crit Care. 2011;15(6):R268.
Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Vincent JL, de Mendonca A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a multicenter, prospective study. Crit Care Med. 1998;26(11):1793–800.
Ozbilgin S, Hanci V, Omur D, et al.Morbidity and mortality predictivity of nutritional assessment tools in the postoperative care unit. Medicine (Baltimore) 2016;95(40):e5038.
Rahman A, Hasan RM, Agarwala R, et al. Identifying critically-ill patients who will benefit most from nutritional therapy: Further validation of the “modified NUTRIC” nutritional risk assessment tool. Clin Nutr. 2016;35(1):158–62.
Oliveira ML, Heyland DK, Silva FM, et al. Complementarity of modified NUTRIC score with or without C-reactive protein and subjective global assessment in predicting mortality in critically ill patients. Rev Bras Ter Intensiva. 2019;31(4):490–6.
Ata Ur-Rehman HM, Ishtiaq W, Yousaf M, et al. Modified Nutrition Risk in Critically Ill (mNUTRIC) score to assess nutritional risk in mechanically ventilated patients: a prospective observational study from the Pakistani population. Cureus. 2018;10(12):e3786.
Zhang P, Bian Y, Tang Z, et al. Use of Nutrition Risk in Critically Ill (NUTRIC) Scoring System for Nutrition Risk Assessment and Prognosis Prediction in Critically Ill Neurological Patients: A Prospective Observational Study. JPEN J Parenter Enteral Nutr. 2021;45:1032–41.
Brascher JMM, Peres WAF, Padilha PC. Use of the modified “Nutrition Risk in the critically ill” score and its association with the death of critically ill patients. Clin Nutr ESPEN. 2020;35:162–6.
Jeong DH, Hong SB, Lim CM,et al. Comparison of accuracy of NUTRIC and modified NUTRIC scores in predicting 28-day mortality in patients with sepsis: a single center retrospective study. Nutrients. 2018;10(7):911.
de Vries MC, Koekkoek WK, Opdam MH, et al. Nutritional assessment of critically ill patients: validation of the modified NUTRIC score. Eur J Clin Nutr. 2018;72:428–35.
Son DH, Kim KS, Lee HS, et al. Derivation and validation of a new nutritional index for predicting 90 days mortality after ICU admission in a Korean population. J Formos Med Assoc. 2020;119(8):1283–91.
Mendes R, Policarpo S, Fortuna P, Alves M, Virella D, Heyland DK. Portuguese NUTRIC Study Group. Nutritional risk assessment and cultural validation of the modified NUTRIC score in critically ill patients – A multicenter prospective cohort study. J Crit Care. 2017;37:249.
Kumar S, Gattani SC, Baheti AH, et al. Comparison of the Performance of APACHE II, SOFA, and mNUTRIC Scoring Systems in Critically Ill Patients: A 2-year Cross-sectional Study. Indian J Crit Care Med. 2020;24(11):1057–61.
Mayr U, Pfau J, Lukas M, et al. NUTRIC and Modified NUTRIC are Accurate Predictors of Outcome in End-Stage Liver Disease: A Validation in Critically Ill Patients with Liver Cirrhosis. Nutrients. 2020;12(7):2134.
Luo X, Jiang L, Du B, Wen Y, et al. A comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care. 2014;18(4):R144.
Piccinni P, Cruz DN, Gramaticopolo S, et al. Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiol. 2011;77(11):1072–83.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–63.
McClave SA, Martindale RG, Vanek VW, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2009; 33(3):277–316.
KDIGO AKI Work Group.KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;17:1–138.
Lew CCH, Wong GJY, Cheung KP,et al. Association between malnutrition and 28-day mortality and intensive care length-of-stay in the critically ill: a prospective cohort study. Nutrients. 2017;10(1):10.
Kalaiselvan M, Renuka M, Arunkumar A. Use of nutrition risk in critically ill (nutric) score to assess nutritional risk in mechanically ventilated patients: A prospective observational study. Indian J Crit Care Med. 2017;21(5):253–6.
Mukhopadhyay A, Henry J, Ong V, et al. Association of modified NUTRIC score with 28-day mortality in critically ill patients. Clin Nutr. 2017;36(4):1143–8.
Jung YT, Park JY, Jeon J, et al. Association of Inadequate Caloric Supplementation with 30-Day Mortality in Critically Ill Postoperative Patients with High Modified NUTRIC Score. Nutrients. 2018;10:1589.
Acknowledgements
The authors thank all members of the Beijing Acute Kidney Injury Trial (BAKIT) work group (see Additional file 1) for participating in database management.
Funding
The study was supported by a grant from the Beijing Municipal Science & Technology Commission, a government fund used to improve health-care quality (No. D101100050010058). It offered financial support for data collection.
Author information
Authors and Affiliations
Contributions
NW and MPW designed and carried out the study, NW performed the statistical analysis, and drafted the manuscript. LJ and BD were involved in design and in acquisition of data and helped to revise the manuscript critically for important content. BZ was involved in the design and the statistical analysis. The Beijing Acute Kidney Injury Trial (BAKIT) Workgroup participated in acquisition and interpretation of data. XX conceived of the study, participated in its design, and helped to revise manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Boards of the Ethics Committees of the lead study centre (Fu Xing Hospital, Capital Medical University, China) and all other participating hospitals (Additional file 2). We confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Being an observational study, written informed consent from participants to partake into the study was not necessary. Hence, we obtained an informed consent waiver from the above ethical committees.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, N., Wang, MP., Jiang, L. et al. Association between the modified Nutrition Risk in Critically Ill (mNUTRIC) score and clinical outcomes in the intensive care unit: a secondary analysis of a large prospective observational study. BMC Anesthesiol 21, 220 (2021). https://doi.org/10.1186/s12871-021-01439-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-021-01439-x