Abstract
Background
Difficult tracheal intubation is a common problem encountered by anesthesiologists in the clinic. This study was conducted to assess the difficulty of tracheal intubation in infants with Pierre Robin syndrome (PRS) by incorporating computed tomography (CT) to guide airway management for anesthesia.
Methods
In this retrospective study, we analyzed case-level clinical data and CT images of 96 infants with PRS. First, a clinically experienced physician labeled CT images, after which the color space conversion, binarization, contour acquisition, and area calculation processing were performed on the annotated files. Finally, the correlation coefficient between the seven clinical factors and tracheal intubation difficulty, as well as the differences in each risk factor under tracheal intubation difficulty were calculated.
Results
The absolute value of the correlation coefficient between the throat area and tracheal intubation difficulty was 0.54; the observed difference was statistically significant. Body surface area, weight, and gender also showed significant difference under tracheal intubation difficulty.
Conclusions
There is a significant correlation between throat area and tracheal intubation difficulty in infants with PRS. Body surface area, weight and gender may have an impact on tracheal intubation difficulty in infants with PRS.
Similar content being viewed by others
Background
Difficult tracheal intubation is common in clinical practice, and it mostly refers to tracheal intubation that cannot be successfully completed by an ordinary indirect laryngoscope [1]. It represents the most difficult problem encountered by anesthesiologists in their daily work and is mainly caused by anatomical deformities, restricted back tilting activities, obesity and limited mouth opening [2]. These factors have an adverse effect on treatment. In practice, the level of difficulty is evaluated before the formal implementation of tracheal intubation. For patients with different levels of difficulty, preparations should be done in advance to avoid local mucosal damage caused by multiple intubation or complications such as dislocation of the circular cartilage [3].
In 2016, Münster et al [4] have reported that the position of vocal cords is related to laryngeal exposure and that difficult laryngoscopy is more likely to occur when vocal cords are closer to the head. From 2016 to 2018, many studies have utilized ultrasound for the clinical diagnosis of difficult tracheal intubation [5,6,7,8,9,10] Ultrasound provides not only real-time images but also reveals dynamic structural changes of the airway. In 2019, Lee et al [11] found that the distance from the mandibular groove to the hyoid bone and the distance from the inner edge of the mandible to the hyoid bone on X-ray images of the lateral neck were important for predicting difficult tracheal intubation in patients with acromegaly. However, there are only a few available methods for infant airway assessment and their accuracy is relatively poor [12].
Pierre Robin syndrome [13, 14] is the triad of micrognathia, glossoptosis, and cleft palate. These conditions could easily lead to difficult tracheal intubation which is the most significant risk factor for intubation anesthesia. Accurate preoperative prediction of intubation difficulty and adequate preparations are essential for ensuring successful airway management in infants with PRS. There are many methods for assessing the difficulty of tracheal intubation [3]; yet, no existing method is suitable for infants, especially infants with PRS. Moreover, few reports have focused on the application of CT on tracheal intubation difficulty assessment in infants with PRS [15, 16]. Therefore, this study was conducted to assess the difficulty of tracheal intubation in infants with PRS by incorporating CT to guide airway management for anesthesia [17].
Methods
Dataset
This retrospective study was approved by the Institutional Ethics Committee of Children’s Hospital of Nanjing Medical University and was conducted using the data obtained from Picture Archiving and Communication System (PACS) database and Operation Anesthesia Information System (OAIS) database. Informed patient consent was waived by our IEC. Clinical information and CT images were collected from infants with PRS who underwent intubation anesthesia in 2018 at Children’s Hospital of Nanjing Medical University.
Seven clinical risk factors [18] that may have an impact on tracheal intubation difficulty were provided by experienced clinicians, including gender, height, weight, body surface area (BSA), throat area, age, and pneumonia (Table 1). The calculation of the throat area was elaborated below, and the remaining indicators could be directly obtained or simply calculated. Tracheal intubation difficulty is divided into three levels based on whether glottis can be completely observed under visual laryngoscope, where level I refers to complete observation, level II refers to partial observation, and level III refers to the case when the only epiglottis can be observed.
Labeling criteria
To assess the impact of the throat area on tracheal intubation difficulty, the collected CT images (Fig. 1a) were labeled according to the irregularity of the area being labeled using Labelme, an annotation tool which is based on the Python language and allows for irregular area annotation [19]. A radiologist with 20 years of clinical experience, who was blinded to the infants’ difficulty level, was responsible for labeling. Through a three-dimensional reconstruction technique, the median sagittal image of the upper airway of the infants was obtained, after which then the area of the oropharyngeal cavity (ie, the pharyngeal area between the plane of the tongue and the glottis) was labeled.
Annotation file processing and area calculation
The overall workflow is shown in Fig. 2. The annotation file generated by Labelme is in the format of .json (Fig. 1b) [20]. To calculate the throat area, the annotation file was first converted to a single-channel image in .png format (Fig. 1c).
OpenCV performed subsequent processing in the Python environment. First, the single-channel image that was obtained during the previous step underwent color space conversion using the cvtColor function of OpenCV and was converted into a grayscale image (Fig. 1d) [21, 22]. The grayscale image was then thresholded (the threshold was set to 1) using the threshold function and becoming a binary image (Fig. 1e) [22, 23]. The throat contour information of the marker was then obtained by the findContours function, with pixel position difference between two adjacent points in all contour points no larger than 1 [22, 24]. Finally, the contour information obtained in the previous step in the form of a point set was input into the contourArea function of OpenCV to calculate the area [22, 25].
Correlation analysis
Correlation coefficients were used to assess the impact of each risk factor on tracheal intubation difficulty. Clinical risk factors highly correlated with difficulty level had better predicative effects in the clinic.
Statistical analysis
Since clinical risk factors include numerical and categorical variables and tracheal intubation difficulty is categorical, the correlation was measured by the Spearman rank correlation coefficient. Besides, to analyze whether there is a significant difference in each clinical risk factor under tracheal intubation difficulty, the Kruskal-Wallis test was used for numerical factors, and Pearson’s Chi-squared test was used for categorical factors.
Results
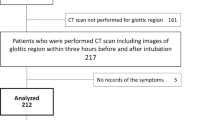
The flow chart of the study is shown in Fig. 2. Eight infants were excluded due to censored data (4 cases of censored pneumonia data and 4 cases of censored throat area data). Finally, 96 infants were included in the study, among whom 29 were level I difficulty, 43 were level II difficulty, and 24 were level III difficulty of tracheal intubation. Additional data with sufficient clinical information were collected.
The correlation coefficients are integrated in Fig. 3, where darker color indicates stronger correlations, while the lighter color represents weaker correlations. The correlation was strongest between the throat area and tracheal intubation difficulty with the correlation coefficient of − 0.54. Risk factors that were moderately correlated with tracheal intubation difficulty were BSA, weight, and gender with correlation coefficients of − 0.29, − 0.29 and 0.26, respectively. All numerical risk factors were negatively correlated with tracheal intubation difficulty. Among categorical risk factors, males were more difficult to intubate than females, and infants with pneumonia had a lower level of difficulty in intubation than infants without pneumonia.
The results of the internal difference analysis of risk factors are shown in Table 2. The difference in throat area under tracheal intubation difficulty was significant, with P < 0.0001 (Level I vs. II: P = 0.0022, Level II vs. III: P = 0.0002, Level I vs.III: P < 0.0001). The differences in BSA, weight, and gender under tracheal intubation difficulty were also significant, and their corresponding P values were 0.0117, 0.0117 and 0.0043, respectively. BSA, weight, and gender were significantly different when comparing level II to level III and level I to level III. Height, age, and pneumonia showed no significant difference under tracheal intubation difficulty.
Discussion
In this study, we used clinical data from 96 PRS infants who underwent intubation anesthesia to perform correlation analysis, which demonstrated that the throat area had a significant effect on tracheal intubation difficulty. Our results revealed that a larger throat area was associated with a lower level of tracheal intubation difficulty, which is consistent with the clinician’s subjective perception. Besides, we found that high BSA and weight corresponded to low tracheal intubation difficulty, which may be related to the better physical development of these infants. Moreover, male infants had a higher tracheal intubation difficulty than females. Pneumonia, age, and height were slightly correlated with the difficulty of tracheal intubation, which may be due to the small amount of collected data and thus needs to be further analyzed.
After further P-value analysis, we found that four factors, namely throat area, gender, weight, and BSA, were internally different under the difficulty of tracheal intubation. Among them, the difference in the throat area was significant between all levels of tracheal intubation difficulty. Gender, weight, and BSA were only significantly different between level II and level III, level I, and level III. We speculate that it may be because the sample size of the level I tracheal intubation difficulty is too small. In addition height, age, and pneumonia under tracheal intubation difficulty were not statistically significant, which may be related to the small sample size.
Attention should be paid to some of the limitations of our research. First, we studied the correlation between risk factors and tracheal intubation difficulty without building a predictive model, because the limited number of cases obtained in this study could not meet the requirements for modelling. Second, in order to facilitate the drawing of the correlation coefficient map, the correlation measure was based on the Spearman rank correlation coefficient. In addition, this was a single-center study. Finally, the annotation of the region of interest in the throat was done by one experienced doctor, which may be subjectively biased.
This study has few limitations: first, future studies should expand the number of cases collected and construct a predictive model of intubation difficulty. Secondly, the regional annotation should be performed by multiple physicians, and artificial intelligence annotation tools should be constructed. Finally, the integration of labeling and difficulty prediction should be performed.
Conclusion
The throat area may be helpful for predicting the difficulty of tracheal intubation in infants with PRS. Besides, gender, weight and BSA may also affect the prediction of the difficulty of airway intubation to some extent.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PRS:
-
Pierre Robin Syndrome
- CT:
-
Computed Tomography
- BSA:
-
Body Surface Area
References
Xu Z, Ma W, Hester DL, et al. Anticipated and unanticipated difficult airway management. Curr Opin Anaesthesiol. 2018;31(1):96–103.
Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the fourth National Audit Project of the Royal College of Anaesthetists and the difficult airway society. Part 1: anaesthesia. Br J Anaesth. 2011;106(5):617–31.
Rosenblatt WH. Preoperative planning of airway management in critical carepatients. Crit Care Med. 2004;32(4):186–92.
Münster T, Hoffmann M, Schlaffer S, et al. Anatomical location of the vocal cords in relation to cervical vertebrae. Eur J Anaesthesiol. 2016;33(4):257–62.
Guttman J, Nelson BP. Diagnostic emergency ultrasound: assessment techniques inthe pediatric patient. Pediatr Emerg Med Pract. 2016;13(1):1–27.
Erer OF, Erol S, Anar C, et al. Contribution of cell block obtained by endobronchial ultrasound-guided transbronchial needle aspiration in the diagnosis of malignant diseases and sarcoidosis. Endosc Ultrasound. 2017;6(4):265–8.
Leversedge FJ, Cotterell IH, Nickel B, et al. Ultrasonography guided de Quervain injection: accuracy and anatomic considerations in a cadaver model. J Am Acad Orthop Surg. 2016;24(6):399–404.
Li Y, Wang W, Yang T, et al. Incorporating uterine artery embolization in the treatment of cesarean scar pregnancy following diagnostic ultrasonography. Int J Gynaecol Obstet. 2016;134(2):202–7.
Osman A, Sum KM. Role of upper airway ultrasound in airway management. J Intensive Care. 2016;4(1):52.
Falcetta S, Cavallo S, Gabbanelli V, Pelaia P, Sorbello M, Zdravkovic I, Donati A. (2018). Evaluation of two neck ultrasound measurements as predictors of difficult direct laryngoscopy: a prospective study. Eur J Anaesthesiol. 2018;35:605–12.
Lee HC, Kim MK, Kim YH, et al. Radiographic predictors of difficult laryngoscopy in acromegaly patients. J Neurosurg Anesthesiol. 2019;31(1):50–6.
Karišik M, Janjević D, Sorbello M. Fiberoptic bronchoscopy versus video laryngoscopy in pediatric airway management. Acta Clinica Croatica. 2016;55:51–4.
Benko S, Fantes JA, Amiel J, et al. Highly conserved non-coding elements on either side of SOX9 associated with Pierre Robin sequence. Nat Genet. 2009;41(3):359–64.
Evans KN, Sie KC, Hopper RA, et al. Robin sequence: from diagnosis to development of an effective management plan. Pediatrics. 2011;127(5):936–48.
Plaza AM, Valadés RF, López AE, et al. Changes in airway dimensions after mandibular distraction in patients with Pierre-Robin sequence associated with malformation syndromes. Revista Española De Cirugía Oral Y Maxilofacial. 2015;37(2):71–9.
Frova G, Guarino A, Petrini F, et al. Recommendations for airway control and difficult airway management in paediatric patients. Minerva Anestesiol. 2006;72(9):723–48.
Ondik MP, Kimatian S, et al. Management of the difficult airway in the pediatric patient. J Pediatr Intensive Care. 2007;18(2):121–6.
Loftus PA, Ow TJ, Siegel B, et al. Risk factors for perioperative airway difficulty and evaluation of intubation approaches among patients with benign goiter. Ann Otol Rhinol Laryngol. 2014;123(4):279–85.
Xue FS, Yuan YJ, Wang Q, et al. Difficulties and possible solutions for tracheal intubation with the airway scope. Am J Emerg Med. 2011;29(1):123–4.
Hong L, Jin Q, Li X, et al. Image and medical annotations using non-homogeneous 2D ruler learning models. Comput Electrical Eng. 2016;50:102–10.
Domínguez C, Heras J, Pascual V. IJ-OpenCV: combining ImageJ and OpenCV for processing images in biomedicine. Comput Biol Med. 2017;84:189–94.
Culjak I, Abram D, Pribanic T, et al. A brief introduction to OpenCV [C]// MIPRO, 2012 proceedings of the 35th international convention. IEEE, 2012.
Chernov V, Alander J, Bochko V. Integer-based accurate conversion between RGB and HSV color spaces. Comput Electrical Eng. 2015;46:328–37.
Shin JW. High-accuracy skin lesion segmentation and size determination. Dissertations & Theses - Gradworks, 2011.
Raymond WH, Garder A. A spatial filter for use in finite area calculations. Mon Weather Rev. 2009;116(1):209–22.
Acknowledgements
Not applicable.
Funding
The study was funded by departmental resources.
Author information
Authors and Affiliations
Contributions
YlL is the main contributor in writing the manuscript. SZ is responsible for the collection and annotation of CT images. JSW processes the image and calculates the area, and performs statistical analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was approved by the Institutional Ethics Committee of Children’s Hospital of Nanjing Medical University and was conducted using the data obtained from Picture Archiving and Communication System (PACS) database and Operation Anesthesia Information System (OAIS) database. Informed consent was waived by our IEC based on minimal harm to the patient.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., Wang, J. & Zhong, S. Correlation between clinical risk factors and tracheal intubation difficulty in infants with Pierre-Robin syndrome: a retrospective study. BMC Anesthesiol 20, 82 (2020). https://doi.org/10.1186/s12871-020-00997-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-020-00997-w