Abstract
Background
Head injury is one of the top three diagnosis leading to intensive care unit (ICU) admission in Malaysia. There has been growing interest in using immunonutrition as a mode of modulating the inflammatory response to injury or infection with the aim of improving clinical outcome. The aim of the present study was to evaluate the effect of an immunonutrition on biomarkers (IL-6, glutathione, CRP, total protein and albumin) in traumatic brain injury patients.
Methods
Thirty six patients with head injury admitted to neurosurgical ICU in University Malaya Medical Centre were recruited for this study, over a 6-month period from July 2014 to January 2015. Patients were randomized to receive either an immunonutrition (Group A) or a standard (Group B) enteral feed. Levels of biomarkers were measured at day 1, 5 and 7 of enteral feeding.
Results
Patients in Group A showed significant reduction of IL-6 at day 5 (p < 0.001) with concurrent rise in glutathione levels (p = 0.049). Patients in Group A also demonstrated a significant increase of total protein level at the end of the study (day 7).
Conclusion
These findings indicate the potential of immunonutrition reducing cytokines and increasing antioxidant indices in patients with TBI. However, further studies incorporating patient outcomes are needed to determine its overall clinical benefits.
Trial registration
National Medical Research Register (NMRR) ID: 14–1430-23,171. ClinicalTrials.gov identifier: NCT03166449.
Similar content being viewed by others
Background
In 2014, injury ranked fifth as the most common cause of hospitalisation in Malaysia, with 86% of major trauma patients sustaining injuries to head and neck [1, 2]. It is known that injuries to the brain is among the most likely to result in death and disability [3]. Therefore, it was unsurprising when the Malaysian Registry of Intensive Care reported head injury as one of the top three diagnosis leading to intensive care unit (ICU) admissions with an in-hospital mortality rate of 22.1% [4]. In addition to causing a significant problem in Malaysia, injury related mortality and morbidity also affects countries worldwide and is expected to be a major cause of death and disability by the year 2030 [5].
Patients with traumatic brain injury (TBI) often develop a hypermetabolic state whereby there is an increase in energy expenditure [6,7,8]. Consequently, this led to clinicians acknowledging nutritional support as an essential component in managing critically ill patients [9]. A recent meta-analysis showed that early nutrition in patients sustaining TBI was associated with a significant reduction in mortality rate, lower risk of infectious complications and lower risk of poor outcome [10].
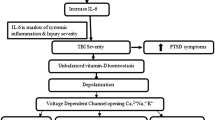
Due to its dynamic pathophysiology, the damage in TBI does not stop following the primary insult. A combination of systemic derangements (hypoxia, hypotension or hypercarbia) and local events (inflammation, oxidative stress and ion imbalance) often lead to secondary brain injury [11]. There has been growing interest in using immunonutrition as a mode of modulating the inflammatory response to injury or infection with the aim of improving clinical outcome [12, 13]. Immune-enhancing or immune-modulation enteral formula has been shown to significantly reduce infection rate in TBI patients [10, 14,15,16]. In fact, a systemic review involving critically ill patients showed that the use of immune-modulating diets supplemented with fish oil improved the outcome of medical ICU patients (with SIRS/sepsis/ARDS) [17]. Omega-3 fatty acids namely docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) found in fish oil are thought to play an important role in the repair and resolution of inflammation [18]. These two fatty acids also boost immune response by improving lymphocyte function [19]. Interestingly, research on DHA and EPA using animal model have shown favourable outcome in its neuro-restorative capacities in TBI [20].
This study aims to evaluate the effect of a specific immunonutrition, Neomune, on biomarkers (cytokines, acute phase serum proteins and antioxidants) in traumatic brain injury patients. This immune enhancing enteral feed contains arginine, glutamine and omega-3 fatty acid.
Methods
This study and its protocol was approved by the Medical Ethics Committee University Malaya Medical Center (MEC ID NO: 20,143–15). Written informed consent was obtained from patient’s next of kin.
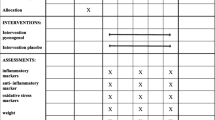
A prospective randomized controlled trial in patients with head injury comparing two high energy protein entera formula; Neomune (manufactured by Thai Otsuka Pharmaceutical Co., Ltd., Thailand) and Fresubin® HP (manufactured by Fresenius Kabi, Bod Hamburg, Germany) was conducted. Fresubin® HP energy is the standard enteral feeding used in neurosurgical ICU patients in University Malaya Medical Centre. Neomune was chosen to study its immune-modulating effects.
Patients receiving Neomune were classified as Group A (n = 18), whereas those receiving Fresubin® HP energy as Group B (n = 18). Neomune is enriched with arginine, glutamine and omega-3 fatty acid. The composition of these two formulas are described in Table 1.
Subject recruitment criteria
Thirty six patients with head injury admitted to neurosurgical ICU, University Malaya Medical Centre were recruited for this study, over a 6-month period from July 2014 to January 2015. Patient’s inclusion criteria were a) age between 15 and 78 years old, b) admission within 48 h of post traumatic event, c) moderate to severe head injury (Glasgow Coma Scale 3–12) and, d) requiring enteral nutrition. Exclusion criteria were a) history of uncontrolled diabetes mellitus, b) history of renal or liver dysfunction, c) severe sepsis with multi organ failure and d) history of significant abdominal or chest injuries requiring major surgery.
Feeding protocol
Eligible patients were randomized into receiving either Neomune (Group A) or Fresubin® HP energy (Group B) using a computerized random number generator. Fresubin® HP energy is a premixed formula with an energy of 1.5 kcal/ml. Neomune formula comes in powder form and thus was prepared to reach a concentration of 1.5 kcal/ml in order to make it comparable for the trial.
Enteral feeding was delivered within 24 to 48 h after admission or surgery according to Brain Trauma Foundation (BTF) Guidelines [21]. All feeding were introduced via nasogastric tube and carried out using infusion pump. Enteral feeding was commenced at an initial rate of 20 ml/h, and increased by 20 ml/h every 6 h until target calorie was reached, provided that there was no significant gastric residual volume (<300 mL). The target calorie for each patient was determined by the clinician working alongside the dietitian using Harris Benedict equation which measures Resting Energy Expenditure (REE). This was further corrected 140% of REE based on studies done on traumatic brain injured patients [22, 23] and nutrition guidelines published by the BTF, the American Association of Neurological Surgeons, and the Joint Section on Neurotrauma and Critical Care [21]. Patients going for scheduled surgery are kept nil by mouth 6 h prior surgery. Feeding interruption are also kept to a minimal if patients are undergoing procedures, extubation or imaging.
Data collection
Venous blood was withdrawn from patients at day 1, 5 and 7 of enteral nutrition to measure the levels of interleukin-6 (IL-6), glutathione, C-reactive protein (CRP), total protein and albumin. The concentration of IL-6 and glutathione were determined by ELISA (R&D Systems, Minneapolis, USA) according to manufacturer’s protocol. Prealbumin was not included as a nutritional biomarker in this study because this test is not available in our standard laboratory test. Furthermore, we were also limited by resource constraint. All measured outcomes were compared between Group A and Group B.
Sample size analysis
The sample size for this study was calculated based on a similar study done previously on immune enhancing nutrition in traumatic brain injury by Painter et al. [24]. The following formula was applied:
where n is the required sample size. The symbol σ represents the standard deviation of the outcome variable. Painter et al., found that the mortality rate for patients receiving immune enhancing nutrition formula in TBI was 7.5% (0.075) and thus, this value was used as σ in the above calculation [24]. ∆ symbolizes the effect size, Zα/2 represents the desired level of statistical significance whereas Zβ represents the desired power. In this study, we determined our effect size as 0.05 as the standard value for detectable difference, confidence interval as 95% (Zα/2 = 1.96) and power of 80% (Zβ = 0.84). The final sample size obtained was 35.28. A total number of 36 patients were used in this study.
Statistical analysis
The data were analysed using SPSS (Statistical Package for the Social Sciences) software version 20.0. Paired t-test was used to compare the concentration of cytokines, acute phase serum proteins and antioxidants between day 1, 5 and 7 after the administration of enteral feeding. Independent sample t-test was used to compare continuous data which include cytokines, acute phase serum proteins and antioxidant levels between Group A and Group B. Statistical significance was predetermined at p < 0.05.
Results
Demographic and clinical characteristics
Demographic and clinical characteristics were obtained from all 36 patients as displayed in Table 2. Mean age in Group A and Group B was 42 ± 70 (range: 15–75) and 32 ± 50 (range: 15–56) years old respectively, with male predominating in both groups. The main cause of brain injury in this study were a consequence of motor-vehicle accident, with more than half of patients in each group being admitted with severe Glasgow Coma scale (GCS) score (<8). There were no significant differences between Group A and Group B with respect to demographic data, GCS scoring, diagnosis and clinical interventions.
Effects of immunonutrition on cytokines, acute phase serum proteins and antioxidants indices
Observation in group A from day 1 to 7 showed a downward trend of IL-6 concentration (Table 3). This reduction was significant at day 5 and 7 (Table 4). On the other hand, glutathione and total protein concentration increased from day 1 to 7 which reached significance at day 5 and 7 respectively (Tables 3 and 4). Although there were changes in cytokines, acute phase serum proteins and antioxidants indices in Group B throughout the study, its trend were not consistent and none of the changes were significant.
Comparison between both groups revealed significantly lower IL-6 levels at day 7 of receiving enteral feeding in Group A (Table 3). Additionally, glutathione levels in group A at day 5 and 7 were significantly higher compared to Group B (Table 3).
Discussion
Protein requirements in trauma patients are proportionately higher and thus are not met by provision of routine enteral formula [25]. The appropriate and safe level in the critically ill or hypermetabolic patient in which a pro-inflammatory state exists is much more difficult to determine. Therefore, the enteral formulas used in this study are both of high protein content to meet the BTF recommendation of providing a formula containing at least 15% of calories as protein [21].
This study showed that patients receiving Neomune, an immunonutrition, had significant reduction in their IL-6 levels compared to patients in Group B. Similar observations were reported when immunonutrition was administered to patients with TBI, patients undergoing major hepatobiliary resection and patients with gastrointestinal cancer [16, 26, 27]. Following TBI, IL-6, a key regulator of the inflammatory response, rises in brain tissue [28], cerebrospinal fluid and serum [29]. This cytokine plays a dual opposing role as it is associated with both pro and anti-inflammatory effects [30]. Previous research on TBI serum IL-6 have shown contradicting findings. Kalabalikis et al. reported that there was no association between IL-6 levels with neurological outcome [31]. Whereas, others have demonstrated that high IL-6 level is correlated with poor outcome [32, 33]. For this reason, some authors have suggested reducing inflammatory mediators as a therapeutic strategy for TBI [34, 35]. An animal study showed that the presence of IL-6 may be beneficial during early stages of TBI and therefore, suggested that a timely, targeted approach is recommended in improving outcomes following TBI [36]. Another study involving animals with mild TBI showed that the neutralization of IL-6 resulted in restoration of normal motor coordination and it also mitigates the adverse effects of hypoxia which include exacerbated brain inflammation and injury [37]. Although subject to further studies, we postulate that the outcome from the use of immunomodulation in TBI can be extrapolated to humans and this concept can be exploited using immunonutrition to lower IL-6 levels in order to prevent secondary brain injuries.
This present study also demonstrated a significant increase of glutathione levels in patients receiving Neomune. Since glutamine is an important substrate for glutathione, depletions in glutamine will be reflected by glutathione reduction [38, 39]. In patients experiencing physiological stress, the synthesis of glutamine, a non-essential amino acid is unable to cater to the increased glutamine requirement [40]. Furthermore, patients with brain injury have been observed to experience profound hypoglutaminemia [41,42,43,44]. Glutathione has important function as anti-oxidant as it is a scavenger for reactive oxygen species [17]. During the acute ischemic phase of TBI, a hypermetabolic state leads to hyperglycaemia and intracellular lactate production which is associated with the development of reactive oxygen species [45,46,47,48]. Thus, tissues depleted of glutathione may undergo oxidative stress leading to complications such as predisposing patients to bacterial translocation and recurrent sepsis [49, 50]. Glutamine supplementation has been associated with lower mortality rates, shorter hospital stay and decreased occurrence of pneumonia and stress ulcer [51].
Patients receiving Neomune demonstrated a significant increase of total protein level at the end of the study whereas no significant change was seen in albumin level throughout the study. Although serum protein and albumin were previously suggested as biomarkers for malnutrition [52], serum albumin is not well correlated to protein mass [53] and does not always significantly increase following nutritional programmes [54]. Whilst albumin and protein level may be useful in the assessment of malnutrition [53], these biomarkers are not helpful at monitoring potential therapeutic effects of nutrition [55].
Immunonutrition came into existence as part of an immune-modulating strategy to improve patient outcome in the critically ill. Many clinical trials, meta-analyses and systemic reviews have been done on the use of immunonutrition in diversed population with inconsistent outcomes [56]. One review on the use of immunonutrition showed that it may reduce infectious complications in trauma and perioperative patients [57], whereas another meta-analyses revealed no effect of immune modulating diets on mortality or length of stay [17]. Other systematic reviews looking at the efficacy of immunonutrition in the critically ill generally concluded that the incidence of infection and hospital length of stay are reduced, with no reduction in mortality [56, 58, 59]. Additionally, another meta-analysis showed that glutamine and selenium supplementation may result in reduction of nosocomial infections among the critically ill [60]. Although it is postulated that immunonutrition influence immune parameters and has anti-inflammatory effects, it is has not always been associated with better clinical outcomes. Some researchers propose that immunonutrition may be harmful in some subgroups of critically ill patients [55]. Rathmacher et al. found that blood urea was raised in patients receiving immunonutrition and attributed this to the combination of increased nitrogen load and the specific effect of arginine and glutamine in stimulating ureagenesis [61]. As such, careful assessment may be needed in patients with kidney and liver disease before immunonutrition can be prescribed. There is an emerging paradigm shift to move from immunonutrition to pharmaconutrition, where effect of individual immunonutrients are assessed independent of standard nutritional support [62]. The way forward is to design future studies similar to drug trials, which include evaluating clinically relevant outcome in a well-defined population [63].
Interestingly, immunomodulators have also been used in combination with antimicrobial therapy in clinical trials in search of new strategies for the treatment of bacterial infections [64]. Unfortunately, the use of immunonutritian was found not to be encouraging the antimicrobial therapy in bacterial infections [65,66,67]. However, this is an intelligent use of immunomodulators and this idea can be explored to look at other usage of immunonutrition.
This study has some limitations which have to be pointed out. Due to resource constraint, other cytokines indices such as tumour necrosis factor, IL-1, IL-8 and IL-10 were not measured. Confounding factors that may affect biomarker levels such as sepsis was also not included during data collection. Since patients’ overall progress and outcome were not looked into in this study, no definite correlation can be made between immunonutrition and patient outcome.
Conclusions
The present study showed that IL-6 levels were significantly reduced whereas glutathione levels were significantly higher following feeding with Neomune, an immunonutrition. These findings indicate the potential of immunonutrition reducing cytokines and increasing antioxidant indices in patients with TBI. However, further studies incorporating patient outcomes are needed to determine its overall clinical benefits.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- ICU:
-
Intensive care unit
- SIRS:
-
Systemic inflammatory response syndrome
- TBI:
-
Traumatic brain injury
References
MOH: National trauma database January 2009 to December 2009 fourth report. 2011.
Health Facts 2015 [http://vlib.moh.gov.my/cms/documentstorage/com.tms.cms.document.Document_2e8efe25-a0188549-d5315d00-e9ca9560/KKM_HEALTH_FACTS_2015.pdf].
Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation. 2007;22(5):341–53.
MOH: Malaysian registry of intensive care report for 2013. Malaysian Registry of Intensive Care, Clinical Research Centre, Ministry of Health Malaysia. 2013. http://www.moh.gov.my/index.php/file_manager/dl_item/554756755a584a696158526862693942626d567a6447567a61573973623264704947526862694253595864686447467549464a6863476.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442.
Clifton GL, Robertson CS, Grossman RG, Hodge S, Foltz R, Garza C. The metabolic response to severe head injury. J Neurosurg. 1984;60(4):687–96.
Clifton GL, Robertson CS, Choi SC. Assessment of nutritional requirements of head-injured patients. J Neurosurg. 1986;64(6):895–901.
Young B, Ott L, Norton J, Tibbs P, Rapp R, McClain C, et al. Metabolic and nutritional sequelae in the non-steroid treated head injury patient. Neurosurgery. 1985;17(5):784–91.
Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med. 2009;35(10):1728–37.
Wang X, Dong Y, Han X, Qi XQ, Huang CG, Hou LJ. Nutritional support for patients sustaining traumatic brain injury: a systematic review and meta-analysis of prospective studies. PLoS One. 2013;8(3):e58838.
Rosenfeld JV, Maas AI, Bragge P, Morganti-Kossmann MC, Manley GT, Gruen RL. Early management of severe traumatic brain injury. Lancet. 2012;380(9847):1088–98.
Grimble R. Nutritional modulation of immune function. Proc Nutr Soc. 2001;60(03):389–97.
Peterik A, Milbrandt EB, Darby JM. Immunonutrition in critical illness: still fishing for the truth. Crit Care. 2009;13(3):1–3.
De Arruda ISF, de Aguilar-Nascimento JE. Benefits of early enteral nutrition with glutamine and probiotics in brain injury patients. Clin Sci. 2004;106(3):287–92.
Briassoulis G, Filippou O, Kanariou M, Papassotiriou I, Hatzis T. Temporal nutritional and inflammatory changes in children with severe head injury fed a regular or an immune-enhancing diet: a randomized, controlled trial. Pediatr Crit Care Med. 2006;7(1):56–62.
Khorana J, Rerkasem K, Apichartpiyakul C, Sakonwasun C, Watcharasalcslip W, Waniyapong T, et al. Immunonutrition and cytokine response in patients with head injury. J Med Assoc Thail. 2009;92(2):188.
Marik PE, Zaloga GP. Immunonutrition in critically ill patients: a systematic review and analysis of the literature. Intensive Care Med. 2008;34(11):1980–90.
Serhan CN, Chiang N, Van Dyke TE. Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nat Rev Immunol. 2008;8(5):349–61.
Calder PC. n-3 Polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am J Clin Nutr. 2006;83:S1505–19.
Hasadsri L, Wang BH, Lee JV, Erdman JW, Llano DA, Barbey AK, et al. Omega-3 fatty acids as a putative treatment for traumatic brain injury. J Neurotrauma. 2013;30(11):897–906.
Bullock MR, Povlishock JT. Guidelines for the management of severe traumatic brain injury. Editor’s Commentary. J Neurotrauma. 2007;24(Suppl 1):2. p preceding S1
Harris JA, Benedict FG. A biometric study of human basal metabolism. Proc Natl Acad Sci. 1918;4(12):370–3.
Roza AM, Shizgal HM. The Harris Benedict equation reevaluated: resting energy requirements and the body cell mass. Am J Clin Nutr. 1984;40(1):168–82.
Painter TJ, Rickerds J, Alban RF. Immune enhancing nutrition in traumatic brain injury–A preliminary study. Int J Surg. 2015;21:70–4.
McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN). J Parenter Enter Nutr. 2009;33(3):277–316.
Wu GH, Zhang YW, Wu ZH. Modulation of postoperative immune and inflammatory response by immune-enhancing enteral diet in gastrointestinal cancer patients. World J Gastroenterol. 2001;7(3):357–62.
Uno H, Furukawa K, Suzuki D, Shimizu H, Ohtsuka M, Kato A, et al. Immunonutrition suppresses acute inflammatory responses through modulation of resolvin E1 in patients undergoing major hepatobiliary resection. Surgery. 2016;
Frugier T, Morganti-Kossmann MC, O’Reilly D, McLean CA. In situ detection of inflammatory mediators in post mortem human brain tissue after traumatic injury. J Neurotrauma. 2010;27(3):497–507.
Kossmann T, Hans VH, Imhof HG, Stocker R, Grob P, Trentz O, et al. Intrathecal and serum interleukin-6 and the acute-phase response in patients with severe traumatic brain injuries. Shock. 1995;4(5):311–7.
Lenzlinger PM, Morganti-Kossmann M-C, Laurer HL, McIntosh TK. The duality of the inflammatory response to traumatic brain injury. Mol Neurobiol. 2001;24(1–3):169–81.
Kalabalikis P, Papazoglou K, Gouriotis D, Papadopoulos N, Kardara M, Papageorgiou F, et al. Correlation between serum IL-6 and CRP levels and severity of head injury in children. Intensive Care Med. 1999;25(3):288–92.
Arand M, Melzner H, Kinzl L, Bruckner UB, Gebhard F. Early inflammatory mediator response following isolated traumatic brain injury and other major trauma in humans. Langenbeck's Arch Surg. 2001;386:241–8.
Woiciechowsky C, Schoning B, Cobanov J, Lanksch WR, Volk HD, Docke WD. Early IL-6 plasma concentrations correlate with severity of brain injury and pneumonia in brain-injured patients. J Trauma. 2002;5:339–45.
Lloyd E, Somera-Molina K, Van Eldik LJ, Watterson DM, Wainwright MS. Suppression of acute proinflammatory cytokine and chemokine upregulation by post-injury administration of a novel small molecule improves long-term neurologic outcome in a mouse model of traumatic brain injury. J Neuroinflammation. 2008;5(1):28.
Bracken MB. CRASH (corticosteroid randomization after significant head injury trial): landmark and storm warning. Neurosurgery. 2005;57(6):1300–2.
Ley EJ, Clond MA, Singer MB, Shouhed D, Salim A. IL6 deficiency affects function after traumatic brain injury. J Surg Res. 2011;170(2):253–6.
Yang SH, Gangidine M, Pritts TA, Goodman MD, Lentsch AB. Interleukin 6 mediates neuroinflammation and motor coordination deficits after mild traumatic brain injury and brief hypoxia in mice. Shock. 2013;40(6):471.
Marik PE. Arginine: too much of a good thing may be bad! Crit Care Med. 2006;34(11):2844–7.
Flaring UB, Rooyackers OE, Wernerman J, Hammarqvist F. Glutamine attenuates post-traumatic glutathione depletion in human muscle. Clin Sci (Lond). 2003;104(3):275–82.
Adesanya TA, Sullivan RC, Stawicki SP, Evans DC. Nutrition in Traumatic Brain Injury: Focus on the Immune Modulating Supplements. 2014.
Petersen SR, Jeevanandam M, Holaday NJ, Lubhan CL. Arterial-jugular vein free amino acid levels in patients with head injuries: important role of glutamine in cerebral nitrogen metabolism. J Trauma. 1996;41(4):687–94. discussion 694–685
Platt SR. The role of glutamate in central nervous system health and disease--a review. Vet J. 2007;173(2):278–86.
van Landeghem FK, Weiss T, Oehmichen M, von Deimling A. Decreased expression of glutamate transporters in astrocytes after human traumatic brain injury. J Neurotrauma. 2006;23(10):1518–28.
Zlotnik A, Gurevich B, Tkachov S, Maoz I, Shapira Y, Teichberg VI. Brain neuroprotection by scavenging blood glutamate. Exp Neurol. 2007;203(1):213–20.
Cook AM, Peppard A, Magnuson B. Nutrition considerations in traumatic brain injury. Nutr Clin Pract. 2008;23(6):608–20.
Fruin AH, Taylon C, Pettis MS. Caloric requirements in patients with severe head injuries. Surg Neurol. 1986;25(1):25–8.
Li P-A, Liu G-J, He QP, Floyd RA, Siesjö BK. Production of hydroxyl free radical by brain tissues in hyperglycemic rats subjected to transient forebrain ischemia. Free Radic Biol Med. 1999;27(9):1033–40.
Diaz-Parejo P, Ståhl N, Xu W, Reinstrup P, Ungerstedt U, Nordström C-H. Cerebral energy metabolism during transient hyperglycemia in patients with severe brain trauma. Intensive Care Med. 2003;29(4):544–50.
O'Dwyer ST, Smith RJ, Hwang TL, Wilmore DW. Maintenance of small bowel mucosa with glutamine-enriched parenteral nutrition. J Parenter Enter Nutr. 1989;13(6):579–85.
Houdijk AP, Van Leeuwen PA, Boermeester MA, Van Lambalgen T, Teerlink T, Flinkerbusch EL, et al. Glutamine-enriched enteral diet increases splanchnic blood flow in the rat. Am J Phys. 1994;267(6 Pt 1):G1035–40.
Yang DL, Xu JF. Effect of dipeptide of glutamine and alanine on severe traumatic brain injury. Chin J Traumatol. 2007;10(3):145–9.
Marik PE, Zaloga GP. Immunonutrition in High-Risk surgical patients a systematic review and analysis of the literature. J Parenter Enter Nutr. 2010;34(4):378–86.
Forget P, Echeverria G, Giglioli S, Bertrand B, Nikis S, Lechat J-P, De Kock M. Biomarkers in immunonutrition programme, is there still a need for new ones? A brief review. Ecancermedicalscience. 2015;9:546.
Aussel C, Cynober L. Is serum albumin a marker of nutritional status? Nutr Clin Metab. 2013;27(1):28–33.
Heyland DK, Novak F, Drover JW, Jain M, Su X, Suchner U. Should immunonutrition become routine in critically ill patients? A systematic review of the evidence. JAMA. 2001;286(8):944–53.
Roehl K. Immunonutrition in 2016: Benefit, Harm or Neither? Pract Gastroenterol. 2016;154:27.
McCowen KC, Bistrian BR. Immunonutrition: problematic or problem solving? Am J Clin Nutr. 2003;77(4):764–70.
Beale RJ, Bryg DJ, Bihari DJ. Immunonutrition in the critically ill: a systematic review of clinical outcome. Crit Care Med. 1999;27(12):2799–805.
Montejo JC, Zarazaga A, Lόpez-Martínez J, Urrútia G, Roqué M, Blesa AL, et al. Immunonutrition in the intensive care unit. A systematic review and consensus statement. Clin Nutr. 2003;22(3):221–33.
Chen QH, Yang Y, He HL, Xie JF, Cai SX, Liu AR, et al. The effect of glutamine therapy on outcomes in critically ill patients: a meta-analysis of randomized controlled trials. Crit Care. 2014;18(1):R8.
Rathmacher JA, Nissen S, Panton L, Clark RH, May PE, Barber AE, et al. Supplementation with a combination of β-hydroxy-β-methylbutyrate(HMB), arginine, and glutamine is safe and could improve hematological parameters. J Parenter Enter Nutr. 2003;28:65–75.
Heyland D, Dhaliwal R. Immunonutrition in the critically ill: from old approaches to new paradigms. Intensive Care Med. 2005;31:501–3.
Jones NE, Heyland DK. Pharmaconutrition: a new emerging paradigm. Curr Opin Gastroenterol. 2008;24:215–22.
Sparo M, Sanchez Bruni SF. Approach to optimise the treatment of bacterial infections: combined antimicrobial therapy with enhancers of innate immunity. Clin Exp Pharmacol. 2012;2:e106.
Vincent JL. Search for effective immunomodulating strategies against sepsis. Lancet. 1998;351(9107):922–3.
Dellinger RP. Severe sepsis trials: why have they failed? Minerva Anestsesiol. 1999;65(6):340–5.
Cohen J. Adjunctive therapy in sepsis: a critical analysis of the clinical trial programme. Br Med Bull. 1999;55(1):212–25.
Acknowledgements
Not applicable.
Funding
This work was supported by the University of Malaya Research Grant (P0010-2014A) and Fundamental Research Grant Scheme initiative (FP019-2013B).
Availability of data and materials
The datasets collected and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Authors’ contributions
VRHR, GO, LFP, SFS developed and supervised the study. LFP, JSV, PSL, PCT and RO coordinated the study, recruited subjects and gathered informed consent. AA, MKAK and MIOJ interpreted, analysed the data and performed statistical analyses. AA wrote the first draft. AA, VRHR, PCT, PSL and MIOJ revised subsequent drafts of the manuscript and performed additional statistical analyses. All authors have read and approved of the final manuscript.
Competing interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethical approval and consent to participate
This study and its protocol was approved by the Medical Ethics Committee University Malaya Medical Center (MEC ID NO: 20,143–15). Written informed consent was obtained from patient’s next of kin.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Rai, V.R.H., Phang, L.F., Sia, S.F. et al. Effects of immunonutrition on biomarkers in traumatic brain injury patients in Malaysia: a prospective randomized controlled trial. BMC Anesthesiol 17, 81 (2017). https://doi.org/10.1186/s12871-017-0369-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-017-0369-4