Abstract
Background
This study was aimed to evaluate the prevalence and molecular characteristics of ciprofloxacin resistance among 346 Escherichia coli isolates collected from clinical specimens (n = 82), healthy children (n = 176), municipal wastewater (n = 34), hospital wastewater (n = 33), poultry slaughterhouse wastewater (n = 12) and livestock (n = 9) slaughterhouse wastewater in Iran.
Methods
Ciprofloxacin minimum inhibitory concentration (MIC) was determined by agar dilution assay. Phylogroups and plasmid-mediated quinolone resistance (PMQR) genes were identified using PCR. Mutations in gyrA, gyrB, parC, and parE genes and amino acid alterations were screened through sequencing assay. The effect of efflux pump inhibitor (PAβN) on ciprofloxacin MICs in ciprofloxacin-resistant isolates was investigated using the microdilution method.
Results
In total, 28.03% of E. coli isolates were phenotypically resistant to ciprofloxacin. Based on sources of isolation, 64.63%, 51.51%, 33.33%, 14.70%, 10.22% and 8.33% of isolates from clinical specimens, hospital wastewater, livestock wastewater, municipal wastewater, healthy children and poultry wastewater were ciprofloxacin-resistant, respectively. Eighty-one point eighty-one percent (Ser-83 → Leu + Asp-87 → Asn; 78.78% and Ser-83 → Leu only; 3.03% (of ciprofloxacin-resistant E. coli isolates showed missense mutation in GyrA subunit of DNA gyrase, while no amino-acid substitution was noted in the GyrB subunit. DNA sequence analyses of the ParC and ParE subunits of topoisomerase IV exhibited amino-acid changes in 30.30% (Ser-80 → Ile + Glu-84 → Val; 18.18%, Ser-80 → Ile only; 9.10% and Glu-84 → Val only; 3.03%0 (and 15.38% (Ser-458 → Ala) of ciprofloxacin-resistant E. coli isolates, respectively. The PMQR genes, aac(6')-Ib-cr, qnrS, qnrB, oqxA, oqxB, and qepA were detected in 43.29%, 74.22%, 9.27%, 14.43%, 30.92% and 1.03% of ciprofloxacin-resistant isolates, respectively. No isolate was found to be positive for qnrA and qnrD genes. In isolates harboring the OqxA/B efflux pump, the MIC of ciprofloxacin was reduced twofold in the presence of PAβN, as an efflux pump inhibitor. The phylogroups B2 (48.45%) and A (20.65%) were the most predominant groups identified in ciprofloxacin-resistant isolates.
Conclusions
This study proved the high incidence of ciprofloxacin-resistant E. coli isolates in both clinical and non-clinical settings in Iran. Chromosomal gene mutations and PMQR genes were identified in ciprofloxacin resistance among E. coli population.
Similar content being viewed by others
Background
Escherichia coli is the most common gram-negative rod responsible for a variety of intestinal and extraintestinal infections worldwide [1]. As a major part of the natural human intestinal microbial flora, E. coli is associated with a variety of community- and hospital-acquired opportunistic infections such as urinary tract infections (UTIs), septicemia, pneumonia, peritonitis, neonatal meningitis, and some other diseases [1]. Commonly, beta-lactam antibiotics are used to treat infections caused by E. coli. However, currently, due to increased resistance to β-lactam antibiotics, fluoroquinolones are used as alternative drugs to treat urinary tract infections caused by E. coli particularly in Asian countries [2]. These synthetic antibiotics inhibit the activity of DNA gyrase and topoisomerase IV, and break down the DNA strands, thereby killing the bacteria [3]. Resistance to fluoroquinolones in gram-negative bacteria is acquired either vertically by mutations in chromosomal genes or by horizontal transfer of resistance plasmids [4].
Mutations in genes encoding the target enzymes reduce the affinity of fluoroquinolones to bind to the DNA-enzyme complex and confer high levels of resistance to fluoroquinolones [5]. Mutations occur in the GyrA and GyrB subunits of DNA gyrase and the ParC and ParE subunits of topoisomerase IV enzymes [3]. Mutations in genes encoding outer membrane porins, e.g., OmpF, and efflux pumps, e.g., AcrAB-TolC, have also been shown in E. coli. These mutations reduce the expression of porins and increase the expression of efflux pumps, which decreases the intracellular concentration of antibiotics [6].
Plasmid-mediated quinolone resistance (PMQR) mechanisms include (i) Qnr proteins family including QnrA, QnrB, QnrD, QnrC, and QnrS, which protect gyrase and topoisomerase IV from fluoroquinolone inhibition. (ii) A new aminoglycoside acetyltransferase enzyme, AAC(6')-Ib-cr, which in addition to resistance to aminoglycosides, can acetylate fluoroquinolones [4]. (iii) Plasmid-dependent efflux pumps such as OqxA/B and QepA which extrude antibiotics out of the cell [7].
As mentioned above, the accumulation of mutations in bacterial DNA gyrase and topoisomerase IV is the main mechanism of resistance to fluoroquinolones in gram-negative bacteria [8]. Plasmid-mediated mechanisms usually confer low-level fluoroquinolone resistance which can lead to the occurrence of selective pressure for the growth of higher-level resistant mutants in the presence of fluoroquinolones at therapeutic concentrations [9]. Moreover, plasmid-mediated resistance can be transferred horizontally among the Enterobacteriaceae family, which could further facilitate the dissemination of antibiotic-resistance genes within different reservoirs [10].
Fluoroquinolones are widely used as antibiotics in human and veterinary medicine, and also as growth promoters in food-producing animals which lead to an increased prevalence of fluoroquinolone-resistant bacteria [11]. In Enterobacteriaceae family members particularly in E. coli isolates, the fluoroquinolone resistance is becoming increasingly common both in hospital- and community-acquired infections [2, 12]. However, the dissemination of fluoroquinolone-resistant E. coli isolates is not limited to clinical infections but also has been reported in various non-clinical resources [13].
Understanding the prevalence of ciprofloxacin resistance and elucidating the resistance genetic mechanisms would enable better decisions in treating E. coli infections and applying effective infection control measures.
Because of the lack of information on ciprofloxacin resistance in E. coli isolates especially in isolates derived from non-clinical settings in Iran, this study aimed: (i) to investigate the frequency of ciprofloxacin resistance in E. coli strains isolated from both clinical and non-clinical settings (healthy carriers, municipal, hospital, poultry and livestock wastewaters). (ii) to explore the genetic background behind ciprofloxacin resistance and (iii) to elucidate the molecular epidemiology of ciprofloxacin-resistant isolates using a phylogenetic grouping approach.
Results
In the current study, 28.03% (n = 97) of E. coli isolates showed MICs above the resistance breakpoint (≥ 1 μg/mL) and were considered ciprofloxacin-resistant (Table 1). Clinical E. coli isolates with 64.63% (n = 53/82) showed the highest frequency of ciprofloxacin resistance followed by isolates from hospital wastewater (51.51%, n = 17/33), livestock slaughterhouse wastewater (33.33%, n = 3/9), municipal wastewater (14.7%, n = 5/34), healthy carriers (10.22%, n = 18/176) and poultry slaughterhouse wastewater (8.33%, n = 1/12). However, in comparison, there were no significant differences in the rate of ciprofloxacin resistance in isolates collected from clinical specimens with hospital wastewater (P > 0.05), healthy carriers with municipal wastewater (P > 0.05), and poultry slaughterhouse wastewater with livestock slaughterhouse wastewater (P > 0.05).
Overall, the MICs of ciprofloxacin for ciprofloxacin-resistant E. coli isolates were between 2 and 256 μg/mL (Table 1). The isolates collected from clinical specimens, hospital wastewater, poultry slaughterhouse wastewater, and livestock slaughterhouse wastewater showed an MIC50 value of 32 µg/mL for each one, while for isolates collected from healthy carriers and municipal wastewater, the MIC50 value was 4 µg/mL.
In the current study, as shown in Figure 1A, 81.81% (n = 27/33) of ciprofloxacin-resistant E. coli isolates showed at least a missense mutation in the gyrA gene. Among them, 78.78% (n = 26/33) of isolates had double amino-acid substitution at sites 83 (Ser-83→Leu) and 87 (Asp-87→Asn), and 3.03% (n = 1/33) of isolates showed a single substitution at site 83 (Ser-83→Leu) in GyrA subunit of DNA gyrase enzyme. Statistically, there was no association between the types of mutation in the gyrA gene and the sources of the isolates (P > 0.05). In this study, no missense mutation was identified in gyrB.
DNA sequence analyses of the ParC subunit of topoisomerase IV exhibited amino-acid changes in 30.30% (n = 10/33) of ciprofloxacin-resistant E. coli isolates. Among them, 18.18% (n = 6/33) of isolates showed double amino-acid substitution at positions 80 (Ser-80→Ile) and 84 (Glu-84→Val). Additionally, 9.09% (n = 3/33) and 3.03% (n = 1/33) of ciprofloxacin-resistant E. coli isolates harbored single substitutions at positions 80 (Ser-80→ Ile) and 84 (Glu -84→Val), respectively (Fig. 1B). These changes were significantly associated with isolates from clinical specimens and hospital wastewater.
In the present study, we identified 15.38% of isolates with a single missense mutation in ParE subunit of topoisomerase IV, which encodes Ser-458→Ala (Fig. 1C). Statistically, there was no association between the types of mutation in parE gene and sources of the isolates (P > 0.05).
The isolates with single or no mutation in topoisomerase IV and DNA gyrase showed lower ciprofloxacin MIC50 and MIC90 values (Table 2).
The prevalence of PMQR genes is described in Table 3. Overall, the aac (6')-Ib-cr gene was detected in 43.29% (n = 42/97) of ciprofloxacin-resistant isolates. qnrS and qnrB genes were identified in 74.22% (n = 72/97) and 9.27% (n = 9/97) of ciprofloxacin-resistant E. coli isolates, respectively. In this study, no isolate was found to be positive for qnrA and qnrD genes. The genes encoding efflux pumps; oqxB, oqxA, and qepA were identified in 30.92% (n = 30/97), 14.43% (n = 14/97), and 1.03% (n = 1/97) of ciprofloxacin-resistant E. coli isolates, respectively. The MIC50 values for ciprofloxacin in isolates harboring aac (6')-Ib-cr and qepA were higher than those containing other genes. Overall, MIC90 values were high in all isolates except for those containing qnrB (Table 3).
Analysis of ciprofloxacin resistance genes co-occurrences in ciprofloxacin-resistant E. coli isolates revealed 16 different patterns. Among them, 17.52% of isolates contained profiles with 3 different PMQR genes, simultaneously (Table 4). Increased levels of ciprofloxacin MICs were not observed in isolates containing multiple PMQR genes.
As shown in Table 5, in isolates harboring OqxA/B efflux pumps the MIC of ciprofloxacin was reduced twofold in the presence of PAβN (the efflux pump inhibitor) compared to the absence of inhibitor. No change in MIC of ciprofloxacin was observed in isolates lacking oqxA/B genes in the presence of PAβN.
In the present study, as shown in Figure 2, ciprofloxacin-resistant E. coli isolates were distributed among different phylogroups. However, irrespective of the source of collection, phylogroups B2 and A with 48.45% (n = 47/97) and 20.65% (n = 20/97) of the isolates were the most predominant groups identified, respectively. According to the source of collection, the incidence of phylogroup B2 was significantly higher than other groups among strains isolated from clinical specimens; 54.71% (n = 29/53), municipal wastewater; 60% (n = 3/5), hospital wastewater; 47.05% (n= 8/17) and healthy people; 38.90% (n = 7/18). In isolates collected from livestock wastewater, the occurrence of strains belonging to phylogroup A was significantly higher and a single ciprofloxacin-resistant E. coli isolate collected from poultry wastewater belonged to clade I/II phylogroup.
The relative frequency distribution of PMQR genes among ciprofloxacin-resistant E. coli phylogroups was significantly different (Table 6). qnrS and oqxA genes were most frequently detected in phylogroup D, oqxB in phylogroup E, qepA in phylogroup B2, and qnrB in isolates with unknown phylogroup.
Discussion
Ciprofloxacin, a fluoroquinolone antibiotic, has been widely used to treat infections caused by E. coli [14]. Hence, E. coli resistance to ciprofloxacin has been steadily increasing worldwide [14]. Previous reports in Iran indicated ciprofloxacin resistance varying from 30 to 100% in E. coli isolates collected from clinical specimens [15, 16]. Our results in this study also confirmed a high prevalence of ciprofloxacin-resistant E. coli clinical isolates in Ardabil hospitals (64.6%). The high resistance rate of E. coli clinical isolates can be attributed to the high consumption of ciprofloxacin in Iranian hospitals [17, 18]. Additionally, geographical differences in the prevalence of resistance to ciprofloxacin can be due to the extent of use of fluoroquinolone in each region or differences in methods of the assessment of antibiotic resistance [15].
Notably, the prevalence of resistance to ciprofloxacin in E. coli isolates in healthy children (10.22%) was lower than in clinical isolates. A study reported a higher incidence of colonization with ciprofloxacin-resistant E. coli in Spanish healthy adults (24%) and children (16%) [19, 20]. Exposure of commensal flora to antibiotics is a known risk factor correlated with increased antimicrobial resistance rate [21]. The high prevalence of multidrug-resistant commensal E. coli isolated from healthy individuals is being reported from different regions, especially in low- and middle-income countries [22]. The widespread exposure of commensal E. coli to ciprofloxacin is not the case in the current study because fluoroquinolones are not frequently prescribed in outpatient settings in Iran [23]. Similarly, resistance to ciprofloxacin in commensal E. coli isolates was reported in children with no previous exposure to ciprofloxacin [12]. Healthy children may acquire ciprofloxacin-resistant E. coli from adults or through foods and environmental contaminations.
In wastewater resources, the rate of resistance to ciprofloxacin in E. coli strains isolated from hospital wastewater was significantly higher than in isolates collected from other resources (51.5%). Similar results were reported from the studies in Hamadan (30.61%), Tabriz (29%), and the Netherlands (54%) [24,25,26]. In the current study, 14.70% of E. coli isolates from municipal wastewater were found to be ciprofloxacin-resistant. These findings are somewhat akin to the profile obtained in fecal isolates from healthy individuals, discussed above. The bacterial profile of untreated municipal wastewater has been shown to mirror that of human fecal flora [27], in a way that municipal wastewater isolates can be used as a surrogate to study human commensal E. coli in a local population [28, 29]. In a study in Iran, it has been shown that fluoroquinolones accounted for 5.7% of the antibiotics sold out by veterinary pharmaceutical companies in 2010 [30], which can promote the emergence of resistance to ciprofloxacin in bacteria from food-producing animals [31]. However, in countries where fluoroquinolones are not permitted for use in food-producing animals, ciprofloxacin resistance has also not been observed in bacteria of animals [32]. In the present study, 33.3% of isolates from livestock slaughterhouse wastewater and 8.3% of poultry slaughterhouse wastewater isolates were resistant to ciprofloxacin, which is in accordance with the results of the study by Naraghi et al. in northeast Iran [33].
Point mutations in the chromosomal target genes (i.e, gyrA, gyrB, parC, and parE genes) are the most common bacterial resistance mechanisms to quinolones, which missense amino-acid substitutions occur at several sites in the QRDR region of target proteins [8]. It has been documented that the accumulation of specific mutations in both the DNA gyrase and topoisomerase genes causes high resistance to ciprofloxacin in E. coli isolates [8], accordingly similar results were observed in the current study. However, a single mutation in one of these genes is often sufficient to increase the ciprofloxacin MIC beyond the resistance breakpoints, hence allowing the emergence of secondary mutations in the presence of ciprofloxacin selective pressure, that further increase the MIC level [8]. Most reported point mutation in the gyrA gene occurs in nucleotides 248 and 260 changing serine-83 and asparagine-87 amino acids [34]. Similarly, Ser-83→Leu and Asp-87→Asn amino-acid substitutions in the GyrA subunit were the most identified mutations in our isolates. Amino-acid changes in the GyrB subunit of DNA gyrase enzyme are relatively low [8, 35,36,37,38,39]. Likewise, in the present study, no missense mutation was observed in the GyrB subunit in E. coli strains resistant to ciprofloxacin.
The most common missense mutations in the parC gene are reported in nucleotides 238/239 and 250/251 leading to changes in serine-80 and glutamate-84 [34]. In the current study, the most common amino-acid changes in the ParC subunit were the substitution of glutamate to valine (E-84→V) (21.2%) and serine to isoleucine (S-80→I) (27.2%). Similar findings were reported from different regions of Iran [40,41,42] and other countries [36,37,38,39, 43]. In general, missense mutations in the QRDR region of ParE subunit in E. coli is infrequent compared to the ParC subunit of topoisomerase IV [8]. The sole replacement observed in the current study was Ser-458→Ala consistent with reports from other countries [42, 44,45,46,47].
Genes carried by a plasmid, such as aac (6')-Ib-cr, qnr, qepA, and oqxA/B contribute to ciprofloxacin resistance in E. coli as reported in bacteria from human, animal, and environmental resources [48]. The PMQR genes often confer low-level resistance to quinolones and/or fluoroquinolones by themselves, but instead, they create favorable conditions for the selection of more resistant mutants [9]. However, among different PMQR determinates some genes like aac (6')-Ib-cr and qepA are slightly associated with higher ciprofloxacin MIC values [10]. In accordance with previous reports, E. coli isolates containing these genes showed higher ciprofloxacin MIC50 values in our study. The aac (6')-Ib-cr is more commonly found in E. coli compared to other Enterobacteriaceae members [49]. We detected aac (6')-Ib-cr in 43.2% of ciprofloxacin-resistant E. coli isolates. In controversy to other studies that reported qnrB as the most frequent Qnr protein-encoding gene [50], we identified the qnrS gene in most ciprofloxacin-resistant E. coli isolates. Yanat et. al reported the distribution of the PMQR genes differs by geographic region and isolates selection criteria [48] which may explain the mentioned controversy. However, our results on the qnr genes pattern are inconsistent with the findings in Iran and some countries [8, 31, 37, 41, 51,52,53]. The oqxA, oqxB, and qepA genes encoding plasmid-mediated efflux pumps were identified in 14.43%, 30.92% and 1.03% of ciprofloxacin-resistant E. coli isolates, respectively. The QepA and OqxA/B are generally rare in Enterobacteriaceae members [48] meanwhile most OqxA/B cases were reported from animal isolates in China [54]. Surprisingly, oqxA/B positive ciprofloxacin-resistant E. coli isolates were from healthy children and hospital wastewater in this study. Similar to findings reported by Khalil, et.al. [55], we found that PaβN, as an efflux pump inhibitor, reduced the ciprofloxacin MIC in isolates containing OqxA/B supporting the importance of OqxA/B in ciprofloxacin resistance. It has been shown that the coexistence of PMQR determinates in E. coli could potentially cause higher levels of quinolone resistance [50]. However, such an association was not observed in our isolates. This controversy may be explained by the additional undetected resistance mechanisms such as overexpression of chromosomal ArcAB-TolC multi-drug efflux pump in ciprofloxacin-resistant E. coli isolates [6].
In addition to ciprofloxacin resistance data, we also provided relevant information on the molecular epidemiologic characteristics of ciprofloxacin-resistant E. coli isolates. E. coli is classified into eight phylogroups named A, B1, B2, C, D, E, F, and clade I/II [56]. Irrespective of collection sources, the phylogroup B2 (48.45%) and A (20.65%) were the predominant groups in ciprofloxacin-resistant E. coli isolates in the current study. It has been documented that the distribution of E. coli phylogroups differs according to geographic location, climate, specific lifestyles, and hosts [57]. We observed a positive correlation between the occurrences of phylogroups in isolates from clinical specimens with hospital wastewater, and healthy carriers with municipal wastewater. The phylogroup B2 was the most common group in isolates collected from the abovementioned sources. This may express the possibility of dissemination of ciprofloxacin-resistant E. coli isolates from hospital discharges and fecal materials from healthy children into hospital and municipal wastewaters, respectively [27]. This explanation is also supported by the fact that the ciprofloxacin resistance prevalence and MIC50 levels coincided in clinical and commensal isolates with those from hospital and municipal wastewaters, respectively.
Some shreds of evidence represent the higher antibiotic resistance rate in certain E. coli phylogroups compared to others [15]. Our literature surveys did not get any results on the association between phylogroups of E. coli with a specific antibiotic resistance phenotype. Here, we report that ciprofloxacin resistance in E. coli may link to phylogroup B2. The distribution of PMQR genes was significantly different among phylogroups. However, more diverse PMQR genes were observed in phylogroup B2 isolates. This is similar to the findings reported by Nojoomi et al., which showed a higher incidence of some beta-lactamase encoding genes and virulence determinants in phylogroup B2 isolates [58].
Limitations of the study
Due to limited resources, the mutations in DNA gyrase and topoisomerase genes were not studied on all ciprofloxacin-resistant E. coli isolates. Additionally, the expression level of chromosomal multi-drug efflux pump ArcAB-TolC was not studied which could contribute to ciprofloxacin resistance.
We characterized the molecular relatedness of the ciprofloxacin-resistant E. coli isolates using the PCR-based phylotyping method. However, more robust molecular typing methods such as pulsed-field gel electrophoresis (PFGE) and multi-locus sequence typing (MLST) methods need to determine the isolates' precise genetic relatedness from different resources.
Conclusion
To conclude, ciprofloxacin resistance was significantly prevalent in E. coli isolates from clinical specimens, healthy children, and wastewaters in Iran. Hence, continuous surveillance of ciprofloxacin resistance trends and MIC values along with prudent use of fluoroquinolone antibiotics in clinics, prohibition of its use in food-producing animals, and efficient disinfection of wastewater are recommended to prevent the emergence and spread of ciprofloxacin-resistant E. coli isolates. On the other hand, we confirmed the role of multiple mechanisms including the presence of PMQR genes and mutations in the QRDRs in the emergence of ciprofloxacin resistance in E. coli isolates from both clinical and non-clinical sources in Ardabil. Double and concurrent mutations within gyrA and parC genes were common and associated with increased ciprofloxacin MICs in ciprofloxacin-resistant isolates. Furthermore, aac(6')-Ib-cr, qnrS, and oqxB were the most prevalent PMQR genes in ciprofloxacin-resistant isolates, and the presence of aac(6')-Ib-cr and qepA genes were associated with higher ciprofloxacin MIC50 levels. Ciprofloxacin-resistant E. coli isolates were mainly linked to phylogroup B2. This suggests the possible dissemination of ciprofloxacin-resistant E. coli through various environments. Therefore, understanding antibiotic resistance mechanisms and the genetic relatedness of bacteria using reliable methods can help develop effective strategies to prevent the spread of resistant bacteria.
Materials and methods
Bacterial isolates
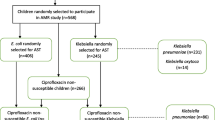
In this study, a total of 346 E. coli isolates from clinical specimens (n = 82), healthy children (n = 176) and municipal (n = 34), hospital (n = 33), poultry (n = 12) and livestock (n = 9) slaughterhouse wastewater were included. The isolates from healthy children [28] and wastewater resources were previously collected in Ardabil from April 2017 to February 2019. Wastewater samples had been collected from the raw sewage influent of four teaching hospitals (Imam, Fatemi, Alavi, and Bouali) affiliated with Ardabil University of Medical Sciences (ARUMS), and also poultry slaughterhouse, livestock slaughterhouse, and municipal wastewater treatment plants in Ardabil province, Iran. Liquid wastewater samples were collected from one sampling point in 500 mL sterile bottles in accordance with the U.S. Environmental Protection Agency (US EPA) standard operating procedure for wastewater sampling [59]. Collected samples were immediately transferred to the microbiology laboratory in cold box containers and kept at 4 °C. Microbiological analysis was performed in less than 2 h after sample collection. Clinical isolates were from patients admitted to a referral hospital (Imam) affiliated with ARUMS from April 2021 to September 2021. The study was approved by the regional ethics committee in ARUMS (reference no. IR.ARUMS.REC.1399.553). Isolates were identified using conventional microbiology and biochemical tests [60] and kept in 15 % glycerol stock cultures at – 70 °C for further studies.
Ciprofloxacin susceptibility assay
The minimum inhibitory concentrations (MICs) of ciprofloxacin (Sigma-Aldrich, USA) for E. coli were determined using the agar dilution method [61]. The concentration of ciprofloxacin ranged from 0.12 to 256 µg/mL. The results were interpreted according to CLSI guidelines [62]. The isolates with MICs ≥1 µg/mL and 0.5 µg/mL were considered ciprofloxacin-resistant and -intermediate-resistant (I), respectively.
Amplification of ciprofloxacin resistance encoding genes
Genomic DNA from ciprofloxacin-resistant E. coli isolates was extracted using the boiling method as previously reported [63]. The presence of PMQR encoding genes: qnr (A, B, D, and S), aac (6')-Ib-cr, qepA, and oqxA/B were detected by PCR using previously described primer sequences (synthesized in SinaClon Co. Iran) and cycling parameters [42, 56, 64, 65].
A representative PCR product for each gene was sequenced (Microsynth Co. Switzerland) and aligned using the Basic Local Alignment Search Tool (BLAST) at National Center for Biotechnology Information (NCBI) Center database [available at http://blast.ncbi.nlm.nih.gov/]. Genomic DNA from isolates carrying the corresponding resistance genes was used as a positive control in PCR experiments.
Detection of missense mutations in topoisomerase enzymes
In total, 33 ciprofloxacin-resistant isolates were selected based on distribution frequency and MIC levels from hospital wastewater (n = 10), municipal wastewater (n = 5) livestock slaughterhouse wastewater (n = 2), poultry slaughterhouse wastewater (n = 1), healthy carriers (n = 5) and clinical isolates (n = 10). The gyrA, and gyrB genes encoding DNA gyrase and parC gene encoding topoisomerase IV enzymes were amplified using specific primers as described previously [42, 45]. For topoisomerase IV parE gene 13 isolates were included [45]. The amplified DNA fragments were sent for sequencing by Microsynth Co. Switzerland. Point mutations in gyrA, gyrB, parC, and parE genes were identified throughout the nucleotide sequences by comparing them with the corresponding sequence of E. coli ATCC 25922 using DNAMAN software version 10 [https://dnaman.software.informer.com/].
Inhibition study of efflux pumps using phenylalanine -Arginine β- naphthylamide (PAβN)
To evaluate the role of OqxA/B efflux pumps in E. coli ciprofloxacin resistance, 5 isolates harboring oqxA/B genes were selected. The reduction in MICs of ciprofloxacin was evaluated using the microdilution method in 96-house plates in accordance with CLSI instructions [62]. Briefly, serially twofold dilutions of the ciprofloxacin, with concentrations ranging from 0.12 to 256 µg/mL, were prepared in a sterile Müller Hinton Broth (Himedia, India) culture medium. Then, 100 μL from each dilution was transferred into wells of a microtiter plate and inoculated with 5 µL of standardized bacterial suspension (1.5 × 107 CFU/mL). Finally, a constant volume (4 μL) of the efflux pump inhibitor (PAβN) at a concentration of 100 μg/mL was added to each well. The plates were incubated at 37 °C for 24 h. The change of ciprofloxacin MIC in the presence of the inhibitor was recorded compared to those with no PAβN [66].
Phylotyping of E. coli isolates
The phylogroups of ciprofloxacin-resistant E. coli strains were determined by Quadruplex-PCR as previously described by Clermont et al. In this method, based on the combined patterns of arpA, chuA, yjaA, TspE4.C2, trpA, arpAgpE, trpAgpC, and internal control genes, E. coli isolates are classified into groups A, B1, B2, C, D, E, F and clade I [56].
Statistical analyses
Comparison of the prevalence of resistance to ciprofloxacin and association between resistance genes in E. coli isolates from clinical specimens, hospital wastewater, municipal wastewater, poultry slaughterhouse wastewater, and livestock slaughterhouse wastewater were evaluated using the Chi-square and Fisher’s exact tests. A p-value of < 0.05 was used to indicate statistically significant results.
Availability of data and materials
The datasets generated and analyzed during the current study are available in the NCBI GenBank repository, under the accession numbers: OM791372 to OM791375, MZ359353 to MZ359375, OM791362 to OM791371 and OM831129.
Abbreviations
- ATCC:
-
American-type culture collection
- BLAST:
-
Basic local alignment search tool
- CLSI:
-
Clinical and laboratory standards institute
- DNA:
-
Deoxyribonucleic acid
- EPA:
-
Environmental protection agency
- MIC:
-
Minimum inhibitory concentration
- NCBI:
-
National Center for biotechnology information
- PAβN:
-
Phenylalanine -arginine β- naphthylamide
- PCR:
-
Polymerase chain reaction
- PMQR:
-
Plasmid-mediated quinolone resistance
References
Mueller M, Escherichia TCR, Coli, in StatPearls. StatPearls Publishing Copyright © 2022. Treasure Island (FL): StatPearls Publishing LLC; 2022.
Stapleton AE, Wagenlehner FME, Mulgirigama A, Twynholm M. Escherichia coli resistance to fluoroquinolones in community-acquired uncomplicated urinary tract infection in women: a Systematic Review. Antimicrob Agents Chemother. 2020;64:e00862-e920.
Pham TDM, Ziora ZM. Blaskovich MAT. Quinolone antibiotics Medchemcomm. 2019;10(10):1719–39.
Ayobola ED, Oscar WO, Ejovwokoghene EF. Plasmid-mediated quinolone resistance genes transfer among enteric bacteria isolated from human and animal sources. AIMS Microbiol. 2021;7(2):200–15.
Mares M, Lim SHE, Lai K-S, Cristina R-T, editors. Antimicrobial resistance: A one health perspective. London, England: IntechOpen; 2021.
Arzanlou M, Chai WC, Venter H. Intrinsic, adaptive and acquired antimicrobial resistance in Gram-negative bacteria. Essays Biochem. 2017;61(1):49–59.
Li J, Zhang H, Ning J, Sajid A, Cheng G, Yuan Z, et al. The nature and epidemiology of OqxAB, a multidrug efflux pump. Antimicrob Resist Infect Control. 2019;8(1):44.
Correia S, Poeta P, Hébraud M, Luis Capelo J, Igrejas G. Mechanisms of quinolone action and resistance: where do we stand? J Med Microbiol. 2017;66(5):551–9.
Strahilevitz J, Jacoby GA, Hooper DC, Robicsek A. Plasmid-mediated quinolone resistance: a multifaceted threat. Clin Microbiol Rev. 2009;22(4):664–89.
Poirel L, Cattoir V, Nordmann P. Plasmid-mediated quinolone resistance; interactions between human, animal, and environmental ecologies. Front Microbiol. 2012;3:24.
Kenyon C. Positive association between the use of quinolones in food animals and the prevalence of fluoroquinolone resistance in E. coli and K. pneumoniae, A. baumannii and P. aeruginosa: A global ecological analysis. Antibiotics. 2021;10(10):1193.
Dalhoff A. Global fluoroquinolone resistance epidemiology and implications for clinical use. Interdiscip Perspect Infect Dis. 2012;2012:976273.
Belotindos L, Villanueva M, Miguel J Jr, Bwalya P, Harada T, Kawahara R, et al. Prevalence and characterization of quinolone-resistance determinants in Escherichia coli isolated from food-producing animals and animal-derived food in the Philippines. Antibiotics. 2021;10(4):413.
Fasugba O, Gardner A, Mitchell BG, Mnatzaganian G. Ciprofloxacin resistance in community- and hospital-acquired Escherichia coli urinary tract infections: a systematic review and meta-analysis of observational studies. BMC Infect Dis. 2015;15:545.
Halaji M, Fayyazi A, Rajabnia M, Zare D, Pournajaf A, Ranjbar R. Phylogenetic group distribution of uropathogenic Escherichia coli and related antimicrobial resistance pattern: A meta-analysis and systematic review. Front Cell Infect Microbiol. 2022;12:790184.
Mortazavi-Tabatabaei SAR, Ghaderkhani J, Nazari A, Sayehmiri K, Sayehmiri F, Pakzad I. Pattern of antibacterial resistance in urinary tract infections: A systematic review and meta-analysis. Int J Prev Med. 2019;10:169.
Abbasian H, Hajimolaali M, Yektadoost A, Zartab S. Antibiotic utilization in Iran 2000–2016: Pattern analysis and benchmarking with organization for economic co-operation and development countries. J Res Pharm Pract. 2019;8(3):162–7.
Hassanshahi G, Darehkordi A, Sheikh Fathollahi M, Khanamani Falahati-Pour S, Rezazadeh Zarandi E, Assar SH. Resistance pattern of Escherichia coli to levofloxacin in Iran: a narrative review. Iran J Microbiol. 2020;12(3):177–84.
Garau J, Xercavins M, Rodríguez-Carballeira M, Ramón Gómez-Vera J, Coll I, Vidal D, et al. Emergence and dissemination of quinolone-resistant Escherichia coli in the community. Antimicrob Agents Chemother. 1999;43(11):2736–41.
Oteo J, Lázaro E, Baquero F, Campos J. Antimicrobial-resistant invasive Escherichia coli. Spain Emerg Infect Dis. 2005;11(4):546–53.
Mahmoodi F, Rezatofighi SE, Akhoond MR. Antimicrobial resistance and metallo-beta-lactamase producing among commensal Escherichia coli isolates from healthy children of Khuzestan and Fars provinces; Iran. BMC Microbiol. 2020;20(1):366.
Nji E, Kazibwe J, Hambridge T, Joko CA, Larbi AA, Damptey LAO, et al. High prevalence of antibiotic resistance in commensal Escherichia coli from healthy human sources in community settings. Sci Rep. 2021;1(1):3372.
Nabovati E, TaherZadeh Z, Eslami S, Abu-Hanna A, Abbasi R. Antibiotic prescribing in inpatient and outpatient settings in Iran: a systematic review and meta-analysis study. Antimicrob Resist Infect Control. 2021;10(1):15.
Blaak H, Lynch G, Italiaander R, Hamidjaja RA, Schets FM, de Roda Husman AM. Multidrug-resistant and extended spectrum beta-lactamase-producing Escherichia coli in Dutch surface water and wastewater. PLoS ONE. 2015;10(6):e0127752.
Dehghanzadeh Reihani R, Roshani M, Farshchian M. Determination of antibiotic resistance spectrum in Enterobacteriaceae and Staphylococcus bacteria Isolated from hospital wastewaters in Tabriz, 2015. Med J Tabriz Uni Med Sciences Health Services. 2018;40(4):24–30.
Hadi M, Shokoohi R, Ebrahimzadeh Namvar A, Karimi M, Solaimany AM. Antibiotic resistance of isolated bacteria from urban and hospital wastewaters in Hamadan city. Iran J Health Environ. 2011;4(1):105–14.
Cai L, Ju F, Zhang T. Tracking human sewage microbiome in a municipal wastewater treatment plant. Appl Microbiol Biotechnol. 2014;98(7):3317–26.
Habibzadeh N, Peeri Doghaheh H, Manouchehri Far M, Alimohammadi Asl H, Iranpour S, Arzanlou M. Fecal carriage of extended-spectrum β-lactamases and pAmpC producing Enterobacterales in an Iranian community: Prevalence, risk factors, molecular epidemiology, and antibiotic resistance. Microb Drug Resist. 2022;28(9):921–34.
Stoppe NC, Silva JS, Carlos C, Saraiva AM, Ottoboni LMM, et al. Worldwide phylogenetic group patterns of Escherichia coli from commensal human and wastewater treatment plant isolates. Front Microbiol. 2017;8:2512.
Aalipour F, Mirlohi M, Jalali M. Determination of antibiotic consumption index for animal originated foods produced in animal husbandry in Iran, 2010. J Environ Health Sci Eng. 2014;12(1):42.
Akya A, Chegenelorestani R, Elahi A, Hamzavi Y. Frequency of plasmid-mediated quinolone resistance genes in extended-spectum β-lactamase-producing Escherichia coli. J Mazandaran Univ Med Sci. 2017;27(151):41–51.
Butzler JP. Campylobacter, from obscurity to celebrity. Clin Microbiol Infect. 2004;10(10):868–76.
Naraghi B, Afsharnia M, Mardaneh J, Kianmehr M, Biglari H, Bazeli J, et al. Pathogenesis traits and antimicrobial resistance pattern in Escherichia coli isolates recovered from sewage. Crescent J Med Biol Sci. 2020; 7(4).
Ghadiri K, Akya A, Elahi A, Jafari S, Chegenelorestani R. Evaluation of resistance to ciprofloxacin and identification of mutations in topoisomerase genes in Escherichia coli and Klebsiella pneumonia isolated from pediatric urinary tract infections. J Pediatr Res. 2019;6(4):322–8.
Abou El-Khier NT, El Sayed ZM. Molecular detection and frequency of fluoroquinolone-resistant Escherichia coli by multiplex allele specific polymerase chain reaction (MAS-PCR). Egypt J Basic Appl Sci. 2020;7(1):1–7.
Jazeela K, Chakraborty G, Seetharam Shetty SH, Rohit A, Vijaya Kumar D. Comparison of mismatch amplification mutation assay PCR and PCR-restriction fragment length polymorphism for detection of major mutations in gyrA and parC of Escherichia coli associated with fluoroquinolone resistance. Microb Drug Resist. 2019;25(1):23–31.
Liu B-T, Liao X-P, Yang S-S, Wang X-M, Li L-L, Sun J, et al. Detection of mutations in the gyrA and parC genes in Escherichia coli isolates carrying plasmid-mediated quinolone resistance genes from diseased food-producing animals. J Med Microbiol. 2012;61(Pt 11):1591–9.
Röderova M, Halova D, Papousek I, Dolejska M, Masarikova M, Hanulik V, et al. Characteristics of quinolone resistance in Escherichia coli isolates from humans, animals, and the environment in the Czech Republic. Front Microbiol. 2016;7:2147.
Sung J. Analysis of quinolone resistance determinants in Escherichia coli isolated from clinical specimens and livestock feces. Korean J Clin Lab Sci. 2018;50:422–30.
Mirzaii M, Jamshidi S, Zamanzadeh M, Marashifard M, Malek Hosseini SAA, Haeili M, et al. Determination of gyrA and parC mutations and prevalence of plasmid-mediated quinolone resistance genes in Escherichia coli and Klebsiella pneumoniae isolated from patients with urinary tract infection in Iran. J Glob Antimicrob Resist. 2018;13:197–200.
Hajihasani A, Ebrahimi-Rad M, Rasoulinasab M, Mehdi Aslani M, Shahcheraghi F. The molecular characterization and risk factors of ST131 and non-ST131 Escherichia coli in healthy fecal carriers in Tehran. Iran Jundishapur J Microbiol. 2022;15(5):e122468.
Azargun R, Soroush Barhaghi MH, Samadi Kafil H, Ahangar Oskouee M, Sadeghi V, Memar MY, et al. Frequency of DNA gyrase and topoisomerase IV mutations and plasmid-mediated quinolone resistance genes among Escherichia coli and Klebsiella pneumoniae isolated from urinary tract infections in Azerbaijan. Iran J Glob Antimicrob Resist. 2019;17:39–43.
Anssour L, Messai Y, Estepa V, Torres C, Bakour R. Characteristics of ciprofloxacin-resistant Enterobacteriaceae isolates recovered from wastewater of an Algerian hospital. J Infect Dev Ctries. 2016;10(7):728–34.
Moon DC, Seol SY, Gurung M, Jin JS, Choi CH, Kim J, et al. Emergence of a new mutation and its accumulation in the topoisomerase IV gene confers high levels of resistance to fluoroquinolones in Escherichia coli isolates. Int J Antimicrob Agents. 2010;35(1):76–9.
Sorlozano A, Gutierrez J, Jimenez A, de Dios LJ, Martínez JL. Contribution of a new mutation in parE to quinolone resistance in extended-spectrum-beta-lactamase-producing Escherichia coli isolates. J Clin Microbiol. 2007;45(8):2740–2.
Yang F, Zhang SH, Shang X, Wang L, Li H, Wang X. Characteristics of quinolone-resistant Escherichia coli isolated from bovine mastitis in China. J Dairy Sci. 2018;101(7):6244–52.
Zurfluh K, Abgottspon H, Hächler H, Nüesch-Inderbinen M, Stephan R. Quinolone resistance mechanisms among extended-spectrum beta-lactamase (ESBL) producing Escherichia coli isolated from rivers and lakes in Switzerland. PLoS ONE. 2014;9(4):e95864.
Yanat B, Rodríguez-Martínez JM, Touati A. Plasmid-mediated quinolone resistance in Enterobacteriaceae: a systematic review with a focus on Mediterranean countries. Eur J Clin Microbiol Infect Dis. 2017;36(3):421–35.
Sana F, Mabrouka S, Claudine Q, Faouzi SA, Boubaker Ilhem BB, Véronique D. Prevalence and characterization of uropathogenic Escherichia coli harboring plasmid-mediated quinolone resistance in a Tunisian university hospital. Diagn Microbiol Infect Dis. 2014;79(2):247–51.
Jacoby GA, Strahilevitz J, Hooper DC. Plasmid-mediated quinolone resistance. Microbiol Spectr. 2014; 2(5).
Al-Agamy MH, Aljallal A, Radwan HH, Hibl AM. Characterization of carbapenemases, ESBLs, and plasmid-mediated quinolone determinants in carbapenem-insensitive Escherichia coli and Klebsiella pneumoniae in Riyadh hospitals. J Infect Public Health. 2018;11(1):64–8.
Moumouni A, Diagbouga S, Nadembèga C, Dabire AM, Salah F, Obiri-Yeboah D, et al. Quinolone resistance (qnr) genes in fecal carriage of extended spectrum beta-lactamases producing Enterobacteria isolated from children in Niger. Curr Res Microbiol Biotechnol. 2017;5:953–7.
Rezazadeh M, Baghchesaraei H, Peymani A. Plasmid-mediated quinolone-resistance (qnr) genes in clinical isolates of Escherichia coli collected from several hospitals of Qazvin and Zanjan provinces. Iran Osong Public Health Res Perspect. 2016;7(5):307–12.
Zhao J, Chen Z, Chen S, Deng Y, Liu Y, Tian W, et al. Prevalence and dissemination of oqxAB in Escherichia coli isolates from animals, farmworkers, and the environment. Antimicrob Agents Chemother. 2010;54(10):4219–24.
Khalil M, Elsherif R, Ghaith D, Ismail DK, Mohamed S, Jastaniah S, et al. Quinolone resistance detection by PCR-RFLP and Multiplex-PCspectrum extended-spectrum β- lactamase producing Enterobacteriaceae. Int J Clin Med Microbiol. 2017;2:119.
Clermont O, Christenson JK, Denamur E, Gordon DM. The Clermont Escherichia coli phylo-typing method revisited: improvement of specificity and detection of new phylo-groups. Environ Microbiol Rep. 2013;5(1):58–65.
Gordon DM, Cowling A. The distribution and genetic structure of Escherichia coli in Australian vertebrates: host and geographic effects. Microbiology. 2003;149(Pt 12):3575–86.
Nojoomi F, Ghasemian A. The relation of phylogroups, serogroups, virulence factors and resistance pattern of Escherichia coli isolated from children with septicemia. New Microbes New Infect. 2019;29: 100517.
EPA Wastewater sampling. Number: SESDPROC-306-R3. (February 28, 2013)
Mahon CR, Lehman DC. Textbook of diagnostic microbiology. 6th ed. Philadelphia, PA: Saunders; 2018.
Schwalbe R, Steele-Moore L, Goodwin AC. Antimicrobial susceptibility testing protocols. London, England: CRC Press; 2007.
Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. In: CLSI (32Ed.), 2022. CLSI Standard M07, 11th ed. Wayne, PA, Clinical and Laboratory Standards Institute.
Khademi F, Maarofi K, Arzanlou M, Peeri-Dogaheh H, Sahebkar A. Which missense mutations associated with DNA gyrase and topoisomerase IV are involved in Pseudomonas aeruginosa clinical isolates resistance to ciprofloxacin in Ardabil? Gene Rep. 2021;24:101211.
Buruk CK, Ocak HO, Bayramoğlu G. Aydın F.Investigation of plasmid-mediated quinolone resistance genes in quinolone-resistant Escherichia coli and Klebsiella spp. isolates from bloodstream infections. Mikrobiyol Bul. 2016;50(2):186–95.
Hamed SM, Aboshanab KMA, El-Mahallawy HA, Helmy MM, Ashour MS, Elkhatib WF. Plasmid-mediated quinolone resistance in gram-negative pathogens isolated from cancer patients in Egypt. Microb Drug Resist. 2018;24(9):1316–25.
Helaly GF, Abou Shleib H, Fanaki NH, Kader OA, Ali GH. Potential co-prevalence of plasmid-mediated quinolone resistance determinant qepA and 16S rRNA methylase rmtB among E.coli clinical isolates from Alexandria- Egypt. J Egypt Public Health Assoc. 2010;85(5–6):247–72.
Acknowledgements
The authors wish to thank Dr. Sohrab Iranpour (Ardabil University of Medical Sciences, Iran) for his help in statistical analysis.
Funding
The present study was financially supported by the vice-chancellor of research and technology of Ardabil University of Medical Sciences, Ardabil, Iran.
Author information
Authors and Affiliations
Contributions
ZN: Methodology, Investigation, Formal analysis, and Original draft preparation. FK: Conceptualization, Review, and Editing RT: Investigation and Formal Analysis MA: Formal analysis, Review, and Editing MA: Supervision and Project administration.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All experimental protocols in this study were approved by the regional ethics committee of the Ardabil University of Medical Sciences under the reference “IR.ARUMS.REC.1399.553”. All methods were carried out in accordance with relevant guidelines and regulations. Clinical isolates were obtained from the bacterial collection of the hospital for research purposes and no patient samples or data were used in this study. In order to collect samples from healthy children, informed consent was obtained from their parents or legal guardians. To collect the wastewater samples, permissions were obtained from Ardabil Water and Wastewater Company for municipal wastewater treatment plant and Ardabil provincial Veterinary Organization office for poultry and livestock slaughterhouse wastewater treatment plants.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Neyestani, Z., Khademi, F., Teimourpour, R. et al. Prevalence and mechanisms of ciprofloxacin resistance in Escherichia coli isolated from hospitalized patients, healthy carriers, and wastewaters in Iran. BMC Microbiol 23, 191 (2023). https://doi.org/10.1186/s12866-023-02940-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-023-02940-8