Abstract
Background
SARS-CoV-2 is a novel coronavirus first recognized in late December 2019 that causes coronavirus disease 19 (COVID-19). Due to the highly contagious nature of SARS-CoV-2, it has developed into a global pandemic in just a few months. Antibody testing is an effective method to supplement the diagnosis of COVID-19. However, multicentre studies are lacking to support the understanding of the seroprevalence and kinetics of SARS-CoV-2 antibodies in COVID-19 epidemic regions.
Method
A multicentre cross-sectional study of suspected and confirmed patients from 4 epidemic cities in China and a cohort study of consecutive follow-up patients were conducted from 29/01/2020 to 12/03/2020. IgM and IgG antibodies elicited by SARS-CoV-2 were tested by a chemiluminescence assay. Clinical information, including basic demographic data, clinical classification, and time interval from onset to sampling, was collected from each centre.
Results
A total of 571 patients were enrolled in the cross-sectional study, including 235 COVID-19 patients and 336 suspected patients, each with 91.9%:2.1% seroprevalence of SARS-CoV-2 IgG and 92.3%:5.4% seroprevalence of SARS-CoV-2 IgM. The seroprevalence of SARS-CoV-2 IgM and IgG in COVID-19 patients was over 70% less than 7 days after symptom onset. Thirty COVID-19 patients were enrolled in the cohort study and followed up for 20 days. The peak concentrations of IgM and IgG were reached on the 10th and 20th days, respectively, after symptom onset. The seroprevalence of COVID-19 IgG and IgM increased along with the clinical classification and treatment time delay.
Conclusion
We demonstrated the kinetics of IgM and IgG SARS-CoV-2 antibodies in COVID-19 patients and the association between clinical classification and antibodies, which will contribute to the interpretation of IgM and IgG SARS-CoV-2 antibody tests and in predicting the outcomes of patients with COVID-19.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) has caused a great pandemic worldwide. As of October 12,020, more than 3 billion cases had been diagnosed with COVID-19, and the mortality rate was about 3.0% according to World Health Organization (WHO) reports. The challenges of this epidemics include treatment, avoiding viral transmission. The Chinese diagnostic and therapeutic guidelines of COVID-19 have been updated 7 times [1]. More detailed information on COVID-19 has been uncovered by clinical and basic research.
One of the dilemmas in the treatment of COVID-19 is the relatively high rate of false-negative results using nucleic acid tests as the diagnostic method. The reasons for this include several aspects, including a low viral concentration in the upper respiratory tract, unstandardized sample collection methods, various gene application performances, and a decrease in viral load one week after disease onset [2, 3].
Since an immune reaction is involved in COVID-19 progression, serological assays have been developed and put into practice in many countries [4]. Antibody tests have been confirmed as a good supplement for nucleic acid tests. They can be used as an immunity passport or proof of a previous infection, an asymptomatic infection or immunization. However, there are still many challenges and knowledge gaps in the clinical applications of antibodies in COVID-19 [5]. including the performances of various SARS-CoV-2 antibody products, the variable prevalences of antibodies in different regions, and the interpretation of positive results in various clinical stages. Previous studies on SARS-CoV-2 antibody tests in China were mostly conducted in a single centre or restricted to one province. Our study collected data from four epidemic cities during the outbreak stage of COVID-19 in China to better understand the significance of SARS-CoV-2 serological tests.
Methods
Patients and data collection
This study consists of a cross-sectional study and a cohort study. 235 confirmed COVID-19 patients and 336 suspected COVID-19 patients were identified in this multicentre study from Peking Union Medical College Hospital, Tianjin Haihe Hospital, the Fifth Hospital of Shijiazhuang, and Zhongnan Hospital of Wuhan University from 29/01/2020 to 12/03/2020. SARS-CoV-2 infection was confirmed by two repeated positive results from the local hospital using commercial RT-PCR kits for nasal and pharyngeal swab specimens. The suspected cases were defined as clinical manifestations, chest radiography imaging, and history of contacting COVID-19 confirmed patients. These suspected patients must have negative nucleic acid tests and the second test must be tested 1 day after the first negative nucleic acid test results. All patients were enrolled in the cross-sectional study. 30 patients in Tianjin were included in the cohort study to investigate the dynamic changes in IgM and IgG concentrations. All clinical data were retrieved from the Laboratory Information System and Hospital Information System from each centre. The ethics committee of Peking Union Medical College Hospital approved this study and waived informed consents for the usage of the remaining clinical samples (ZS-2303).
Measurements
The remaining serum or plasma samples of included patients were collected after routine clinical tests. IgM and IgG antibodies elicited by SARS-CoV-2 in plasma and serum were tested immediately after sample collection by a chemiluminescence assay (CLIA, Lot Number: 20200127) developed by Beier Bioengineering Company (Beijing, China, http://www.beierbio.com/en/Default.aspx). The IgM antibody test was based on a μ-chain capture immunoassay, and the IgG antibody was detected by indirect immunoassays. Recombinant antigen-containing receptor-binding domain (RBD) of the SARS-CoV-2 spike protein and nucleocapsid (N) proteins were used to develop the IgM and IgG antibody assays. Horseradish peroxidase-conjugated mouse against human IgM/IgG antibody was used as the detection antibody. Both IgM and IgG tests were performed on an automatic chemiluminescence analyser (VI-200, Beier, Beijing, China) according to the manufacturer’s instructions. Cut-off values of IgM and IgG were 8 AU/ml. We clarify all methods used in our study comply with institutional, national, or international guidelines.
Statistical analysis
Results were analysed using SPSS version 12.0 (SAS Institute, Cary, NC, USA). Continuous variables were expressed as mean with standard deviation for normally distributed data and the median with interquartile range (IQR) for skewed distribution data. Categorical variables are expressed as numbers (%). Kruskal-Wallis tests for continuous variables and chi-square tests for categorical variables were used for comparisons between groups. Patients were classified as light, regular, severe, and critical according to the Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment (7th edition). They were stratified according to the time from disease onset to sampling into three groups: ≤7 days, 8–15 days, and > 15 days. Seroprevalence was defined as the proportion of patients with positive antibody results in the study. P < 0.05 was considered statistically significant. In the cohort study, the mean concentration of SARS-Cov-2 IgG and IgM were plotted with the time interval from disease onset to sampling.
Results
Baseline characteristics
A total of 571 patients were enrolled in this study, of which 144 patients were from Beijing, 147 patients were from Tianjin, 29 patients were from Wuhan, and 241 were from Shijiazhuang. The baseline characteristics of the 235 COVID-19 patients and 336 suspected patients are summarised in Table 1. The average interval from symptom onset to COVID-19 testing in patients in Wuhan was 20.9 days, which was longer than that at other study sites, while the time interval in Beijing was the shortest at 3.3 days. Suspected patients in Beijing and Tianjin were generally older than the confirmed COVID-19 patients. However, suspected patients in all hospitals was younger than that of the confirmed COVID-19 patients for patients from Shijiazhuang. There were relatively more male patients in this study. 216 (91.9%) and 217 (92.3%) were IgG positive and IgM positive in COVID-19 patients, respectively. In 336 suspected patients, 7 (2.1%) tested IgG positive, and 18 (5.4%) tested IgM positive.
Antibodies concentration
Antibody concentrations stratified by clinical classification
Forty-one COVID-19 patients with clinical classification information from Beijing and Wuhan were analysed. Characteristics of these patients are shown in Table 2. Although there was only one patient with very mild symptoms, there was an increase in median age, concentration, and positive rate of IgG and IgM with aggravation of the illness.
Comparison of SARS-Cov-2 IgG and IgM level in COVID-19 patients between regions and symptom onset intervals
We collected the time interval from symptom onset to sampling in all COVID-19 patients in the cross-sectional study. The SARS-Cov-2 IgG- and IgM-positive rates stratified by the time interval are shown in Fig. 1a. The positive rate gradually increased with the increase in testing time interval from symptom onset. The positive rate of SARS-Cov-2 IgG was close to 100% at > 15 days. Figure 1b and c shows the median concentrations of SARS-Cov-2 IgG and IgM in various regions. The concentrations of SARS-Cov-2 IgG and IgM rose after 7 days of onset in all hospitals. The concentrations of SARS-Cov-2 IgM in patients from Wuhan and IgG in patients from Tianjin ascended distinctively step by step along with the time intervals.
The seroprevalence and concentration comparison of COVID-19 IgG and IgM in diagnosed patients stratified by region and symptom onset interval. a The seroprevalence of COVID-19 IgG and IgM stratified by symptom onset interval. b The seroprevalence of COVID-19 IgM stratified by symptom onset interval and region. c The seroprevalence of COVID-19 IgG stratified by symptom onset interval and region
The dynamic characteristics of SARS-Cov-2 IgM and IgG in the cohort study
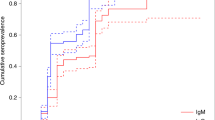
The dynamic changes in SARS-Cov-2 IgM and IgG concentrations over time were investigated in 30 COVID-19 patients from Tianjin. The dynamic change of SARS-Cov-2 IgM and IgG are shown in Fig. 2. The concentration of SARS-Cov-2 IgM was higher than that of IgG before the 15th day after symptom onset. The concentration of SARS-Cov-2 IgG was higher than that of IgM after 15th day since symptom onset. The SARS-Cov-2 IgM concentration reached a peak on the 10th day after symptom onset and then decreased slowly. The concentration of SARS-Cov-2 IgG on the 20th day continued to increase.
Discussion
This is the first multicentre study of antibodies against SARS-COV-2 from four outbreak areas in China. We found a good clinical coincidence rate of the antibody tests, an association between the clinical classification and the concentration of antibodies, and the kinetics of the antibodies, which could improve our understanding in the immune response after patients are infected with SARS-CoV-2. In this study, we investigated the seroprevalence of SARS-Cov-2 IgG and IgM as well as the kinetics of the antibody response in COVID-19 from four epidemic regions of China in early 2020 [6]. In the cross-sectional study, 91.9 and 92.3% of patients with confirmed SARS-CoV-2 infection tested IgG and IgM positive, respectively. 2.1% of 336 suspected patients tested IgG positive, and 5.4% tested IgM positive. In the cohort study, the peaks of IgM and IgG were reached on the 10th and 20th days, respectively, after symptom onset. The seroprevalence of SARS-CoV-2 IgG and IgM increased along with the clinical classification and treatment time delay.
There has been an urgent need for novel in-vitro diagnostic products. The sensitivity and specificity of these products ranged 88–100% and 75–100%, respectively [7,8,9]. Sensitive and stable CLIA was used as a measurement method in our study. Figure 1a shows that the positive antibody rate increased along with the symptom onset intervals. The seroprevalence of SARS-CoV-2 IgM and IgG on ≤7 days since onset of symptoms were 81 and 83%, respectively. The seroprevalence of both antibodies raised to 95% at 2 weeks since symptom onset [10].
Approximately 8% of COVID-19 patients tested negative for IgM or IgG. We speculated three explanations which might contribute to the negative results for confirmed COVID-19 patients. First, the heterogeneity of testing times from the onset of the disease are an important factor [11, 12]. Previous study showed that antibodies elicited by SARS-CoV-2 develop three days after symptom onset or one week after infection with SARS-CoV-2 [13]. In our study, the average time interval from onset to sampling was 3 days in Beijing, followed by Tianjin, Shijiazhuang, and Wuhan in an increasing order of average time interval (Table 1). Therefore, the seroprevalences of IgM and IgG antibodies in Shijiazhuang and Tianjin were higher than those in Beijing and Wuhan. Therefore, antibody testing during the window phase of COVID-19 progression could lead to false-negative results [14, 15]. Secondly, individual differences in the immune response are also a contributing factor. Some COVID-19 patients were negative for SARS-CoV-2 IgM and IgG from onset to recovery [16], which indicates that innate immunity could clear the virus without adaptive immunity and these patients might not produce detectable antibodies against SARS-CoV-2 [15, 16]. Additionally, the sample size of COVID-19 patients was limited in Beijing and Wuhan, which might lead to underestimation of the seroprevalence [17].
On the other hand, 2.1 and 5.4% of patients were found SARS-CoV-2 IgG and IgM positive in suspected patients. Many causes of false-positive results have been reported, including autoimmune disease, cancer, drug usage, and other infections [18, 19]. Therefore, antibody tests are recommended in combination with nucleic acid tests for the diagnosis and treatment of COVID-19.
The association of SARS-CoV-2 antibody concentration, positive rate, and clinical stage was explored in our study. Although there was no statistical significance due to limited number of patients included in this study, SARS-CoV-2 IgM and IgG antibody concentrations and positive rates in severe cases were distinctively higher than those in milder cases (Table 2). Our study further confirmed the findings from the previous study. Long et al. and Qu et al. indicated that critical COVID-19 patients had higher IgM and IgG antibody responses than non-critical patients [20, 21] due to a high level of viral load or inflammatory storm in severe or critical cases [22]. In addition, we found that the mean ages of COVID-19 patients with severe cases were older than those with milder cases, although the difference was not statistically significant. Many studies have reported that patients who died were generally older than survivors in critical cases of COVID-19 [23,24,25], especially among patients with comorbid diseases, including hypertension, coronary artery disease, and diabetes [25, 26]. Age is one of the risk factors for susceptibility and poor prognosis of COVID-19 [27].
The kinetics of SARS-CoV-2 IgM and IgG in COVID-19 patients are shown in Fig. 2. The IgM antibody concentration reached a peak 10 days earlier than the IgG antibody concentration. The SARS-CoV-2 IgG antibodies maintained an upward trend after 20 days. Andrea et al. reported that IgM antibody levels peaked at 10–12 days and significantly declined after 18 days [28] which was similar to our study. IgG against COVID-19 has been reported to persist over seven weeks [11]. Some studies showed that COVID-19 patients with high IgG titres might produce neutralizing antibody activity, clearing the virus [29, 30]. Wang et al. reported a moderate correlation between anti–SARS-CoV-2 spike protein IgG levels and neutralization titres in COVID-19 patient plasma [5]. In contrast, some studies observed higher levels of anti-RBD IgG antibodies from COVID-19 patients that did not contribute to neutralization. They suggest that anti-RBD IgM and IgA also contribute to neutralization [31, 32]. Since the virus-neutralizing antibody titre was determined by the virus infection inhibition rate, the content of neutralizing antibodies in the serum was found to be complex and is being recognized gradually [33]. The detection antibodies in commercial reagents usually target spike and/or nucleocapsid proteins and may not distinguish among different immunogenic regions of the spike protein of SARS-CoV-2 [34]. Therefore, predicting whether serum with positive antibodies is protective or therapeutic should be approached with caution.
Nevertheless, there were some limitations in our study. First, the limited sample size and clinical information in some regions restricted more analysis to perform. Additionally, individuals with asymptomatic SARS-CoV-2 infection were not included in our studies, so information from those patients was lacking.
In conclusion, we demonstrated the seroprevalence of SARS-CoV-2 IgM and IgG antibody and antibody titre alterations in COVID-19 patients, which could help in better interpreting the antibody testing results during COVID-19 progression.
References
NHC. Chinese Recommendations for Diagnosis and Treatment of SARS-CoV-2 infection. 2020.03.04 2020. http://www.nhc.gov.cn/xcs/zhengcwj/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml. (Accessed 07.07 2020).
To KK, Tsang OT, Chik-Yan Yip C, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;71(15):841-3.
Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020;20(4):411–2.
Lerner AM, Eisinger RW, Lowy DR, et al. The COVID-19 serology studies workshop: recommendations and challenges. Immunity. 2020;53(1):1-5.
Xu M, Wang D, Wang H, et al. COVID-19 diagnostic testing: technology perspective. Clin Transl Med. 2020;10(4):e158.
Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689–97.
Haselmann V, Kittel M, Gerhards C, et al. Comparison of test performance of commercial anti-SARS-CoV-2 immunoassays in serum and plasma samples. Clin Chim Acta. 2020;510:73–8.
Shaw AM, Hyde C, Merrick B, et al. Real-world evaluation of a novel technology for quantitative simultaneous antibody detection against multiple SARS-CoV-2 antigens in a cohort of patients presenting with COVID-19 syndrome. Analyst. 2020;145(16):5638-46.
GeurtsvanKessel CH, Okba NMA, Igloi Z, et al. An evaluation of COVID-19 serological assays informs future diagnostics and exposure assessment. Nat Commun. 2020;11(1):3436.
Xu X, Sun J, Nie S, et al. Seroprevalence of immunoglobulin M and G antibodies against SARS-CoV-2 in China. Nat Med. 2020;26(8):1193-5.
Sethuraman N, Jeremiah SS, Ryo A. Interpreting diagnostic tests for SARS-CoV-2. Jama. 2020;323(22):2249-51.
Zainol Rashid Z, Othman SN, Abdul Samat MN, Ali UK, Wong KK. Diagnostic performance of COVID-19 serology assays. Malaysian J Pathol. 2020;42(1):13–21.
Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–82.
Lou B, Li TD, Zheng SF, et al. Serology characteristics of SARS-CoV-2 infection after exposure and post-symptom onset. Eur Respir J. 2020;56(2):2000763.
Younes N, Al-Sadeq DW, Al-Jighefee H, et al. Challenges in Laboratory Diagnosis of the Novel Coronavirus SARS-CoV-2. Viruses. 2020;12(6):582.
Wang B, Wang L, Kong X, et al. Long-term coexistence of SARS-CoV-2 with antibody response in COVID-19 patients. J Med Virol. 2020;92(9):1684-9.
Freiman JA, Chalmers TC, Smith H Jr, Kuebler RR. The importance of beta, the type II error and sample size in the design and interpretation of the randomized control trial. Survey of 71 "negative" trials. N Engl J Med. 1978;299(13):690–4.
Li Z, Yi Y, Luo X, et al. Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-CoV-2 infection diagnosis. J Med Virol. 2020;92(9):1518-24.
Deeks JJ, Dinnes J, Takwoingi Y, et al. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst Rev. 2020;6:Cd013652.
Long QX, Liu BZ, Deng HJ, et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat Med. 2020;26(6):845–8.
Qu J, Wu C, Li X, et al. Profile of IgG and IgM antibodies against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clin Infect Dis. 2020;71(16):2255-8.
Yongchen Z, Shen H, Wang X, et al. Different longitudinal patterns of nucleic acid and serology testing results based on disease severity of COVID-19 patients. Emerg Microbes Infect. 2020;9(1):833–6.
Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.
Zhang P, Zhu L, Cai J, et al. Association of Inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020;126(12):1671–81.
Davies NG, Klepac P, Liu Y, Prem K, Jit M, Eggo RM. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020;26(8):1205-11.
Padoan A, Sciacovelli L, Basso D, et al. IgA-Ab response to spike glycoprotein of SARS-CoV-2 in patients with COVID-19: A longitudinal study. Clin Chim Acta. 2020;507:164–6.
Perera RA, Mok CK, Tsang OT, et al. Serological assays for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), March 2020. Euro Surveill. 2020;25(16):2000421.
To KK, Tsang OT, Leung WS, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20(5):565–74.
Garcia-Beltran WF, Lam EC, Astudillo MG, et al. COVID-19 neutralizing antibodies predict disease severity and survival. Cell. 2021;184(2):476-88.
Zhao J, Yuan Q, Wang H, et al. Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. Clin Infect Dis. 2020;71(16):2027-34.
Barnes CO, Jette CA, Abernathy ME, et al. SARS-CoV-2 neutralizing antibody structures inform therapeutic strategies. Nature. 2020;588:682-7.
Huo J, Le Bas A, Ruza RR, et al. Neutralizing nanobodies bind SARS-CoV-2 spike RBD and block interaction with ACE2. Nat Struct Mol Biol. 2020;27(9):846–54.
Acknowledgements
The manufacturer provided equipment and reagents for this study but had no role in directing the study or influencing the study outcomes.
Declarations
We declare that the authors have no competing interests as defined by BMC, or other interests that might be perceived to influence the results and/or discussion reported in this paper. The results/data/figures in this manuscript have not been published elsewhere, nor are they under consideration. All materials are owned by the authors and/or no permissions are required. We are responsible for the submission of this article and accept the conditions of submission and the BMC Copyright and License Agreement.
Funding
This research was supported by grants from the CAMS Innovation Fund for Medical Sciences (CIFMS) (2020-I2M-CoV19–001, 2017-I2M-3-001, and 2017-I2M-B&R-01) and the National Natural Science Foundation of China Grants (81671618, 81871302).
Author information
Authors and Affiliations
Contributions
XZ Q and HL L wrote the draft; JS, DE H, GD T, LX Z and PJ conducted the research in branch center; XH, MY L, XW, DS M and JJ Z conducted the research in core center and revised the draft; MF T helped revised the draft; YZ L assigned the study. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Peking Union Medical College Hospital (ZS-2303).
Consent for publication
Informed consent was waived for the use in this study of the remaining samples left after diagnosis.
Competing interests
The authors state no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qin, X., Shen, J., Dai, E. et al. The seroprevalence and kinetics of IgM and IgG in the progression of COVID-19. BMC Immunol 22, 14 (2021). https://doi.org/10.1186/s12865-021-00404-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12865-021-00404-0