Abstract
Background
Peutz-Jeghers syndrome is an autosomal dominant disease characterized by mucocutaneous pigmentation and hamartomatous polyps in the gastrointestinal tract (GIT). There have also been cases of extra GIT polyps such as the renal pelvis, urinary bladder, lungs and nares. Bladder hamartoma is an extremely rare finding, with only 12 cases described in the literature up to now. The rarity of the condition necessitates a comprehensive compilation of managements up to now so as to provide a better tool for the treatment of such conditions in the future.
Case presentation
A twenty-year-old male, known to have Peutz-Jeghers syndrome, presented to us complaining of obstructive urinary symptoms. A urethrogram done showed a filling defect at the base of the urinary bladder. The mass was resected transurethrally, and histopathology revealed a hamartoma of the bladder. The patient has since remained tumor-free on follow-up.
Conclusions
Transurethral resection of the bladder mass proved to be an effective therapy in this patient with no recurrence on the patient’s follow-up till now. There is still, however, a dearth of knowledge regarding the management of bladder hamartomas owing to the extreme rarity of the case.
Similar content being viewed by others
1 Background
Hamartoma of the urinary bladder is an unusual and very rare type of tumor. Only 12 such cases have been reported up to now. It is made up of a mixture of tissues resembling cystitis cystica, cystitis glandularis and von Brunn’s nests. The stroma may be edematous, fibrous or muscular. The 12 reported cases all had varying modes of presentation, which are documented in Table 1. However, a thorough search of literature was not fruitful in finding any diagnostic criteria of PJS in the urinary tract. It is generally benign after excision, and almost no recurrences have been reported. The mass can be identified by conventional imaging methods such as an ultrasound, an excretory urography or even a computed tomography (CT) scan; however, the final diagnosis is always histopathologic.
2 Case presentation
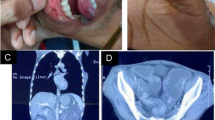
A 20-year-old man with no reported co-morbids, previously known to have Peutz-Jeghers syndrome, was presented in our outpatient department with lower urinary tract symptoms (LUTS) for 3 months, which included straining on voiding, intermittency, urgency, and urge incontinence. He did not complain of any hesitancy, sense of incomplete emptying of the bladder, hematuria or passage of per urethral stone. Patient did not have any sexual history. He did, however, have a positive family history of tuberculosis. (His father had the disease when he was a child and had undergone full treatment course.) He had occasional episodes of diarrhea, owing to his Peutz-Jeghers syndrome (PJS), and normal sleep and appetite. Patient had had an endoscopic polypectomy, to confirm the diagnosis of PJS. He did not have any other significant surgical or medical history. On examination, the patient was of normal average built and height and comfortably lying down. General physical examination revealed hyperpigmented spots in his oral mucosa. There were no other striking features on the general physical examination. His blood biochemistry was within the normal range, whereas the ultrasound of the kidneys and bladder done showed a normal right kidney and a calculus of 5.6 mm in mid-pole calyx of the left kidney causing mild hydronephrosis and a very trabeculated bladder. Pre-void volume was 313 ml, and post-void was 113 ml.
Owing to the fact that the patient had obstructive lower urinary tract symptoms, a urethrogram was done, which showed a filling defect in the region of the bladder neck (Fig. 1). A provisional diagnosis of bladder mass was made, and the patient underwent cystoscopy, which showed multiple polypoidal growths at the neck of the bladder, a single central fibrotic band on the bladder diving the bladder in 2 halves and normal ureteric orifices. The polyps were resected transurethrally, and the specimen was sent for histopathology.. Later, he was followed in consultant clinic, and histopathology revealed a bladder mucosa exhibiting downward growing papillary architecture lined with transitional epithelium, representing a hamartoma of the urinary bladder (Fig. 2). No comment was made on tumor-free surgical margins. Postoperatively, patient was given injection mitomycin 40 mg intravesically, for one hour, since it was assumed at the time that the patient had a bladder tumor and treated as such. The patient was followed with a check cystoscopy, which was negative. He is scheduled to be followed with a check cystoscopy every 3 months to check for recurrence.
3 Discussion
PJS is a rare hereditary disorder, which is characterized by hamartomatous polyps in the gastrointestinal tract and typical pigment lesions [1]. Cases of extraintestinal polyps have been rarely reported in the literature. Possible sites of these polyps include the respiratory tract, urogenital tract [2, 3] and gallbladder [4]. There have also been general concerns regarding the malignant potential of the PJS, namely the LKB1 germline mutations [5]. Although a hamartoma is a benign condition, the diagnosis is only made after histopathology, and keeping in mind the malignant potential of hamartomas of the intestinal tract [6], a swift removal and biopsy of the bladder mass were needed.
The pathological definition of a hamartoma, irrespective of site of origin, is an abnormal proliferation of tissue indigenous to the organ to create a mass or tumor [7]. They can occur in a multitude of organs, including the spleen, liver, kidney and the lungs. They are, however, extremely rare in the urinary bladder [8, 9]. Since the first case reported by Davis in 1949 [10], only twelve cases (Table 1), to the best of our knowledge, have been reported in the literature up to now [11, 12], with only one case found in the literature associated with PJS [13]. Most cases tend to occur near to the trigone [8, 9], while the mass in our case was at the bladder neck. The patients can present with hematuria, pyuria, suprapubic discomfort [12] and now even obstructive LUTS.
Many treatment options have been suggested for such a lesion, but a transurethral resection (TUR) or even a partial cystectomy is the method which has been used in the literature [8]. There has been no evidence up to now that isolated bladder hamartomas, including invasive hamartomas, have any tendency for recurrence or malignant potential after partial cystectomy. With the rarity of the lesion, they set guidelines for the follow-up schedule of such patients. As such, certain reported cases have advocated cystoscopy to be done every three months for a year, then yearly for four years [13], a follow-up examination ranging from four months to five years [14], or simply a long-term periodic cystoscopy as surveillance—since the malignant potential of these lesions is as such unknown [11]. Our patient has had only one check cystoscopy done 3 months after the resection, and no growths were seen on check cysto. It is also worthwhile to mention that the patient received mitomycin 40 mg intravesically after his TURBT since he was thought to have a bladder mass at the time and treated as such.
4 Conclusion
Transurethral resection of the bladder mass, followed by intravesical mitomycin, proved to be an effective therapy in this patient with no recurrence on the patient’s follow-up till now. Follow-up regimens have been varied in different cases, but with the unknown potential of the lesion, with only 13 cases reported, there is still, however, a dearth of knowledge regarding the management of bladder hamartomas owing to the extreme rarity of the case and, as such, is being followed up very stringently every 3 months.
Availability of data and materials
All the data published in this article have been taken from public and have been duly referenced
Abbreviations
- PJS:
-
Peutz-Jeghers syndrome
- CT:
-
Computed tomography
- LUTS:
-
Lower urinary tract symptoms
- TUR:
-
Transurethral resection
References
Peutz J (1921) Very remarkable case of familial polyposis of mucous membrane of intestinal tract and nasopharynx accompanied by peculiar pigmentation of skin and mucous membrane. Ned Maandschr Geneeskd 10:134–146
Keating MA, Young RH, Lillehei CW, Retik AB (1987) Hamartoma of the bladder in a 4-year-old girl with hamartomatous polyps of the gastrointestinal tract. J Urol 138(2):366–369. https://doi.org/10.1016/S0022-5347(17)43148-X
Dormandy TL (1957) Gastrointestinal polyposis with mucocutaneous pigmentation (Peutz–Jeghers syndrome). N Engl J Med 256(25):1186–1190. https://doi.org/10.1056/NEJM195706202562506
Foster DR, Foster DB (1980) Gall-bladder polyps in Peutz-Jeghers syndrome. Postgrad Med J 56(655):373–376. https://doi.org/10.1136/pgmj.56.655.373
Jansen M, de Leng WW, Baas AF, Myoshi H, Mathus-Vliegen L, Taketo MM et al (2006) Mucosal prolapse in the pathogenesis of Peutz-Jeghers polyposis. Gut 55(1):1–5. https://doi.org/10.1136/gut.2005.069062
Giardiello FM, Welsh SB, Hamilton SR, Offerhaus GJA, Gittelsohn AM, Booker SV et al (1987) Increased risk of cancer in the Peutz-Jeghers syndrome. N Engl J Med 316(24):1511–1514. https://doi.org/10.1056/NEJM198706113162404
Chinyama CN. Hamartoma. Breast Pathology. 2020:135–43.
Ota T, Kawai K, Hattori K, Uchida K, Akaza H, Harada M (1999) Hamartoma of the urinary bladder. Int J Urol 6(4):211–214. https://doi.org/10.1046/j.1442-2042.1999.06434.x
Brancatelli G, Midiri M, Sparacia G, Martino R, Rizzo G, Lagalla R (1999) Hamartoma of the urinary bladder: case report and review of the literature. Eur Radiol 9(1):42–44
Davis T (1949) Hamartoma of the urinary bladder. Northwest Med 48:182–185
Al Shahwani N, Alnaimi AR, Ammar A, Al-ahdal EM (2016) Hamartoma of the urinary bladder in a 15-year-old boy. Turkish J Urol 42(2):101. https://doi.org/10.5152/tud.2016.45077
Adam A, Gayaparsad K, Engelbrecht MJ, Moshokoa EM (2013) Bladder hamartoma: a unique cause of urinary retention in a child with Goldenhar syndrome
Moose LT, Garvey FK (1963) Hamartoma of the bladder. J Urol 89(2):185–187. https://doi.org/10.1016/S0022-5347(17)64526-9
McCallion W, Herron B, Keane P (1993) Bladder hamartoma. British J Urol (Print) 72(3):382–383
Friedman NB, Ash JE (1959) Tumors of the urinary bladder: Armed Forces Institute of Pathology
Borski A (1970) Hamartoma of the bladder. J Urol 104(5):718–719. https://doi.org/10.1016/S0022-5347(17)61819-6
Keating MA, Young RH, Lillehei Cw, Retik Ab (1987) Hamartoma of the bladder in a 4-year-old girl with hamartomatous polyps of the gastrointestinal tract. J Urol, 138(2):366–9. https://doi.org/https://doi.org/10.1016/S0022-5347(17)43148-X
Williams Ml, Ibrahim S, Rickwood AK (1990) Hamartoma of the urinary bladder in an infant with Beckwith-Wiedemann syndrome. British J Urol (Print), 65(1): 106–7
Duvenage G, Dreyer L, Reif S, Bornman M, Steinmann C (1997) Bladder hamartoma. Br J Urol 79(1):133–134. https://doi.org/10.1046/j.1464-410X.1997.128832.x
Pieretti A, Wu C-L, Pieretti RV (2014) Bladder Hamartoma in a Fetus: Case Report. Urology Case Rep 2(5):154. https://doi.org/10.1016/j.eucr.2014.06.005
Acknowledgements
Not applicable
Funding
No funding was obtained in this study
Author information
Authors and Affiliations
Contributions
JK prepared the manuscript and interdepartmental coordination. MAI prepared the manuscript and proofreading. NAS edited the manuscript. AHQ is a treating consultant and edited the manuscript. All authors have read and approved the manuscript
Corresponding author
Ethics declarations
Ethics Approval and consent to participate
Due consent taken from patient.
Consent to publish
The patient has agreed to allow the concerned physicians, to report pertinent details of his care in an academic setting or publication, including but not limited to a public conference or academic journal. His name, birthdate or images will not be disclosed in any setting, including radiographical or such images. Informed and written consent was taken from the patient. Details of his care can include my age, laboratory and physical findings, antecedent history, radiographic and histopathologic imaging, course of treatment, therapy and outcomes.
Competing interest
The authors whose names are listed immediately above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kumar, J., Albeerdy, M.I., Shaikh, N.A. et al. Bladder hamartoma in Peutz-Jeghers syndrome: a rare case report. Afr J Urol 27, 74 (2021). https://doi.org/10.1186/s12301-021-00172-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-021-00172-8