Abstract
Background
There are few data on the clinical outcomes of patients with coronavirus disease 2019 (COVID-19) in cities over 1000 m above sea level (masl).
Objectives
To describe the clinical characteristics and mortality of patients with COVID-19 treated at a high complexity hospital in Bogotá, Colombia, at 2640 masl.
Methods
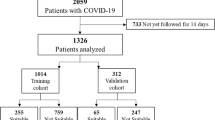
This was an observational study of a cohort including 5161 patients with confirmed COVID-19 infection from 19 March 2020 to 30 April 2021. Demographic data, laboratory values, comorbidities, oxygenation indices, and clinical outcomes were collected. Data were compared between survivors and nonsurvivors. An independent predictive model was performed for mortality and invasive mechanical ventilation (IMV) using classification and regression trees (CART).
Results
The median cohort age was 66 years (interquartile range (IQR) 53–77), with 1305 patients dying (25%) and 3856 surviving (75%). The intensive care unit (ICU) received 1223 patients (24%). Of 898 patients who received IMV, 613 (68%) of them perished. The ratio of partial pressure arterial oxygen (PaO2) to fraction inspired oxygen (FiO2), or the P/F ratio, upon ICU admission was 105 (IQR 77–146) and 137 (IQR 91–199) in the deceased and survivors, respectively. The CART model showed that the need for IMV, age greater than 79 years, ratio of oxygen saturation (SaO2) to FiO2, or the S/F ratio, less than 259, and lactate dehydrogenase (LDH) greater than 617 U/L at admission were associated with a greater probability of death.
Conclusion
Among more than 5000 patients with COVID-19 treated in our hospital, mortality at hospital discharge was 25%. Older age, low S/F ratio, and high LDH at admission were predictors of mortality.
Similar content being viewed by others
Background
Epidemiological data on risk factors and clinical outcomes related to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and the associated clinical entity (i.e. COVID-19) have emerged from all over the world; however, there are limited data on the clinical outcomes of patients with COVID-19 living in cities over 1000 masl.
According to the Wilderness Medicine Society, regions are classified according to altitude as high altitude when they are located at more than 2500 masl [1]. More than 140 million people in the world live above 2500 masl, with this being more frequent in the Latin American Andean region [2]. With higher altitudes come a lower barometric pressure (BP), and the FiO2 remains constant (20.93%) at any altitude. The pressure of inspired oxygen (PiO2) is positively correlated with BP. At sea level (BP = 760 mmHg), the PiO2 is 159.1 mmHg [3], while in Bogotá (2640 masl; BP = 560 mmHg), it is 117.2 mmHg. Lower PiO2 leads to lower alveolar oxygen pressure and PaO2, causing tissue hypoxia [4]. The average PaO2 in Bogotá is 67 mmHg [5]. This phenomenon is known as hypobaric hypoxaemia. Despite this, prolonged exposure to hypobaric hypoxaemia allows adaptation of the respiratory, cardiovascular, haematological, muscular, and microcirculatory systems to optimize the cellular supply and use of oxygen [6].
High altitude has effects on the burdens of chronic diseases. Convincing data from population studies show that living above 2000 masl reduces mortality from coronary heart disease and stroke [7], in addition to the risk of developing obesity and diabetes [8, 9]. It is speculated that, at altitude, cold induces thermogenesis and decreases appetite, and there is an unintentional increase in physical activity and a better tolerance to glucose related to hypoxaemia [10]. Each of these phenomena represents an explanatory mechanism of the inverse relationship between altitude and cardiovascular diseases. These findings are compatible with those reported by Seclén et al. [11] who, in an ecological study, found the incidence and mortality of patients with COVID-19 in 25 Peruvian regions with altitudes between 1 and 3744 masl, finding an inverse relationship between the prevalence of diabetes, obesity, and hypertension with altitude.
It is known that high altitude has varying effects on other respiratory conditions, such as influenza pneumonia and tuberculosis. Influenza pneumonia at high altitude is associated with higher mortality, stating that hypobaric hypoxaemia directly increases the risk of serious disease and requires early treatment with oxygen [12], whereas pulmonary tuberculosis at high altitude shows lower mortality compared to rates at sea level, which is associated with an increase in cellular antimycobacterial immunity [13].
Arias-Reyes et al. [14] raised the hypothesis that living at high altitude can protect against the effects of SARS-CoV-2 infection based on the observation of the low severity and prevalence of COVID-19 in regions located at more than 3000 masl in Tibet, Bolivia, and Ecuador. Cano-Pérez et al. [15] in Colombia analysed data from 70 municipalities with altitudes between 1 and 3180 masl, finding an inverse relationship in the case fatality rate of COVID-19 and altitude level. Data from other ecological studies support these observations [16–18]. This can be explained via physiological adaptations of the angiotensin-converting enzyme (ACE) system [19]. SARS-CoV-2 enters human cells through the binding of its spike protein to ACE-2; then, it is internalized, and its replication begins. ACE-2 is widely present in human organs, with high expression in the respiratory tract, vascular endothelium, myocardium, renal tubules, gastrointestinal tract, testicles, and central nervous system, which explains the multisystemic involvement of severe COVID-19 disease [20]. Arias-Reyes et al. [14] also proposed that SARS-CoV-2 may be less virulent at high altitude owing to hypoxia-induced downregulation of ACE-2 expression, thus limiting viral replication and organ compromise.
However, information is contradictory. Zhang et al. and Dang et al. found a decrease in ACE-2 in cellular and animal models with hypoxaemia [21, 22]; however, other studies in different models have reported that hypoxia upregulates ACE-2 [23, 24]. The potential negative or positive clinical impact of ACE-2 upregulation or downregulation by oxygenation levels in COVID-19 has yet to be determined [20]. More recent additional ecological studies also do not support the positive effect of high altitude on clinical results. Valverde-Bruffau et al. [25], after analysing 1122 municipalities in Colombia, did not find a protective effect between the altitude and severity of COVID-19 disease, findings similar to those of Cardenas et al. [26] who, in 2881 municipalities of Peru and Colombia with altitudes between 2 and 4705 masl, found no difference in mortality.
The current evidence does not allow us to ascertain whether hypobaric hypoxaemia can prevent, treat, or aggravate COVID-19 infection [27].
This study was carried out in the city of Bogotá, capital of Colombia, located 2640 masl, with 8,848,588 inhabitants. By June 2021, more than 1,382,000 COVID-19 cases and 25,000 deaths had been reported https://saludata.saludcapital.gov.co/osb/index.php/datos-de-salud/enfermedades-trasmisibles/covid19/.
The aim of this study was to describe the clinical characteristics, laboratory findings, and mortality of patients with COVID-19 treated at the Hospital Universitario Mayor Méderi located in Bogotá, Colombia.
Methods
Study design and participants
This was an observational, single-centre, cohort study that included all patients with COVID-19 admitted to the Hospital Universitario Mayor Méderi in Bogotá, Colombia, conducted between 19 March 2020 and 30 April 2021. This is a high complexity university hospital located in the centre of the city of Bogotá, at 2640 masl. It has 99 intensive care beds, which during the pandemic were expanded to 131 beds, with 94 exclusively for the care of patients with COVID-19. It also has 790 general hospital beds, of which 295 are used for the care of patients with COVID-19. SARS-CoV-2 infection was confirmed by real-time reverse transcription-polymerase chain reaction (RT-PCR) in throat swab samples. We excluded individuals with incomplete medical records and patients under 16 years of age.
Data collection
We reviewed clinical electronic medical records and laboratory findings for all patients with laboratory-confirmed SARS-CoV-2 infection. On admission, we collected the following data: age, sex, past medical history, days of hospital stay, days of ICU stay, body mass index (BMI), management site (outpatients, inpatients, ICU, or emergency patients), laboratory values on admission (leucocyte blood count, neutrophil-lymphocyte ratio (NLR), haematocrit, haemoglobin, LDH, D-dimer, procalcitonin, ferritin), and oxygenation indices (S/F ratio at admission and at 48 h, P/F ratio at admission, 48 h, and at ICU admission). As is routine, electronic medical data were archived onto a local server, from which we retrieved these data.
Outcomes
The clinical outcomes assessed were discharge or death, need for IMV, and site management. For this study, 4 management sites were defined as follows:
-
1.
Outpatients: those who consulted and were discharged in the first 24 h and were not readmitted in the following 3 weeks.
-
2.
Inpatients: those who were admitted to the hospitalization service, with a stay > 24 h and did not transfer to the ICU at any time during their hospital stay.
-
3.
Intensive care unit (ICU): those who were admitted to the ICU at any time during their hospital stay.
-
4.
Emergency department (ED): those who received care only in the ED.
Statistical analysis
Qualitative variables were reported as frequencies and percentages, while quantitative variables were reported as medians and interquartile ranges. Clinical, sociodemographic, and laboratory characteristics were compared in relation to mortality, mechanical ventilation requirements, and management site (emergency room, ICU, hospitalization, or outpatient management) using nonparametric Mann-Whitney U-tests for all continuous variables (assuming heterogeneous variance) and X2 tests for categorical variables. We fitted a classification and regression tree (CART) using all the collected variables for comparison purposes. Selection of the covariates included for CART modelling was based on their biological and clinical relevance, on what was previously reported in the literature, and their statistical significance in the bivariate analysis. The CART algorithm quantified each variable’s weight and built risk profiles. This methodology contrasts with classical regression models in that the CART algorithm can discover effective modifiers and complex interactions between variables, whereas in regression models, the researcher must provide those interactions based on a prior hypothesis. Statistical analysis was performed using R software version 4.1.0 (Free Software Foundation’s GNU Public Licence), and the CART were modelled using the package RPART (recursive partition and regression trees).
Results
The cohort included 5161 adult patients treated at the Hospital Universitario Mayor Méderi. Patients who were still hospitalized by 30 April 2021 and 1 patient in whom the review of the electronic medical record was not possible were excluded from the final analysis. In total, 321 patients were excluded.
Of the 5161 patients, 2340 (45%) of them were women. A total of 1305 patients died (25%), and 3856 survived to hospital discharge (75%). The median age was 66 years (IQR 53–77). All patients were identified as Latino.
The most frequent comorbidity was arterial hypertension (23%), followed by hypothyroidism (7%), chronic obstructive pulmonary disease (COPD) (5.6%), and diabetes mellitus (5%).
Table 1 shows the baseline characteristics of the patients and the bivariate analysis in relation to mortality.
A total of 114 patients (2%) were managed in the ED, with 114 deaths (100%). In all, 39 of these patients (34%) were ventilated and died before being transferred to the ICU, and 75 patients (66%) were admitted for conservative management but remained in the emergency expansion area of the ED until their deaths due to high hospital occupancy. This high mortality can be explained given that the median age in this group was 81 years (IQR, 72–85, 75).
In all, 854 patients (17%) received outpatient management without reporting any mortality in the national registry system the month after discharge; these patients were the youngest in the cohort, with a median age of 47 years (IQR, 31–64.75).
A total to 2970 (58%) participants were inpatients, with 511 deaths (17%). The median age in this group was 68 years (IQR, 56–79). The high number of patients who died while hospitalized without being admitted to the ICU is explained by the elderly characteristics of the group, as the median age was 83 years (IQR, 74.5–88.0). Out of these 511 patients, 8 (0.02%) were ventilated and died before being transferred to the ICU, and the 503 remaining inpatients, together with the family and the guidelines of the institutional ethics committee, decided to limit invasive manoeuvres, such as orotracheal intubation or transfer to the ICU.
A total of 1223 participants (24%) were admitted to the ICU, with 680 deaths (56%). Of the 1223 ICU admissions, 851 of them were ventilated (70%). Out of the ventilated group, 566 of them died (67%) vs. 114 (31%) in the nonventilated group. These patients were admitted to the ICU but did not want orotracheal intubation, and this intervention was not performed. It is clarified that some patients were admitted to the ICU to receive noninvasive mechanical ventilation and haemodynamic support without orotracheal intubation, which was possible only at moments without the pandemic peaking. In Bogotá, for the date of the performance of this analysis, May 2021, there were 2 peaks with high hospital occupancy, the first in July and August 2020 and the second in December 2020 and January 2021, at which time only patients were admitted to the ICU with requirements of IMV.
Forty-seven patients received IMV and did not enter the ICU, along with 39 patients in the emergency room and 8 patients in hospitalization; these patients died before being transferred to the ICU because they were so sick. A total of 898 patients (17%) received IMV in this cohort, of whom 613 died (68%).
Table 2 shows the bivariate analysis in relation to the management site, and Table 3 shows the bivariate analysis in relation to the requirement for IMV.
The inflammatory markers ferritin, D-dimer, NLR, procalcitonin, and LDH were higher in the group of patients who died and required IMV and increased progressively, were lower in outpatients, were increased in hospitalized patients, and reached the highest levels in patients admitted to the ICU and those who died in the emergency room, indicating significant differences in each of the groups. All these values were statistically significant with p < 0.05, where p = 0.05 is the limitation for statistical significance (Tables 1, 2, and 3).
The oxygenation indices evaluated were the S/F ratio and the P/F ratio. In the entire admission cohort, the median S/F was 339 (IQR, 310–423), and the median P/F ratio was 233 (IQR, 180–274). Among the patients who remained in the hospital for 48 h, the S/F ratio decreased by a median of 325 (IQR, 254–341). The median S/F ratio at ICU admission was 168 (IQR, 105–255), and the median P/F ratio was 118 (IQR, 81–171). In the ICU patients who died, the median P/F ratio was 105 (IQR, 76–146), and in those who survived, it was 137 (IQR, 91–198). The median P/F ratio at ICU admission in patients who underwent IMV was 112 (IQR, 79–150) and 154 (IQR, 91-244) in those who did not. It is clearly observed that as oxygenation indices fall, the possibility of dying, requiring IMV, and entering the ICU increases (Tables 1, 2, and 3).
CART predictive model
Using the CART method, 2 predictive models were constructed, the first for IMV and the second for mortality.
A prediction model is presented in the CART methodology, which shows that a S/F ratio < 272 at 48 h of admission, high LDH levels at admission, and the presence of COPD are associated with an increase in the probability of requiring IMV. In the model, age ≥ 81 years decreased the possibility of the need for IMV, which is explained by the fact that many of these patients, due to personal decisions or clinical futility, were not taken to this therapy.
This model shows how the S/F ratio at 48 h ≥ 272 gives a 92% probability of not requiring IMV during the hospital stay (Fig. 1).
Need for invasive mechanical ventilation in patients with COVID-19, classification and regression tree (CART) risk groups: this method built a predictive model and five clinical profiles using the oxygen saturation to inspired oxygen fraction (SaO2/FiO2) ratio at 48 h after admission, age, lactate dehydrogenase (LDH), and chronic obstructive pulmonary disease (COPD) as predictor variables
A prediction model is also presented using the same methodology, which shows that the main predictor of mortality in this cohort is the requirement of IMV. We see how age ≥ 79, S/F ratio < 259 at admission, and LDH level ≥ 617 U/L increase the probability of death (Fig. 2). In this model, patients with a S/F ratio greater than 259 at admission who also had an elevated LDH level (> 617 U/L) had a high probability of death, possibly indicating that the inflammatory response is a determining factor.
Mortality in patients with COVID-19, classification and regression tree (CART) risk groups: this method built a predictive model and five clinical profiles using the need for invasive mechanical ventilation (IMV), age, the oxygen saturation to inspired oxygen fraction (SaO2/FiO2) ratio on admission, and initial lactate dehydrogenase (LDH) as predictor variables
Discussion
To our knowledge, this is the largest cohort of patients with COVID-19 living in a city located at an altitude of more than 2000 masl and one of the largest in a single centre.
The overall mean age in this cohort was 66 years (IQR, 53–77), which was one of the oldest reported [28–33], and 69 years (IQR, 59-76) in patients admitted to the ICU, which was the highest age reported in patients admitted to this service [33–37].
In all, 25% of the patients in this study died. If we excluded patients who were managed as outpatients and lost to follow-up, the mortality of patients requiring hospitalization was 30%, which is similar to other series reported in Italy (25%), the United States (US) (21%), Iran (24%), and Germany (27%) [30, 32, 38, 39] and higher than the series from China (5% to 16%) [28, 31, 40].
In this cohort, 1223 patients (24%) required ICU management, which was a larger proportion than the 7% found by Yang et al. in China [33] but similar to previous reports from the USA ranging from 22 to 32% [29, 37]. IMV was given to 898 patients (17%), which was a value higher than the Chinese studies, in which the use of IMV ranged from 1.4 to 8% [31, 40], and in an Italian study (8.7%) [30] but similar to studies from the USA in which 12.2%, 21%, and 22% of patients, respectively, required IMV [32, 37, 41]. This suggests that, in China, in-hospital management was given to patients with less severe disease.
Out of the 898 patients who received IMV, 613 of them died (68%), which is a figure lower than the studies from the onset of the pandemic in China (81%) [33] and the USA (88.1%) [41], which is similar to reports from the UK in March and April 2020 (66.3%) [42] and at the Brazilian National Registry of Intensive Care (66.9%) [43]. In later studies in high-income countries, the mortality reported in patients with IMV was lower, and among those, an Italian study showed mortality of 52% in ventilated patient s[36], and a multicentre prospective cohort of patients admitted to ICUs in France, Belgium, and Switzerland showed a 36% mortality rate [34].
Roedl et al. [44], in a multicentre study conducted in Germany, showed a mortality rate of 44% in patients with IMV. Lim et al. [45], in a review of 69 studies with more than 57,420 patients ventilated for severe COVID-19, found a mortality rate of 45% (95% CI, 39–52%); however, at the time of publication, many patients were still hospitalized. In this same study, the estimated mortality for patients aged 61 to 70 years was 77%.
Oxygenation indices have been broadly studied around the world as predictors of mortality and ICU admission in patients with COVID-19, leading to useful clinical practices to prioritize patients at hospital and ICU admission. Within those, a lower P/F ratio at ICU admission has been found to be a predictor of mortality among these patients, but few studies have been carried out regionally where this is stated.
In this study, the P/F ratio at ICU admission is one of the lowest when compared to other cohorts around the world, 118 vs. 129 in the USA; 160 in Italy; 154 in France, Belgium, and Switzerland; and 172 in China [29, 34, 35, 46]. This may be explained by the hypobaric hypoxaemia expected with altitude in Bogotá, Colombia. Although a study developed in critically ill patients in the USA at sea level [37] described a median P/F ratio of 103 at ICU admission, we analysed their parameters and found that the median FiO2 at ICU admission in these patients was 90%, compared to ours, in which the median FiO2 at ICU admission was 50%.
The P/F ratio on admission to the ICU in patients who underwent IMV was 112 vs. 154 in those who did not, thus indicating that the decision to start IMV was based not only on the oxygenation indices but also on the clinical presence of respiratory failure, and that a higher level of hypoxaemia was tolerated for the start of this therapy in relation to cities located at altitudes less than 1000 masl.
In patients admitted to the ICU, the P/F ratio was also significantly lower in patients who died (105) than in those who survived (137) compared to other studies where the P/F ratios in deceased patients and survivors were 134 and 163 [34], respectively.
There is insufficient clinical evidence to change the standard management of patients with COVID-19 based on oxygenation indices. The 2012 Berlin consensus [47] recommends an adjustment of the P/F ratio based on the BP in places over 1000 masl (BP/760); however, this recommendation does not have references on how it was derived [48]. In daily practice, based on experience and institutional management guidelines, patients with a P/F ratio greater than 250 without supplemental oxygen and without clinical dyspnoea may receive outpatient management. Patients with a P/F ratio of 200 to 250 are admitted to the hospital for surveillance, and supplemental oxygen is used for oxygen saturation greater than 88% and PaO2 greater than 60 mmHg. Patients with a P/F ratio less than 200 require surveillance in intermediate care with a high risk of requiring admission to the ICU. The decision to initiate IMV should not only be based on oxygenation indices but also on the presence of respiratory distress and tolerance and response to other methods of oxygen administration, such as high-flow cannula and noninvasive mechanical ventilation. Clinical trials are required to evaluate which oxygenation level once the patient is on mechanical ventilation is optimal for the initiation of neuromuscular relaxants and prone use. In the institutional guidelines of the Hospital Universitario Mayor, we recommend P/F levels of between 120 and 150 for these interventions at the discretion of the clinician.
Based on the current evidence, the oxygenation level at which it is best to start IMV is unknown. It must also be taken into account that during peaks of the pandemic, hospital occupancy was close to 100%, which interferes with the quality of care and may delay the start of IMV.
There is little information about the clinical characteristics of patients in high-altitude areas. Chen et al. [49], in a retrospective court of 67 patients who live in the Tibetan and Qiang Autonomous Prefecture of Ngawa, China, located at 2600 masl, found 4 severe cases (6%), 39 nonsevere cases (58.2%), and 24 (35.8%) asymptomatic cases, suggesting, as in the work of Seclén et al. [11], that altitude can protect against severe diseases caused by SARS-CoV-2. These results differ greatly from our findings, where only 17% of the patients were nonsevere cases with outpatient management, mortality was 25%, 24% of the patients were admitted to the ICU, and in 17% of the cases, IMV was used.
Abdelsalam et al. [50] analysed the clinical characteristics and laboratory findings of patients infected with COVID-19 in the city of Taif, Saudi Arabia, located at 1879 masl. Of 790 patients included in the analysis, 91.5% recovered without ICU admission, 6.8% recovered after ICU admission, and 1.7% died. In addition, a paired analysis was performed by age and comorbidities with 208 patients from the city of Jeddah, Saudi Arabia, located at sea level, finding a mortality of 14.4% and observing a lower mortality in people living at a high altitude. This reported mortality is much lower than that found in this study, which is explained by the age of the patients, since the total mean age was 41.4 years and 57.3 years among those who died, which is in great contrast with our population where the mean age of the entire population was 63.5 years and 74.3 years in the patients who died.
Several authors have documented alterations in C-reactive protein, D-dimer, and LDH that are associated with severity and mortality from COVID-19 [51]. Variations in the haemogram, coagulation tests, markers of myocardial injury, creatinine, and factors associated with systemic inflammation have been identified [52]. In the present study, the paraclinics that had a greater relationship with clinical outcomes in the bivariate analysis were LDH, D-dimer, and the neutrophil-lymphocyte ratio (NLR).
An uncontrolled inflammatory response is associated with worse clinical outcomes in SARS-CoV-2-infected patients [53]. Elevated serum concentrations of some inflammatory mediators have been described in patients with severe COVID-19, in particular, cytokines such as IL-1 and IL-6 [54]. However, in countries with limited resources, its clinical use is rare. More widely available tools, such as the NLR, can be used as markers of hyperinflammatory states [55, 56]. In COVID-19, it has been found that elevated NLR values are associated with a worse prognosis [57]. In addition, its ability to predict the severity and risk of death has been evaluated, as summarized in a meta-analysis that found an acceptable performance (mortality AUC 0.90 and severity AUC 0.85) with a cut-off of 6.5 [58].
Similar to the data described, our findings show a higher NLR among the deceased (NLR 11.78) than among the survivors (NLR 7.58). Likewise, the NLR was higher in patients admitted to the ICU (outpatient NLR 5.64, hospitalized NLR 7.82, and ICU NLR 11.58) and those who required IMV.
Moreover, the NLR among surviving patients was higher than those previously reported [59]. It remains to be confirmed whether high altitude can influence the baseline expression of inflammatory markers [60] or if it is a manifestation of disease severity at altitude. No previous articles have reported this ratio at high altitude.
LDH is the enzyme responsible for the passage from pyruvate to lactate, and its elevation has been associated with severity and death in infectious and neoplastic diseases [61, 62]. Different studies have established the performance of LDH as a prognostic biomarker in patients with SARS-CoV-2 infection [51, 63–65]. It has been documented that its elevation is associated with a risk up to six times higher for developing severe forms of COVID-19 (OR 6.7, 95% CI: 2.4–18.9) [63] and four times higher for mortality (OR 4.22, 95% CI: 2.49–7.14) [66]. In our study, the data were consistent with those previously reported. LDH was higher among the dead patients (471 U/L) than among the living patients (351 U/L). Likewise, its value was higher among ventilated patients (510 U/L) than among those who did not require this support (354 U/L).
Ballaz et al. [67] described the findings of the haemogram upon admission in Quito, Ecuador, at 2850 masl, finding expected inflammatory changes for patients with COVID-19, with a high NLR, and lymphopenia in the most severe cases. The study by Ballaz showed mean haemoglobin values similar to those in our study, 14.9 g/dL vs. 14.7 g/dL in nonsevere cases and 15.4 g/dL vs. 14.3 g/dL in severe cases. These findings suggest that haemoglobin values associated with exposure to high altitude at altitudes between 2500 and 3000 masl may not be relevant to the severity of COVID-19 presentation.
In the prediction model presented by the CART methodology, oxygenation indices, LDH level (as an inflammatory marker), and COPD (as a comorbidity) increase the probability of IMV, findings similar to other studies [37, 44].
In the prediction model for mortality, it is not surprising that the requirement for IMV is the main factor associated with death, since this indicates which patients are sicker; however, the model allows us to observe that being older than 79 years, hypoxaemia and elevated levels of LDH (as an inflammatory marker) increase the probability of death, even in nonventilated patients. These findings are similar to other studies [31, 33, 44, 46]. The advantage of this modelling is that it allows us to discover effect modifiers and complex interactions between variables.
Conclusion
We conclude that, although the oxygenation indices are lower in the city of Bogotá due to hypobaric hypoxaemia, the need for hospitalization, admission to the ICU, and IMV are similar to other regions less than 1000 masl, except China, where most data indicate that patients with less severe disease were hospitalized.
The mortality of patients with IMV in this study is high but similar to that reported in high-income countries at the beginning of the pandemic and in other Latin American countries; however, it has remained high throughout the entire pandemic, unlike high-income countries where it has decreased, suggesting hypobaric hypoxaemia may not be the main factor in mortality from COVID-19 leading to IMV, and the availability of resources is an important factor in mortality.
In this study, it was also found that the levels of oxygenation indices at altitude, which is management decisions such as the start of IMV and therefore associated therapies (e.g. use of neuromuscular relaxants and prone), are lower than at sea level; however, clinical trials should be performed to determine the P/F ratio cut-off point of greatest benefit for these therapies.
Limitations
This study has many limitations. It is a descriptive study of a single-centre high complexity hospital in the city of Bogotá, which may not reflect the behaviour of the pandemic throughout the country. It does not describe the pharmacological therapies used in the patients; however, it is noted that, in Colombia, in the drugs with some evidence of benefit in clinical use in patients with COVID-19 for general use, only dexamethasone in patients admitted to the hospital with supplemental oxygen was available (no other drug therapies were available (e.g. remdesivir and tocilizumab). Also, the vaccination effort began at the end of March 2021, so this study does not yet reflect the impact of this measure. The use of other ventilation therapies, such as noninvasive and high-flow cannulas, is not described, since these were used outside of the ICU and in expansion areas, and the quantification of their time of use given that the records in the clinical history were not performed exactly.
Availability of data and materials
All data used and analysed during this study are available from the corresponding author on reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- masl:
-
Metres above sea level
- IMV:
-
Invasive mechanical ventilation
- CART:
-
Classification and regression trees
- IQR:
-
Interquartile range
- ICU:
-
Intensive care unit
- PaO2 :
-
Pressure arterial oxygen
- FiO2 :
-
Fraction inspired oxygen
- P/F:
-
Ratio of partial pressure arterial oxygen to fraction inspired oxygen
- SaO2 :
-
Oxygen saturation
- S/F:
-
Ratio of oxygen saturation to fraction inspired oxygen
- LDH:
-
Lactate dehydrogenase
- BP:
-
Barometric pressure
- PiO2 :
-
Pressure of inspired oxygen
- ACE:
-
Angiotensin-converting enzyme
- RT-PCR:
-
Real-time reverse transcription-polymerase chain reaction
- BMI:
-
Body mass index
- NLR:
-
Neutrophil-lymphocyte ratio
- ED:
-
Emergency department
- RPART:
-
Recursive partition and regression trees
- COPD:
-
Chronic obstructive pulmonary disease
- AUC:
-
Area under the curve
References
Luks AM, Auerbach PS, Freer L, Grissom CK, Keyes LE, McIntosh SE, et al. Wilderness Medical Society clinical practice guidelines for the prevention and treatment of acute altitude illness: 2019 update. Wilderness Environ Med. 2019;30(4):S3–18 Available from: https://linkinghub.elsevier.com/retrieve/pii/S1080603219300900 [cited 9 Oct 2021].
Penaloza D. Efectos de la exposición a grandes alturas en la circulación pulmonar. Rev Esp Cardiol. 2012;65(12):1075–8 Available from: https://linkinghub.elsevier.com/retrieve/pii/S0300893212004605 [cited 23 Jul 2021].
Sharma P, Misra K. High altitude and hypoxia. In: Management of High Altitude Pathophysiology: Elsevier; 2018. p. 3–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/B978012813999800001X [cited 23 Jul 2021].
Netzer N, Strohl K, Faulhaber M, Gatterer H, Burtscher M. Hypoxia-related altitude illnesses. J Travel Med. 2013;20(4):247–55 Available from: https://academic.oup.com/jtm/article-lookup/doi/10.1111/jtm.12017 [cited 23 Jul 2021].
Lasso Apráez MD, JI. Interpretación de los gases arteriales en Bogotá (2.640 msnm) basada en el nomograma de Siggaard-Andersen. Una propuesta para facilitar y unificar la lectura. Rev Colomb Neumol. 2014;26(1) Available from: http://sena.metarevistas.org/index.php/rcneumologia/article/view/56 [cited 23 Jul 2021].
Avellanas Chavala ML. Un viaje entre la hipoxia de la gran altitud y la hipoxia del enfermo crítico: ¿qué puede enseñarnos en la compresión y manejo de las enfermedades críticas? Med Intensiva (Engl Ed). 2018;42(6):380–90 Available from: https://linkinghub.elsevier.com/retrieve/pii/S0210569117302309 [cited 23 Jul 2021].
Faeh D, Gutzwiller F, Bopp M. Lower mortality from coronary heart disease and stroke at higher altitudes in Switzerland. Circulation. 2009;120(6):495–501 Available from: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.108.819250 [cited 9 Oct 2021].
Díaz-Gutiérrez J, Martínez-González MÁ, Pons Izquierdo JJ, González-Muniesa P, Martínez JA, Bes-Rastrollo M. Living at higher altitude and incidence of overweight/obesity: prospective analysis of the SUN cohort. PLoS One. 2016;11(11):e0164483 Available from: https://dx.plos.org/10.1371/journal.pone.0164483 [cited 10 Jul 2021]. Schooling CM, editor.
Woolcott OO, Castillo OA, Gutierrez C, Elashoff RM, Stefanovski D, Bergman RN. Inverse association between diabetes and altitude: a cross-sectional study in the adult population of the United States: diabetes at high altitude. Obesity. 2014;22(9):2080–90 Available from: https://onlinelibrary.wiley.com/doi/10.1002/oby.20800 [cited 10 Jul 2021].
Burtscher M. Lower mortality rates in those living at moderate altitude. Aging. 2016;8(10):2603–4 Available from: https://www.aging-us.com/lookup/doi/10.18632/aging.101057 [cited 9 Oct 2021].
Seclén SN, Nunez-Robles E, Yovera-Aldana M, Arias-Chumpitaz A. Incidence of COVID-19 infection and prevalence of diabetes, obesity and hypertension according to altitude in Peruvian population. Diabetes Res Clin Pract. 2020;169:108463 Available from: https://linkinghub.elsevier.com/retrieve/pii/S0168822720307166 [cited 9 Oct 2021].
Pérez-Padilla R, García-Sancho C, Fernández R, Franco-Marina F, López-Gatell H, Bojórquez I. The impact of altitude on hospitalization and hospital mortality from pandemic 2009 influenza A (H1N1) virus pneumonia in Mexico. Salud Pública Méx. 2013;55(1):92–5 Available from: http://www.scielosp.org/scielo.php?script=sci_arttext&pid=S0036-36342013000100013&lng=en&nrm=iso&tlng=en [cited 10 Jul 2021].
Eisen S, Pealing L, Aldridge RW, Siedner MJ, Necochea A, Leybell I, et al. Effects of ascent to high altitude on human antimycobacterial immunity. PLoS One. 2013;8(9):e74220 Available from: https://dx.plos.org/10.1371/journal.pone.0074220 [cited 10 Jul 2021]. Pai M, editor.
Arias-Reyes C, Zubieta-DeUrioste N, Poma-Machicao L, Aliaga-Raduan F, Carvajal-Rodriguez F, Dutschmann M, et al. Does the pathogenesis of SARS-CoV-2 virus decrease at high-altitude? Respir Physiol Neurobiol. 2020;277:103443 Available from: https://linkinghub.elsevier.com/retrieve/pii/S1569904820301014 [cited 9 Oct 2021].
Cano-Pérez E, Torres-Pacheco J, Fragozo-Ramos MC, García-Díaz G, Montalvo-Varela E, Pozo-Palacios JC. Negative correlation between altitude and COVID-19 pandemic in Colombia: a preliminary report. Am J Trop Med Hyg. 2020;103(6):2347–9 Available from: https://ajtmh.org/doi/10.4269/ajtmh.20-1027 [cited 9 Oct 2021].
Stephens KE, Chernyavskiy P, Bruns DR. Impact of altitude on COVID-19 infection and death in the United States: a modeling and observational study. PLoS One. 2021;16(1):e0245055 Available from: https://dx.plos.org/10.1371/journal.pone.0245055. Shaman J, editor [cited 10 Jul 2021].
Castagnetto JM, Segovia-Juarez J, Gonzales GF. Letter to the Editor: COVID-19 Infections do not change with increasing altitudes from 1,000 to 4,700 m. High Alt Med Biol. 2020;21(4):428–30 Available from: https://www.liebertpub.com/doi/10.1089/ham.2020.0173 [cited 10 Jul 2021].
Fernandes JSC, da Silva RS, Silva AC, Villela DC, Mendonça VA, Lacerda ACR. Altitude conditions seem to determine the evolution of COVID-19 in Brazil. Sci Rep. 2021;11(1):4402 Available from: http://www.nature.com/articles/s41598-021-83971-x [cited 10 Jul 2021].
Burtscher J, Burtscher M, Millet GP. Caution is needed on the effect of altitude on the pathogenesis of SAR-CoV-2 virus. Respir Physiol Neurobiol. 2020;279:103464 Available from: https://linkinghub.elsevier.com/retrieve/pii/S1569904820301221 [cited 9 Oct 2021].
Pun M, Turner R, Strapazzon G, Brugger H, Swenson ER. Lower incidence of COVID-19 at high altitude: facts and confounders. High Alt Med Biol. 2020;21(3):217–22 Available from: https://www.liebertpub.com/doi/10.1089/ham.2020.0114 [cited 9 Oct 2021].
Zhang R, Wu Y, Zhao M, Liu C, Zhou L, Shen S, et al. Role of HIF-1α in the regulation ACE and ACE2 expression in hypoxic human pulmonary artery smooth muscle cells. Am J Physiol Lung Cell Mol Physiol. 2009;297(4):L631–40 Available from: https://www.physiology.org/doi/10.1152/ajplung.90415.2008 [cited 9 Oct 2021].
Dang Z, Su S, Jin G, Nan X, Ma L, Li Z, et al. Tsantan Sumtang attenuated chronic hypoxia-induced right ventricular structure remodeling and fibrosis by equilibrating local ACE-AngII-AT1R/ACE2-Ang1-7-Mas axis in rat. J Ethnopharmacol. 2020;250:112470 Available from: https://linkinghub.elsevier.com/retrieve/pii/S037887411931387X [cited 9 Oct 2021].
Oarhe CI, Dang V, Dang M, Nguyen H, Gopallawa I, Gewolb IH, et al. Hyperoxia downregulates angiotensin-converting enzyme-2 in human fetal lung fibroblasts. Pediatr Res. 2015;77(5):656–62 Available from: http://www.nature.com/articles/pr201527 [cited 9 Oct 2021].
Hampl V, Herget J, Bíbová J, Baňasová A, Husková Z, Vaňourková Z, et al. Intrapulmonary activation of the angiotensin-converting enzyme type 2/angiotensin 1-7/G-protein-coupled mas receptor axis attenuates pulmonary hypertension in Ren-2 transgenic rats exposed to chronic hypoxia. Physiol Res. 2015:25–38 Available from: https://www.biomed.cas.cz/physiolres/pdf/64/64_25.pdf [cited 9 Oct 2021].
Valverde-Bruffau VJ, Cárdenas L, Gonzales GF. The pathogenicity of COVID-19 is independent of increasing altitude: the case of Colombia. Am J Trop Med Hyg. 2020; Available from: https://ajtmh.org/doi/10.4269/ajtmh.20-1465 [cited 10 Jul 2021].
Cardenas L, Valverde-Bruffau V, Gonzales GF. Altitude does not protect against SARS-CoV-2 infections and mortality due to COVID-19. Physiol Rep. 2021;9(11) Available from: https://onlinelibrary.wiley.com/doi/10.14814/phy2.14922 [cited 10 Jul 2021].
Millet GP, Debevec T, Brocherie F, Burtscher M, Burtscher J. Altitude and COVID-19: friend or foe? A narrative review. Physiol Rep. 2021;8(24) Available from: https://onlinelibrary.wiley.com/doi/10.14814/phy2.14615 [cited 10 Jul 2021].
Du R-H, Liang L-R, Yang C-Q, Wang W, Cao T-Z, Li M, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5):2000524 Available from: http://erj.ersjournals.com/lookup/doi/10.1183/13993003.00524-2020 [cited 10 Jul 2021].
Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395:9.
Santus P, Radovanovic D, Saderi L, Marino P, Cogliati C, De Filippis G, et al. Severity of respiratory failure at admission and in-hospital mortality in patients with COVID-19: a prospective observational multicentre study. BMJ Open. 2020;10(10):e043651 Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2020-043651 [cited 10 Jul 2021].
Zhang X-B, Hu L, Ming Q, Wei X-J, Zhang Z-Y, Chen L-D, et al. Risk factors for mortality of coronavirus disease-2019 (COVID-19) patients in two centers of Hubei province, China: a retrospective analysis. PLoS One. 2021;16(1):e0246030 Available from: https://dx.plos.org/10.1371/journal.pone.0246030. Lucas A, editor [cited 10 Jul 2021].
Garibaldi BT, Fiksel J, Muschelli J, Robinson ML, Rouhizadeh M, Perin J, et al. Patient trajectories among persons hospitalized for COVID-19: a cohort study. Ann Intern Med. 2021;174(1):33–41 Available from: https://www.acpjournals.org/doi/10.7326/M20-3905 [cited 10 Jul 2021].
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81 Available from: https://linkinghub.elsevier.com/retrieve/pii/S2213260020300795 [cited 10 Jul 2021].
COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47(1):60–73 Available from: http://link.springer.com/10.1007/s00134-020-06294-x [cited 10 Jul 2021].
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574 Available from: https://jamanetwork.com/journals/jama/fullarticle/2764365 [cited 10 Jul 2021].
Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;180(10):1345 Available from: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2768601 [cited 10 Jul 2021].
Anesi GL, Jablonski J, Harhay MO, Atkins JH, Bajaj J, Baston C, et al. Characteristics, outcomes, and trends of patients with COVID-19–related critical illness at a learning health system in the United States. Ann Intern Med. 2021;174(5):613–21 Available from: https://www.acpjournals.org/doi/10.7326/M20-5327 [cited 10 Jul 2021].
Jalili M, Payandemehr P, Saghaei A, Sari HN, Safikhani H, Kolivand P. Characteristics and mortality of hospitalized patients with COVID-19 in Iran: a national retrospective cohort study. Ann Intern Med. 2021;174(1):125–7 Available from: https://www.acpjournals.org/doi/10.7326/M20-2911 [cited 10 Jul 2021].
Budweiser S, Baş Ş, Jörres RA, Engelhardt S, von Delius S, Lenherr K, et al. Patients’ treatment limitations as predictive factor for mortality in COVID-19: results from hospitalized patients of a hotspot region for SARS-CoV-2 infections. Respir Res. 2021;22(1):168 Available from: https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-021-01756-2 [cited 10 Jul 2021].
Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110–8 Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091674920304954 [cited 10 Jul 2021].
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052 Available from: https://jamanetwork.com/journals/jama/fullarticle/2765184 [cited 10 Jul 2021].
House N, Holborn H, Wc L. ICNARC report on COVID-19 in critical care; 2020. p. 17.
http://www.utisbrasileiras.com.br/sari-covid-19/benchmarking-covid-19/. Available from: 16. http://www.utisbrasileiras.com.br/sari-covid-19/benchmarking-covid-19/
Roedl K, Jarczak D, Thasler L, Bachmann M, Schulte F, Bein B, et al. Mechanical ventilation and mortality among 223 critically ill patients with coronavirus disease 2019: a multicentric study in Germany. Aust Crit Care. 2021;34(2):167–75 Available from: https://linkinghub.elsevier.com/retrieve/pii/S1036731420303349 [cited 10 Jul 2021].
Lim ZJ, Subramaniam A, Ponnapa Reddy M, Blecher G, Kadam U, Afroz A, et al. Case fatality rates for patients with COVID-19 requiring invasive mechanical ventilation. A meta-analysis. Am J Respir Crit Care Med. 2021;203(1):54–66 Available from: https://www.atsjournals.org/doi/10.1164/rccm.202006-2405OC [cited 10 Jul 2021].
Gu Y, Wang D, Chen C, Lu W, Liu H, Lv T, et al. PaO2/FiO2 and IL-6 are risk factors of mortality for intensive care COVID-19 patients. Sci Rep. 2021;11(1):7334 Available from: http://www.nature.com/articles/s41598-021-86676-3 [cited 10 Jul 2021].
ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E,Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526-33. https://doi.org/10.1001/jama.2012.5669.
Pérez-Padilla R, Hernández-Cárdenas CM, Lugo-Goytia G. Classifying acute respiratory distress syndrome severity: correcting the arterial oxygen partial pressure to fractional inspired oxygen at altitude. Rev Investig Clin Organo Hosp Enfermedades Nutr. 2016;68(4):169–70.
Chen H, Qin L, Wu S, Xu W, Gao R, Zhang X. Clinical characteristics and laboratory features of COVID-19 in high altitude areas: a retrospective cohort study. PLoS One. 2021;16(5):e0249964 Available from: https://dx.plos.org/10.1371/journal.pone.0249964. Serra R, editor [cited 9 Oct 2021].
Abdelsalam M, Althaqafi RMM, Assiri SA, Althagafi TM, Althagafi SM, Fouda AY, et al. Clinical and laboratory findings of COVID-19 in high-altitude inhabitants of Saudi Arabia. Front Med. 2021;8:670195 Available from: https://www.frontiersin.org/articles/10.3389/fmed.2021.670195/full [cited 9 Oct 2021].
Ghahramani S, Tabrizi R, Lankarani KB, Kashani SMA, Rezaei S, Zeidi N, et al. Laboratory features of severe vs. non-severe COVID-19 patients in Asian populations: a systematic review and meta-analysis. Eur J Med Res. 2020;25(1):30 Available from: https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-020-00432-3 [cited 22 Jul 2021].
Lippi G, Plebani M. Laboratory abnormalities in patients with COVID-2019 infection. Clin Chem Lab Med CCLM. 2020;58(7):1131–4.
Mangalmurti N, Hunter CA. Cytokine storms: understanding COVID-19. Immunity. 2020;53(1):19–25.
Tang Y, Liu J, Zhang D, Xu Z, Ji J, Wen C. Cytokine storm in COVID-19: the current evidence and treatment strategies. Front Immunol. 2020;11:1708.
Pantzaris N-D, Platanaki C, Pierrako C, Karamouzos V, Velissaris D. Neutrophil-to-lymphocyte ratio relation to sepsis severity scores and inflammatory biomarkers in patients with community-acquired pneumonia: a case series. J Transl Intern Med. 2018;6(1):43–6 Available from: https://www.sciendo.com/article/10.2478/jtim-2018-0009 [cited 10 Jul 2021].
Chen X-Q, Xue C-R, Hou P, Lin B-Q, Zhang J-R. Lymphocyte-to-monocyte ratio effectively predicts survival outcome of patients with obstructive colorectal cancer. World J Gastroenterol. 2019;25(33):4970–84 Available from: https://www.wjgnet.com/1007-9327/full/v25/i33/4970.htm [cited 10 Jul 2021].
Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. 2020;18(1):206 Available from: https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02374-0 [cited 10 Jul 2021].
Li X, Liu C, Mao Z, Xiao M, Wang L, Qi S, et al. Predictive values of neutrophil-to-lymphocyte ratio on disease severity and mortality in COVID-19 patients: a systematic review and meta-analysis. Crit Care. 2020;24(1):647.
Ye W, Chen G, Li X, Lan X, Ji C, Hou M, et al. Dynamic changes of D-dimer and neutrophil-lymphocyte count ratio as prognostic biomarkers in COVID-19. Respir Res. 2020;21(1):169 Available from: https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-020-01428-7 [cited 10 Jul 2021].
Pham K, Parikh K, Heinrich EC. Hypoxia and inflammation: insights from high-altitude physiology. Front Physiol. 2021;12:676782 Available from: https://www.frontiersin.org/articles/10.3389/fphys.2021.676782/full [cited 10 Jul 2021].
Lu J, Wei Z, Jiang H, Cheng L, Chen Q, Chen M, et al. Lactate dehydrogenase is associated with 28-day mortality in patients with sepsis: a retrospective observational study. J Surg Res. 2018;228:314–21 Available from: https://linkinghub.elsevier.com/retrieve/pii/S0022480418301987 [cited 22 Jul 2021].
Forkasiewicz A, Dorociak M, Stach K, Szelachowski P, Tabola R, Augoff K. The usefulness of lactate dehydrogenase measurements in current oncological practice. Cell Mol Biol Lett. 2020;25(1):–35 Available from: https://cmbl.biomedcentral.com/articles/10.1186/s11658-020-00228-7 [cited 22 Jul 2021].
Zhang Z-L, Hou Y-L, Li D-T, Li F-Z. Laboratory findings of COVID-19: a systematic review and meta-analysis. Scand J Clin Lab Invest. 2020;80(6):441–7 Available from: https://www.tandfonline.com/doi/full/10.1080/00365513.2020.1768587 [cited 22 Jul 2021].
Izcovich A, Ragusa MA, Tortosa F, Lavena Marzio MA, Agnoletti C, Bengolea A, et al. Prognostic factors for severity and mortality in patients infected with COVID-19: a systematic review. PLoS One. 2020;15(11):e0241955 Available from: https://dx.plos.org/10.1371/journal.pone.0241955. Lazzeri C, editor. [cited 22 Jul 2021].
Szarpak L, Ruetzler K, Safiejko K, Hampel M, Pruc M, Kanczuga-Koda L, et al. Lactate dehydrogenase level as a COVID-19 severity marker. Am J Emerg Med. 2021;45:638–9 Available from: https://linkinghub.elsevier.com/retrieve/pii/S0735675720310342 [cited 22 Jul 2021].
Martha JW, Wibowo A, Pranata R. Prognostic value of elevated lactate dehydrogenase in patients with COVID-19: a systematic review and meta-analysis. Postgrad Med J. 2021:postgradmedj-2020-139542 Available from: https://pmj.bmj.com/lookup/doi/10.1136/postgradmedj-2020-139542 [cited 22 Jul 2021].
Ballaz SJ, Pulgar-Sánchez M, Chamorro K, Fernández-Moreira E, Ramírez H, Mora FX, et al. Common laboratory tests as indicators of COVID-19 severity on admission at high altitude: a single-center retrospective study in Quito (ECUADOR). Clin Chem Lab Med CCLM. 2021;59(8):e326–9 Available from: https://www.degruyter.com/document/doi/10.1515/cclm-2021-0156/html [cited 9 Oct 2021].
Acknowledgements
Not applicable
Funding
Hospital Universitario Mayor Mederi funded the collection, analysis, and interpretation of the data in this manuscript.
Author information
Authors and Affiliations
Contributions
DR is the principal investigator of this trial. DR, AP, CR, DP, MJ, MD, JC, AA, and AR were responsible for the data collection. DR and NM interpreted the statistical analyses. All authors contributed to interpretation of data, critically reviewed, and revised and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work is in line with the recommendations for biomedical research of the Declaration of Helsinki of the World Medical Association and is based on the regulations set forth in Resolution No. 8430 of 1993 (October 4, 1993) of the Colombian Ministry of Health, which establishes academic, technical, and administrative standards for health research. According to article 11 of Resolution 8430 of 1993, this research is classified as minimal risk research, because it uses documentary research techniques, and there is no intervention or intentional modification of the biological, physiological, psychological, or social variables of individuals participating in the study. The use of this information was approved and evaluated by the Research Technician of Hospital Universitario Mayor Méderi and the Ethics Committee of Universidad del Rosario. Each patient or legal representative signed a general institutional informed consent form upon admission to the ICU of Hospital Universitario Mayor Mederi, in which he or she expresses his or her will to allow the use of clinical history data, diagnostic images, photographs, and the publication of this information for academic purposes. It is specified in this consent that all information that can identify or correlate to the person will be anonymized to guarantee their confidentiality.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rodriguez Lima, D.R., Pinzón Rondón, Á.M., Rubio Ramos, C. et al. Clinical characteristics and mortality associated with COVID-19 at high altitude: a cohort of 5161 patients in Bogotá, Colombia. Int J Emerg Med 15, 22 (2022). https://doi.org/10.1186/s12245-022-00426-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12245-022-00426-4