Abstract
Background
Primary polydipsia is commonly seen in patients with psychiatric illnesses. Excess water intake is also seen in patient with anorexia and anticholinergic medications. We report a patient who had hyponatraemia and rhabdomyolysis after consuming excess water for ureteric calculus.
Case presentation
A healthy middle-aged male presented with an episode of generalized tonic-clonic seizure and reduced level of consciousness preceded by consumption of excess water. He was recently diagnosed to have a ureteric calculus and was advised to consume plenty of water. On examination, he was disoriented in place, person and time. Except for the generalized diminished reflexes, other neurological and systemic examinations were normal. He had severe hyponatraemia, mild hypokalaemia and myoglobulinuria. His serum creatinine phosphokinase and aspartate aminotransferase were markedly elevated. The diagnosis of rhabdomyolysis in the setting of acute water intoxication was made. Optimum fluid and electrolyte management achieved a dramatic recovery of consciousness, hyponatraemia and rhabdomyolysis.
Discussion
The patient has had excess water intake due to a compulsive act in the background fear of ureteric calculus. Such act could lead to severe hyponatraemia and rhabdomyolysis. Therefore, future similar acts could be prevented by proper medical advice. Further, emergency physicians should be vigilant for rhabdomyolysis in patients with hyponatraemia or hypokalaemia.
Similar content being viewed by others
Background
Psychogenic polydipsia can induce hyponatraemia [1,2,3,4,5]. Hyponatraemia in turn could lead to cerebral oedema and subsequent neurological complications like seizure or coma. Moreover, hyponatraemia could cause rhabdomyolysis [6]. This is a serious complication which could be easily ignored. Therefore, polydipsia can rarely lead to rhabdomyolysis and prevention of which needs optimum vigilance [1,2,3,4,5,6,7,8,9]. We discuss the management and monitoring of a patient who had acute water intoxication induced hyponatraemia and rhabdomyolysis after being advised to consume water for his recently diagnosed ureteric calculus.
Case presentation
History and examination
A 41-year-old male was in good health until 2 weeks ago when he developed a left-sided renal colicky type pain and was diagnosed to have a left mid ureteric calculus by radiography. He was reassured and requested to consume plenty of water. Two days before, he had consumed excessive amount of water, about 10 l per day, and developed polyuria. During these 2 days, he has had fever, dark urine, generalized weakness and altered level of consciousness. On the day of admission, he developed a single episode of self-terminating generalized tonic-clonic seizure lasting for 5 min followed by reduced level of consciousness. There was no previous history or family history of adult-onset seizures. There were no features suggestive of psychiatric illness like low mood, reduced sleep or overtalkative behaviour. The patient was never transfused with blood or blood products. There was no recent travel history. He is married and has a 10-year-old child. He is an accountant by profession. The patient has had good income and family support. He occasionally consumed alcohol and smoked cigarette, but denied any drug abuse. He was not on any long-term medication. On examination, he was disoriented in place, person and time. The Glasgow coma scale (GCS) score was 9 on admission (motor—5, verbal—2, eye—2). Except for a temperature of 101 °F and the generalized diminished reflexes, other vital signs and cardiovascular, respiratory, abdominal and neurological examinations were normal. Table 1 outlines the timeline of this case report.
Differential diagnosis
This is a previously healthy male who presented with fever for 2 days complicated with generalized tonic-clonic seizure and reduced level of consciousness. In the acute setting, the first working diagnosis was meningoencephalitis. It could be due to viral or bacterial aetiology. Moreover, he had dark coloured urine; therefore, falciparum malaria which can led to cerebral malaria was also suspected. Collateral history from the patient’s family revealed an excessive water intake of about 10 l per day for 2 days which led to an additional differential diagnosis. One possibility is psychogenic polydipsia which is the most common cause for excessive water intake. However, there was no history of psychiatric illness or any long-term drug history which can lead to polydipsia. The reason for his excessive water intake was to get rid of the unpleasant pain due to the ureteric calculus.
Investigation and management
On admission, he was found to have hypoosmolar (242 mOsm/kg of water), hyponatraemia (119 mmol/L), hypokalaemia (2.9 mmol/L), hypoosmolar urine (195 mOsm/kg of water), mild leucocytosis (12.7 × 103 per microliter) with neutrophilia and myoglobinuria. His serum creatinine phosphokinase (10,000 U/L) was markedly elevated with a rise in aspartate aminotransferase (AST) (2316 U/L) and alanine aminotransferase (ALT) (463 U/L) levels. Renal functions were within normal ranges. Blood for malaria parasite was negative. Non-contrast computed tomography scan of the brain was normal. Electroencephalogram done on the 5th day revealed generalized, continuous, slow activity suggestive of diffuse cortical dysfunction. This could be due to an encephalopathy preceded by hyponatraemia.
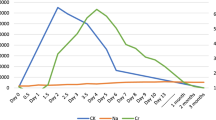
Hyponatraemia-induced generalized tonic-clonic seizure, altered level of consciousness and rhabdomyolysis were diagnosed in our patient. His hyponatraemia was most probably due to excess water intake. The patient was given a bolus of 3% hypertonic saline (100 mL over 20 min) for symptomatic severe hyponatraemia [10]. The diagnosis of rhabdomyolysis was made because he had body aches, dark urine, elevated levels of creatine kinase and urinary myoglobin. His serum creatinine phosphokinase peaked to the highest level (54,841 U/L) by the 7th day. Also, the patient’s elevated AST and ALT could be due to the muscle damage. As there was rhabdomyolysis, hypokalaemia correction was done once (KCl 40 mmol over 12 h) and serum potassium level was assessed regularly. Further doses of potassium were not required. A strict fluid restriction was not followed as there was a high risk of developing acute renal failure due to rhabdomyolysis. The input per hour was decided by measuring the previous hours’ output and adding 20 mL for the first 5 days. He did not develop oliguria or features of acute renal failure. Considering the history of fever and seizure with altered level of consciousness, he was started on intravenous cefotaxime (2 g 6 hourly), intravenous acyclovir (500 mg 8 hourly) and intravenous dexamethasone (2 mg 6 hourly) after collecting blood and urine for culture. However, the patient’s family denied consent for lumbar puncture. Blood and urine culture revealed no growth, but the antibiotics were continued for a total of 10 days as we could not exclude central nervous system infection without a lumbar puncture. The magnetic resonance imaging of the brain was normal on the 11th day of admission.
Outcome
GCS score improved gradually to 15, and serum sodium and potassium were normalized by the 3rd day of admission. The patient did not have any further episode of seizure. His fever settled, and serum and urine osmolality were normalized by the 5th day. He responded to the above management and did not develop any complications of rhabdomyolysis. On discharge, his serum creatinine phosphokinase (49 U/L), AST (66 U/L) and ALT (78 U/L) levels were near normal. He was discharged on the 15th day of admission with appropriate medical advice to prevent similar complications.
Discussion
Cases of acute water intoxication leading to hyponatraemia and rhabdomyolysis were found in few reports of previous literature. The first such case was reported by Browne PM in 1979 where an elderly patient drank excess water to increase his urine output which he thought was low [11]. Another patient was reported in 1987 when a 64-year-old patient with major depression developed self-induced water intoxication associated with rhabdomyolysis [12]. Most of the other cases were reported in patients with psychiatric illness [1,2,3,4,5,6,7,8], while Putterman et al. reported on a patient who had acute voluntary water intoxication following exercise [9]. However, our patient had an acute voluntary water intoxication following a compulsive act for renal colicky type pain.
Hyponatraemia is the most common electrolyte abnormality in the hospitalized patients [13]. Severity of its presentation depends on how rapidly the condition develops and the degree of cerebral oedema. Symptoms of hyponatraemia include poor concentration, anorexia, headache, irritability, restlessness, nausea, vomiting, fatigue, disorientation, confusion, seizure and respiratory arrest [14, 15]. Too rapid correction of hyponatraemia could cause a rapid shift in plasma osmolality and lead to central or extra pontine myelinolysis [16]. Thus, in our patient, a gradual correction of hyponatraemia was achieved. Causes of hyponatraemia are divided according to the volume status (euvolaemic, hypovolaemic and hypervolaemic) [17]. As the patient had a euvolaemic status, possible cause for euvolaemic hyponatraemia in this patient could be primary polydipsia ahead of syndrome of inappropriate antidiuretic hormone secretion, hypothyroidism or reset osmostat [17]. Primary polydipsia is a well-known entity which is commonly seen in patients with psychiatric illness like schizophrenia or in patients who are on antipsychotic treatment [18]. However, our patient had excessive water intake that led to hyponatraemia due to a compulsive act of fear for ureteric calculus.
Polydipsia-induced hyponatraemia can rarely lead to rhabdomyolysis [1,2,3,4,5,6,7,8,9, 19]. Rhabdomyolysis is a rare but serious clinical entity, and the mechanism of its occurrence is unclear [6]. Moreover, potassium released from muscles during exercise can cause vasodilation and increase the blood flow to the muscle. Thus, hypokalaemia may induce rhabdomyolysis by reducing blood flow to muscles in response to exertion. In our patient, both hyponatraemia and hypokalaemia were noted which might have contributed for the development of rhabdomyolysis. Rhabdomyolysis is a condition characterized by muscle necrosis and the release of intracellular muscle constituents into the circulation. Classic triad of muscle pain, muscle weakness and dark coloured urine was not seen in all patients [20]. Above half of the patients with confirmed rhabdomyolysis do not exhibit the muscle symptoms [20]. The spectrum of disease ranges from asymptomatic elevations in serum muscle enzymes to life-threatening illness associated with acute kidney injury and electrolyte imbalances [21]. Management of rhabdomyolysis should include treatment of the cause and prevention of its complications such as acute kidney injury. For the prevention of acute kidney injury, early and aggressive fluid resuscitation is essential. But our patient had water intoxication and hyponatraemia; therefore, fluid resuscitation was done with less aggression.
Polydipsia-induced hyponatraemia is a rare cause of rhabdomyolysis. Emergency physicians should be vigilant of this potential complication. One of the key points to learn from this case is that the physician should consider checking a serum creatinine phosphokinase level in patients presenting with hyponatraemia or hypokalaemia. Future studies need to explore the mechanism by which hyponatraemia could cause rhabdomyolysis. The patient has had excess water intake due to a compulsive act leading to severe hyponatraemia and rhabdomyolysis. Therefore, compulsive act of excess water intake should be prevented by individualized medical advice. Further, emergency physicians should keep in mind that hyponatraemia or hypokalaemia can be associated with rhabdomyolysis.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- GCS:
-
Glasgow coma scale
References
Shenoi AN, Stockwell J. Recurrent rhabdomyolysis in a teenager with psychosis-intermittent hyponatremia-polydipsia syndrome. Pediatr Emerg Care. 2015;31(4):274–6.
Tényi T, Vörös V. Successful switch to olanzapine after rhabdomyolysis caused by water intoxication and clozapine use. Pharmacopsychiatry. 2006;39(4):157–8.
Zaidi AN. Rhabdomyolysis after correction of hyponatremia in psychogenic polydipsia possibly complicated by ziprasidone. Ann Pharmacother. 2005;39(10):1726–31.
Rizzieri DA. Rhabdomyolysis after correction of hyponatremia due to psychogenic polydipsia. Mayo Clin Proc. 1995;70(5):473–6.
Akasaki Y, Nagatomo I, Akasaki Y, Nomaguchi M, Akasaki Y, Matsumoto K. Water intoxication in a schizophrenic patient with rhabdomyolysis. Jpn J Psychiatry Neurol. 1993;47(4):843–6.
Katsarou A, Singh S. Hyponatraemia associated rhabdomyolysis following water intoxication. BMJ Case Rep. 2010;2010:bcr0220102720.
Ting JY. Rhabdomyolysis and polydipsic hyponatraemia. Emerg Med J. 2001;18(6):520.
Korzets A, Ori Y, Floro S, Ish-Tov E, Chagnac A, Weinstein T, Zevin D, Gruzman C. Case report: severe hyponatremia after water intoxication: a potential cause of rhabdomyolysis. Am J Med Sci. 1996;312(2):92–4.
Putterman C, Levy L, Rubinger D. Transient exercise-induced water intoxication and rhabdomyolysis. Am J Kidney Dis. 1993;21(2):206–9.
Sterns RH, Nigwekar SU, Hix JK. The treatment of hyponatremia. Semin Nephrol. 2009;29(3):282–99.
Browne PM. Rhabdomyolysis and myoglobinuria associated with acute water intoxication. West J Med. 1979;130(5):459–61.
Mor F, Mor-Snir I, Wysenbeek AJ. Rhabdomyolysis in self-induced water intoxication. J Nerv Ment Dis. 1987;175(12):742–3.
Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med. 2006;119(7 Suppl 1):S30–5.
Lien Y-HH, Shapiro JI. Hyponatremia: clinical diagnosis and management. Am J Med. 2007;120(8):653–8.
Mount DB. The brain in hyponatremia: both culprit and victim. Semin Nephrol. 2009;29(3):196–215.
Sterns RH . Osmotic demyelination syndrome (ODS) and overly rapid correction of hyponatremia. UpToDate. 2019. Available from: https://www.uptodate.com/contents/osmotic-demyelination-syndrome-ods-and-overly-rapid-correction-of-hyponatremia. [cited 2019 Aug 6]
Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and management of sodium disorders: hyponatremia and hypernatremia. Am Fam Physician. 2015;91(5):299–307.
Sailer C, Winzeler B, Christ-Crain M. Primary polydipsia in the medical and psychiatric patient: characteristics, complications and therapy. Swiss Med Wkly. 2017;147:w14514.
Morita S, Inokuchi S, Yamamoto R, Inoue S, Tamura K, Ohama S, Nakagawa Y, Yamamoto I. Risk factors for rhabdomyolysis in self-induced water intoxication (SIWI) patients. J Emerg Med. 2010;38(3):293–6.
Cervellin G, Comelli I, Lippi G. Rhabdomyolysis: historical background, clinical, diagnostic and therapeutic features. Clin Chem Lab Med. 2010;48(6):749–56.
Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: rhabdomyolysis -- an overview for clinicians. Crit Care. 2005;9(2):158–69.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SF and FS diagnosed and managed the patient. SF and DR recorded data. SF drafted the initial report. DR did the literature search. FS and DR critically revised the report. All authors read and approved the final report.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for the publication of their clinical details was obtained from the patient. A copy of the consent form is available for review by the editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Fernando, S., Sivagnanam, F. & Rathish, D. A compulsive act of excess water intake leading to hyponatraemia and rhabdomyolysis: a case report. Int J Emerg Med 12, 34 (2019). https://doi.org/10.1186/s12245-019-0255-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12245-019-0255-6