Abstract
The right person in the right place and at the right time is not always possible; telemedicine offers the potential to give audio and visual access to the appropriate clinician for patients. Advances in information and communication technology (ICT) in the area of video-to-video communication have led to growth in telemedicine applications in recent years. For these advances to be properly integrated into healthcare delivery, a regulatory framework, supported by definitive high-quality research, should be developed. Telemedicine is well suited to extending the reach of specialist services particularly in the pre-hospital care of acute emergencies where treatment delays may affect clinical outcome. The exponential growth in research and development in telemedicine has led to improvements in clinical outcomes in emergency medical care. This review is part of the LiveCity project to examine the history and existing applications of telemedicine in the pre-hospital environment. A search of electronic databases including Medline, Excerpta Medica Database (EMBASE), Cochrane, and Cumulative Index to Nursing and Allied Health Literature (CINAHL) for relevant papers was performed. All studies addressing the use of telemedicine in emergency medical or pre-hospital care setting were included. Out of a total of 1,279 articles reviewed, 39 met the inclusion criteria and were critically analysed. A majority of the studies were on stroke management. The studies suggested that overall, telemedicine had a positive impact on emergency medical care. It improved the pre-hospital diagnosis of stroke and myocardial infarction and enhanced the supervision of delivery of tissue thromboplasminogen activator in acute ischaemic stroke. Telemedicine presents an opportunity to enhance patient management. There are as yet few definitive studies that have demonstrated whether it had an effect on clinical outcome.
Similar content being viewed by others
Review
Introduction
There is a critical global shortage of healthcare professionals. As a consequence, qualified professionals may not be physically present particularly in under-resourced regions, and providing quality healthcare may be quite challenging. This challenge can be tackled by providing specialist medical services using information and communication technologies to remotely located healthcare workers and patients where such expertise is not immediately available. This is known as telemedicine. In telemedicine, the client is separated from the expert in space [[1]]. The concept of telemedicine has been used in one form or another for centuries. Smoke signals were used in ancient African villages to alert adjoining villages of disease outbreaks, and bonfires were used to warn of bubonic plague in the Middle Ages in Europe. With advances in telecommunication, newer systems such as the telegraph were used to transmit medical information about epidemics and war casualties. However, the use of telemedicine was facilitated by the invention of the telephone in the nineteenth century. This culminated in one of the earliest recorded uses of information and communication technology (ICT) in telemedicine, when Einthoven, on 7th February 1906, transmitted electrocardiogram (ECG) tracings over telephone lines [[2]]. By the 1930s, medical information was being transmitted from remote regions of Australia and Alaska to specialist medical centres. With the invention of the television in the 1950s, advances in closed-circuit television and video conferencing led to the adoption of telemedicine in patient monitoring and consultations [[3]]. Perhaps, the earliest implementation of modern telemedicine was by the National Aeronautics and Space Administration (NASA) in the 1960s when it was used for remote physiological monitoring of astronauts during manned space flights [[4]]. NASA continued to play a pivotal role in the development of telemedicine with the development of the Space Technology Applied to Rural Papago Advanced Health Care (STARPAHC) project on the Papago Indian Reservation in Arizona, USA, in 1972. The STARPAHC project included a van equipped with an X-ray machine and other medical instruments, and it was staffed by two paramedics. The van was linked by two-way microwave transmission to the Public Health Service Hospital complemented by a remotely located clinic staffed by a physician assistant linked to the control centre in the hospital [[5]]. After the December 1988 earthquake disaster in Armenia, NASA established the first international telemedicine project known as the Spacebridge to Armenia that allowed telemedicine consultation between medical centres in the United States and Armenia [[6]]. By the 1970s, the National Library of Medicine funded research into the reliability of telemedicine via satellite communication to 26 sites in Alaska, USA. Improvements in telecommunications technology have led to advances in network infrastructure that enabled the development of high-definition live interactive video-to-video networks such as the European Union-funded LiveCity project. These, in turn, have led to increased telemedicine use over the past 40 to 50 years with a subsequent increase in research since the 1990s.
Telemedicine potentially holds great promise in facilitating emergency medical practice. It is increasingly being used in emergency medicine with an associated increase in published research. It is particularly suited to medical emergencies where treatment delays adversely affect clinical outcome. A typical scenario is ST elevated myocardial infarction (STEMI) where recognition of ECG changes by paramedics could facilitate early intervention and improve clinical outcome. However, recognition of ECG changes of STEMI by paramedics appears to be suboptimal [[7]], and adverse clinical events that occur during pre-hospital transportation [[8]] may also benefit from real-time clinician advice. Paramedics in ambulances have used telemedicine links with specialists to facilitate pre-hospital diagnosis and reduce treatment delays in stroke, myocardial infarction, and trauma. Telemedicine has also been used by emergency medicine doctors to supervise remotely located nurse practitioners and general practitioners in minor injury clinics [[9]].
This literature review is part of the emergency use case of the LiveCity project and analyses published studies to highlight the use of telemedicine in pre-hospital care.
Methods
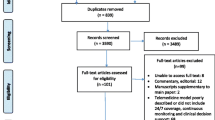
We performed an automated electronic search using the MeSH terms identified in Medline. The terms included the following: Telemedicine, Telecare, Telehealth, Teletrauma, Telestroke, eHealth, mobile Health, Pre-hospital care, and emergency care. The search terms were used as keywords on Medline, Excerpta Medica Database (EMBASE), Cochrane Database of Systemic Reviews (CDSR), Cochrane, and Cumulative Index to Nursing and Allied Health Literature (CINAHL). The search was then finalized using Boolean operators to combine (‘OR’) and cross-reference (‘AND’) between domains. The first ten pages of a basic web search using the Google search engine were analysed for relevant articles. A manual search was done by checking reference lists of selected articles and researching key authors.
Abstracts were independently reviewed by two of the authors, and the full text of articles that met the inclusion criteria were retrieved for further analysis. Included studies were collated and critically analysed based on their methodology and sample size to summarize their results.
Studies carried out between 1970 and 2014 that addressed telemedicine use in the emergency care of trauma, myocardial infarction, and stroke and studies whose outcomes included cost-effectiveness, feasibility, and clinical outcome were included in the review. Case reports and studies that were not published in English and did not address an aspect of emergency medicine were excluded from this review.
Results
The initial literature search yielded 1,279 studies. Based on the inclusion criteria, 1,240 were excluded, while 39 were selected for further analysis. Twenty-five of the studies focused on stroke management, while five and nine were on myocardial infarction and trauma, respectively.
We found eight articles that were feasibility studies, while six articles explored the reliability of telemedicine. Four articles addressed the diagnostic accuracy of telemedicine, and three articles explored the use of telemedicine to reduce treatment delays. Thirteen studies used the ‘Hub and Spoke’ model, while five of the studies used a link between an ambulance and a hospital. Twenty-one of the studies reviewed did not clearly define the model used.
Table 1 shows the characteristics of the studies included. We found 2 randomized controlled studies, 10 case-control studies, and 27 observational and descriptive studies (1). The network types used in the studies were the following: mobile broadband in 8 and wired broadband in 31 of the studies included. The methodologies and subjects of the studies reflect the nascent nature of research in this field. Early studies address the feasibility, accuracy, and reliability of telemedicine use in clinical settings which have not been fully addressed due to design flaws identified in Tables 2, 3, and 4.
Discussion
There has been an exponential growth in the number of telemedicine articles published since the mid-1990s. This review noted the highest amount of research into telemedicine use in stroke care. Trauma and myocardial infarction have seen much less telemedicine-related research.
Stroke
Telemedicine in stroke management has undergone the most extensive study of all areas examined. Its use is feasible [[10],[11]] but dependent on the technical performance of the telemedicine equipment and broadband infrastructure [[12],[21]]. Due to its novel uses, medico-legal concerns have led to questions about the relevance and clarity of communication during informed consent. However, analysis of video-taped telemedicine consultations of acute stroke patients before intravenous administration of tissue plasminogen activator showed that 80% of observers rated informed consent as adequate [[23]]. Administration of tissue thromboplasminogen activator (tPA) within 3 to 4.5 h [[49]–[51]] of an acute ischemic stroke remains the gold standard in its management. However, this approach is restricted by time constraints and requires the supervision of a clinician with expertise in stroke management, and as a result, there is a disappointingly low utilization of thrombolysis in ischaemic stroke [[52],[53]]. Where available, integrating stroke specialists in pre-hospital stroke response teams significantly reduces time to treatment [[54]]. This is however not possible in a large proportion of locations where there is a limited availability of stroke specialists. Remote access to a stroke specialist is now possible, and recent studies comparing in-person consultation with remote consultation suggest that telemedicine is a promising solution to the lack of local expertise. The National Institute of Health Stroke Scale (NIHSS) assessment of stroke patients using telemedicine is as reliable as face-to-face assessment [[20]]. And radiological review of brain CT in stroke management is both feasible and reliable [[34]]. In the ‘hub and spoke model’, under served areas where stroke management expertise is lacking (i.e. spoke), telemedicine provides an ideal opportunity for supervision by a centrally located stroke expert (hub). Analysis of clinical outcomes of patients managed using this model suggest that although there is increased consultation, the quality of care remains similar and there was no statistical difference between telemedicine and face-to-face consultation, in short-term [[14],[15]] and long-term [[25],[26]] mortality. In the context of budgetary constraints, a cost-effectiveness analysis indicated that telemedicine is more expensive than usual care [[16]] partly due to high upfront equipment cost. However, there is the potential for significant cost savings due to reduced length of hospital stay [[55]].
Trauma
The effects of telemedicine on trauma management have not been as widely studied as in stroke, in the emergency medical services. Telemedicine has been deployed in major disasters such as the Armenian earthquake disaster in 1988. It is well suited to the management of major incidents where an acute deficit of healthcare professionals can be ameliorated by teleconsultation [[56]]. Where local expertise is lacking, teleradiology has improved diagnosis and reduced expensive transfer of trauma patients [[57]]. Analysis of the impact of telemedicine on emergency medical services suggests a reduction in mortality and hospital cost [[40]]. In a hub and spoke model of a central burns unit and three peripheral hospitals, telemedicine use led to increased consultation, but burns assessment was as accurate as face-to-face assessment and reduction in transfers to burns units led to significant cost savings [[41]]. Interestingly, paramedics that were guided by an emergency medicine clinician could obtain interpretable focused assessment with sonography for trauma (FAST) ultrasound [[42]], recognize key physical signs, and make better management decisions [[43]]. The use of a telemedicine referral in an acute burns unit led to a reduction in admission that could reduce hospital costs [[45]].
Myocardial infarction
The ideal recommendation for reperfusion of STEMI is within 2 h of first medical contact [[58]]. The requirement for urgent management of patients with myocardial infarction can be facilitated by the use of telemedicine for diagnosis and treatment. Efforts to shorten treatment delay are crucial, and various studies have been published addressing this challenge. Patient transfer directly to percutaneous coronary intervention (PCI) laboratory after pre-hospital diagnosis of STEMI in a telemedicine-equipped ambulance reduced treatment delay [[35],[36]] and reduced mortality from myocardial infarction [[59]]. To expedite reduction in treatment delay, accurate ECG diagnosis of STEMI remains crucial. Currently computer [[60]] and paramedics [[7]] ECG interpretation are not reliable enough to enhance patient triage for urgent PCI.
Conclusion
This review found limited conclusive studies for the effectiveness of telemedicine in emergency medicine. The best evidence is in stroke management where conclusive evidence of the significant positive effect of telestroke on clinical outcome has led to its recommendation for stroke management. Telemedicine appears to have a significant impact on the quality of ECG interpretation, but there is as yet no conclusive evidence that telemedicine affects clinical outcome in myocardial infarction. We could find very few studies that critically analysed telemedicine use in the pre-hospital care of trauma. Studies have demonstrated that burns assessment using telemedicine was as accurate as face-to-face assessment.
The proliferation of smartphones, tablets, and other mobile electronic devices creates an opportunity to extend standard professional health care particularly in medical emergencies where urgent intervention could reduce mortality and improve quality of life. Telemedicine could enhance emergency medical services by helping expedite urgent patient transfer, improve remote consultation, and enhance supervision of paramedics and nurses.
However, in order to regulate and standardize practice, more research is required. Particular emphasis should be on better study design and larger sample size to improve the reliability of results and conclusions. A large proportion of the studies analysed focused on ambulance mounted equipment. Wearable technology such as head-mounted displays that will allow paramedics reach patients in situ may improve early pre-hospital diagnosis and should be investigated. To further reduce response times, consideration should also be given to incorporating smartphone technology into emergency systems and thus facilitate patient or bystander incident reporting. Although technological advances will continue to outpace their utilization in clinical practice, incorporating emerging technologies into medical practice holds promise in improving care and enhancing clinical outcomes, and researchers must continue to evaluate the effectiveness of telemedicine so that communication technology-assisted care is optimized.
References
Craig J, Patterson V: Introduction to the practice of telemedicine. J Telemed Telecare 2005,11(1):3–9. 10.1258/1357633053430494
Hjelm NM, Julius HW: Centenary of tele-electrocardiography and telephonocardiography. J Telemed Telecare 2005,11(7):336–338. 10.1258/135763305774472088
Murphy RL, Bird KT: Telediagnosis: a new community health resource. Observations on the feasibility of telediagnosis based on 1000 patient transactions. Am J Public Health 1974,64(2):113–119. 10.2105/AJPH.64.2.113
Zundel KM: Telemedicine: history, applications, and impact on librarianship. Bull Med Libr Assoc 1996,84(1):71–79.
Freiburger G, Holcomb M, Piper D: The STARPAHC collection: part of an archive of the history of telemedicine. J Telemed Telecare 2007,13(5):221–223. 10.1258/135763307781458949
Doarn CR, Merrell RC: Spacebridge to Armenia: a look back at its impact on telemedicine in disaster response. Telemed J E Health 2011,17(7):546–552. 10.1089/tmj.2010.0212
Mencl F, Wilber S, Frey J, Zalewski J, Maiers JF, Bhalla MC: Paramedic ability to recognize ST-segment elevation myocardial infarction on prehospital electrocardiograms. Prehosp Emerg Care 2013,17(2):203–210. 10.3109/10903127.2012.755585
Ryan D, Craig AM, Turner L, Verbeek PR: Clinical events and treatment in prehospital patients with ST-segment elevation myocardial infarction. Prehosp Emerg Care 2013,17(2):181–186. 10.3109/10903127.2012.744783
Mair F, McClusky C, Wilsgaard T, Wootton R: The added value of video for consultations in telemedicine for minor injuries work. J Telemed Telecare 2011,17(8):427–431. 10.1258/jtt.2011.110318
Waite K, Silver F, Jaigobin C, Black S, Lee L, Murray B, Danyliuk P, Brown EM: Telestroke: a multi-site, emergency-based telemedicine service in Ontario. J Telemed Telecare 2006,12(3):141–145. 10.1258/135763306776738611
Hess DC, Wang S, Hamilton W, Lee S, Pardue C, Waller JL, Gross H, Nichols F, Hall C, Adams RJ: REACH: clinical feasibility of a rural telestroke network. Stroke 2005,36(9):2018–2020. 10.1161/01.STR.0000177534.02969.e4
Liman TG, Winter B, Waldschmidt C, Zerbe N, Hufnagl P, Audebert HJ, Endres M: Telestroke ambulances in prehospital stroke management: concept and pilot feasibility study. Stroke 2012,43(8):2086–2090. 10.1161/STROKEAHA.112.657270
Gonzalez MA, Hanna N, Rodrigo ME, Satler LF, Waksman R: Reliability of prehospital real-time cellular video phone in assessing the simplified National Institutes Of Health Stroke Scale in patients with acute stroke: a novel telemedicine technology. Stroke 2011,42(6):1522–1527. 10.1161/STROKEAHA.110.600296
Pedragosa A, Alvarez-Sabin J, Molina CA, Sanclemente C, Martín MC, Alonso F, Ribo M: Impact of a telemedicine system on acute stroke care in a community hospital. J Telemed Telecare 2009,15(5):260–263. 10.1258/jtt.2009.090102
Demaerschalk BM, Raman R, Ernstrom K, Meyer BC: Efficacy of telemedicine for stroke: pooled analysis of the Stroke Team Remote Evaluation Using a Digital Observation Camera (STRokE DOC) and STRokE DOC Arizona telestroke trials. Telemed J E Health 2012,18(3):230–237. 10.1089/tmj.2011.0116
Nelson RE, Saltzman GM, Skalabrin EJ, Demaerschalk BM, Majersik JJ: The cost-effectiveness of telestroke in the treatment of acute ischemic stroke. Neurology 2011,77(17):1590–1598. 10.1212/WNL.0b013e318234332d
Demaerschalk BM, Bobrow BJ, Raman R, Ernstrom K, Hoxworth JM, Patel AC, Kiernan TE, Aguilar MI, Ingall TJ, Dodick DW, Meyer BC: CT interpretation in a telestroke network: agreement among a spoke radiologist, hub vascular neurologist, and hub neuroradiologist. Stroke 2012,43(11):3095–3097. 10.1161/STROKEAHA.112.666255
Wang S, Lee SB, Pardue C, Ramsingh D, Waller J, Gross H, Nichols FT 3rd, Hess DC, Adams RJ: Remote evaluation of acute ischemic stroke: reliability of National Institutes of Health Stroke Scale via telestroke. Stroke 2003,34(10):e188–191. 10.1161/01.STR.0000091847.82140.9D
LaMonte MP, Xiao Y, Hu PF, Gagliano DM, Bahouth MN, Gunawardane RD, MacKenzie CF, Gaasch WR, Cullen J: Shortening time to stroke treatment using ambulance telemedicine: TeleBAT. J Stroke Cerebrovasc Dis 2004,13(4):148–154. 10.1016/j.jstrokecerebrovasdis.2004.03.004
Handschu R, Littmann R, Reulbach U, Gaul C, Heckmann JG, Neundörfer B, Scibor M: Telemedicine in emergency evaluation of acute stroke: interrater agreement in remote video examination with a novel multimedia system. Stroke 2003,34(12):2842–2846. 10.1161/01.STR.0000102043.70312.E9
Puetz V, Bodechtel U, Gerber JC, Dzialowski I, Kunz A, Wolz M, Hentschel H, Schultheiss T, Kepplinger J, Schneider H, Wiedemann B, Wojciechowski C, Reichmann H, Gahn G, von Kummer R: Reliability of brain CT evaluation by stroke neurologists in telemedicine. Neurology 2013,80(4):332–338. 10.1212/WNL.0b013e31827f07d0
Bergrath S, Reich A, Rossaint R, Rörtgen D, Gerber J, Fischermann H, Beckers SK, Brokmann JC, Schulz JB, Leber C, Fitzner C, Skorning M: Feasibility of prehospital teleconsultation in acute stroke–a pilot study in clinical routine. PLoS One 2012,7(5):e36796. 10.1371/journal.pone.0036796
Thomas L, Viswanathan A, Cochrane TI, Johnson J, O'Brien J, McMahon M, Santimauro JM, Schwamm LH: Variability in the perception of informed consent for IV-tPA during telestroke consultation. Front Neurol 2012, 3: 128. 10.3389/fneur.2012.00128
Zaidi SF, Jumma MA, Urra XN, Hammer M, Massaro L, Reddy V, Jovin T, Lin R, Wechsler LR: Telestroke-guided intravenous tissue-type plasminogen activator treatment achieves a similar clinical outcome as thrombolysis at a comprehensive stroke center. Stroke 2011,42(11):3291–3293. 10.1161/STROKEAHA.111.625046
Chowdhury M, Birns J, Rudd A, Bhalla A: Telemedicine versus face-to-face evaluation in the delivery of thrombolysis for acute ischaemic stroke: a single centre experience. Postgrad Med J 2012,88(1037):134–137. 10.1136/postgradmedj-2011-130060
Pervez MA, Silva G, Masrur S, Betensky RA, Furie KL, Hidalgo R, Lima F, Rosenthal ES, Rost N, Viswanathan A, Schwamm LH: Remote supervision of IV-tPA for acute ischemic stroke by telemedicine or telephone before transfer to a regional stroke center is feasible and safe. Stroke 2010,41(1):e18-e24. 10.1161/STROKEAHA.109.560169
Meyer BC, Raman R, Ernstrom K, Tafreshi GM, Huisa B, Stemer AB, Hemmen TM: Assessment of long-term outcomes for the STRokE DOC telemedicine trial. J Stroke Cerebrovasc Dis 2012,21(4):259–264. 10.1016/j.jstrokecerebrovasdis.2010.08.004
Schwab S, Vatankhah B, Kukla C, Hauchwitz M, Bogdahn U, Fürst A, Audebert HJ, Horn M: Long-term outcome after thrombolysis in telemedical stroke care. Neurology 2007,69(9):898–903. 10.1212/01.wnl.0000269671.08423.14
Audebert HJ, Kukla C, Vatankhah B, Gotzler B, Schenkel J, Hofer S, Fürst A, Haberl RL: Comparison of tissue plasminogen activator administration management between Telestroke Network hospitals and academic stroke centers: the Telemedical Pilot Project for Integrative Stroke Care in Bavaria/Germany. Stroke 2006,37(7):1822–1827. 10.1161/01.STR.0000226741.20629.b2
Ang SH, Tan C, Singh R: Telestroke: rapid treatment of acute ischemic stroke patients using telemedicine in a Singapore emergency department. Eur J Emerg Med 2013,20(5):322–326. 10.1097/MEJ.0b013e32835898d5
Switzer JA, Hall CE, Close B, Nichols FT, Gross H, Bruno A, Hess DC: A telestroke network enhances recruitment into acute stroke clinical trials. Stroke 2010,41(3):566–569. 10.1161/STROKEAHA.109.566844
Agarwal S, Day DJ, Sibson L, Barry PJ, Collas D, Metcalf K, Cotter PE, Guyler P, O'Brien EW, O'Brien A, O'Kane D, Owusu-Agyei P, Phillips P, Shekhar R, Warburton EA: Thrombolysis delivery by a regional telestroke network--experience from the U.K. National Health Service. J Am Heart Assoc 2014,3(1):e000408. 10.1161/JAHA.113.000408
Richard S, Lavandier K, Zioueche Y, Pelletier S, Vezain A, Ducrocq X: Use of telemedicine to manage severe ischaemic strokes in a rural area with an elderly population. Neurol Sci 2014,35(5):683–685. 10.1007/s10072-013-1577-4
Demaerschalk BM, Vargas JE, Channer DD, Noble BN, Kiernan TE, Gleason EA, Vargas BB, Ingall TJ, Aguilar MI, Dodick DW, Bobrow BJ: Smartphone teleradiology application is successfully incorporated into a telestroke network environment. Stroke 2012,43(11):3098–3101. 10.1161/STROKEAHA.112.669325
Terkelsen CJ, Lassen JF, Nørgaard BL, Gerdes JC, Poulsen SH, Bendix K, Ankersen JP, Gøtzsche LB, Rømer FK, Nielsen TT, Andersen HR: Reduction of treatment delay in patients with ST-elevation myocardial infarction: impact of pre-hospital diagnosis and direct referral to primary percutaneous coronary intervention. Eur Heart J 2005,26(8):770–777. 10.1093/eurheartj/ehi100
Zanini R, Aroldi M, Bonatti S, Buffoli F, Izzo A, Lettieri C, Romano M, Tomasi L, Ferrari MR: Impact of prehospital diagnosis in the management of ST elevation myocardial infarction in the era of primary percutaneous coronary intervention: reduction of treatment delay and mortality. J Cardiovasc Med 2008,9(6):570–575. 10.2459/JCM.0b013e3282f2c9bd
Brunetti ND, De Gennaro L, Amodio G, Dellegrottaglie G, Pellegrino PL, Di Biase M, Antonelli G: Telecardiology improves quality of diagnosis and reduces delay to treatment in elderly patients with acute myocardial infarction and atypical presentation. Eur J Cardiovasc Prev Rehabil 2010,17(6):615–620. 10.1097/HJR.0b013e328331f9e5
Terkelsen CJ, Norgaard BL, Lassen JF, Gerdes JC, Ankersen JP, Rømer F, Nielsen TT, Andersen HR: Telemedicine used for remote prehospital diagnosing in patients suspected of acute myocardial infarction. J Intern Med 2002,252(5):412–420. 10.1046/j.1365-2796.2002.01051.x
Sejersten M, Sillesen M, Hansen PR, Nielsen SL, Nielsen H, Trautner S, Hampton D, Wagner GS, Clemmensen P: Effect on treatment delay of prehospital teletransmission of 12-lead electrocardiogram to a cardiologist for immediate triage and direct referral of patients with ST-segment elevation acute myocardial infarction to primary percutaneous coronary intervention. Am J Cardiol 2008,101(7):941–946. 10.1016/j.amjcard.2007.11.038
Duchesne JC, Kyle A, Simmons J, Islam S, Schmieg RE Jr, Olivier J, McSwain NE Jr: Impact of telemedicine upon rural trauma care. J Trauma 2008,64(1):92–97. discussion 97–98 10.1097/TA.0b013e31815dd4c4
Saffle JR, Edelman L, Theurer L, Morris SE, Cochran A: Telemedicine evaluation of acute burns is accurate and cost-effective. J Trauma 2009,67(2):358–365. 10.1097/TA.0b013e3181ae9b02
Boniface KS, Shokoohi H, Smith ER, Scantlebury K: Tele-ultrasound and paramedics: real-time remote physician guidance of the focused assessment with sonography for trauma examination. Am J Emerg Med 2011,29(5):477–481. 10.1016/j.ajem.2009.12.001
Charash WE, Caputo MP, Clark H, Callas PW, Rogers FB, Crookes BA, Alborg MS, Ricci MA: Telemedicine to a moving ambulance improves outcome after trauma in simulated patients. J Trauma 2011,71(1):49–54. discussion 55 10.1097/TA.0b013e31821e4690
Rogers FB, Ricci M, Caputo M, Shackford S, Sartorelli K, Callas P, Dewell J, Daye S: The use of telemedicine for real-time video consultation between trauma center and community hospital in a rural setting improves early trauma care: preliminary results. J Trauma 2001,51(6):1037–1041. 10.1097/00005373-200112000-00002
Wallace DL, Smith RW, Pickford MA: A cohort study of acute plastic surgery trauma and burn referrals using telemedicine. J Telemed Telecare 2007,13(6):282–287. 10.1258/135763307781644933
Tachakra S, Lynch M, Newson R, Stinson A, Sivakumar A, Hayes J, Bak J: A comparison of telemedicine with face-to-face consultations for trauma management. J Telemed Telecare 2000,6(Suppl 1):S178-S181. 10.1258/1357633001934591
Rortgen D, Bergrath S, Rossaint R, Beckers SK, Fischermann H, Na IS, Peters D, Fitzner C, Skorning M: Comparison of physician staffed emergency teams with paramedic teams assisted by telemedicine–a randomized, controlled simulation study. Resuscitation 2013,84(1):85–92. 10.1016/j.resuscitation.2012.06.012
Tachakra S, Loane M, Uche CU: A follow-up study of remote trauma teleconsultations. J Telemed Telecare 2000,6(6):330–334. 10.1258/1357633001936003
Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks EF: Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary working groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation 2007,115(20):e478-e534. 10.1161/CIRCULATIONAHA.107.181486
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D: Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008,359(13):1317–1329. 10.1056/NEJMoa0804656
del Zoppo GJ, Saver JL, Jauch EC, Adams HP: Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator. Stroke 2009,40(8):2945–2948. 10.1161/STROKEAHA.109.192535
Nasr DM, Brinjikji W, Cloft HJ, Rabinstein AA: Utilization of intravenous thrombolysis is increasing in the United States. Int J Stroke 2013,8(8):681–688. 10.1111/j.1747-4949.2012.00844.x
Grotta JC, Burgin WS, El-Mitwalli A, Long M, Campbell M, Morgenstern LB, Malkoff M, Alexandrov AV: Intravenous tissue-type plasminogen activator therapy for ischemic stroke: Houston experience 1996 to 2000. Arch Neurol 2001,58(12):2009–2013. 10.1001/archneur.58.12.2009
Weber JE, Ebinger M, Rozanski M, Waldschmidt C, Wendt M, Winter B, Kellner P, Baumann A, Fiebach JB, Villringer K, Kaczmarek S, Endres M, Audebert HJ: Prehospital thrombolysis in acute stroke: results of the PHANTOM-S pilot study. Neurology 2013,80(2):163–168. 10.1212/WNL.0b013e31827b90e5
Switzer JA, Demaerschalk BM, Xie J, Fan L, Villa KF, Wu EQ: Cost-effectiveness of hub-and-spoke telestroke networks for the management of acute ischemic stroke from the hospitals' perspectives. Circ Cardiovasc Qual Outcomes 2013,6(1):18–26. 10.1161/CIRCOUTCOMES.112.967125
Benner T, Schachinger U, Nerlich M: Telemedicine in trauma and disasters–from war to earthquake: are we ready? Stud Health Tech Informat 2004, 104: 106–115.
Ashkenazi I, Haspel J, Alfici R, Kessel B, Khashan T, Oren M: Effect of teleradiology upon pattern of transfer of head injured patients from a rural general hospital to a neurosurgical referral centre. Emerg Med J 2007,24(8):550–552. 10.1136/emj.2006.044461
Lassen JF, Bøtker HE, Terkelsen CJ: Timely and optimal treatment of patients with STEMI. Nat Rev Cardiol 2013,10(1):41–48. 10.1038/nrcardio.2012.156
Sanchez-Ross M, Oghlakian G, Maher J, Patel B, Mazza V, Hom D, Dhruva V, Langley D, Palmaro J, Ahmed S, Kaluski E, Klapholz M: The STAT-MI (ST-Segment Analysis Using Wireless Technology in Acute Myocardial Infarction) trial improves outcomes. J Am Coll Cardiol Intv 2011,4(2):222–227. 10.1016/j.jcin.2010.11.007
Bhalla MC, Mencl F, Gist MA, Wilber S, Zalewski J: Prehospital electrocardiographic computer identification of ST-segment elevation myocardial infarction. Prehosp Emerg Care 2013,17(2):211–216. 10.3109/10903127.2012.722176
Acknowledgements
This work is funded by the European Union through the LiveCity project.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
This work is funded by the European Union through the LiveCity project. The authors report no conflict of interest.
Authors’ contributions
Conception and design of the review was done by AA, PG, and NO. Articles were independently reviewed by AA and NO. PG provided study oversight. All authors participated in the critical review and revision of manuscripts. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Amadi-Obi, A., Gilligan, P., Owens, N. et al. Telemedicine in pre-hospital care: a review of telemedicine applications in the pre-hospital environment. Int J Emerg Med 7, 29 (2014). https://doi.org/10.1186/s12245-014-0029-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12245-014-0029-0