Abstract
Background
A possible downstream effect of high in-hospital bed occupancy is that patients in the emergency department (ED) who would benefit from in-hospital care are denied admission. The present study aimed at evaluating this hypothesis through investigating associations between in-hospital bed occupancy at the time of presentation in the ED and the probability for unplanned 72-hour (72-h) revisits to the ED among patients discharged at index. A second outcome was unplanned 72-h revisits resulting in admission.
Methods
All visits to the ED of a 420-bed emergency hospital in southern Sweden between 1 January 2011 and 31 December 2012, which did not result in admission, death, or transfer to another hospital were included. Revisiting fractions were computed for in-hospital occupancy intervals <85%, 85% to 90%, 90% to 95%, 95% to 100%, 100% to 105%, and ≥105%. Multivariate models were constructed in an attempt to take confounding factors from, e.g., presenting complaints, age, referral status, and triage priority into account.
Results
Included in the study are 81,878 visits. The fraction of unplanned 72-h revisits/unplanned 72-h revisits resulting in admission was 5.8%/1.4% overall, 6.2%/1.4% for occupancy <85%, 6.4%/1.5% for occupancy 85% to 90%, 5.8%/1.4% for occupancy 90% to 95%, 6.0%/1.6% for occupancy 95% to 100%, 5.4%/1.6% for occupancy 100% to 105%, and 4.9%/1.4% for occupancy ≥105%.
In the multivariate models, a trend to lower probability of unplanned 72-h revisits was observed at occupancy ≥105% compared to occupancy <95% (OR 0.88, CI 0.76 to 1.01). No significant associations between in-hospital occupancy at index and the probability of making unplanned 72-h revisits resulting in admission were observed.
Conclusions
The lack of associations between in-hospital occupancy and unplanned 72-h revisits does not support the hypothesis that ED patients are inappropriately discharged when in-hospital beds are scarce. The results are reassuring as they indicate that physicians are able to make good decisions, also while resources are constrained.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
High in-hospital bed occupancy has been associated with prolonged wait in the emergency department (ED) [[1],[2]], spread of hospital-associated infections [[3],[4]], and declining mental health among personnel [[5]]. Simulation studies suggest that periods of demand exceeding bed capacity are more frequent in systems with high-average occupancy [[6],[7]]. Pooling of resources appears to enable larger systems to operate at higher average levels of bed occupancy [[8]]. Application of the principles of queuing theory to hospital systems has shown that variability in admission rate or in length of stay (LOS) in hospital wards is associated with the presence and length of queues for in-hospital beds [[8],[9]].
Capacity planning in many hospital systems relies on average occupancy and average LOS, which makes them susceptible to overflow when these variables vary [[8]]. Several studies highlight the advantages of minimizing variability in elective volumes, to minimize overflows and increase efficiency [[10]–[13]].
Additional simulation studies have shown that performing discharges earlier in the day prevents collision of peak occupancy and peak demand for admissions, which results in lower daily peak and average bed occupancy [[14]–[16]].
A recent study undertaken by the authors revealed an association between high in-hospital bed occupancy and decreased probability of admission from the ED [[17]]. A possible downstream effect is that patients who benefit from in-hospital care are denied admission and instead receive care in the outpatient setting. The objective of the present study was to evaluate this hypothesis through investigating associations between in-hospital bed occupancy at the time of presentation in the ED and the probability of unplanned 72-h revisits to the ED, among patients discharged at their index visit.
Methods
Study design
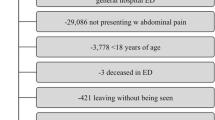
The study was conducted as a retrospective register study, including all visits to the ED of a 420-bed emergency hospital in southern Sweden between 1 January 2011 and 31 December 2012, not resulting in admission, death, or transfer to another hospital. In order to avoid selection bias, no further selection was made.
Setting
The ED of Helsingborg Hospital serves a population of around 250,000. Due to tourism, the population expands to nearly 300,000 during summer. It is one of the four emergency hospitals in the region of Skåne in southern Sweden. The annual ED census is around 60,000, with approximately 15% of patients arriving by ambulance. Patients are registered in the information system Patientliggaren® by a secretary upon arrival. Patients who arrive by ambulance or are referred by a physician gain access to the ED directly after registration. Other patients gain access to the ED in accordance with predefined guidelines, or are further evaluated by a nurse in primary triage. Patients could be referred elsewhere from primary triage (e.g., to primary care). Patients who gain access to the ED undergo secondary triage, which is performed by a nurse. The following is controlled upon secondary triage: Airway, respiratory rate, and SpO2 (pulse oximetry), heart rate, and blood pressure (non-invasive), alertness (Reaction Level Scale (RLS)), and body temperature. The four-level triage system ‘Medical emergency triage and treatment system’ (METTS) was used for secondary triage during the study period. The triage priority is registered in Patientliggaren® directly after the secondary triage. Only physicians may down-prioritize patients (Table 1).
Patients are directed to separate units for Surgery, Orthopedics, Medicine, and Otolaryngology in a triage-to-specialty model after the secondary triage. A complementary unit staffed by emergency physicians capable of handling various complaints except for psychiatric, otolaryngologic, ophthalmologic, and pediatric (medicine) complaints was introduced in 2010 and operates from 8 am to 11 pm daily. There are separate EDs for children with medical conditions (<18 years of age) and for patients with obstetric/gynecologic, psychiatric, or ophthalmologic complaints. Visits to these EDs were not included in the study. Patients with suspected hip fractures or ST elevation myocardial infarction diagnosed in the ambulance bypass the ED in fast tracks and were not included either. Hand surgery, neurosurgery, and thoracic surgery are not available in the hospital. The availability of endovascular surgery and percutaneous coronary intervention is limited from 5 pm to 08 am. Patients with such needs are referred to Skåne University Hospital and were not included in the study.
Physical ED records for patients who are advised to revisit the ED are stored at each specialty desk. Nurses indicate whether a visit is a planned revisit in Patientliggaren® upon patient arrival. Swedish national reimbursement systems are tied to a goal of 80% of visits with ED LOS ≤4 h. At in-hospital bed occupancy close to 100%, the hospital utilizes full-capacity protocols.
Data sources
Data was retrieved from the ED information system Patientliggaren® and the in-hospital information system PASiS®. Data matching was performed by the hospital Informatics Unit using QlikView® software.
Statistics
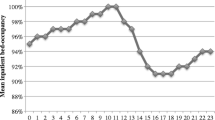
Occupancy was defined as the overall proportion of occupied beds in the hospital at whole-hour intervals. All patients registered in Patientliggaren® during an interval were assigned the same occupancy.
The proportion of visits resulting in an unplanned 72-h revisit was computed for in-hospital occupancy levels of <85%, 85% to 90%, 90% to 95%, 95% to 100%, 100% to 105%, and ≥105%. Subgroup analysis was performed for each specialty unit. Computations were repeated for unplanned 72-h revisits resulting in admission.
Adjusted analysis was performed in an attempt to take confounding factors into account, using binary logistic regression models. Perceived clinical significance governed the decision of screened predictors but was inevitably tainted by data availability. Screened variables were the following: specialty unit, presenting complaint at index, referral status at index, triage priority at index, age group, sex, index presentation on an intense shift, index presentation on a night shift and during weekends, leaving without being seen (LWBS) at index, entering ED via primary triage at index, time to physician at index, and in-hospital occupancy at index. The variable indicating presentation on an intense shift was constructed as a dichotomous variable indicating presentation on one of the 25% of shifts subject to most visits (adjusted for shift type and unit). Night shift was set from 12:00 mn to 08:00 am. Presenting complaint was constructed as a nominal variable indicating the ten most common complaints, using the remainder as reference.
The medicine unit was used as reference among the specialty units. Age was grouped into intervals 0 to 18 years, 18 to 40 years, 40 to 65 years, and ≥65 years. Age ≥65 years was used for reference. Youths in Sweden become of age at 18 and pension age is 65 years.
For the multivariate models, in-hospital occupancy was categorized as <85%, 85% to 90%, 90% to 95%, 95% to 100%, 100% to 105%, and ≥105%. The reference interval was set to <85%. Sensitivity analysis was performed using occupancy <95% as reference.
Predictors were tested for crude association with the outcome before entering the preliminary primary effects model. Associations weaker than P = 0.25, but of clinical importance were still included [[18]]. Multicollinearity testing was performed using Spearman correlation [[19]]. Selection of interaction terms screened for inclusion in the final models was governed by perceived clinical significance and made a priori to analysis. Variables were manually added to the models, rather than stepwise [[18]]. Missing data was indicated by a separate category and included in the models [[20]].
Model fit was evaluated through Nagelkerke’s R2. The association between each predictor and the outcome was addressed by the −2LL and the Wald statistics. The final models were the models with the highest explanatory value and the fewest number of predictors [[19]]. Additionally, the models were screened for influential cases by addressing standardized residuals and Cook’s distance.
Statistical analyses were performed in IBM® SPSS® Statistics 19. Data was anonymized before analysis. The Regional Ethical Review Board in Lund granted ethical approval for the study.
Results
A total of 83,586 ED visits resulting in discharge were registered in Patientliggaren®. Of these, 81,878 did not result in referral to another hospital or death and were hence included in the study.
Unadjusted analysis
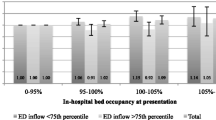
Out of the 81,878 cases, 4,753 cases resulted in an unplanned 72-h revisit, and 1,213 cases resulted in an unplanned 72-h revisit and admission. Proportions of unplanned 72-h revisits/unplanned 72-h revisits resulting in admission were 5.8%/1.5% overall, 6.2%/1.4% for occupancy <85%, 6.4%/1.5% for occupancy 85% to 90%, 5.8%/1.4% for occupancy 90% to 95%, 6.0%/1.6% for occupancy 95% to 100%, 5.4%/1.6% for occupancy 100% to 105%, and 4.9%/1.4% for occupancy ≥105% (Figure 1).
Adjusted analysis
All predictors screened for inclusion in the multivariate models were included, except from time to physician, which was omitted as it violated the assumption of linearity in the logit [[19]]. No significant associations between in-hospital bed occupancy at the index visit and the probability for unplanned 72-h revisits was observed in the model using occupancy <85% as the reference. In the sensitivity analysis, a trend to lower odds for unplanned 72-h revisits was observed among patients being discharged from the ED at occupancy ≥105% relative to at <95%, OR 0.88 (CI 0.76 to 1.01, P = 0.062). No significant associations between in-hospital bed occupancy and the probability for unplanned 72-h revisits resulting in admission were seen in either model. A full account of the models (including coefficients of overall fit) is shown in Additional file 1 (Figures 2 and 3).
Discussion
No significant association between making an index visit to the ED at times of high in-hospital bed occupancy and the probability for making an unplanned 72-h revisit was revealed in the multivariate model using occupancy <85% for reference. In the sensitivity analysis, a trend to lower odds for revisiting was observed among patients being discharged at occupancy ≥105% relative to at <95%. As the hospital rarely operates at occupancy <85%, the sensitivity analysis is considered most stable. The results are supported by the unadjusted analysis, which reveals that 4.9% of cases who were discharged at in-hospital occupancy ≥105% made an unplanned 72-h revisit, compared to 6.2% at occupancy <85%. The overall fraction of unplanned 72-h revisits of 5.8% is higher than the 1.4% to 5.5% described in other studies [[21]–[25]]. No associations between in-hospital bed occupancy and the probability of making an unplanned 72-h revisit resulting in admission were observed, either in the adjusted or unadjusted analyses. The 1.5% of discharged cases who made an unplanned revisit resulting in admission is somewhat higher than the 1.1% to 1.2% reported in other studies [[22],[23]].
One interpretation of the results is that the patients who are discharged from the ED at times of high in-hospital bed occupancy are not sicker than the patients being discharged at other times. Considering our previous results, which showed that the probability for being admitted from the ED is lower at times of high in-hospital occupancy [[17]], the present results suggest that ED physicians make good decisions, also when resources are constrained.
Limitations
The Nagelkerke R2 coefficients (given in Additional file 1) indicate that the variables that were not available for study, e.g., diagnosis and co-morbidity, influenced the outcome in the adjusted analyses. This is also supported by the presence of some influential cases. The relatively large sample size is thought to have balanced some of this effect. As diagnosis and IPLOS vary across specialties, it might have been better to model occupancy in different in-hospital units separately. Unfortunately, this was not possible. The external validity of the results is limited, as the study was performed in a single hospital. The fact that some groups of patients are cared for in separate EDs (children with medical conditions and patients with obstetric/gynecologic, psychiatric, or ophthalmologic complaints) and others bypass the ED in fast tracks (patients with STEMI diagnosed in the ambulance and patients with suspected hip fractures) is important to note when comparing results to other EDs. Another limitation is that patients making an unplanned revisit to another ED in the region are not included in the study, but empirical knowledge suggests that this fraction is small. The authors also recognize that the chosen outcomes are not designed to evaluate the appropriateness of ED discharges. Their selection was motivated by frequent use in other studies and that the Swedish National Board for Health and Welfare made unplanned 72-h revisits subject to national follow-up from April 2013.
Conclusions
The present study yields no support for the hypothesis that ED patients who are discharged from the ED at times of high in-hospital bed occupancy make more unplanned 72-h revisits to the ED than patients who are discharged when bed availability is better. The results are reassuring as they indicate that ED physicians make good decisions, also while resources are constrained. As the present study includes only two endpoints, the reader should interpret it carefully. The implementation of information systems capable of measuring more outcomes on the individual level and tracking patients on their journey across medical specialties is an essential step to allow more accurate description of potential risks.
Additional file
References
Rathlev N, Chessare J, Olshaker J, Obendorfer D, Mehta SD, Rothenhaus T, Crespo S, Magauran B, Davidson K, Shemin R, Lewis K, Becker JM, Fisher L, Guy L, Cooper A, Litvak E: Time series analysis of variables associated with daily mean emergency department length of stay. Ann Emerg Med 2007,49(3):265–271. 10.1016/j.annemergmed.2006.11.007
Cooke M, Wilson S, Roalfe A, Halsall J: Total time in English accident and emergency departments is related to bed occupancy. Emerg Med J 2004,21(5):575–576. 10.1136/emj.2004.015081
Kaier K, Mutters N, Frank U: Bed occupancy rates and hospital-acquired infections—should beds be kept empty? Clin Microbiol Infect 2012,18(10):941–945. 10.1111/j.1469-0691.2012.03956.x
Clements A, Halton K, Graves N, Pettitt A, Morton A, Looke D, Whitby M: Overcrowding and understaffing in modern health-care systems: key determinants in meticillin-resistant Staphylococcus aureus transmission. Lancet Infect Dis 2008,8(7):427–434. 10.1016/S1473-3099(08)70151-8
Virtanen M, Pentti J, Vahtera J, Ferrie JE, Stansfeld SA, Helenius H, Elovainio M, Honkonen T, Terho K, Oksanen T, Kivimäki M: Overcrowding in hospital wards as a predictor of antidepressant treatment among hospital staff. Am J Psychiatry 2008,165(11):1482–1486. 10.1176/appi.ajp.2008.07121929
Bagust A, Place M, Posnett J: Dynamics of bed use in accommodating emergency admissions: stochastic simulation model. Br Med J 1999,318(7203):155–158. 10.1136/bmj.319.7203.155
Bain CA, Taylor PG, McDonell G, Georgiou A: Myths of ideal hospital occupancy. Med J Aust 2010,192(1):42–43.
Morgan I: Managing capacity and demand across the patient journey. J R Coll Physicians Lond Clin Med 2010,10(4):417–418.
Walley P, Silvester K, Steyn R: Managing variation in demand: lessons from the UK National Health Service. J Healthcare Manage 2006,51(5):309–320.
Bekker R, Koeleman P: Scheduling admissions and reducing variability in bed demand. Health Care Manag Sci 2011,14(3):237–249. 10.1007/s10729-011-9163-x
Black S, Proudlove N: Hospital bed utilisation in the NHS and Kaiser Permanente: bed management in the NHS can be improved easily. BMJ 2004,328(7439):582–583. 10.1136/bmj.328.7439.582-c
Gallivan S, Utley M: Modelling admissions booking of elective in-patients into a treatment centre. IMA J Manage Math 2005,16(3):305–315. 10.1093/imaman/dpi024
Fieldston ES, Hall M, Shah SS, Hain PD, Sills MR, Slonim AD, Myers AL, Cannon C, Pati S: Addressing inpatient crowding by smoothing occupancy at children’s hospitals. J Hosp Med 2011,6(8):466–473. 10.1002/jhm.904
Khanna S, Boyle J, Good N, Lind J: Unravelling relationships: hospital occupancy levels, discharge timing and emergency department access block. Emerg Med Australas 2012,24(5):510–517. 10.1111/j.1742-6723.2012.01587.x
Powell E, Khare R, Adams J, Venkatesh A, Van Roo B, Reinhardt G: The relationship between inpatient discharge timing and emergency department boarding. J Emerg Med 2012,42(2):186–196. 10.1016/j.jemermed.2010.06.028
Zhu Z: Impact of different discharge patterns on bed occupancy rate and bed waiting time: a simulation approach. J Med Eng Technol 2011,35(6–7):338–343. 10.3109/03091902.2011.595528
Blom M, Jonsson F, Landin-Olsson M, Ivarsson K: The probability of patients being admitted from the emergency department of Helsingborg general hospital is negatively correlated to in-hospital bed occupancy—an observational study. Int J Emerg Med 2014,7(1):8. 10.1186/1865-1380-7-8
Hosmer DW, Lemeshow S: Model-building strategies and methods for logistic regression. In Applied Logistic Regression. 2nd edition. Edited by: Cressie NAC, Fisher NI, Johnstone IM, Kadane JB, Scott DW, Silverman BW, Smith AFM, Teugels JL, Barnett V, Bradley RA, Hunter JS, Kendall DG. Wiley, Hoboken; 2006:47–142.
Tabachnick B, Fidell LS: Limitations to logistic regression analysis. In Using Multivariate Statistics. 5th edition. Edited by: Hartman S. Pearson, Boston; 2006:437–505.
von Elm E, Altman DG, Egger M, Pocock SJ, Goetzsche PC, Vandenbroucke JP: The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007,370(9596):1453–1457. 10.1016/S0140-6736(07)61602-X
Sauvin G, Freund Y, Saidi K, Riou B, Hausfater P: Unscheduled return visits to the emergency department: consequences for triage. Acad Emerg Med 2013,20(3):E3-E9. 10.1111/acem.12124
Robinson K, Lam B: Early emergency department representations. Emerg Med Australas 2013,25(2):140–146. 10.1111/1742-6723.12048
Hu K, Lu Y, Lin H, Guo H, Foo N: Unscheduled return visits with and without admission post emergency department discharge. J Emerg Med 2012,43(6):1110–1118. 10.1016/j.jemermed.2012.01.062
Wu C, Wang F, Chiang Y, Chiu Y, Lin T, Fu L, Tsai T: Unplanned emergency department revisits within 72 hours to a secondary teaching referral hospital in Taiwan. J Emerg Med 2010,38(4):512–517. 10.1016/j.jemermed.2008.03.039
Kuan W, Mahadevan M: Emergency unscheduled returns: can we do better? Singapore Med J 2009,50(11):1068–1071.
Acknowledgements
Thanks to Harvard Medical Faculty Physicians - Emergency Medicine Consulting for the inspiration and feedback. Thanks to the Laerdal Foundation for the project grants which made the study possible. Thanks to the Swedish Medical Association for the project grants as well. Thanks to Ola Bratt, Helsingborg Hospital; Kristina Forslind, Helsingborg Hospital; and Eva Ekvall-Hansson, Lund University, for proofreading the manuscript. Thanks to Lars Gustavsson, Helsingborg Hospital Informatics Unit, for making data extracts from PASIS and for matching the data. Thanks to Ingemar Petersson, Epi-Centrum Skåne, for his input regarding the ‘Statistics’ section and the validity of the dataset.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MB, FJ, KI, and MLO designed the study protocol together. MB gathered and matched the data and carried out the statistical analyses and the writing of the draft. All authors proofread repeated versions of the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
12245_2014_25_MOESM1_ESM.docx
Additional file 1:A full account of the models (including coefficients of overall fit). Table S2: fraction of unplanned 72-h revisits (rev) for different levels of in-hospital occupancy. Table S3: data from adjusted analysis, with in-hospital bed occupancy <85% used for reference. Table S4: data from adjusted analysis, with in-hospital bed occupancy <95% used for reference. (DOCX 61 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Blom, M.C., Jonsson, F., Landin-Olsson, M. et al. Associations between in-hospital bed occupancy and unplanned 72-h revisits to the emergency department: a register study. Int J Emerg Med 7, 25 (2014). https://doi.org/10.1186/s12245-014-0025-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12245-014-0025-4