Abstract
Background
Previous studies have suggested that exposure to air pollution may increase stroke risk, but the results remain inconsistent. Evidence of more recent studies is highly warranted, especially gas air pollutants.
Methods
We searched PubMed, Embase, and Web of Science to identify studies till February 2020 and conducted a meta-analysis on the association between air pollution (PM2.5, particulate matter with aerodynamic diameter less than 2.5 μm; PM10, particulate matter with aerodynamic diameter less than 10 μm; NO2, nitrogen dioxide; SO2, sulfur dioxide; CO, carbon monoxide; O3, ozone) and stroke (hospital admission, incidence, and mortality). Fixed- or random-effects model was used to calculate pooled odds ratios (OR)/hazard ratio (HR) and their 95% confidence intervals (CI) for a 10 μg/m3 increase in air pollutant concentration.
Results
A total of 68 studies conducted from more than 23 million participants were included in our meta-analysis. Meta-analyses showed significant associations of all six air pollutants and stroke hospital admission (e.g., PM2.5: OR = 1.008 (95% CI 1.005, 1.011); NO2: OR = 1.023 (95% CI 1.015, 1.030), per 10 μg/m3 increases in air pollutant concentration). Exposure to PM2.5, SO2, and NO2 was associated with increased risks of stroke incidence (PM2.5: HR = 1.048 (95% CI 1.020, 1.076); SO2: HR = 1.002 (95% CI 1.000, 1.003); NO2: HR = 1.002 (95% CI 1.000, 1.003), respectively). However, no significant differences were found in associations of PM10, CO, O3, and stroke incidence. Except for CO and O3, we found that higher level of air pollution (PM2.5, PM10, SO2, and NO2) exposure was associated with higher stroke mortality (e.g., PM10: OR = 1.006 (95% CI 1.003, 1.010), SO2: OR = 1.006 (95% CI 1.005, 1.008).
Conclusions
Exposure to air pollution was positively associated with an increased risk of stroke hospital admission (PM2.5, PM10, SO2, NO2, CO, and O3), incidence (PM2.5, SO2, and NO2), and mortality (PM2.5, PM10, SO2, and NO2). Our study would provide a more comprehensive evidence of air pollution and stroke, especially SO2 and NO2.
Similar content being viewed by others
Introduction
Stroke, characterized by acute cerebral blood circulation disorder, is caused by artery stenosis, occlusion, or rupture caused by various inducing factors in patients with cerebrovascular diseases [1]. Stroke has become a leading contributor to the global burden of disease and the second leading cause of death worldwide [2, 3]. According to the Global Burden of Disease Study (GBD) report, there were approximately 80.1 million stroke patients, and 5.5 million deaths were attributed to stroke in 2016 globally [4]. Considering stroke is characterized with high incidence, high mortality, and contribute to severe burden disease, identifying potential risk factor of stroke is of great significance for public health. In parallel, air pollution has also been regarded as one of the major environmental problems and a risk factor of many cardiovascular diseases (CVD), including stroke [5]. GBD 2019 showed that air pollution was globally the sixth leading cause of stroke death during 1990 to 2017, and 28.1% disability-adjusted life years (DALYs) of stroke attribute to environmental factors exposure [6, 7].
Air pollution is the most significant environmental risk factor for all-cause mortality [8]. Increasing number of human epidemiologic studies has been conducted to assess the potential association between air pollution exposure and stroke admission, incidence, and mortality in recent years. However, the results were inconsistent, and the associations between exposure to air pollution and stroke have not been fully understood. Some studies reported positive association between air pollution exposure and stroke hospital admission/incidence/mortality, whereas others did not [4, 9,10,11,12,13,14]. For example, Huang et al. 2019 indicated that exposure to PM2.5 was associated with increased stroke incidence and the adjusted risk ratio (RR) was 1.130 (95%CI: 1.090, 82 1.170) for each increase of 10 μg/m3 in n PM2.5 concentration [4]. The adjusted risk ratio (RR) was 1.130 (95% CI 1.090, 1.170) for each increase of 10 μg/m3 in PM2.5 concentration, while Wing et al. suggested no association was found between PM2.5 exposure and stroke incidence (RR = 0.950, 95% CI 0.710, 1.280) [11]. Previous meta-analyses have explored the associations between air pollution exposure and stroke [15,16,17,18,19]. However, these studies were mainly focused on the studies of particulate matter (PM2.5, particulate matter with aerodynamic diameter less than 2.5 μm; PM10, particulate matter with aerodynamic diameter less than 10 μm) and stroke outcomes [16,17,18,19]; results of gas air pollutants (NO2, nitrogen dioxide; SO2, sulfur dioxide; CO, carbon monoxide; O3, ozone) were scarce. Moreover, to the best of our knowledge, more than 30 studies exploring the association between air pollution exposure and stroke, especially conducted from the multi-city level and with large sample sizes, were published after the most recent meta-analysis. The more recent and comprehensive studies should be included in the meta-analysis to conclude an updated pooled effect estimate.
We therefore conducted an updated systematic review and meta-analysis to assess the association between 6 main air pollutants (PM2.5, PM10, NO2, SO2, CO, and O3) and 3 stroke outcomes (hospital admission, incidence, and mortality). This systematic review and meta-analysis was performed according to the guidelines of the Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) criteria (Table S1).
Methods
Search strategy
Literature was searched in three databases (PubMed, Embase, and Web of Science), with published date until 1 February 2020. The search strategy was pairwise of combinations of terms concerning air pollution (e.g., air pollution, particulate matter, particles, PM2.5, PM10, nitrogen oxides (NOx), NO2, SO2, CO, and O3) and stroke (e.g., stroke, cerebrovascular disease, cerebrovascular disorder, cerebral hemorrhage, cerebral infarction, subarachnoid hemorrhage).
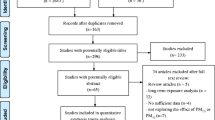
We first selected articles by screening titles and abstracts and then the full texts of potentially eligible studies were further evaluated. Reference lists of all the included studies were also manually searched. Literature selection was finished by two independent authors (ZP N and FF L), and conflicts between the two authors were resolved by discussing with an arbitrator (H X).
Inclusion and exclusion criteria
Articles that met the following criteria were included: (1) provided quantitative measure of the associations between air pollution exposure with stroke admission, incidence, and/or mortality (relative risk (RR), odds ratio (OR), or hazard ratio (HR), and their 95% confidence interval (95%CI); (2) cohort, cross-sectional, time series, cross-sectional, case-control, case-crossover, or panel studies; (3) focused on outdoor (ambient) air pollution exposure but not indoor air pollution; (4) original peer-reviewed human subject research studies; (5) published in English. Studies were excluded if they were (1) toxicological studies, summaries, or reviews, and (2) articles without effect estimates after contacting the authors. In addition, for more than one article conducted from the same population, only the most recent studies were included.
Data extraction
Data were extracted from all eligible studies, including the following: (1) study characteristics (first author, published year, study location, and period); (2) study population (sample size, proportion of males, range of age, mean age); (3) outcome (type of stroke and outcome was admission, incidence, and/or mortality); (4) air pollution assessment method and increment of air pollution used in effect estimates (per interquartile range (IQR), standard deviation (SD), or per 10 μg/m3); (5) effect estimates of the association between air pollution and stroke risk (OR, RR, HR with 95% CI). The effect estimates of single-pollutant model, generally called “main model” or “fully adjusted model,” were extracted [20].
Quality assessment
Two authors (ZP N and FF L) worked independently, and inconsistencies in quality assessment were resolved through discussion. We employed the Newcastle-Ottawa Scale (NOS) to evaluate the quality of included studies. The NOS Tool has designed 8 items to assess the critical appraisal of the potential risk of bias. Total score of NOS ranged from 0–9. Study score higher than or equal to 7 was regarded as high-quality; otherwise, the study was regarded as “low quality” [21].
Statistical analyses
This meta-analysis focused on examining the association between air pollution and three stroke outcomes, including admission, incidence, and/or mortality. We extracted effect estimates (OR, HR, RR, and 95%CI) from individual studies and then converted them into a standardized form of per 10 μg/m3 increases in air pollution. The significance of the pooled OR, RR, or HR was determined by the Z test [22], and p value less than 0.05 was considered statistically significant. Standard error (SE) for each effect estimate was calculated by using the formula: (upper limit − lower limit)/3.92.
Heterogeneity among studies was evaluated using I2 statistics and Q test [23]. If the values of I2 > 50% or p < 0.01, the heterogeneity was “high” and random effect model was used to pool estimates. Otherwise, heterogeneity was considered as “low or moderate,” and fixed-effect model was used to pool estimates.
Begg’s test and Egger’s test were conducted to assess publication bias. The influence of individual studies on the pooled estimates was examined by removing each study from the analysis one by one. Moreover, we also performed sensitivity analysis and subgroup analysis to evaluate if the exposure period would change the significance of the pooled results. Because long-term studies were limited, sensitivity analysis was conducted by omitting long-term exposure (cohort) studies. Subgroup analysis was only performed if the number of short-term exposure studies or long-term exposure studies was more than 3. Publication bias and sensitivity analysis were only performed if the number of included studies was more than 5. All statistical analysis was performed in Stata version 15.0 (StataCorp, College Station, TX, USA).
Results
Literature search and characteristics of included studies
After removing duplicates, 737 records were identified in the initial literature search. By reviewing title and abstracts, 93 studies were downloaded for full-text reading. According to the inclusion and exclusion criteria, a total of 68 studies were included in our meta-analysis (Fig. 1).
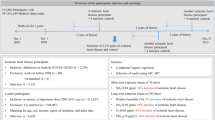
Table 1 provides the characteristics of 68 studies included in meta-analysis. As for air pollution involved in the study, there were 26 studies that reported the association between air pollution exposure and stroke hospital admission, 19 reported air pollution exposure and stroke incidence, 19 reported air pollution exposure and stroke mortality, and 3 reported both stroke incidence and mortality. The sample size of included studies ranged between 407 and 8,834,533; more than 23 million participants were included in meta-analysis eventually. Furthermore, the studies included were conducted from 18 countries. Time-series and cross-sectional were the most commonly adopted study designs. In our meta-analysis, all 68 included studies were considered as “high quality,” and the average NOS score was 8.26 for all studies (Table S2)
.
Air pollution and stroke hospital admission
A total of 29 studies were performed to assess the association for air pollution and stroke hospital admission, and the results were inconsistent. Most studies showed a positive correlation between exposure to air pollution and the risk of hospital admission for stroke. In meta-analysis, we enrolled 13 studies on PM2.5, 11 studies on PM10 and NO2, 10 studies on SO2 and O3, and 6 studies on CO with stroke hospital admission and suggested an increased stroke hospital admission risk after air pollution exposure. The pooled odds ratio (OR) of stroke with a 10 μg/m3 increase in PM2.5, PM10, SO2, NO2, CO, and O3 was 1.008 (95% CI 1.005, 1.011), 1.004 (95% CI 1.001, 1.006), 1.013 (95% CI 1.007, 1.020), 1.023 (95% CI 1.015, 1.030), 1.000 (95% CI 1.000, 1.001), and 1.002 (95% CI 1.000, 1.003), respectively (Table 2, Figure S1-S6). Heterogeneity among studies was significant (I2 ≥ 50%, p < 0.001).
Air pollution and stroke incidence
Twenty-three studies have investigated the association of air pollution on stroke incidence (Table 1). For meta-analysis, we extracted 18 studies on PM2.5, 13 studies on PM10, 10 studies on O3, 7 studies on NO2, and 4 studies on SO2 and CO. Ten of these studies suggested increased risks for stroke incidence for at least one of the investigated pollutants. Meta-analysis showed that exposure to PM2.5, SO2, and NO2 was associated with increased risks of stroke incidence, and the pooled HR with a 10 μg/m3 increase was 1.048 (95% CI 1.020, 1.076), 1.002 (95% CI 1.000, 1.003), 1.002 (95% CI 1.000, 1.003), respectively. However, no significant differences were found in associations of PM10, CO, O3, and stroke incidence (Table 3, Figure S7-S12).
Air pollution and stroke mortality
Twenty-two population-based studies have explored the association for exposure to air pollution and stroke mortality. As for meta-analysis, 11 articles on PM2.5, 10 articles on NO2, 9 articles on PM10, 6 articles on O3, and 4 articles on CO exposure were included. Meta-analysis showed that exposure to ambient PM2.5 (OR = 1.008 95% CI 1.005, 1.012, per 10 μg/m3 increment), PM10 (OR = 1.006, 95% CI 1.003, 1.010, per 10 μg/m3 increment), SO2 (OR = 1.006, 95% CI 1.005, 1.008, per 10 μg/m3 increment), and NO2 (OR = 1.009, 95% CI 1.003, 1.016, per 10 μg/m3 increment) was associated with increased risks of mortality due to stroke. No significant difference was shown in association between CO, O3 exposure, and stroke mortality (Table 4, Figure S13-S18).
Publication bias and sensitivity analysis
Publication bias of studies on PM10 exposure and stroke hospital admission may exist, since p values of Begg’s test were less than 0.05. Publication bias of studies was remarkable in association of exposure to PM2.5 and O3 and stroke incidence according to funnel plots and Egger’s test. For PM2.5 and stroke mortality, the p value of Egger’s test was 0.009, suggesting publication bias may exist. Other publication bias test indicated that no substantial publication bias of studies was observed according to funnel plots, Begg’s test, and Egger’s test (Table S3, Figure S19-34).
Sensitivity analysis showed that the relation of exposure to CO and stroke hospital admission might be influenced by Tian et al.’s study [10]. And the association between exposure to NO2 and stroke incidence may be influenced by Dong et al.’s study [1]. The pooled OR of exposure to air pollution and stroke mortality might be influenced by some studies (PM2.5: Wang et al.’s study [33]; O3: Yin et al.’s study [37]). We recalculated the pooled OR/HR and 95% CI after removing those studies (Table S3). Due to limited studies after excluding those studies, the pooled estimated effects of SO2 and stroke incidence and O3 and stroke mortality were not recalculated. Other sensitivity analyses indicated that excluding each individual study did not change the results, suggesting the results of the meta-analysis were stable (Table S4, Figure S35-50). Sensitivity analyses by exposure period found that the pooled effect estimates were not changed significantly after excluding the long-term (cohort) studies (Table S5). Subgroup analysis suggested that both short-term and long-term exposure to air pollution would increase the risk of stroke incidence (PM2.5, PM10, and NO2) and mortality (NO2) (Table S6).
Discussion
We conducted a systematic review and meta-analysis of 68 epidemiological studies and performed a comprehensive evaluation on exposure ambient air pollution and stroke, which were conducted from more than 23 million participants. Most studies suggested that exposure to a higher level of air pollution was associated with increased stroke risk. Meta-analysis showed that exposures to air pollutants were associated with increased risk of stroke hospital admission (PM2.5, PM10, SO2, NO2, CO, and O3), incidence (PM2.5, SO2, and NO2), and mortality (PM2.5, PM10, SO2, and NO2). Although the high heterogeneity may reduce the credibility of the pooled evidence to some extent, the large number of studies included and the consistency of the results indicated that our conclusions were credible to some extent.
The positive associations between exposure to PM2.5, PM10, SO2, NO2, CO, and O3, and stroke hospital admission were observed in other meta-analysis. Yang et al. meta-analyzed 34 case-crossover and time series studies and reported significant associations for PM10 (per 10 μg/m3 increment: RR = 1.007, 95% CI 1.001, 1.013) and O3 (per 10 ppb increment: RR = 1.036, 95% CI 1.016, 1.056), but non-significant association for PM2.5, SO2, NO2, and CO [15]. The meta-analysis performed by Yang et al. was not consistent with our current study completely, which might be caused by the different number of the included studies. To our knowledge, more than 16 studies have been published after 2014, and studies included in Yang et al.’s study were mainly conducted in Europe and North America. Data from more recent studies, especially low- and middle-income countries were not considered. Moreover, many studies conducted from the multi-city level and with large sample sizes have been published in recent years, which were more likely to find a significant association between air pollution and stroke hospital admission. For example, Tian et al. performed a time-series of more than 2 million hospital admissions for ischemic stroke in 172 cities in China and suggested that elevated incidence of ischemic stroke hospital admissions was associated with exposure to higher level of PM2.5 (RR = 1.003, 95% CI 1.002, 1.005, per 10 μg/m3 increment), SO2 (RR = 1.013, 95% CI 1.011, 1.017, per 10 μg/m3 increment), and NO2 (RR = 1.018, 95% CI 1.015, 1.022, per 10 μg/m3 increment) [24].
Three meta-analyses were conducted to examine the association between exposure to particulate matter (PM2.5 and PM10) and stroke incidence, whereas no meta-analysis of gas air pollutants was published before the current study. Li et al. performed a meta-analysis to explore the association between PM10 and stroke incidence in time-series studies and case-crossover studies. These studies indicated that PM10 was not associated with stroke incidence in the time-series design (HR = 1.002, 95% CI 0.999, 1.005, per 10 μg/m3 increment), but significantly associated in case-crossover studies (HR = 1.028, 95% CI 1.001, 1.057, per 10 μg/m3 increment). Meanwhile, PM2.5 exposure was related to an increased risk of stroke incidence in time-series design (HR = 1.006, 95% CI 1.002, 1.010, per 10 μg/m3 increment), but no significant association in case-crossover studies (HR = 1.016, 95% CI 0.937, 1.097, per 10 μg/m3 increment) [16]. Only 12 studies published before 2010 were included in Li et al.’s study. We updated the literature search up to 2020, which generated more than 10 studies. Moreover, Li et al. separately analyzed the data from time-series and case-crossover studies, which would reduce the number of studies calculated the pooled estimates. These might explain the inconsistency in between our study and Li et al.’s study. Yu et al. updated the literature search before 2012 and identified 19 studies [19]. Yu et al. found that exposure to PM10 was associated with an increased risk of stroke incidence (HR = 1.004, 95% CI 1.001, 1.008, per 10 μg/m3 increment), but exposure to PM2.5 was not significantly associated with stroke incidence (HR = 0.999, 95% CI 0.994, 1.003, per 10 μg/m3 increment) [19]. The results of these published meta-analyses were not exactly the same as our study, which might be due to more than 15 studies published after Yu et al.’s study. Moreover, we conducted a meta-analysis of gas air pollutants and stroke incidence and found that exposure to a higher level of SO2 and NO2 was associated with higher risk of stroke incidence, which may fill the gap of meta-analysis of gas air pollutants and stroke incidence. We also found that compared to short-term exposure, long-term exposure to air pollution may be associated with a higher risk of stroke incidence (PM2.5, PM10, and NO2), which may be explained by different pathophysiological pathways.
Studies investigating the association between exposure to air pollution and stroke mortality have been partly analyzed in two meta-analysis [15, 17]. Yang et al. evaluated the association between all 6 pollutants and suggested that stroke mortality increased 1.34% (95% CI 0.27, 2.42) per 10 μg/m3 increase in PM2.5, 0.65% (95% CI 0.54, 0.77) per 10 μg/m3 increase in PM10, 2.45% (95% CI 1.83, 3.07) per 10 parts per billion (ppb) increase in SO2, 7.78% (95% CI 4.49, 11.60) per 1 ppm increase in CO, and 1.50% (95% CI 0.37, 2.63) per 10 ppb increase in NO2, respectively [15]. Consistent with Yang et al.’s study, our meta-analysis also indicated that exposure to a higher level of PM2.5, PM10, SO2, and NO2 was related to higher risk of stroke mortality. No association was observed in both our study and Yang et al.’s study. However, Yang et al. reported a positive association in CO, whereas our study did not, which may be explained by the limited number of included studies. Scheers et al. performed a meta-analysis of exposure to PM10 and stroke events (mortality and incidence) and suggested that exposure to PM10 was positively associated with overall stroke events (mortality and incidence) (HR = 1.061, 95% CI 1.018, 1.105), but no significant association were observed in stroke mortality (HR = 1.080, 95% CI 0.992, 1.177) [17]. Inconsistency of Scheers et al.’s study and current study could be explained that Scheers et al.’s study included the studied estimated exposure to PM10 from studies using PM2.5, which may cause estimation bias to some extent.
Although accurate mechanisms of air pollution exposure and stroke remain unclear, several pathways including systemic inflammation, oxidative stress, thrombosis, and vascular endothelial dysfunction have been proposed [1, 9, 15, 82]. Vascular function injury may be central to mechanisms for air pollution-related stroke, which could lead to raised level of blood pressure and plasma viscosity [26]. It has been showed that exposure to air pollution was associated with increased thrombosis and vascular endothelial dysfunction by provoking oxidative stress and releasing systemic inflammatory cytokines [83]. Moreover, evidence also suggested that exposure to air pollution can lead to dysfunction of the autonomic system, which has been found as the major pathway that could result in air pollution-related adverse cardiovascular outcomes, such as stroke [84]. In addition, stroke status may aggravate the susceptibility of population to air pollution and increase the adverse cardiovascular effects of air pollution circularly [62].
A major strength of our meta-analysis is that our systematic review and meta-analysis covered six main air pollutants (PM2.5, PM10, NO2, SO2, CO, O3) and a rich set of stroke outcomes (hospital admission, incidence, and mortality), which may be difficult to obtain from individual studies or isolated reviews or meta-analyses. However, some limitations should be acknowledged. Firstly, high heterogeneity existed in some meta-analysis, which may be due to different study designs, difference in exposure assessment method and population demographics, and the varied covariable adjustment strategies in different studies. Secondly, our study failed to perform the association between different subtypes of stroke (ischemic stroke, hemorrhagic stroke) and air pollution exposure separately because most included studies (48 out of 68 articles) did not report subtypes of stroke or results of ischemic stroke and hemorrhagic stroke specifically. Finally, the correlation between different air pollutants was not examined in our study because different air pollutants were controlled in different studies, and the results of those studies could not be pooled directly.
Conclusion
Our study demonstrated that exposure to air pollution was positively associated with an increased risk of stroke hospital admission (PM2.5, PM10, SO2, NO2, CO, and O3), incidence (PM2.5, SO2, and NO2), and mortality (PM2.5, PM10, SO2, and NO2). Given the great global burden of stroke and air pollution, our findings could provide some scientific evidence to accurate prevention and treatment of stroke and air pollution exposure.
Availability of data and materials
All data described, analyzed, or discussed in this review are included in cited publications.
Abbreviations
- PM2.5 :
-
Particulate matter with aerodynamic diameter less than 2.5 μm
- PM10 :
-
Particulate matter with aerodynamic diameter less than 10 μm
- NO2 :
-
Nitrogen dioxide
- SO2 :
-
Sulfur dioxide
- CO:
-
Carbon monoxide
- O3 :
-
Ozone
- OR:
-
Odds ratio
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- e.g.:
-
For example
- GBD:
-
The Global Burden of Disease Study
- CVD:
-
Cardiovascular diseases
- DALYs:
-
Disability-adjusted life years
- RR:
-
Risk ratio
- PRISMA:
-
The Preferred Reporting Items for Systematic Review and Meta-analyses
- NOx:
-
Nitrogen oxides
- IQR:
-
Interquartile range
- SD:
-
Standard deviation
- NOS:
-
The Newcastle-Ottawa Scale
- SE:
-
Standard error
- China-PAR:
-
Atherosclerotic Cardiovascular Disease Risk in China (China-PAR) project
- ICH:
-
Intracerebral hemorrhage
- IS:
-
Ischemic stroke
- REGARDS cohort:
-
Reasons for Geographic and Racial Differences in Stroke Cohort
- PPS:
-
Primary prevention study
- CNBSS:
-
Canadian National Breast Screening Study
- HS:
-
Hemorrhagic stroke
- ESCAPE Project:
-
The European Study of Cohorts for Air Pollution Effects
- AOD:
-
Aerosol optic depth
- ISSeP:
-
The Scientific Institute of Public Services
- CMAQ:
-
Community Multiscale Air Quality model
- QOED:
-
The Qingyue Open Environmental Data Center
- USEPA:
-
The US Environmental Protection Agency
- HBM:
-
Hierarchical Bayesian Model
- EPA:
-
The Taiwanese Environmental Protection Administration
- EPD:
-
The Environmental Protection Department
- LUR:
-
Land-use regression model
- IDW:
-
Inverse distance weighting
References
Dong H, Yu Y, Yao S, Lu Y, Chen Z, Li G, et al. Acute effects of air pollution on ischaemic stroke onset and deaths: a time-series study in Changzhou, China. BMJ Open. 2018;8. https://doi.org/10.1136/bmjopen-2017-020425.
Ekker MS, Verhoeven JI, Vaartjes I, Jolink WMT, Klijn CJM, de Leeuw F-E. Association of stroke among adults aged 18 to 49 years with long-term mortality. JAMA. 2019;321:2113–23. https://doi.org/10.1001/jama.2019.6560.
Wang Y, Jiao Y, Nie J, O'Neil A, Huang W, Zhang L, et al. Sex differences in the association between marital status and the risk of cardiovascular, cancer, and all-cause mortality: a systematic review and meta-analysis of 7,881,040 individuals. Glob Health Res Policy. 2020;5:4. https://doi.org/10.1186/s41256-020-00133-8.
Huang K, Liang F, Yang X, Liu F, Li J, Xiao Q, et al. Long term exposure to ambient fine particulate matter and incidence of stroke: prospective cohort study from the China-PAR project. BMJ 2019. doi:10.1136/bmj.l6720. doi:https://doi.org/10.1136/bmj.l6720.
Guo P, Wang Y, Feng W, Wu J, Fu C, Deng H, et al. Ambient air pollution and risk for ischemic stroke: a short-term exposure assessment in South China. Int J Environ Res Public Health. 2017;14. https://doi.org/10.3390/ijerph14091091.
Avan A, Digaleh H, Di Napoli M, Stranges S, Behrouz R, Shojaeianbabaei G, et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019;17:191. https://doi.org/10.1186/s12916-019-1397-3.
GBD. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:439–58. https://doi.org/10.1016/S1474-4422(19)30034-1.
Karan A, Ali K, Teelucksingh S, Sakhamuri S. The impact of air pollution on the incidence and mortality of COVID-19. Glob Health Res Policy. 2020;5:39. https://doi.org/10.1186/s41256-020-00167-y.
Chen R, Yin P, Meng X, Liu C, Wang L, Xu X, et al. Fine particulate air pollution and daily mortality. A nationwide analysis in 272 Chinese cities. Am J Respir Crit Care Med. 2017;196:73–81. https://doi.org/10.1164/rccm.201609-1862OC.
Tian Y, Liu H, Zhao Z, Xiang X, Li M, Juan J, et al. Association between ambient air pollution and daily hospital admissions for ischemic stroke: a nationwide time-series analysis. PLoS Med. 2018;15:e1002668. https://doi.org/10.1371/journal.pmed.1002668.
Wing JJ, Adar SD, Sánchez BN, Morgenstern LB, Smith MA, Lisabeth LD. Short-term exposures to ambient air pollution and risk of recurrent ischemic stroke. Environ Res. 2017;152:304–7. https://doi.org/10.1016/j.envres.2016.11.001.
Tian Y, Liu H, Wu Y, Si Y, Song J, Cao Y, et al. Association between ambient fine particulate pollution and hospital admissions for cause specific cardiovascular disease: time series study in 184 major Chinese cities. BMJ. 2019;367:l6572. https://doi.org/10.1136/bmj.l6572.
Montresor-López JA, Yanosky JD, Mittleman MA, Sapkota A, He X, Hibbert JD, et al. Short-term exposure to ambient ozone and stroke hospital admission: a case-crossover analysis. J Exposure Sci Environ Epidemiol. 2016;26:162–6. https://doi.org/10.1038/jes.2015.48.
Yu Y, Dong H, Yao S, Ji M, Yao X, Zhang Z. Protective effects of ambient ozone on incidence and outcomes of ischemic stroke in Changzhou, China: a time-series study. Int J Environ Res Public Health. 2017;14. https://doi.org/10.3390/ijerph14121610.
Yang WS, Wang X, Deng Q, Fan WY, Wang WY. An evidence-based appraisal of global association between air pollution and risk of stroke. Int J Cardiol. 2014;175:307–13. https://doi.org/10.1016/j.ijcard.2014.05.044.
Li XY, Yu XB, Liang WW, Yu N, Wang L, Ye XJ, et al. Meta-analysis of association between particulate matter and stroke attack. CNS Neurosci Ther. 2012;18:501–8. https://doi.org/10.1111/j.1755-5949.2012.00325.x.
Scheers H, Jacobs L, Casas L, Nemery B, Nawrot TS. Long-term exposure to particulate matter air pollution is a risk factor for stroke: meta-analytical evidence. Stroke. 2015;46:3058–66. https://doi.org/10.1161/STROKEAHA.115.009913.
Wang Y, Eliot MN, Wellenius GA. Short-term changes in ambient particulate matter and risk of stroke: a systematic review and meta-analysis. J Am Heart Assoc. 2014;3. https://doi.org/10.1161/JAHA.114.000983.
Yu X-B, Su J-W, Li X-Y, Chen G. Short-term effects of particulate matter on stroke attack: meta-regression and meta-analyses. PLoS ONE. 2014;9:e95682. https://doi.org/10.1371/journal.pone.0095682.
Liu F, Chen G, Huo W, Wang C, Liu S, Li N, et al. Associations between long-term exposure to ambient air pollution and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Environ Pollut. 2019;252:1235–45. https://doi.org/10.1016/j.envpol.2019.06.033.
Chen X, Liu F, Niu Z, Mao S, Tang H, Li N, et al. The association between short-term exposure to ambient air pollution and fractional exhaled nitric oxide level: a systematic review and meta-analysis of panel studies. Environ Pollut. 2020;265. https://doi.org/10.1016/j.envpol.2020.114833.
Yang BY, Fan S, Thiering E, Seissler J, Nowak D, Dong GH, et al. Ambient air pollution and diabetes: a systematic review and meta-analysis. Environ Res. 2020;180:108817. https://doi.org/10.1016/j.envres.2019.108817.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. https://doi.org/10.1002/sim.1186.
Tian Y, Liu H, Xiang X, Zhao Z, Juan J, Li M, et al. Ambient coarse particulate matter and hospital admissions for ischemic stroke. Stroke. 2019;50:813–9. https://doi.org/10.1161/strokeaha.118.022687.
Chen C, Wang X, Lv C, Li W, Ma D, Zhang Q, et al. The effect of air pollution on hospitalization of individuals with respiratory and cardiovascular diseases in Jinan, China. Medicine. 2019;98. https://doi.org/10.1097/md.0000000000015634.
Chen G, Wang A, Li S, Zhao X, Wang Y, Li H, et al. Long-term exposure to air pollution and survival after ischemic stroke. Stroke. 2019;50:563–70. https://doi.org/10.1161/strokeaha.118.023264.
Xue T, Guan T, Liu Y, Zheng Y, Guo J, Fan S, et al. A national case-crossover study on ambient ozone pollution and first-ever stroke among Chinese adults: interpreting a weak association via differential susceptibility. Sci Total Environ. 2019;654:135–43. https://doi.org/10.1016/j.scitotenv.2018.11.067.
Qian Y, Yu H, Cai B, Fang B, Wang C. Association between incidence of fatal intracerebral hemorrhagic stroke and fine particulate air pollution. Environ Health Prev Med. 2019;24:38. https://doi.org/10.1186/s12199-019-0793-9.
Zhong H, Shu Z, Zhou Y, Lu Y, Yi B, Tang X, et al. Seasonal effect on association between atmospheric pollutants and hospital emergency room visit for stroke. J Stroke Cerebrovasc Dis. 2018;27:169–76. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.08.014.
Vivanco-Hidalgo RM, Wellenius GA, Basagaña X, Cirach M, González AG, Ceballos P, et al. Short-term exposure to traffic-related air pollution and ischemic stroke onset in Barcelona, Spain. Environ Res. 2018;162:160–5. https://doi.org/10.1016/j.envres.2017.12.024.
Yitshak-Sade M, Bobb JF, Schwartz JD, Kloog I, Zanobetti A. The association between short and long-term exposure to PM2.5 and temperature and hospital admissions in New England and the synergistic effect of the short-term exposures. Sci Total Environ. 2018;639:868–75. https://doi.org/10.1016/j.scitotenv.2018.05.181.
Liu C, Yin P, Chen R, Meng X, Wang L, Niu Y, et al. Ambient carbon monoxide and cardiovascular mortality: a nationwide time-series analysis in 272 cities in China. Lancet Planetary Health. 2018;2:e12–e8. https://doi.org/10.1016/s2542-5196(17)30181-x.
Wang X, Qian Z, Wang X, Hong H, Yang Y, Xu Y, et al. Estimating the acute effects of fine and coarse particle pollution on stroke mortality of in six Chinese subtropical cities. Environ Pollut. 2018;239:812–7. https://doi.org/10.1016/j.envpol.2018.04.102.
Collart P, Dubourg D, Levêque A, Sierra NB, Coppieters Y. Short-term effects of nitrogen dioxide on hospital admissions for cardiovascular disease in Wallonia, Belgium. Int J Cardiol. 2018;255:231–6. https://doi.org/10.1016/j.ijcard.2017.12.058.
Chen C, Zhu P, Lan L, Zhou L, Liu R, Sun Q, et al. Short-term exposures to PM(2.5) and cause-specific mortality of cardiovascular health in China. Environ Res. 2018;161:188–94. https://doi.org/10.1016/j.envres.2017.10.046.
Wang L, Liu C, Meng X, Niu Y, Lin Z, Liu Y, et al. Associations between short-term exposure to ambient sulfur dioxide and increased cause-specific mortality in 272 Chinese cities. Environ Int. 2018;117:33–9. https://doi.org/10.1016/j.envint.2018.04.019.
Yin P, Chen R, Wang L, Meng X, Liu C, Niu Y, et al. Ambient ozone pollution and daily mortality: a nationwide study in 272 Chinese cities. Environ Health Perspect. 2017;125:117006. https://doi.org/10.1289/ehp1849.
Ha S, Männistö T, Liu D, Sherman S, Ying Q, Mendola P. Air pollution and cardiovascular events at labor and delivery: a case-crossover analysis. Ann Epidemiol. 2017;27:377–83. https://doi.org/10.1016/j.annepidem.2017.05.007.
Huang F, Luo Y, Tan P, Xu Q, Tao L, Guo J, et al. Gaseous air pollution and the risk for stroke admissions: a case-crossover study in Beijing, China. Int J Environ Res Public Health. 2017;14. https://doi.org/10.3390/ijerph14020189.
Liu H, Tian Y, Xu Y, Huang Z, Huang C, Hu Y, et al. Association between ambient air pollution and hospitalization for ischemic and hemorrhagic stroke in China: a multicity case-crossover study. Environ Pollut. 2017;230:234–41. https://doi.org/10.1016/j.envpol.2017.06.057.
Liu H, Tian Y, Xu Y, Zhang J. Ambient particulate matter concentrations and hospitalization for stroke in 26 Chinese cities: a case-crossover study. Stroke. 2017;48:2052–9. https://doi.org/10.1161/strokeaha.116.016482.
McClure LA, Loop MS, Crosson W, Kleindorfer D, Kissela B, Al-Hamdan M. Fine particulate matter (PM(2.5)) and the risk of stroke in the REGARDS cohort. J Stroke Cerebrovasc Dis. 2017;26:1739–44. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.03.041.
Tian Y, Xiang X, Wu Y, Cao Y, Song J, Sun K, et al. Fine particulate air pollution and first hospital admissions for ischemic stroke in Beijing, China. Sci Rep. 2017;7:3897. https://doi.org/10.1038/s41598-017-04312-5.
Lin H, Guo Y, Di Q, Zheng Y, Kowal P, Xiao J, et al. Ambient PM(2.5) and stroke: effect modifiers and population attributable risk in six low- and middle-income countries. Stroke. 2017;48:1191–7. https://doi.org/10.1161/strokeaha.116.015739.
Hong YC, Lee JT, Kim H, Kwon HJ. Air pollution: a new risk factor in ischemic stroke mortality. Stroke. 2002;33:2165–9. https://doi.org/10.1161/01.str.0000026865.52610.5b.
Stockfelt L, Andersson EM, Molnár P, Gidhagen L, Segersson D, Rosengren A, et al. Long-term effects of total and source-specific particulate air pollution on incident cardiovascular disease in Gothenburg, Sweden. Environ Res. 2017;158:61–71. https://doi.org/10.1016/j.envres.2017.05.036.
Qiu H, Sun S, Tsang H, Wong CM, Lee RS, Schooling CM, et al. Fine particulate matter exposure and incidence of stroke: a cohort study in Hong Kong. Neurology. 2017;88:1709–17. https://doi.org/10.1212/wnl.0000000000003903.
Crichton S, Barratt B, Spiridou A, Hoang U, Liang SF, Kovalchuk Y, et al. Associations between exhaust and non-exhaust particulate matter and stroke incidence by stroke subtype in South London. Sci Total Environ. 2016;568:278–84. https://doi.org/10.1016/j.scitotenv.2016.06.009.
Huang F, Luo Y, Guo Y, Tao L, Xu Q, Wang C, et al. Particulate matter and hospital admissions for stroke in Beijing, China: modification effects by ambient temperature. J Am Heart Assoc. 2016;5. https://doi.org/10.1161/jaha.116.003437.
Lin H, Tao J, Du Y, Liu T, Qian Z, Tian L, et al. Differentiating the effects of characteristics of PM pollution on mortality from ischemic and hemorrhagic strokes. Int J Hyg Environ Health. 2016;219:204–11. https://doi.org/10.1016/j.ijheh.2015.11.002.
Han MH, Yi HJ, Ko Y, Kim YS, Lee YJ. Association between hemorrhagic stroke occurrence and meteorological factors and pollutants. BMC Neurol. 2016;16:59. https://doi.org/10.1186/s12883-016-0579-2.
Korek MJ, Bellander TD, Lind T, Bottai M, Eneroth KM, Caracciolo B, et al. Traffic-related air pollution exposure and incidence of stroke in four cohorts from Stockholm. J Exposure Sci Environ Epidemiol. 2015;25:517–23. https://doi.org/10.1038/jes.2015.22.
Chang CC, Chen PS, Yang CY. Short-term effects of fine particulate air pollution on hospital admissions for cardiovascular diseases: a case-crossover study in a tropical city. J Toxicol Environ Health A. 2015;78:267–77. https://doi.org/10.1080/15287394.2014.960044.
Tian L, Qiu H, Pun VC, Ho KF, Chan CS, Yu IT. Carbon monoxide and stroke: a time series study of ambient air pollution and emergency hospitalizations. Int J Cardiol. 2015;201:4–9. https://doi.org/10.1016/j.ijcard.2015.07.099.
To T, Zhu J, Villeneuve PJ, Simatovic J, Feldman L, Gao C, et al. Chronic disease prevalence in women and air pollution--a 30-year longitudinal cohort study. Environ Int. 2015;80:26–32. https://doi.org/10.1016/j.envint.2015.03.017.
Hoffmann B, Weinmayr G, Hennig F, Fuks K, Moebus S, Weimar C, et al. Air quality, stroke, and coronary events: results of the Heinz Nixdorf Recall Study from the Ruhr Region. Deutsches Arzteblatt Int. 2015;112:195–201. https://doi.org/10.3238/arztebl.2015.0195.
Chen YC, Weng YH, Chiu YW, Yang CY. Short-term effects of coarse particulate matter on hospital admissions for cardiovascular diseases: a case-crossover study in a tropical city. J Toxicol Environ Health A. 2015;78:1241–53. https://doi.org/10.1080/15287394.2015.1083520.
Amancio CT, Nascimento LF. Environmental pollution and deaths due to stroke in a city with low levels of air pollution: ecological time series study. Sao Paulo Med J. 2014;132:353–8.
Chen SY, Lin YL, Chang WT, Lee CT, Chan CC. Increasing emergency room visits for stroke by elevated levels of fine particulate constituents. Sci Total Environ. 2014;473-474:446–50. https://doi.org/10.1016/j.scitotenv.2013.12.035.
Stafoggia M, Cesaroni G, Peters A, Andersen ZJ, Badaloni C, Beelen R, et al. Long-term exposure to ambient air pollution and incidence of cerebrovascular events: results from 11 European cohorts within the ESCAPE project. Environ Health Perspect. 2014;122:919–25. https://doi.org/10.1289/ehp.1307301.
Chiu HF, Chang CC, Yang CY. Relationship between hemorrhagic stroke hospitalization and exposure to fine particulate air pollution in Taipei, Taiwan. J Toxicol Environ Health A. 2014;77:1154–63. https://doi.org/10.1080/15287394.2014.926801.
Chen R, Zhang Y, Yang C, Zhao Z, Xu X, Kan H. Acute effect of ambient air pollution on stroke mortality in the China air pollution and health effects study. Stroke. 2013;44:954–60. https://doi.org/10.1161/strokeaha.111.673442.
Carlsen HK, Forsberg B, Meister K, Gíslason T, Oudin A. Ozone is associated with cardiopulmonary and stroke emergency hospital visits in Reykjavík, Iceland 2003-2009. Environ Health. 2013;12:28. https://doi.org/10.1186/1476-069x-12-28.
Johnson JY, Rowe BH, Allen RW, Peters PA, Villeneuve PJ. A case-control study of medium-term exposure to ambient nitrogen dioxide pollution and hospitalization for stroke. BMC Public Health. 2013;13:368. https://doi.org/10.1186/1471-2458-13-368.
Atkinson RW, Carey IM, Kent AJ, van Staa TP, Anderson HR, Cook DG. Long-term exposure to outdoor air pollution and incidence of cardiovascular diseases. Epidemiology. 2013;24:44–53. https://doi.org/10.1097/EDE.0b013e318276ccb8.
Xu X, Sun Y, Ha S, Talbott EO, Lissaker CT. Association between ozone exposure and onset of stroke in Allegheny County, Pennsylvania, USA, 1994-2000. Neuroepidemiology. 2013;41:2–6. https://doi.org/10.1159/000345138.
Xiang H, Mertz KJ, Arena VC, Brink LL, Xu X, Bi Y, et al. Estimation of short-term effects of air pollution on stroke hospital admissions in Wuhan, China. PLoS One. 2013;8:e61168. https://doi.org/10.1371/journal.pone.0061168.
Yorifuji T, Kawachi I, Sakamoto T, Doi H. Associations of outdoor air pollution with hemorrhagic stroke mortality. J Occup Environ Med. 2011;53:124–6. https://doi.org/10.1097/JOM.0b013e3182099175.
Qian Y, Zhu M, Cai B, Yang Q, Kan H, Song G, et al. Epidemiological evidence on association between ambient air pollution and stroke mortality. J Epidemiol Commun Health. 2013;67:635–40. https://doi.org/10.1136/jech-2012-201096.
Andersen ZJ, Kristiansen LC, Andersen KK, Olsen TS, Hvidberg M, Jensen SS, et al. Stroke and long-term exposure to outdoor air pollution from nitrogen dioxide: a cohort study. Stroke. 2012;43:320–5. https://doi.org/10.1161/STROKEAHA.111.629246.
Nascimento LF, Francisco JB, Patto MB, Antunes AM. Environmental pollutants and stroke-related hospital admissions. Cadernos De Saude Publica. 2012;28:1319–24. https://doi.org/10.1590/s0102-311x2012000700010.
O’Donnell MJ, Fang J, Mittleman MA, Kapral MK, Wellenius GA. Fine particulate air pollution (PM2.5) and the risk of acute ischemic stroke. Epidemiology. 2011;22:422–31. https://doi.org/10.1097/EDE.0b013e3182126580.
Lipsett MJ, Ostro BD, Reynolds P, Goldberg D, Hertz A, Jerrett M, et al. Long-term exposure to air pollution and cardiorespiratory disease in the California teachers study cohort. Am J Respir Crit Care Med. 2011;184:828–35. https://doi.org/10.1164/rccm.201012-2082OC.
Ren C, Melly S, Schwartz J. Modifiers of short-term effects of ozone on mortality in eastern Massachusetts--a case-crossover analysis at individual level. Environ Health. 2010;9:3. https://doi.org/10.1186/1476-069x-9-3.
Zanobetti A, Schwartz J. The effect of fine and coarse particulate air pollution on mortality: a national analysis. Environ Health Perspect. 2009;117:898–903. https://doi.org/10.1289/ehp.0800108.
Kettunen J, Lanki T, Tiittanen P, Aalto PP, Koskentalo T, Kulmala M, et al. Associations of fine and ultrafine particulate air pollution with stroke mortality in an area of low air pollution levels. Stroke. 2007;38:918–22. https://doi.org/10.1161/01.STR.0000257999.49706.3b.
Franklin M, Zeka A, Schwartz J. Association between PM2.5 and all-cause and specific-cause mortality in 27 US communities. J Exposure Sci Environ Epidemiol. 2007;17:279–87. https://doi.org/10.1038/sj.jes.7500530.
Qian Z, He Q, Lin HM, Kong L, Liao D, Dan J, et al. Association of daily cause-specific mortality with ambient particle air pollution in Wuhan, China. Environ Res. 2007;105:380–9. https://doi.org/10.1016/j.envres.2007.05.007.
Villeneuve PJ, Chen L, Stieb D, Rowe BH. Associations between outdoor air pollution and emergency department visits for stroke in Edmonton, Canada. Eur J Epidemiol. 2006;21:689–700. https://doi.org/10.1007/s10654-006-9050-9.
Henrotin JB, Besancenot JP, Bejot Y, Giroud M. Short-term effects of ozone air pollution on ischaemic stroke occurrence: a case-crossover analysis from a 10-year population-based study in Dijon, France. Occup Environ Med. 2007;64:439–45. https://doi.org/10.1136/oem.2006.029306.
Tsai SS, Goggins WB, Chiu HF, Yang CY. Evidence for an association between air pollution and daily stroke admissions in Kaohsiung, Taiwan. Stroke. 2003;34:2612–6. https://doi.org/10.1161/01.str.0000095564.33543.64.
Zhang X, Fan C, Ren Z, Feng H, Zuo S, Hao J, et al. Maternal PM2.5 exposure triggers preterm birth: a cross-sectional study in Wuhan, China. Glob Health. Res Policy. 2020;5:17. https://doi.org/10.1186/s41256-020-00144-5.
Rich DQ, Kipen HM, Huang W, Wang G, Wang Y, Zhu P, et al. Association between changes in air pollution levels during the Beijing Olympics and biomarkers of inflammation and thrombosis in healthy young adults. JAMA. 2012;307. https://doi.org/10.1001/jama.2012.3488.
Wu S, Deng F, Niu J, Huang Q, Liu Y, Guo X. Association of heart rate variability in taxi drivers with marked changes in particulate air pollution in Beijing in 2008. Environ Health Perspect. 2010;118:87–91. https://doi.org/10.1289/ehp.0900818.
Acknowledgments
The authors acknowledge all the participants and administrators of this study.
Funding
This work was supported by the Bill & Melinda Gates Foundation (Grant No. OOP1148464) and the Natural Science Fund of Hubei Province (Granter number: 2018CFB634).
Author information
Authors and Affiliations
Contributions
Conceptualization, ZP.N; methodology, ZP.N; software, ZP.N; validation, H.X.; formal analysis, ZP.N and FF.L; data curation, ZP.N and HM.Y.; writing—original draft preparation, ZP.N, FF.L, and HM.Y; writing—review and editing, ZP.N and H.X; supervision, ST.W; funding acquisition, H.X. All authors read and approved the final manuscript before submission.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors consent for publishing this work.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Niu, Z., Liu, F., Yu, H. et al. Association between exposure to ambient air pollution and hospital admission, incidence, and mortality of stroke: an updated systematic review and meta-analysis of more than 23 million participants. Environ Health Prev Med 26, 15 (2021). https://doi.org/10.1186/s12199-021-00937-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12199-021-00937-1