Abstract
Background
Extensive literature exists about the treatment of ankle osteochondral lesions, but there is no specific review of retrograde drilling, despite its common application. Indications for retrograde drilling are still few and are far from clear, and some evolutions of the technique have recently occurred. The aim of this review is to provide an update on actual applications and techniques of retrograde drilling for ankle osteochondral lesions.
Methods
A systematic review was carried out according to the 2020 PRISMA guidelines. The PubMed and Embase databases were searched in June 2023. The search string focused on studies related to retrograde drilling in the treatment of ankle osteochondral lesions.
Results
Twenty-one articles for a total of 271 ankles were included in this review. The mean length of the treated lesions was 11.4 mm. Different navigation systems were used, with fluoroscopy the most commonly used. Various adjuvants were employed after drilling, with bone graft the most commonly applied. In most cases, postoperative patient satisfaction and symptom relief were reported, and no complications occurred. Retrograde drilling was found to be suitable for the treatment of subchondral cysts with intact cartilage or small lesions. Some modifications to the original technique may allow surgical indications to be extended to more complex cases.
Conclusions
Middle-term results of retrograde drilling showed postoperative satisfaction and symptom relief with both original and modified techniques. Additional research is required to investigate the long-term results.
Level of evidence: IV.
Trial registration: This systematic review was registered on PROSPERO (id number: CRD42022371128).
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Osteochondral lesions are defects of the subchondral bone and the overlying cartilage. Active and young patients are the most commonly affected by this disorder, which causes chronic pain, swelling, and stiffness [1, 2] and is supposed to occur in up to 50% of ankle sprain cases [3]. When conservative treatment fails, surgical management is indicated [1, 4]. Among the various surgical techniques available, drilling represents a common and widespread procedure because of its simplicity and cost-effectiveness. Two variants of drilling can be distinguished based on the direction of the drill toward the lesion: anterograde or retrograde. Anterograde or transmalleolar drilling was described by Kumai et al. in 1999 [5] and consists of the insertion of a K-wire from the medial malleolus directly to the lesion, passing through the intact cartilage [5]. Instead, retrograde drilling (RD) allows the cartilage layer to be preserved by reaching the lesion from behind. RD has the advantage of not damaging the cartilage, so it is particularly indicated in the treatment of subchondral cysts or any osteochondral lesions with an intact and stable cartilage surface [1].
Despite its wide application, current evidence on the indications for and outcomes of RD in the treatment of osteochondral lesions of the ankle is limited, and a comprehensive review is missing. Moreover, in the last few years there has been some evolution of the original technique [6,7,8]. Since RD has provided better results compared to anterograde drilling [9], and the latter is being progressively replaced by microfractures that do not cause heat damage, this review focuses only on RD.
The aim of this systematic review is therefore to provide an update about actual applications, techniques, and outcomes of RD for ankle osteochondral lesions.
Materials and methods
Eligibility criteria
All articles written in English on the treatment of osteochondral lesions of the talus and distal tibia through RD were included in this review. Exclusion criteria were anterograde drilling; RD associated with microfractures, osteochondral transplant, debridement; surgical procedures other than RD (such as microfractures, autologous matrix-induced chondrogenesis, osteochondral autograft or allograft transplant, mosaicplasty, matrix-assisted autologous chondrocyte transplantion); osteochondral lesion sites other than the distal tibia or talus; studies reporting data that do not distinguish among the compared surgical procedures; studies involving cadaveric or animal specimens; single-case reports, editor commentaries, letters to the editor, reviews, and articles not written in English.
No exclusion criteria were applied based on age, sample size, and follow-up.
Search strategy
This systematic review was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines [10] and registered on PROSPERO (id number: CRD42022371128).
The PICO algorithm was established as follows:
-
P (problem): osteochondral lesions of the talus and distal tibia
-
I (intervention): RD
-
C (comparison): no comparison group
-
O (outcomes): clinical scores, patient satisfaction, and complications
A comprehensive literary search was run across the PubMed and Embase databases in June 2023. A combination of the following keywords and the Boolean indicator AND was used: drilling, osteochondral, lesion. Results of the database search are reported in Table 1.
Selection and data collection
After duplicate removal, two authors (EA, SG) independently reviewed all the articles by title and abstract to select those eligible for inclusion based on the aforementioned inclusion and exclusion criteria. The full texts of the retrieved articles were accessed. The bibliographies of the eligible studies were carefully examined to identify additional articles of interest. In the case of uncertainty, the senior author made the final decision.
Data items
Full texts of the retrieved articles were carefully examined to extract the following data. The characteristics of each study—in terms of authors, year of publication, study type, and level of evidence (LOE) according to the Oxford Level of Evidence scale—were noted. Population data were collected, considering the number of patients, number of ankles, sex of patients, mean age at surgery, mean follow-up, and location and size of the osteochondral lesions. Indications consisting of parameters to consider surgery, classification systems, and grades of the lesions. Data concerning the surgical procedure such as the navigation system and adjuvants to the original technique were collected. Clinical outcomes were obtained through the American Orthopedic Foot and Ankle Society's ankle-hindfoot scale (AOFAS), the Visual Analog Scale (VAS), and clinical satisfaction. Intraoperative and postoperative complications were noted.
Assessment of risk of bias and quality of recommendation
Quality assessments of the included studies were conducted through ROBINS-I for non-randomized studies [11]. The following factors pertaining to risk of bias were evaluated: confounding, selection, classification of interventions, deviation from intended intervention, missing data, measurement of outcomes, and selection of the reported results.
The quality of evidence was assessed utilizing the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework.
Data synthesis
Categorical variables were reported as the frequency and/or percentage, while continuous variables were reported as the mean value and its range. Given the differences in reporting patient satisfaction, the following dichotomic classification of the results was needed: “good” and “excellent” were grouped as “satisfied,” and “fair” and “poor” as “unsatisfied”. Data collection was performed using Microsoft Excel (Microsoft Corporation, Redmond, WA) for Windows 11.
Results
Search results
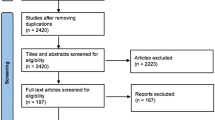
A total of 607 articles were identified via database searching and cross-referencing. After duplicate removal, 435 articles were screened by title and abstract, leaving 56 full texts to be assessed for eligibility. Thirty-five articles were excluded because of the following reasons: mixed surgical techniques (n = 17); anterograde drilling (n = 7); population not of interest (n = 6); case report (n = 4); letter to the editor (n = 1). Twenty-one studies fulfilled the inclusion criteria and were included in the qualitative synthesis. The PRISMA flowchart showing the selection process is presented in Fig. 1.
Assessment of risk of bias and quality of recommendation
The quality assessment of the included studies, conducted through the ROBINS-I tool for non-randomized studies, is reported in Table 2. Due to the considerable amount of retrospective case series (17 articles, 81%), there was a high likelihood of selection bias. The study's overall risk of bias score was low–moderate, indicating a moderate to good level of methodological quality.
Since most of the included articles were observational case series investigating only patients exposed to the intervention, the quality of evidence was rated as low to very low according to the GRADE framework (Table 3).
Study characteristics and results of individual studies
The literature concerning RD was mostly constituted by retrospective case series (17 articles, 81%) [6, 8, 12,13,14,15,16,17,18,19,20,21,22,23,24,25,26], classified as LOE IV. The remaining articles were equally divided into retrospective comparative studies (two articles, 10%) [7, 27] and prospective observational studies (two articles, 10%) [28, 29], both classified as LOE III (Table 3). The majority of the included studies were published in the last 20 years.
A total of 266 patients (271 ankles) were included in this review. When reported, the sex distribution was 99 (54%) males and 83 (46%) females. Mean age at surgery was available in all articles but one [7], and was found to be 28.2 years (range, 9–69). Final follow-up was on average 33 months, and was reported in all articles but four [7, 13, 20, 23].
Most of the osteochondral lesions were in the talus; only Takao et al. included lesions on both the talus and distal tibia [29]. Concerning the osteochondral lesions of the talus, a more detailed localization was provided in 16 articles as follows: 83% (144/174) medial, 15% (27/174) lateral, 2% (3/174) central. Antero-posterior localization was not considered when performing this calculation; therefore, lesions described as posteromedial or anterolateral were counted as medial and lateral, respectively.
Seven articles reported the mean size of the lesions, but in different ways [6, 8, 12, 16, 17, 28, 29]. To compare most of the articles, only the mean length of the lesions was considered; it was found to be 11.4 mm (Table 3).
Synthesis of results
Among the clinical and radiological parameters used in assessing surgical indication, 15 authors agreed that intact cartilage must be present to make patients eligible for RD [7, 8, 12, 14, 16,17,18,19,20,21,22,23,24,25,26,27].
The Berndt and Harty classification [30] was considered in four articles: two authors recommended surgical treatment in grades I–III [13, 17], whereas Masquijo and Geerling restricted the indication to only grades I and II [18, 25]. Regarding lesion size, only two authors set a threshold value to consider surgery, which ranged from 100 mm2 to 125 mm2 [7, 28]. Faldini et al. also extended surgical indication to wide osteochondral lesions with, theoretically, no size limit [8].
Osteochondral lesions were classified by applying different grading systems based on the available radiological imaging. The Berndt and Harty classification on a plain radiograph was used in six studies, with an average grade of 2.2 out of 4 [6, 14, 18, 19, 21, 23]. The Pritsch classification on arthroscopic imaging was used in five studies, with a mean grade of 1.6 [14, 17, 26,27,28]. Other less common grading systems applied are reported in Table 4.
Various evolutions of the original surgical procedures have been described by authors. RD was performed by inserting K-wires retrogradely under different navigation systems. Fluoroscopy was the most extensively used method (13 articles) [7, 8, 12, 15, 17,18,19,20,21, 24, 26, 27]. In terms of fluoro-free surgeries, magnetic resonance imaging (MRI) was used in one article [6], and computer-assisted navigation was used by three authors [13, 23, 25]. Finally, Microvector was used by Beck et al. [28].
Different adjuvants were employed after RD. Cancellous bone grafting was utilized to plug the bone defect by four authors [7, 17, 21, 29]. Saxena et al. also injected platelet-rich plasma onto the bone graft [7]. Faldini et al. retrogradely positioned a hyaluronan scaffold soaked in bone marrow aspirate concentrate and, in addition, filled the talar tunnel with cancellous bone graft [8]. Other injectable solutions were applied alone in a retrograde fashion: Grafton™ gel by Berlet et al. [24] and PRO-DENSE® by Beck et al. [28] (Table 4).
In order to compare the clinical outcomes, 12 articles (195 ankles) preoperatively recorded the AOFAS score, and 12 articles (198 ankles) recorded it postoperatively. The mean preoperative value was 64.2 (range, 0–87), which increased postoperatively to 88.8 (range, 48–100) [7, 13, 15,16,17,18, 21, 24, 25, 27,28,29].
Pain assessment was conducted through VAS by six authors (78 ankles), and the results were on average 6.9 and 2.2 before and after surgery, respectively [6, 8, 12, 14, 18, 19].
Post-treatment satisfaction was investigated in 59 patients, and satisfactory results were achieved in a mean of 83% of the patients [12, 14, 18,19,20, 22, 26] (Table 5).
A few articles registered postoperative complications [8, 14, 16,17,18, 21,22,23,24, 27] (Table 5). In most cases (91%), no complication occurred. Ankle swelling was the most frequently reported complication (five cases), followed by two cases of minor hypoesthesia, one case of delayed wound healing, and one case of progression of the osteochondral lesion.
As Kelbérine et al. merely stated that there was “no serious complication,” it was excluded from this calculation, as some minor complications may have occurred [22].
Discussion
Results from this review confirmed that RD is a safe, effective, low-morbidity procedure for the treatment of ankle osteochondral lesions. Improvements in postoperative AOFAS and VAS were observed at short/medium-term follow-up. However, some concerns remained regarding the risk of degenerative arthritis over time in those cases with persistent lesions on radiographs. The fact that RD was commonly recommended for small lesions with intact cartilage could have contributed to the favorable outcomes, as these lesions are often easier to treat and may have fewer symptoms compared to larger or more extensive lesions. Regardless of the lesion size, the most common criterion for RD was the presence of a subchondral cyst with intact overlying cartilage [7, 8, 12, 14, 16,17,18,19,20,21,22,23,24,25,26]. Moreover, recent modifications to the original technique allowed the indication to be extended to osteochondral lesions with damaged cartilage, but no long-term results have been provided yet [8].
According to the literature, RD was indicated in the treatment of small lesions (area < 100 mm2, depth < 5 mm, diameter < 10 mm) [31] and when defects were difficult to reach through usual arthroscopic portals. The results of this review showed a mean lesion length of 11.4 mm, which was higher than what was recommended. In fact, there was no complete agreement regarding the proper indication for RD, and many surgeons arbitrarily referred to their clinical experience.
Concerning the surgical procedure, some differences were found in the navigation systems, with fluoroscopy being the most commonly used [7, 8, 12, 15, 17,18,19,20,21, 24, 26, 27]. Drawbacks of fluoroscopic guidance included difficulty in osteochondral lesion identification and a lack of 3D imaging intraoperatively [13, 23, 25]. For this reason, up to 20% of fluoroscopically navigated drilling procedures have been shown to be inaccurate, and a drill misplacement can be found in up to 28% of cases [13, 23, 25]. To overcome these issues, other systems have been proposed, such as drill guide systems [28] and, more recently, navigation systems guided by MRI or computed tomography (CT) or that are computer assisted [13, 23, 25]. Although authors argued that newer guidance systems have advantages in terms of reliable cartilage visualization and the precise treatment of osteochondral lesions, the average procedure time did not demonstrate a speed advantage compared to the standard fluoroscopic technique [6]. Moreover, the higher costs of the procedure should also be considered.
Some modifications to the original surgical technique have been made over the years. The drilling technique has been modified by using a 6-mm or 8-mm drill to allow lesion decompression and better cyst curettage. A wide talar tunnel may also be necessary to insert biological adjuvants [8, 28]. Further variations involved the filling of the drill hole and the defect with different materials. One of the most commonly applied was a cancellous bone graft [7, 17, 21, 29], to which some authors added platelet-rich plasma [7]. Other injectable solutions were employed retrogradely, such as Grafton™ gel [21] and PRO-DENSE® [28]. Of particular interest was the retrograde application of a hyaluronan scaffold soaked in bone marrow aspirate concentrate, which combines the advantages of reparative and regenerative techniques [8]. This cartilage-sparing technique derived from RD [8] was developed as an alternative to metal-resurfacing implants [32] and for addressing deeper defects or lesions involving the talar gutter, where thorough osteochondral debridement is necessary.
This systematic review has provided a comprehensive overview of actual indications, surgical techniques, and clinical outcomes of RD, which may be useful to surgeons when choosing among the various treatments of ankle osteochondral lesions. RD is a bone-marrow-stimulating technique which is supposed to induce the production of fibrocartilage at the site of the treated lesion. Since some authors have associated regenerative procedures with standard RD, and it would be highly interesting for future research to evaluate the type of cartilage produced using T2 mapping [2, 8].
When analyzing the results of this review, the nature of the included studies imposes a limitation, as they were mainly retrospective case series and therefore open to selection and detection bias, as shown by the ROBINS-I and GRADE evaluations. Moreover, most of the studies had a small sample size. The mean follow-up was sufficient for assessing postoperative complications but not long enough to evaluate long-term effects. Lastly, postoperative outcomes were only reported through clinical scores, and no radiological outcomes were provided. In addition, different measurements of clinical outcomes and missing data represent some limitations of the study. Therefore, wider samples and are longer follow-up are needed to confirm these early results and to more deeply investigate the effect of RD.
Conclusions
This systematic review has highlighted the suitability of RD for treating subchondral cysts with intact cartilage or small lesions, with good postoperative satisfaction and symptom relief achieved at middle-term follow-up. Modifications to the technique allowed for broader surgical indications, even in complex cases. RD can be performed with different navigation systems and adjuvants, yielding similar outcomes. However, further research is necessary to assess long-term results.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Wodicka R, Ferkel E, Ferkel R (2016) Osteochondral lesions of the ankle. Foot Ankle Int 37:1023–1034. https://doi.org/10.1177/1071100716654691
Giannini S, Buda R, Battaglia M et al (2013) One-step repair in talar osteochondral lesions: 4-year clinical results and t2-mapping capability in outcome prediction. Am J Sports Med 41:511–518. https://doi.org/10.1177/0363546512467622
Saxena A, Eakin C (2007) Articular talar injuries in athletes: results of microfracture and autogenous bone graft. Am J Sports Med 35:1680–1687. https://doi.org/10.1177/0363546507303561
Migliorini F, Maffulli N, Schenker H et al (2022) Surgical management of focal chondral defects of the talus: a Bayesian network meta-analysis. Am J Sports Med 50:2853–2859. https://doi.org/10.1177/03635465211029642
Kumai T, Takakura Y, Higashiyama I, Tamai S (1999) Arthroscopic drilling for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am 81:1229–1235. https://doi.org/10.2106/00004623-199909000-00004
Kerimaa P, Ojala R, Sinikumpu J-J et al (2014) MRI-guided percutaneous retrograde drilling of osteochondritis dissecans of the talus: a feasibility study. Eur Radiol 24:1572–1576. https://doi.org/10.1007/s00330-014-3161-6
Saxena A, Maffulli N, Jin A et al (2022) Outcomes of talar osteochondral and transchondral lesions using an algorithmic approach based on size, location, and subchondral plate integrity: a 10-year study on 204 lesions. J Foot Ankle Surg 61:442–447. https://doi.org/10.1053/j.jfas.2021.06.011LK
Faldini C, Mazzotti A, Artioli E et al (2022) A novel retrograde technique for ankle osteochodral lesions: the sub-endo-chondral regenerative treatment (secret). Musculoskelet Surg. https://doi.org/10.1007/S12306-022-00767-6
Zengerink M, Struijs PAA, Tol JL et al (2010) Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc 18:238–246. https://doi.org/10.1007/s00167-009-0942-6
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. https://doi.org/10.1136/BMJ.N71
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Schwartz AM, Niu S, Mirza FA et al (2021) Surgical treatment of talus OCL: mid- to long-term clinical outcome with detailed analyses of return to sport. J Foot Ankle Surg 60:1188–1192. https://doi.org/10.1053/j.jfas.2021.05.002LK
Rosenberger RE, Fink C, Bale RJ et al (2006) Computer-assisted minimally invasive treatment of osteochondrosis dissecans of the talus. Oper Orthop Traumatol 18:300–316. https://doi.org/10.1007/s00064-006-1179-x
Pritsch M, Horoshovski H, Farine I (1986) Arthroscopic treatment of osteochondral lesions of the talus. J Bone Joint Surg Am 68:862–865
Yasui Y, Takao M, Miyamoto W, Matsushita T (2014) Simultaneous surgery for chronic lateral ankle instability accompanied by only subchondral bone lesion of talus. Arch Orthop Trauma Surg 134:821–827. https://doi.org/10.1007/s00402-014-1969-9
Ikuta Y, Nakasa T, Ota Y et al (2020) Retrograde drilling for osteochondral lesion of the talus in juvenile patients. Foot Ankle Orthop 5:2473011420916139. https://doi.org/10.1177/2473011420916139
Anders S, Lechler P, Rackl W et al (2012) Fluoroscopy-guided retrograde core drilling and cancellous bone grafting in osteochondral defects of the talus. Int Orthop 36:1635–1640. https://doi.org/10.1007/s00264-012-1530-9
Masquijo JJ, Ferreyra A, Baroni E (2016) Arthroscopic retrograde drilling in juvenile osteochondritis dissecans of the talus. J Pediatr Orthop 36:589–593. https://doi.org/10.1097/BPO.0000000000000498
Flick AB, Gould N (1985) Osteochondritis dissecans of the talus (transchondral fractures of the talus): review of the literature and new surgical approach for medial dome lesions. Foot Ankle 5:165–185. https://doi.org/10.1177/107110078500500403
Angermann P, Jensen P (1989) Osteochondritis dissecans of the talus: long-term results of surgical treatment. Foot Ankle 10:161–163. https://doi.org/10.1177/107110078901000309
Taranow WS, Bisignani GA, Towers JD, Conti SF (1999) Retrograde drilling of osteochondral lesions of the medial talar dome. Foot Ankle Int 20:474–480. https://doi.org/10.1177/107110079902000802
Kelbérine F, Frank A, Kelberine F, Frank A (1999) Arthroscopic treatment of osteochondral lesions of the talar dome: a retrospective study of 48 cases. Arthroscopy 15:77–84. https://doi.org/10.1053/ar.1999.v15.0150071LK
Bale RJ, Hoser C, Rosenberger R et al (2001) Osteochondral lesions of the talus: computer-assisted retrograde drilling–feasibility and accuracy in initial experiences. Radiology 218:278–282. https://doi.org/10.1148/radiology.218.1.r01ja18278
Berlet GC, Berlet GC, Philbin TM et al (2008) Retrograde drilling of osteochondral lesions of the talus. Foot Ankle Spec 1:207–209. https://doi.org/10.1177/1938640008321653
Geerling J, Zech S, Kendoff D et al (2009) Initial outcomes of 3-dimensional imaging-based computer-assisted retrograde drilling of talar osteochondral lesions. Am J Sports Med 37:1351–1357. https://doi.org/10.1177/0363546509332499
Minokawa S, Yoshimura I, Kanazawa K et al (2020) Retrograde drilling for osteochondral lesions of the talus in skeletally immature children. Foot Ankle Int 41:827–833. https://doi.org/10.1177/1071100720920847
Kono M, Takao M, Naito K et al (2006) Retrograde drilling for osteochondral lesions of the talar dome. Am J Sports Med 34:1450–1456. https://doi.org/10.1177/0363546506287300
Beck S, Claßen T, Haversath M et al (2016) Operative technique and clinical outcome in endoscopic core decompression of osteochondral lesions of the talus: a pilot study. Med Sci Monit Int Med J Exp Clin Res 22:2278–2283. https://doi.org/10.12659/msm.896522
Takao M, Innami K, Komatsu F, Matsushita T (2010) Retrograde cancellous bone plug transplantation for the treatment of advanced osteochondral lesions with large subchondral lesions of the ankle. Am J Sports Med 38:1653–1660. https://doi.org/10.1177/0363546510364839
Berndt AL, Harty M (1959) Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am 41-A:988–1020
Hannon CP, Bayer S, Murawski CD et al (2018) Debridement, curettage, and bone marrow stimulation: proceedings of the International Consensus Meeting on Cartilage Repair of the Ankle. Foot Ankle Int 39:16S-22S. https://doi.org/10.1177/1071100718779392
Vuurberg G, Reilingh ML, van Bergen CJA et al (2018) Metal resurfacing inlay implant for osteochondral talar defects after failed previous surgery: a midterm prospective follow-up study. Am J Sports Med 46:1685–1692. https://doi.org/10.1177/0363546518764916
Acknowledgements
Not applicable.
Funding
This work was supported by the Italian Ministry of Health—Ricerca Corrente to IRCCS Istituto Ortopedico Rizzoli and by the 5X1000 2019 project entlited “Malattie muscolo scheletriche: dalla analisi fisiopatologica dei tessuti alla proposta di nuove strategie terapeutiche anche attraverso l’uso di algoritmi di Intelligenza Artificiale per una medicina di precisione” (PRWEB: 2021/730571).
Author information
Authors and Affiliations
Contributions
Conceptualization, AM and CF; methodology, EA; investigation, EA and SG; writing—original draft preparation, MM and GV; writing—review and editing, FB and AR; supervision, CF. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Informed consent
Not applicable.
Competing interests
The authors have no competing interest to declare that is relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Artioli, E., Mazzotti, A., Gerardi, S. et al. Retrograde drilling for ankle joint osteochondral lesions: a systematic review. J Orthop Traumatol 24, 37 (2023). https://doi.org/10.1186/s10195-023-00716-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-023-00716-4