Abstract
Background
Although the involvement of calcitonin gene-related peptide (CGRP) in migraines is well-established, its specific role in investigating the aura phase, which often precedes the headache, remains largely unexplored. This study aims to instigate CGRP’s potential in triggering aura, thus establishing its role in the early stages of migraine.
Methods
In this open-label, non-randomized, single-arm trial, 34 participants with migraine with aura received continuous intravenous infusion of CGRP (1.5 µg/min) over 20 min on a single experimental day. Participants were required to be free of headache and report no use of acute medications 24 h before infusion start. The primary endpoint was the incidence of migraine aura during the 12-hour observational period after the start of infusion.
Results
Thirteen (38%) of 34 participants developed migraine aura after CGRP infusion. In addition, 24 (71%) of 34 participants developed migraine headache following CGRP infusion.
Conclusions
Our findings suggest that CGRP could play an important role in the early phases of a migraine attack, including during the aura phase. These insights offer a new perspective on the pathogenesis of migraines with aura. They underscore the need for additional research to further explore the role of CGRP in these initial stages of a migraine attack, and potentially inform future development of therapeutic interventions.
Trial registration
ClinicalTrials.gov Identifier: NCT04592952.
Graphical Abstract

Similar content being viewed by others
Background
Migraine is a prevalent and disabling neurological disorder that affects over 1 billion people worldwide [1]. The clinical presentation is characterized by recurrent attacks of headache accompanied by symptoms such as photophobia, phonophobia, and nausea/vomiting [2]. About 30% of people with migraine also experience aura which is defined as transient, focal neurological symptoms that precede or accompany the headache phase of a migraine attack [3]. The most common aura symptoms include visual disturbances (e.g., as a fortification spectra) and predominantly unilateral paraesthesia (e.g., numbness) that gradually spreads on the face or arm [2, 3].
The neurobiological substrate of aura is believed to be cortical spreading depolarization (CSD), a self-propagating wave of neuronal and glial excitation across the cortex followed by inhibition [4]. The prevailing theory posits that CSD triggers the release of pronociceptive mediators, leading to the dilation of meningeal arteries and activation of perivascular primary afferents, thereby causing headache [4, 5].
However, this theory is largely derived from clinical observations that aura often precedes the onset of headache, and it must be considered with caution due to significant interspecies variations between human and animal CSD. Recent publications have further highlighted the complexities and potential problems with translating findings from animal models to human migraine pathology [6]. As such, while the link between CSD and headache has been long discussed, it remains an area of ongoing investigation, and the question of whether shared disease mechanisms underlie both the aura and headache phase of a migraine attack continues to be an open and complex question [5]. In this context, signalling molecule calcitonin gene-related peptide (CGRP) has received increased attention due to the effectiveness of drugs targeting CGRP signalling in treating migraine, as well as self-reported aura [7,8,9]. Furthermore, 1 experimental study found that CGRP might be able to induce aura in some people with migraine with aura [10]. The study was however limited by a small sample, precluding us from drawing firm conclusions about the involvement of CGRP in the genesis of migraine attacks with aura [10]. Moreover, it is unknown whether the induction of aura symptoms depends on the frequency of aura. If so, it might be speculated that a higher frequency of aura increases the susceptibility to develop CGRP-induced migraine attacks with aura.
In the present open-label, non-randomized, single-arm trial, adult people with migraine with aura were enrolled and allocated to receive a 20-minute continuous intravenous infusion of CGRP on a single experimental day. The aim was to investigate whether CGRP infusion can induce migraine attacks with aura in people with migraine with aura.
Methods
Study Oversight
Registry for Migraine (REFORM) is a prospective, single-centre study of adult people with migraine that was conducted at the Danish Headache Center [11]. The present data was collected as part of the larger parental REFORM study. The study protocol was approved by the relevant ethics committee, and all participants provided written informed consent before the commencement of any study-related assessments or procedures. The study was conducted in accordance with the principles of the Declaration of Helsinki. The study was also registered at ClinicalTrials.gov (NCT04592952).
Study Population
The study enrolled adult participants diagnosed with migraine with aura based on the criteria outlined in the International Classification of Headache Disorders, 3rd edition (ICHD-3) [12]. In addition, participants needed to have an average of ≥ 4 monthly migraine days in the 3 months preceding enrolment and ≥ 1 day with migraine with aura in the past year. Participants were also required to report onset of migraine before the age of 50 years and have a documented history of migraine for a minimum of 12 months prior to enrolment. Eligibility also extended to participants who were already receiving stable doses of preventive medication for migraine. The exclusion criteria were primarily a history of headache disorders other than migraine as well as pregnancy or breastfeeding. For a complete list of inclusion and exclusion criteria, the readers are referred to the Supplemental Appendix Table 1.
Study Design and Procedures
This open-label, non-randomized, single-arm trial was conducted at the research facilities of a tertiary care unit from October 2020 to January 2022. The study consisted of 1 screening visit and 1 experimental day. Prior to the experiment, participants had no restrictions on consuming caffeine, cacao, or alcohol as usual. However, they needed to confirm that they hadn’t used any headache medications or experienced a headache within 24 h before the infusion started. During the screening visit, participants underwent a semi-structured interview and a physical examination performed by trained personnel. An electrocardiogram was then performed, and the participants were instructed that CGRP might induce headache. No specific details were disclosed on the possible onset and characteristics of the headache. All participants received a 20-minute continuous intravenous infusion of αCGRP (1.5 µg/min), and the administered dose and timing was identical to the one used in previous human experimental studies [13, 14]. Drug preparation was performed by independent hospital pharmacy staff.
The participants were placed in a supine position, and the antecubital fossa was cannulated to gain intravenous access. A time- and volume-controlled infusion pump was used to administer CGRP, and vital signs (i.e., blood pressure and heart rate) were recorded throughout the 1-hour in-hospital phase. At the time of infusion start, a headache diary was used to collect outcome data on clinical characteristics (including aura), adverse events, and use of rescue medication. These items were then recorded every 10 min until 1 h after the infusion started. Participants were then discharged and asked to complete headache diary hourly until 12 h post-infusion start. If aura symptoms occurred, participants were instructed to fill out a diagnostic aura diary and perform drawings of the visual and sensory aura symptoms. Moreover, participants were allowed, if needed, to treat their headache with rescue medication (e.g., sumatriptan).
Endpoints
The primary endpoint of the study was the incidence of migraine aura within the 12-hour observational period following the initiation of CGRP infusion. Migraine aura was defined based on the fulfilment of criteria B and C for migraine with aura according to ICHD-3 [12] (see the Supplemental Appendix Table 2A). The secondary endpoint was the incidence of migraine headache within the same 12-hour observational period after CGRP infusion. Migraine headache was defined as meeting criteria C and D for migraine without aura according to ICHD-3 [12] (see the Supplemental Appendix Table 2B), or as the participant reporting a headache that resembles their typical migraine headache and necessitates the use of rescue medication during the 12-hour observational period.
Statistical analysis
Normally distributed data are presented as mean values ± standard deviation or range, while non-normally distributed data are reported as median values with interquartile range (IQR) or range. The normality of the data was assessed using the Shapiro-Wilk’s test. The baseline was defined as the time of infusion start. Categorical data are presented as counts and proportions. The Wilcoxon rank sum test was used to compare the median number of yearly aura attacks between participants who developed migraine aura and those who did not. Significance was accepted at P < 0.05. All statistics were performed in R version 4.1.0.
Results
Characteristics of the study population
Thirty-four participants with migraine with aura completed the study. The mean age was 43 ± 14 years, and most participants were women (n = 30). The mean body mass index was 23 ± 4 kg/m2, and 29 (85%) of 34 participants had a diagnosis of migraine with and without aura, whilst 5 (15%) had a diagnosis of migraine with aura exclusively. The median number of migraine attacks with aura was 25 (IQR, 7 to 72) in the past year, and 17 (81%) participants reported current use of preventive medication for migraine. Regarding the aura type, 18 (53%) participants experienced exclusively visual aura, 14 (41%) had both visual and sensory aura, and 2 (6%) reported exclusively sensory aura. Table 1 summarizes the characteristics of the study population.
Migraine aura
During the 12-hour observational period following the start of CGRP infusion, 13 (38%) of 34 participants experienced migraine aura (Table 2). The CGRP-induced aura symptoms predominantly consisted of visual disturbances (n = 10), while sensory disturbances were less common (n = 7). Of the 13 participants, 11 had the onset of migraine aura occur during the 60-minute in-hospital phase.
All 13 participants reported that the CGRP-induced migraine aura closely resembled their typical spontaneous migraine attacks with aura. Among these participants, 10 reported using current preventive medication for migraine. The median time to onset of CGRP-induced migraine aura was 30 min (IQR, 20 to 30) after the start of the infusion (Fig. 1A-C). Twelve of the 13 participants developed migraine aura and migraine headache, while 1 participant developed migraine aura and a headache of severe intensity, but the headache characteristics did not meet the criteria for migraine headache outlined in ICHD-3 (see the Supplemental Appendix Table 3). Regarding migraine headache, the median time to onset was 30 min (IQR, 20 to 53). Moreover, participants who experienced CGRP-induced migraine aura had a higher median number of aura attacks in the past year (60; IQR, 36 to 96), compared with those who did not develop CGRP-induced migraine aura (9; IQR, 5 to 60) (P = 0.03) (Table 1).
A Headache intensity from 0 min to 12 h in participants who reported migraine aura and migraine headache following calcitonin gene-related peptide infusion, The abscissa refers to the time (min). Median (thick, red line) and individual (thin, black lines) headache intensity on NRS. The median time to onset of migraine aura and migraine headache was 30 min (IQR aura, 20 to 30; IQR headache, 20 to 53). The median time to intake rescue medication was 180 min (IQR, 120 to 300). B Headache intensity from 0 min to 12 h in participants who only reported migraine headache following calcitonin gene-related peptide infusion. The abscissa refers to the time (min). Median (thick, red line) and individual (thin, black lines) headache intensity on NRS. The median time to onset of migraine headache was 40 min (IQR, 20 to 120). The median time to intake rescue medication was 120 min (IQR, 60 to 330). C Headache intensity from 0 min to 12 h in participants who did not report migraine aura or migraine headache following calcitonin gene-related peptide infusion. The abscissa refers to the time (min). Median (thick, red line) and individual (thin, black lines) headache intensity an NRS. The median time to onset of headache was 10 min (IQR, 10 to 20). None of these participants took rescue medication
Migraine Headache
During the 12-hour observational period following CGRP infusion, 24 (71%) of 34 participants reported experiencing migraine headache (see the Supplemental Appendix Table 3). As mentioned previously, 12 of these 24 participants also developed migraine aura along with migraine headache. The median time to onset of migraine headache was 40 min (IQR, 20 to 120) after the start of the infusion, and the median peak intensity of the headache was 6 (IQR, 6 to 7). Among the 24 participants who experienced CGRP-induced migraine headache, 13 (54%) reported currently using preventive medication for migraine.
Vital signs, adverse events, and rescue medication
During the 60-minute in-hospital phase, the mean percentagewise increase in heart rate was 38% ± 22%, and the mean percentagewise decrease in blood pressure was 12% ± 12% (see the Supplemental Appendix Fig. 1). Furthermore, post-infusion start, the most common adverse events reported were flushing (n = 33 [97%]), warm sensations (n = 32 [94%]), heart palpitations (n = 21 [62%]), neck pain (n = 20 [59%]), and unusual tiredness (n = 8 [24%]). Moreover, 17 (50%) of 34 required rescue medication to treat their headache.
Discussion
Our study revealed that 13 (38%) of 34 participants developed migraine aura following intravenous infusion of CGRP. Importantly, all induced migraine aura attacks were reported to closely resemble the participants’ usual spontaneous migraine attacks with aura. Another notable observation was that those who experienced migraine aura after CGRP infusion had a higher frequency of migraine aura in the past year, compared with those who did not. These findings provide preliminary evidence indicating that further exploration of therapeutics targeting CGRP signalling could potentially be beneficial in preventing migraine attacks with aura.
CGRP and aura
An intriguing finding from a previous experimental study is that intravenous infusion of CGRP induced migraine aura in 4 (29%) of 14 individuals exclusively diagnosed with migraine with aura [10]. This rate is less than the 38% induction rate in our study. In contrast to the prior study, our participants had a much higher frequency of migraine attacks with aura in the past year, and most of them also experienced migraine attacks without aura. The relationship between the frequency of aura and the coexistence of migraine with and without aura and the susceptibility to develop CGRP-induced migraine aura remains unclear. However, our findings suggest that a higher frequency of aura may increase the likelihood of developing CGRP-induced migraine aura. Table 1 shows no variations between individuals who responded to CGRP infusion and those who did not. Due to the limited size of participants in each grope, no statistical analyses were performed.
When considering the interpretation of our results, it is essential to recognize the potential influence of nocebo effects. This may arise from various factors, including individual psychosocial variables (such as anxiety and stress), the open-label design of our study, and the occurrence of spontaneous attacks. However, in 4 randomized, placebo-controlled trials, migraine aura was only reported in 1 (2%) of 61 participants who received placebo infusion (isotonic saline) (Fig. 2; Table 3) [15,16,17,18]. This suggests that the aura induction rate we observed in our study is less likely to be a result of nocebo effects. Furthermore, it is improbable that the open-label design had a significant impact on the nocebo effect for migraine aura. Across 3 open-label studies involving 55 participants with migraine aura who received glyceryl trinitrate (GTN), only 4 (7%) participants developed migraine aura [19,20,21]. Pooling our previous study [10] and the current one brings the total number of participants who received CGRP to 48, yielding an aura induction rate of 35%, which is higher than that observed after GTN administration. This suggests a response higher than what would be typically expected from nocebo effects among patients with migraine aura.
Human provocation studies investigating migraine aura. *Healthy controls as comparison; **placebo; ***no comparison. GTN, glyceryl trinitrate; CGRP, calcitonin gene-related peptide; CZL, Cilostazol; ET-1, Endothelin-1; LEVC, levcromakalim; SD, Sildenafil. MA, migraine aura exclusively; MA/MO, migraine aura, but not exclusively migraine aura; FHM, familial hemiplegic migraine (unknown mutations); FHM1, familial hemiplegic migraine with known mutations (R583Q and C1369Y mutations); FHM2, familial hemiplegic migraine with known mutations (R202Q and R763C mutations)
It is important to ascertain that the reported migraine auras following CGRP administration were not spontaneous. Given that the median number of migraine aura days in the previous year was 25, the probability of this seems low. With an induction rate of 38%, one would anticipate a median of 139 migraine aura days per year. Another key argument against the occurrence of spontaneous migraine aura is that the median time to onset of CGRP-induced migraine aura was 30 min. Furthermore, among the 13 participants who experienced migraine aura, 10 of them had the aura onset within 1 h of starting the infusion. Given the rapid aura onset following CGRP infusion, it is challenging to argue that spontaneous migraine aura coincidentally occurred during this period. Nevertheless, future placebo-controlled studies are warranted to further confirm migraine aura inducing effects of CGRP.
Our study uncovers a new link between the frequency of aura episodes and susceptibility to CGRP-triggered migraine aura, shedding new light on this complex relationship. Moreover, our data rule out the possibility that the migraine aura induced by CGRP infusion is simply a nocebo effect, removing a significant confounding factor and strengthening the credibility of our conclusions. Finally, we show that the observed migraine aura following CGRP administration is not likely to be spontaneous, given its rapid onset. This finding sets our work apart from previous research and adds to our understanding of CGRP-induced migraine aura, providing a more detailed view that could guide future treatment approaches.
Aura-headache linkage
In the present trial, intravenous infusion of CGRP induced immediate onset of headache in all participants. The onset of migraine aura and migraine headache followed soon after, with 4 participants reporting migraine headache before aura, 3 simultaneously with aura, and 5 after aura onset. Interestingly, 10 of 13 participants who experienced CGRP-induced migraine aura reported that headache sometimes preceded or coincided with the onset of their usual spontaneous migraine attacks with aura. This accords well with an observational study reporting that half of patients with migraine with aura experience migraine headache at the time of aura onset or within 15 min [26].
The linkage between migraine aura and migraine headache remains a topic of ongoing research, marked by the complexities in translating CSD features from animals to clinical features of migraine aura, as well as the inherent difficulties in measuring CSD in humans. Despite these challenges, two concepts have been proposed to explain the aura-headache relationship [27,28,29]. The first concept is known as the sequential concept, which suggests that CSD, manifested as aura, promotes the dilation of intracranial blood vessels and neurogenic inflammation, leading to the development of migraine headache [29]. The second concept is the parallel concept, which proposes that migraine aura and migraine headache are separate events occurring in close temporal relation and in response to a shared initiating factor [27, 28]. Building upon these existing theories, our study provides new insights having identified CGRP as a trigger of not only migraine headache but also migraine aura.
Neurobiological underpinnings of CGRP-induced migraine aura
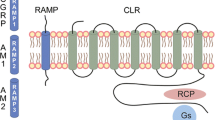
Within the CNS, CGRP and its receptors are found in structures that are central to headache pathophysiology, including the trigeminocervical complex (TCC) and the thalamus [30]. CGRP’s role extends beyond vascular effects, as it modulates nociceptive transmission within the second-order neurons of the TCC in the trigeminovascular pathway [31, 32]. Experimental evidence has shown that introducing CGRP into the periaqueductal gray area can enhance TCC nociceptive transmission [33], while CGRP antagonism has the opposite effect, inhibiting this transmission [32]. In rodent models, the cortical application of potassium chloride has been found to induce CSD and CGRP release [34]. Interestingly, CGRP antagonism has been shown to prevent the activation and sensitization of central trigeminovascular neurons activated by CSD [34]. This finding adds a layer of complexity to our understanding of CGRP’s role in migraine. It is also important to acknowledge that while both fremanezumab and atogepant have failed to completely prevent CSD, they have demonstrated the ability to slow down the propagation of CSD and reduce the duration of cortical recovery following the event [35,36,37]. This understanding of CGRP’s dual role in vascular and non-vascular processes provides important knowledge of migraine pathophysiology and may shape the direction of upcoming therapeutic approaches. In summary, the understanding of CGRP’s dual role in vascular and non-vascular processes provides important knowledge of migraine pathophysiology and may shape the direction of upcoming therapeutic approaches.
Our findings raise an important question regarding the mechanism by which intravenously administered CGRP induces migraine aura, specifically in relation to the CSD. The molecular size of CGRP suggests a limited capability to penetrate the blood-brain barrier, a concept further supported by the absence of middle cerebral artery dilation observed in humans following intravenous infusion [38, 39].
To explain the present results, we therefore propose that intravenously administered CGRP reaches the meningeal arteries and binds to its G protein-coupled receptors on the vascular smooth muscle cells [2, 40, 41]. This binding activates cAMP-dependent pathways, leading to the opening of specific potassium channels, such as ATP-sensitive potassium channels (a recently discovered trigger of migraine aura) [18, 40]. The efflux of potassium then promotes dilation of the meningeal arteries [18, 40, 42]. The combination of increased extracellular potassium and vasodilation is hypothesized to provide chemical and mechanical stimuli, respectively, which activates and sensitizes perivascular primary afferents [2, 41]. The latter transmits nociceptive information to certain cortical and subcortical areas (e.g., somatosensory cortex, visual cortex) through second-order neurons in the brain stem and third-order neurons in the thalamus [2, 41]. Ultimately, the somatosensory cortex and other cortical/subcortical areas are responsible for generating perceptions of cephalic pain, including migraine headache. This proposed sequence of events provides a potential explanation for CGRP-induced migraine headache but might also explain the genesis of CGRP-induced migraine aura, as detailed below.
We hypothesize that the excitatory stimuli reaching areas such as the visual cortex might reach the threshold for CSD initiation in susceptible individuals. Preclinical data does indeed suggest that axonal projections to the visual cortex release the excitatory neurotransmitter glutamate, which lower the threshold for CSD initiation [43,44,45]. Also, functional magnetic resonance imaging studies have demonstrated that nociceptive trigeminal stimulation might activate the visual cortex [38, 46, 47]. This is congruent with preclinical data showing that trigeminal and visual input converge at the level of third-order thalamic neurons, which then project to the visual cortex [43, 48]. Interestingly, visual stimulation with a checkerboard has been shown to elicit migraine aura in people with migraine with aura and this was associated with blood oxygenation level-dependent (BOLD) changes resembling CSD [49,50,51,52]. Taken together, it seems reasonable to assert that CGRP-induced activation of ascending cephalic pain pathways might provide sufficient excitatory stimuli to areas such as the visual cortex which, in turn, results in CSD initiation. Further translational research is warranted to explore the relationship between migraine aura and headache, including what role CGRP plays in this context.
On another note, it is interesting to consider the data regarding the prevention of migraine aura with the use of monoclonal antibodies targeting CGRP signalling [7, 53]. Some evidence suggests that these medications are also effective in people with history of aura, providing additional support for our assertion that CGRP can induce aura without crossing the blood-brain barrier. This is because monoclonal antibodies are much larger molecules than CGRP and have very limited ability to penetrate brain barriers. However, caution is warranted as the efficacy data of these drugs in preventing migraine aura is currently limited by small sample sizes and inadequate methods for evaluating aura [7, 53].
Limitations
We recognize several constraints in our study. A significant portion of participants reported ongoing use of preventative migraine medications, which may have influenced their responsiveness to CGRP infusion. Most participants came from a tertiary referral center, which might limit the applicability of our results to a broader population of individuals with migraine aura. We also omitted an a priori sample size calculation, emphasizing that our study’s primary aim was exploratory. The absence of a placebo arm could have influenced participants’ expectations and responses regarding CGRP-induced migraine aura attacks.
Conclusions
Our study presents novel evidence that intravenous CGRP infusion can induce migraine aura in people with migraine with aura. This indicates that CGRP can trigger CSD, possibly by initiating interactive processes between ascending cephalic pain pathways and CSD-susceptible areas, such as the visual cortex. Moreover, our findings highlight the potential of CGRP-targeted drugs in preventing both migraine headache and aura. Further research is required to unravel the underlying mechanisms of CGRP-induced migraine aura and headache.
Availability of data and materials
Upon reasonable request, the corresponding author will provide the necessary data and materials to interested researchers for the purpose of academic scrutiny, reproducibility, and further scientific investigation.
Abbreviations
- CGRP:
-
Calcitonin gene-related peptide
- CSD:
-
Cortical spreading depolarization
- REFORM:
-
Registry for Migraine
- ICHD-3:
-
International Classification of Headache Disorders, 3rd edition
- IQR:
-
Interquartile range
- FHM:
-
Familial hemiplegic migraine
- TCC:
-
Trigeminocervical complex
- BOLD:
-
Blood oxygenation level-dependent
References
Stovner LJ, Nichols E, Steiner TJ (2018) Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Neurol 17:954–976. https://doi.org/10.1016/S1474-4422(18)30322-3
Ashina M, Migraine N. Engl J Med. 2020;383:1866–1876. https://doi.org/10.1056/NEJMra1915327
Ashina M, Katsarava Z, Do TP et al (2021) Migraine: epidemiology and systems of care. Lancet 397:1485–1495. https://doi.org/10.1016/S0140-6736(20)32160-7
Ayata C, Lauritzen M (2015) Spreading Depression, spreading depolarizations, and the cerebral vasculature. Physiol Rev 95:953–993. https://doi.org/10.1152/physrev.00027.2014
Bolay H, Reuter U, Dunn AK et al (2002) Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nat Med 8:136–142. https://doi.org/10.1038/nm0202-136
Vuralli D, Karatas H, Yemisci M, Bolay H (2021) Updated review on the link between cortical spreading depression and headache disorders. Expert Rev Neurother 21:1069–1084. https://doi.org/10.1080/14737175.2021.1947797
Ashina M, Goadsby PJ, Dodick DW et al (2022) Assessment of Erenumab Safety and Efficacy in patients with migraine with and without aura: a secondary analysis of Randomized clinical trials. JAMA Neurol 79:159–168. https://doi.org/10.1001/jamaneurol.2021.4678
Ashina M, McAllister P, Cady R et al (2022) Efficacy and safety of eptinezumab in patients with migraine and self-reported aura: Post hoc analysis of PROMISE-1 and PROMISE-2. Cephalalgia 42:696–704. https://doi.org/10.1177/03331024221077646
Charles A, Pozo-Rosich P (2019) Targeting calcitonin gene-related peptide: a new era in migraine therapy. Lancet 394:1765–1774. https://doi.org/10.1016/S0140-6736(19)32504-8
Hansen JM, Hauge AW, Olesen J, Ashina M (2010) Calcitonin gene-related peptide triggers migraine-like attacks in patients with migraine with aura. Cephalalgia 30:1179–1186. https://doi.org/10.1177/0333102410368444
Karlsson WK, Ashina H, Cullum CK, Christensen RH, Al-Khazali HM, Amin FM, Ashina M (2023) REFORM Investigators. The Registry for Migraine (REFORM) study: methodology, demographics, and baseline clinical characteristics. J Headache Pain 24(1):70. https://doi.org/10.1186/s10194-023-01604-2
Headache Classification Committee of the International Headache Society (IHS) (2018) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38(1):1–211. https://doi.org/10.1177/0333102417738202
Iljazi A, Ashina H, Zhuang ZA et al (2021) Hypersensitivity to calcitonin gene-related peptide in chronic migraine. Cephalalgia 41:701–710. https://doi.org/10.1177/0333102420981666
Ashina H, Iljazi A, Al-Khazali HM et al (2020) Hypersensitivity to calcitonin gene-related peptide in post-traumatic headache. Ann Neurol 88:1220–1228. https://doi.org/10.1002/ana.25915
Butt JH, Rostrup E, Hansen AS et al (2018) Induction of migraine-like headache, but not aura, by cilostazol in patients with migraine with aura. Brain 141:2943–2951. https://doi.org/10.1093/brain/awy228
Butt JH, Eddelien S, Kruuse H C (2022) The headache and aura-inducing effects of sildenafil in patients with migraine with aura. Cephalalgia 42:984–992. https://doi.org/10.1177/03331024221088998
Hougaard A, Younis S, Iljazi A et al (2020) Intravenous Endothelin-1 infusion does not induce aura or headache in migraine patients with aura. Headache 60:724–734. https://doi.org/10.1111/head.13753
Al-Karagholi MA-M, Ghanizada H, Nielsen CAW et al (2021) Opening of ATP sensitive potassium channels causes migraine attacks with aura. Brain 144:2322–2332. https://doi.org/10.1093/brain/awab136
Afridi KS, Kaube H, Goadsby JP (2004) Glyceryl trinitrate triggers premonitory symptoms in migraineurs. Pain 110:675–680. https://doi.org/10.1016/j.pain.2004.05.007
Sances G, Tassorelli C, Pucci E et al (2004) Reliability of the nitroglycerin provocative test in the diagnosis of neurovascular headaches. Cephalalgia 24:110–119. https://doi.org/10.1111/j.1468-2982.2004.00639.x
Christiansen I, Thomsen L, Daugaard D et al (1999) Glyceryl Trinitrate induces attacks of Migraine without Aura in Sufferers of Migraine with Aura. Cephalalgia 19:660–667. https://doi.org/10.1046/j.1468-2982.1999.019007660.x
Hansen JM, Thomsen LL, Olesen J, Ashina M (2008) Familial hemiplegic migraine type 1 shows no hypersensitivity to nitric oxide. Cephalalgia 28(5):496–505. https://doi.org/10.1111/j.1468-2982.2008.01559.x. Epub 2008 Mar 31
Hansen JM, Thomsen LL, Olesen J, Ashina M (2010) Coexisting typical migraine in familial hemiplegic migraine. Neurology 74(7):594–600. https://doi.org/10.1212/WNL.0b013e3181cff79d
Hansen JM, Thomsen LL, Olesen J, Ashina M (2008) Calcitonin gene-related peptide does not cause the familial hemiplegic migraine phenotype. Neurology 71(11):841–7. https://doi.org/10.1212/01.wnl.0000325482.64106.3f
Hansen JM, Thomsen LL, Olesen J, Ashina M (2011) Calcitonin gene-related peptide does not cause migraine attacks in patients with familial hemiplegic migraine. Headache 51(4):544–53. https://doi.org/10.1111/j.1526-4610.2011.01861.x
Hansen JM, Lipton RB, Dodick DW et al (2012) Migraine headache is present in the aura phase: a prospective study. Neurology 79:2044–2049. https://doi.org/10.1212/WNL.0b013e3182749eed
Spierings ELH (2002) Parallel concept of migraine pathogenesis. Ann Neurol 51:139–140. https://doi.org/10.1002/ana.10026
Spierings EL (1988) Recent advances in the understanding of migraine. Headache 28:655–658. https://doi.org/10.1111/j.1526-4610.1988.hed2810655.x
Akkermans R (2015) Harold G Wolff. Lancet Neurol 14:982–983. https://doi.org/10.1016/s1474-4422(15)00184-2
Warfvinge K, Edvinsson L, Pickering DS, Sheykhzade M (2019) The Presence of Calcitonin Gene-Related peptide and its receptors in rat, Pig and Human Brain: species differences in calcitonin gene-related peptide pharmacology. Pharmacology 104:332–341. https://doi.org/10.1159/000502471
Summ O, Charbit AR, Andreou AP, Goadsby PJ (2010) Modulation of nocioceptive transmission with calcitonin gene-related peptide receptor antagonists in the thalamus. Brain 133:2540–2548. https://doi.org/10.1093/brain/awq224
Storer RJ, Akerman S, Goadsby PJ (2004) Calcitonin gene-related peptide (CGRP) modulates nociceptive trigeminovascular transmission in the cat. Br J Pharmacol 142:1171–1181. https://doi.org/10.1038/sj.bjp.0705807
Pozo-Rosich P, Storer R, Charbit A, Goadsby P (2015) Periaqueductal gray calcitonin gene-related peptide modulates trigeminovascular neurons. Cephalalgia 35:1298–1307. https://doi.org/10.1177/0333102415576723
Close LN, Eftekhari S, Wang M et al (2019) Cortical spreading depression as a site of origin for migraine: role of CGRP. Cephalalgia 39:428–434. https://doi.org/10.1177/0333102418774299
Schain AJ, Melo-Carrillo A, Stratton J et al (2019) CSD-Induced arterial dilatation and plasma protein extravasation are unaffected by Fremanezumab: implications for CGRP’s role in migraine with aura. J Neurosci 39:6001–6011. https://doi.org/10.1523/JNEUROSCI.0232-19.2019
Melo-Carrillo A, Schain AJ, Stratton J et al (2020) Fremanezumab and its isotype slow propagation rate and shorten cortical recovery period but do not prevent occurrence of cortical spreading depression in rats with compromised blood–brain barrier. Pain 161:1037–1043. https://doi.org/10.1097/j.pain.0000000000001791
Strassman AM, Melo-Carrillo A, Houle TT et al (2022) Atogepant – an orally-administered CGRP antagonist – attenuates activation of meningeal nociceptors by CSD. Cephalalgia 42:933–943. https://doi.org/10.1177/03331024221083544
Asghar MS, Becerra L, Larsson HBW et al (2016) Calcitonin gene-related peptide modulates Heat Nociception in the human brain - an fMRI study in healthy volunteers. PLoS ONE 11:e0150334. https://doi.org/10.1371/journal.pone.0150334
Wiggers A, Ashina H, Hadjikhani N et al (2022) Brain barriers and their potential role in migraine pathophysiology. J Headache Pain 23:16. https://doi.org/10.1186/s10194-021-01365-w
Al-Karagholi MA-M, Hansen JM, Guo S et al (2019) Opening of ATP-sensitive potassium channels causes migraine attacks: a new target for the treatment of migraine. Brain 142:2644–2654. https://doi.org/10.1093/brain/awz199
Ashina M, Terwindt GM, Al-Karagholi MA-M et al (2021) Migraine: disease characterisation, biomarkers, and precision medicine. Lancet 397:1496–1504. https://doi.org/10.1016/S0140-6736(20)32162-0
Al-Karagholi MA-M, Ghanizada H, Hansen JM et al (2019) Extracranial activation of ATP-sensitive potassium channels induces vasodilation without nociceptive effects. Cephalalgia 39:1789–1797. https://doi.org/10.1177/0333102419888490
Noseda R, Kainz V, Jakubowski M et al (2010) A neural mechanism for exacerbation of headache by light. Nat Neurosci 13:239–245. https://doi.org/10.1038/nn.2475
Noseda R, Kainz V, Borsook D, Burstein R (2014) Neurochemical pathways that converge on thalamic trigeminovascular neurons: potential substrate for modulation of migraine by sleep, food intake, stress and anxiety. PLoS ONE 9:e103929. https://doi.org/10.1371/journal.pone.0103929
Kharazia VN, Weinberg RJ (1994) Glutamate in thalamic fibers terminating in layer IV of primary sensory cortex. J Neurosci 14:6021–6032. https://doi.org/10.1523/JNEUROSCI.14-10-06021.1994
Ziegeler C, Mehnert J, Asmussen K, May A (2020) Central effects of erenumab in migraine patients: an event-related functional imaging study. Neurology 95:e2794–e2802. https://doi.org/10.1212/WNL.0000000000010740
Billot P-E, Comte A, Galliot E et al (2011) Time course of odorant- and trigeminal-induced activation in the human brain: an event-related functional magnetic resonance imaging study. Neuroscience 189:370–376. https://doi.org/10.1016/j.neuroscience.2011.05.035
Noseda R, Jakubowski M, Kainz V et al (2011) Cortical projections of functionally identified thalamic trigeminovascular neurons: implications for migraine headache and its associated symptoms. J Neurosci 31:14204–14217. https://doi.org/10.1523/JNEUROSCI.3285-11.2011
Hougaard A, Amin FM, Hauge AW et al (2013) Provocation of migraine with aura using natural trigger factors. Neurology 80:428–431. https://doi.org/10.1212/WNL.0b013e31827f0f10
Cao Y, Welch KM, Aurora S, Vikingstad EM (1999) Functional MRI-BOLD of visually triggered headache in patients with migraine. Arch Neurol 56:548–554. https://doi.org/10.1001/archneur.56.5.548
Cao Y, Aurora SK, Nagesh V et al (2002) Functional MRI-BOLD of brainstem structures during visually triggered migraine. Neurology 59:72–78. https://doi.org/10.1212/wnl.59.1.72
Bowyer SM, Aurora KS, Moran JE et al (2001) Magnetoencephalographic fields from patients with spontaneous and induced migraine aura. Ann Neurol 50:582–587. https://doi.org/10.1002/ana.1293
Schoenen J, Timmermans G, Nonis R et al (2021) Erenumab for Migraine Prevention in a 1-Year compassionate use program: efficacy, tolerability, and differences between clinical phenotypes. Front Neurol 12:805334. https://doi.org/10.3389/fneur.2021.805334
Acknowledgements
The authors thank all the study participants and the research staff the Danish Headache Center (Mohammad B. (A) Lafta, Sarra Al-Khazali, Amir Al-Saoudi, Merete (B) Bertelsen, and Janne Jensen).
Funding
Open access funding provided by Royal Library, Copenhagen University Library This study was funded by a research grant from the Lundbeck Foundation (R310-2018-3711).
Author information
Authors and Affiliations
Contributions
All authors had full access to and take responsibility for the integrity and accuracy of the data analysis. HA, AI, FMA, HS, and MA conceptualized and designed the study. All authors were responsible for data acquisition, analysis, and interpretation. HMA, AW, and KR drafted the manuscript, while all authors provided critical revisions for important intellectual content. HA, FMA, HS, and MA supervised the study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of Capital Region, Denmark, and and written informed consent was obtained from all participants.
Competing interests
HA reports receiving personal fees from Teva outside of the submitted work. HS reports receiving personal fees from AbbVie, Teva, Lundbeck, Novartis, Eli Lilly, outside of the submitted work. FMA reports receiving personal fees from Pfizer, Teva, Lundbeck, Novartis, and Eli Lilly outside of the submitted work. MA reports receiving personal fees from AbbVie, Amgen, Eli Lilly, GlaxoSmithKline, Lundbeck, Novartis, Pfizer, and Teva Pharmaceuticals outside of the submitted work. MA also serves as an associate editor of Cephalalgia, an associate editor of The Journal of Headache and Pain, and an associate editor of Brain. The remaining authors report no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional File 1:
Supplementary Material. Figure 1. MAP and HR after infusion of calcitonin gene-related peptide. Table 1. Inclusion and exclusion criteria. Table 2A. Criteria B and C for migraine aura according to ICHD-3. Table 2B. Criteria C and D for migraine without aura according to ICHD-3. Table 3. Clinical characteristics of headache and associated symptoms in participants with migraine after calcitonin gene-related peptide provocation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Al-Khazali, H.M., Ashina, H., Wiggers, A. et al. Calcitonin gene-related peptide causes migraine aura. J Headache Pain 24, 124 (2023). https://doi.org/10.1186/s10194-023-01656-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-023-01656-4