Abstract
Background
The efficacy and safety of OnabotulinumtoxinA (BOTOX®) in adults with chronic migraine (CM) were demonstrated in the PREEMPT program. However, the dosage used in this study was flexible from 155 U to 195 U at the physician’s discretion. Therefore, the objective of this prospective study was to compare the efficacy and safety of OnabotulinumtoxinA 195 U vs. 155 U for the treatment of CM and medication overuse headache (MOH) during a 2-year period.
Methods
We prospectively evaluated the mean reduction in headache days, migraine days, acute pain medication intake days and Headache Impact Test (HIT)-6 score in 172 patients injected with OnabotulinumtoxinA 195 U. Successively, we compared the efficacy measures with data of 155 patients injected with OnabotulinumtoxinA 155 U and followed up for 2 years. All patients were affected by CM and MOH, and failed one or more previous detoxification and preventative therapies.
Results
Both OnabotulinumtoxinA 195 U and 155 U reduced significantly the number of headache and migraine days, acute pain medication intake days and HIT-6 score, when compared with the baseline measures. Nevertheless, OnabotulinumtoxinA 195 U proved to be superior of 155 U in all efficacy measures since the first injection and for all the 2 years of treatment, with the exception of the reduction in pain medication intake days that resulted significantly larger with 195 U only after the 4th injection. The safety and tolerability of the two doses were similar and treatment related adverse events were transient and mild-moderate.
Conclusions
This study represents the largest and longest post-marketing studies of doses comparison with OnabotulinumtoxinA in a real-life clinical setting.
Here, we demonstrate the superior efficacy of OnabotulinumtoxinA 195 U compared to 155 U in CM patients with MOH during a 2-year treatment period with similar safety and tolerability profile.
Similar content being viewed by others
Background
Migraine has a large individual and socioeconomic burden of disease and, globally, is currently considered the sixth most influential disabling condition according to World Health Organization [1, 2].
Chronic migraine (CM) is a complex and debilitating neurological disorder with a prevalence ranging 1–3 % of the general population and an incidence estimated to be 2.5 % per year [3].
Patients with CM are more likely to have a lower health-related quality of life (HRQoL), greater lost productive time, and greater healthcare resource utilization than episodic migraine patients [4–6].
A significant proportion of patients with CM have a high intake of abortive medications. It is estimated that around 50–80 % of patients with CM referring to headache clinics show analgesic overuse that may lead to the development of medication overuse headache (MOH) [7]. There is not a complete agreement whether MOH is a consequence or a cause of CM [8].
In presence of MOH, prophylactic treatment will be more effective after an adequate withdrawal from the overused medication [9, 10]. At present, prophylactic treatment options are limited and only around the 33 % of CM patients report to be treated and take prophylactic medications [11].
For decades, antiepileptic drugs (e.g., topiramate, divalproex sodium), antihypertensive agents (e.g., beta blockers, calcium channel blockers, angiotensin-converting enzyme [ACE] inhibitors, aldosterone receptor blockers) and tricyclic antidepressants (e.g., amitriptyline, nortriptyline) have been used “off-label” in CM prevention.
Nowadays, OnabotulinumtoxinA is the unique drug specifically indicated for prophylaxis of headache in adult patients with CM [12]. This indication is based on the result of two large-scale, placebo-controlled, multicenter trials (PREEMPT: Phase 3 REsearch Evaluating Migraine Prophylaxis Therapy) that demonstrated the efficacy, safety and tolerability of OnabotulinumtoxinA (155–195 U) as a prophylactic treatment for CM in adults [13–15].
The OnabotulinumtoxinA administration used in the PREEMPT protocol required the intramuscular injection of 155 U of OnabotulinumtoxinA in 31 sites across 7 head and neck muscles using a “fixed-site, fixed-dose” (FSFD) injection paradigm (each injection was 5 U) [16]. Up to 40 U of additional OnabotulinumtoxinA could have been injected at the physician’s discretion using a “follow the pain” (FTP) strategy in 8 additional sites across 3 head and neck muscles [16].
The mechanisms by which OnabotulinumtoxinA decreases the frequency and intensity of pain attacks in CM patients have not been clearly clarified yet. It is known that the activation of the trigeminovascular system is accompanied by release of vasoactive neuropeptides from the presynaptic nerve terminals around leptomeningeal and pericranial vessels [17]. The local release of these neuropeptides induces vasodilation and neurogenic inflammation [17]. Repeated episodes of activation of the trigeminovascular system can sensitize central pain pathways and lead to migraine chronicization [18]. OnabotulinumtoxinA inhibits the release of neurotransmitters (such as serotonin, noradrenaline, dopamine, Gamma-Amynobutirric Acid [GABA], acetylcholine, glutamate, substance P, and Calcitonin Gene-Related Peptide [CGRP]) from peripheral terminals of primary afferents [19], thereby preventing the neurogenic inflammation. Consequently, the peripheral sensitization of nociceptive nerve fibers is inhibited and indirectly reduces the central sensitization [20]. Moreover, it has been recently hypothesized that the antinociceptive effect could not be only dependent from a peripheral mechanism of action of the toxin, but even centrally mediated and axonal transport-dependent [21].
Our experience with OnabotulinumtoxinA for the prevention of chronic daily headaches started in 2001 [22]. In our Headache Clinic the preventive treatment with OnabotulinumtoxinA was offered to all the adults patients that were affected by CM with or without medication overuse (diagnosis made according with the IHS criteria 2004 revised in 2006) (Headache Classification Subcommittee; Headache Classification Committee) [23, 24]. We offered such treatment only to patients with contraindications or lack of efficacy or tolerability to other preventive drugs (beta-blockers, calcium channel blockers, antiepileptics and antidepressants). We did not offer OnabotulinumtoxinA treatment to patients with co-morbid neuromuscular disorders, psychiatric diseases considered incompatible with such kind of treatment, pregnancy and breast-feeding.
Since 2010, we have strictly followed the injection paradigm proposed in the PREEMPT studies [16] using only the FSFD paradigm (155 U in 31 injection sites) and, since 2012, we adopted as standard the combined paradigm FSFD+ FTP (195 U in 39 injection sites) for all the new patients treated with OnabotulinumtoxinA.
With the except of the PREEEMPT studies, large and long-term studies on OnabotulinumtoxinA efficacy and safety have not been published. Moreover, the PREEMPT studies allowed the variable dose from 155 to 195 U, following the pain localization. In this prospective study, we used the 195 U dose and we compared the efficacy and safety profile for the treatment of CM and MOH with a population treated with 155 U over a 2 years period.
Methods
The protocol was reviewed and approved by the Ethical Committee of Sant’Andrea Hospital, Sapienza University of Rome. Each patient gave a free, informed consent for the participation in the study and the analysis and publication of the protocol data.
We included in the study all the patients affected by CM with MOH, able to fill diaries without any lack of information, referred to our Headache Clinic between January 2012 and January 2013 and followed up for two years.
All patients overused acute pain medications during the one-month baseline period. Medication overuse was defined as simple analgesics intake on ≥15 days, or other medication types or combination of types intake for ≥10 days, with intake ≥2 days/week from the category of overuse.
We included only patients with criteria for MOH who had failed one or more withdrawal attempt, and all the CM patients who had received and failed other preventive therapies due to lack of efficacy or intolerable side effects. Any patient was allowed to take other preventive oral medication during treatment with OnabotulinumtoxinA.
Patients were treated with OnabotulinumtoxinA injections, in multiple sites, combining the “FDFS” and the “FTP” injection paradigm according to the protocol of the PREEMPT study, at the dosage of 195 U for 39 sites. Every session of local injection was repeated every 3 months (±1 week) during a 2-year period.
Headache days, migraine days, and acute pain medication intake were used as efficacy measures. Baseline data were collected from patients headache diary referred to the previous month before starting OnabotulinumtoxinA, and patients were evaluated every three months at the time of each injection. Every six months patients were asked to fill the Headache Impact Test (HIT)-6, used as a measure of efficacy as well, and the results were compared with the baseline score. During the 24 months all adverse events (AEs), related to the drug, were registered and used as a safety measure.
To evaluate if the 195 U was associate with a different efficacy and tolerability than the 155 U, we compared our outcomes with those from a population of patients treated with OnabotulinumtoxinA 155 U and followed up for 2 years with the same injections and clinical evaluation schedule [25].
Continuous variables are reported as mean ± standard deviation, rates and categorical values are reported as subjects-counts and percentage. In the population treated with OnabotulinumtoxinA 195 U, paired t-Test was used to compare the mean headache days, migraine days, medication intake days and HIT-6 score at baseline and at each cycle of injections after Hartley’s ƒ-Max test to assess equal variance of data. A χ 2 test was used to compare categorical variables.
The comparison between OnabotulinumtoxinA 155 U and 195 U was performed using the Student’s t-Test for the continuous variables and the χ2 test for the categorical variables. p ≤ 0.05 was considered statistically significant.
Results
Demographic and baseline headache characteristics
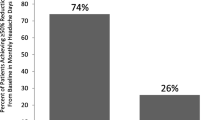
The initial population included was of 172 patients but only 143 patients completed the 2 years follow-up. Table 1 shows the reasons for OnabotulinumtoxinA discontinuation before 24 months.
Demographic and baseline headache characteristics of the 143 patients who completed the protocol are reported in Table 2, together with the comparison with the same demographic data of 132 patients treated with 155 U.
The majority of patients were female (79.7 %), with mean age 44.9 years (range 18–78). The average time since onset of CM was 9.3 years (range 1–40) (Table 2).
The 95.8 % of patients had a severe (≥60) HIT-6 score. No statistically significant differences in demographic and clinical characteristics at baseline were found between the 155 U and 195 U groups of patients (Table 2).
Efficacy of 195 U
The comparison of all pre- and post-treatment outcomes is shown in Table 3. The headache days per month decreased significantly during the period of treatment from the first to the eighth session of therapy (pre 22.2 ± 4.9, post 4.1 ± 1.0; p < 0.001).
There was also a significant reduction of the migraine days per month during the period of treatment from the first to the eighth session of therapy (pre 21.6 ± 4.8, post 3.8 ± 1.0; p < 0.001).
Accordingly, also medication intake days decreased significantly during the period of treatment from the first to the eighth session of therapy (pre 21.0 ± 5.1, post 3.7 ± 1.3; p < 0.001).
The mean HIT-6 score decreased significantly during the period of treatment from the first to the last injection (pre 67.9 ± 4.2, post 49 ± 6.7; p < 0.001), and the proportion of patients with severe (≥60) HIT-6 score decreased as well (pre 95.8 %, post 15.4 %) (Additional file 1: Table S1). After two years of treatment the mean HIT-6 score was ≤55 (some impact, little or no impact) in 68.2 % of patients and ≤49 (little or no impact) in 40.9 % of patients (data not shown). Notably, all the efficacy measures showed a progressive reduction over the 2 years of treatment, that resulted all significant when compared with baseline measures.
Comparison between 195 U and 155 U
A graphic comparison of all pre- and post-treatment outcomes in the two populations treated with OnabotulinumtoxinA 195 U and 155 U are shown in Figs. 1, 2, 3 and 4.
Although both dosages were per se effective in reducing headache days frequency since the first injection, OnabotulinumtoxinA 195 U was significantly more effective than the 155 U in reducing the mean headache days at every time point (p < 0.001) (Fig. 1, Additional file 1: Table S2).
There was also a significantly larger reduction of migraine days in the group treated with 195 U (p < 0.001) (Fig. 2, Additional file 1: Table S3). Moreover, OnabotulinumtoxinA 195 U also significantly decreased medication intake days per month, even if only after the second injection (p < 0.001) (Fig. 3, Additional file 1: Table S4).
Similar results were evident also when comparing the mean HIT-6 score between the 195 U and the 155 U treated groups. In fact, OnabotulinumtoxinA 195 U was significantly more effective in reducing the mean HIT-6 score during all the treatment period (p < 0.05) (Fig. 4, Additional file 1: Table S5), even if the proportion of patients with severe (≥60) HIT-6 score was not significantly different between the 195 U and the 155 U groups, with the exception of the third injection time (Additional file 1: Table S1).
Safety and tolerability
Treatment-related AEs were consistent with the known tolerability profile of OnabotulinumtoxinA and were not significantly different between the 195 U and the 155 U treated patients (Table 4). In both groups, the AEs were mild to moderate for severity and persisted for less than a week (e.g., headache, injection-site pain) to a maximum of two months (e.g., eyelid ptosis, cervical musculoskeletal weakness).
Some AEs occurred more frequently during the first three cycles of injections for both groups (>75 % of all the cases of neck pain and musculoskeletal weakness), whereas others AEs did not show any correlation with the treatment cycle (e.g., headache, eyelid ptosis and injection-site pain) (data not shown).
Discussion
CM is a serious clinical condition with high risk of medication overuse given by the frequent partial response to treatment, both abortive and preventive. Therefore, the opportunity to provide new effective therapeutic options to patients represents a crucial step in CM treatment [26].
The PREEMPT clinical trials showed that OnabotulinumtoxinA is a safe, well-tolerated, and effective prophylactic therapy for CM patients [13, 14]. To date, the PREEMPT clinical program is the largest (1384 patients) and longest (24-week, double-blind period followed by a 32-week, open-label phase) study in CM [15].
Its remarkable results led to the worldwide specific indication of OnabotulinumtoxinA for the prevention of headache in CM patients [16].
One of the criticisms made to the PREEMPT study design regarded the high percentage (nearly 40 %) of the CM recruited patients that have never received other drugs for migraine prophylaxis. Therefore, in this study we recruited only CM patients that already failed other preventive treatments that were subsequently treated with OnabotulinumtoxinA for 24 months, without taking any other prophylactic treatment.
Several studies have demonstrated that repeated injections over time are able to increase the benefit obtained after the first cycle of treatment, with a prophylactic cumulative effect [27, 28]. In this study, we demonstrated the efficacy and safety of OnabotulinumtoxinA 195 U in the CM with MOH treatment, over a period of 24 months.
Moreover, even if 195 U and the 155 U doses were both effective and safe in the treatment of CM with MOH [25], we found the higher dose being significantly more effective then the 155 U in terms of mean reduction of headache days, migraine days, pain medication intake days and HIT-6 score. Only the severe HIT-6 score proportion of patients did not significantly differ between OnabotulinumtoxinA 195 U and 155 U over the 24 months, with the exception of the second injection time (6 months) in which the 195 U proportion of HIT-6 severe patients resulted significantly lower. These results suggest that the OnabotulinumtoxinA higher dose treatment lead to a faster reduction of the HIT-6 score. The 195 U superior efficacy in all the considered measures was evident since the first injection and was maintained over a period of two years, with the exception of the mean medication intake days reduction that was larger with 195 U only after 6 months.
CM prevention and reduction of attacks might also be essential for the cardiovascular risk reduction, as CM represents an independent risk factor for cardiovascular disorders and ischemic stroke [29]. The reduced attacks frequency implies a greater intake of non-steroidal anti-inflammatory drugs (NSAIDs) and triptans, both associated with a greater likelihood of developing cardiovascular events [29]. Therefore, the greater efficacy of 195 U with respect to 155 U in reducing migraine, headache and medication intake days might be also associated with a larger reduction of cardiovascular risk.
Migraine patients often suffer greatly as a result of the systemic AEs related to the prophylactic drugs, reporting a reduced attention, somnolence, tremor, dizziness, fatigue, depression, loss of appetite, weight gain, hair loss and changes in libido. These side effects are not known in association with OnabotulinumtoxinA.
The safety and tolerability of OnabotulinumtoxinA 195 U were similar to that of OnabotulinumtoxinA 155 U. In our study we enrolled only CM with coexisting MOH patients. We strongly believe that MOH might be a consequence of CM and not just a simple and distinct form of secondary headache [30].
One of the major criticisms made to the PREEMPT studies was about the diagnosis of CM. In fact, in PREEMPT studies, the 65.3 % of patients had medication overuse, which, according to the ICHD-II, precluded the diagnosis of CM [24]. In PREEMPT studies the decision to not to exclude patients overusing acute medications was based on a consultation with the Task Force of the International Headache Society Clinical Trials Subcommittee [31]. In fact, the Task Force guidelines for controlled trials of CM prophylactic treatment in adults recommended the inclusion and stratification of medications overusing patients in clinical studies [32]. Accordingly, a sub-group analysis of the PREEMPT data showed OnabotulinumtoxinA to be equally effective in patients affected by CM with medication overuse [33]. In this study, we provided further evidence in clinical setting of the OnabotulinumtoxinA efficacy for the headache prophylaxis in CM with MOH patients.
Several studies suggest that some migraineurs respond better to OnabotulinumtoxinA than others. A better response has been seen in: CM patients with unilateral headache, pericranial allodynia and pericranial muscle tenderness [34, 35]; those with imploding headache and ocular headache [36]; those with a shorter disease duration (<30 years) [37]; and those with elevated interictal plasma levels of CGRP and vasoactive intestinal peptide (VIP) [38]. Conversely, the prevalence of aura, photophobia, phonophobia, osmophobia, nausea, and throbbing are similar between responders and non-responders [36]. Similarly the presence of white matter lesions at MRI scans did not show the ability to predict a positive response to OnabotulinumtoxinA [39]. In this study, we did not evaluated inter-individual variations in headache features, that might be predictive of a OnabotulinumtoxinA better response, but we can state that the MOH presence do not affect OnabotulinumtoxinA efficacy in CM prophylaxis.
The pharmacologic profile of OnabotulinumtoxinA makes it an appealing candidate for CM patients. Its long duration of action (3 months on average) is attractive for patients with poor compliance to the daily use of preventive medications [40], while its good safety profile makes it the best option when other preventive medications are poor tolerated or non-effective.
OnabotulinumtoxinA mechanism of action is poorly understood. Recent studies have shown that OnabotulinumtoxinA is able to modulate the inflammatory mediators in the trigeminal ganglion [41] and decrease interictal CGRP plasma levels in patients with CM [42], and therefore be effective in the migraine attacks prevention.
There are still questions open in the OnabotulinumtoxinA treatment for CM, such as the possible existence of response predictors (biomarkers, clinical features), the possible OnabotulinumtoxinA paradigm variations depending on the extent of the response, the possible superior efficacy of concomitant oral prophylactic therapies and the optimal management of patients after 2 years of treatment.
Conclusions
We believe that these results represent the largest and longest post-marketing study of doses comparison with OnabotulinumtoxinA in a real-life clinical setting.
OnabotulinumtoxinA administered at 195 U proved to have indisputable advantages over the 155 U: higher efficacy and same safety and tolerability profile maintained even after a long period of treatment.
On the basis of our results we suggest that the prevention of headache in CM with MOH should be obtained with the higher OnabotulinumtoxinA dosage.
References
Global Burden of Disease Study 2013 Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386:743–800
Steiner TJ, Birbeck GL, Jensen RH, Katsarava Z, Stovner LJ, Martelletti P (2015) Headache disorders are third cause of disability worldwide. J Headache Pain 16:58
Natoli JL, Manack A, Dean B, Butler Q, Turkel CC, Stovner L, Lipton RB (2010) Global prevalence of chronic migraine: a systematic review. Cephalalgia 30:599–609
Buse DC, Manack A, Serrano D, Turkel C, Lipton RB (2010) Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J Neurol Neurosurg Psychiatry 81:428–432
Blumenfeld AM, Varon SF, Wilcox TK, Buse DC, Kawata AK, Manack A, Goadsby PJ, Lipton RB (2011) Disability, HRQoL and resource use among chronic and episodic migraineurs: Results from the International Burden of Migraine Study (IBMS). Cephalalgia 31:301–315
Stewart WF, Wood GC, Manack A, Varon SF, Buse DC, Lipton RB (2010) Employment and work impact of chronic migraine and episodic migraine. J Occup Environ Med 52:8–14
Deiner HC, Limmroth V (2004) Medication overuse headache: a worldwide problem. Lancet Neurol 3:475–483
Negro A, D’Alonzo L, Martelletti P (2010) Chronic migraine: comorbidities, risk factors, and rehabilitation. Intern Emerg Med 5(Suppl 1):S13–S19
Negro A, Rocchietti-March M, Fiorillo M, Martelletti P (2011) Chronic migraine: current concepts and ongoing treatments. Eur Rev Med Pharmacol Sci 15:1401–1420
Zeeberg P, Olesen J, Jensen R (2006) Discontinuation of medication overuse in headache patients: recovery of therapeutic responsiveness. Cephalalgia 26:1192–1198
Bigal ME, Serrano D, Reed M, Lipton RB (2008) Chronic migraine in the population: burden, diagnosis, and satisfaction with treatment. Neurology 71:559–566
Allergan Inc (2013) BOTOX (onabotulinumtoxinA) full prescribing information. Allergan Inc, Irvine
Aurora SK, Dodick DW, Turkel CC, DeGryse RE, Silberstein SD, Lipton RB, Diener HC, Brin MF, PREEMPT 1 Chronic Migraine Study Group (2010) OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia 30:793–803
Diener HC, Dodick DW, Aurora SK, Turkel CC, DeGryse RE, Lipton RB, Silberstein SD, Brin MF, PREEMPT 2 Chronic Migraine Study Group (2010) OnabotulinumtoxinA for threat- ment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalalgia 30:804–814
Dodick DW, Turkel CC, DeGryse RE, Aurora SK, Silberstein SD, Lipton RB, Diener HC, Brin MF, PREEMPT Chronic Migraine Study Group (2010) OnabotulinumtoxinA for treatment of chronic migraine: pooled results from the double-blind, ran- domized placebo-controlled phases of the PREEMPT clinical program. Headache 50:921–936
Blumenfeld A, Silberstein SD, Dodick DW, Aurora SK, Turkel CC, Binder WJ (2010) Method of injection of onabotulinumtoxinA for chronic migraine: a safe, well-tolerated, and effective treatment paradigm based on the PREEMPT clinical program. Headache 50:1406–1418
Edvinsson L, Uddman R (2005) Neurobiology in primary headaches. Brain Res Brain Res Rev 48:438–456
Seybold VS (2009) The role of peptides in central sensitization. Handb Exp Pharmacol 194:451–491
Aoki KR (2005) Review of a proposed mechanisms for the antinociceptive action of botulinum toxin type A. Neurotoxicology 26:785–793
Mathew NT (2011) Pathophysiology of chronic migraine and mode of action of preventive medications. Headache 51:84–92
Matak I, Lacković Z (2014) Botulinum toxin A, brain and pain. Prog Neurobiol 119–120:39–59
Farinelli I, Coloprisco G, De Filippis S, Martelletti P (2006) Long-term benefits of botulinum toxin type A (BOTOX) in chronic daily headache: a five-year long experience. J Headache Pain 7:407–412
Headache Classification Subcommittee of the International Headache Society (2004) The International classification of headache disorders-2nd edition. Cephalalgia 24(suppl 1):1–160
Headache Classification Committee, Olesen J, Bousser MG, Diener HC, Dodick D, First M, Goadsby PJ, Göbel H, Lainez MJ, Lance JW, Lipton RB, Nappi G, Sakai F, Schoenen J, Silberstein SD, Steiner TJ (2006) New appendix criteria open for a broader concept of chronic migraine. Cephalalgia 26:742–746
Negro A, D’Alonzo L, Lala N, Martelletti P (2015) A 2-year prospective evaluation study on onabotulinumtoxinA 155 U in chronic migraine. J Headache Pain 16(Suppl 1):A137. doi:10.1186/1129-2377-16-S1-A137
Lionetto L, Negro A, Palmisani S, Gentile G, Del Fiore MR, Mercieri M, Simmaco M, Smith T, Al-Kaisy A, Arcioni R, Martelletti P (2012) Emerging treatment for chronic migraine and refractory chronic migraine. Expert Opin Emerg Drugs 17:393–406
Aurora SK, Dodick DW, Diener HC, Aurora SK, Dodick DW, Diener HC, DeGryse RE, Turkel CC, Lipton RB, Silberstein SD et al (2014) Onabotulinumtoxin A for chronic migraine: efficacy, safety and tolerability in patients who received all five treatment cycles in the PREEMPT clinical program. Acta Neurol Scand 129:61–70
Silberstein SD, Dodick WD, Aurora SK, Dienere H-C, DeGryse RE, Lipton RB, Turkel CC (2015) Per cent of patients with chronic migraine who responded per onabotulinumtoxinA treatment cycle: PREEMPT. J Neurol Neurosurg Psychiatry 86:996–1001
Tana C, Tafuri E, Tana M, Martelletti P, Negro A, Affaitati G, Fabrizio A, Costantini R, Mezzetti A, Giamberardino MA (2013) New insights into the cardiovascular risk of migraine and the role of white matter hyperintensities: is gold all that glitters? J Headache Pain 14:9
Negro A, Martelletti P (2011) Chronic migraine plus medication overuse headache: two entities or not? J Headache Pain 12:593–601
Aurora S, Diener HC, Dodick D, PREEMPT Chronic Migraine Study Group (2011) Reply: clinical trials on onabotulinumtoxinA for the treatment of chronic migraine. J Headache Pain 12:137–138
Silberstein S, Tfelt-Hansen P, Dodick DW, Limmroth V, Lipton RB, Pascual J, Wang SJ, Task Force of the International Headache Society Clinical Trials Subcommittee (2008) Guidelines for controlled trials of prophylactic treatment of chronic migraine in adults. Cephalalgia 28:484–495
Silberstein SD, Blumenfield AM, Cady RK, Turner IM, Lipton RB, Deiner HC, Aurora SK, Sirimanne M, DeGryse RE, Turkel CC, Dodick DW (2013) OnabotulinumtoxinA for treatment of chronic migraine: PREEMPT 24-week pooled subgroup analysis of patients who had acute headache medication overuse at baseline. J Neurol Sci 331:48–56
Mathew NT, Kailasam J, Meadors L (2008) Predictors of response to botulinum toxin type A (BoNTA) in chronic daily headache. Headache 48:194–200
Sandrini G, Perrotta A, Tassorelli C, Torelli P, Brighina F, Sances G, Nappi G (2011) Botulinum toxin type-A in the prophylactic treatment of medication-overuse headache: a multicenter, double-blind, randomized, placebo-controlled, parallel group study. J Headache Pain 12:427–433
Jakubowski M, McAllister PJ, Bajwa ZH, Ward TN, Smith P, Burstein R (2006) Exploding vs. imploding headache in migraine prophylaxis with botulinum toxin A. Pain 125:286–295
Eross EJ, Gladstone JP, Lewis S, Rogers R, Dodick DW (2005) Duration of migraine is a predictor for response to botulinum toxin type A. Headache 45:308–314
Cernuda-Morollón E, Martínez-Camblor P, Ramón C, Larrosa D, Serrano-Pertierra E, Pascual J (2014) CGRP and VIP levels as predictors of efficacy of Onabotulinumtoxin type A in chronic migraine. Headache 54:987–995
Bumb A, Seifert B, Wetzel S, Agosti R (2013) Patients profiling for Botox® (onabotulinum toxin A) treatment for migraine: a look at white matter lesions in the MRI as a potential marker. Springerplus 2:377
Cady R, Schreiber C (2008) Botulinum toxin type A as migraine preventive treatment in patients previously failing oral prophylactic treatment due to compliance issues. Headache 48:900–913
Edvinsson J, Warfvinge K, Edvinsson L (2015) Modulation of inflammatory mediators in the trigeminal ganglion by botulinum neurotoxin type A: an organ culture study. J Headache Pain 16:555
Cernuda-Morollón E, Ramón C, Martínez-Camblor P, Serrano-Pertierra E, Larrosa D, Pascual J (2015) OnabotulinumtoxinA decreases interictal CGRP plasma levels in patients with chronic migraine. Pain 156:820–824
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
AN received travel grants, honoraria consultancy and participated in Advisory Board from Allergan, ElectroCore, and Medtronic. PM received travel grants, honoraria consultancy and participated in Advisory Board from Allergan, Medtronic, and Mylan. MC, LL: none. Publication fees for this manuscript will be supported by Allergan.
Authors’ contributions
AN and PM designed the protocol. AN and MC performed the injections. AN, MC and LL reviewed statistic content. AN drafted the manuscript. AN and PM reviewed critically the final draft. All authors read and approved the final manuscript.
Additional file
Additional file 1:
Supplementary Tables. (DOCX 69 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Negro, A., Curto, M., Lionetto, L. et al. A two years open-label prospective study of OnabotulinumtoxinA 195 U in medication overuse headache: a real-world experience. J Headache Pain 17, 1 (2015). https://doi.org/10.1186/s10194-016-0591-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-016-0591-3