Abstract
Regeneration and restoration of the airway epithelium after mechanical, viral or bacterial injury have a determinant role in the evolution of numerous respiratory diseases such as chronic bronchitis, asthma and cystic fibrosis. The study in vivo of epithelial regeneration in animal models has shown that airway epithelial cells are able to dedifferentiate, spread, migrate over the denuded basement membrane and progressively redifferentiate to restore a functional respiratory epithelium after several weeks. Recently, human tracheal xenografts have been developed in immunodeficient severe combined immunodeficiency (SCID) and nude mice. In this review we recall that human airway cells implanted in such conditioned host grafts can regenerate a well-differentiated and functional human epithelium; we stress the interest in these humanized mice in assaying candidate progenitor and stem cells of the human airway mucosa.
Similar content being viewed by others
Introduction
The pseudostratified surface epithelium lining human conducting airways is composed of differentiated cell phenotypes including basal, secretory and ciliated cells. These airway epithelial cells act together to ensure airway mucosa defence through different mechanisms such as mucociliary clearance, active secretion of ions and the regulation of water balance, and the release of antibacterial, antioxidant and anti-inflammatory molecules in the airway surface liquid. The airway surface epithelium also possesses a variety of intercellular junctional complexes that create an efficient barrier against inhaled pathogens and other noxious agents.
However, because of permanent contact with the outer environment, the airway epithelium is frequently injured. Bacterial and viral infections, the inhalation of pollutants and toxic agents or mechanical stress can more or less severely alter the integrity of the epithelial barrier [1]. The response of the airway surface epithelium to an acute injury includes a succession of cellular events varying from loss of surface epithelial impermeability to partial shedding of the epithelium or even to complete denudation of the basement membrane. In response to chronic injury, the airway epithelium can also transdifferentiate, with a shift from serous to mucous cells, from ciliated to secretory cells or from secretory to squamous cells. Such a remodelling illustrates the marked plasticity and capacity of the airway epithelium to regenerate [2].
These transient or permanent alterations in the structure and functions of the airway epithelium after injury have a determinant role in the pathogenesis of numerous respiratory diseases such as chronic bronchitis, asthma and cystic fibrosis (CF).
Animal models of airway epithelium regeneration
A variety of animal models including dogs, rabbits, guinea pigs, hamsters, rats and mice, and different sources of injury (oxidants, cigarette smoke, mechanical injury, and viral or bacterial infections) have been developed. These models of airway epithelium injury and repair in vivo point to several common sequential processes of repair and epithelial regeneration, including the following: (1) spreading and migration of the basal cells neighbouring the wound, (2) rapid restoration of tight junctions, (3) pre-mitosis dedifferentiation followed by squamous metaplasia, (4) active mitosis leading to basal and mucous cell hyperplasia, followed by (5) progressive redifferentiation with the emergence of 'pre-ciliated' cells (a mixed phenotype of ciliated and mucous cells) and ciliogenesis, allowing the regeneration of a functional mucociliary epithelium [3].
Regeneration of the hamster tracheal epithelium after mechanical injury has demonstrated rapid re-epithelialization of the denuded epithelium and has shown that cell migration, rather than cell proliferation, occurs first [4]. Epithelial cells at the border of the wounded area are able to dedifferentiate, spread and migrate over the denuded basement membrane to cover the deepithelialized area. Ramphal et al [5] have shown that, after infection with influenza virus, complete desquamation of the epithelium occurs within 3 days, whereas regeneration begins within 5 days and is completed in 2 weeks.
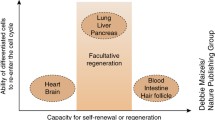
Of the three main airway epithelial cell types, basal and secretory cells are known to divide, whereas ciliated cells are considered to be terminally differentiated. Several investigations support the role of basal cells as progenitors [6,7,8,9]; others suggest that only secretory cells can regenerate a complete mucociliary epithelium [10].
Animal tracheal xenograft models have also been developed to analyse airway epithelium regeneration and to try to identify progenitor cell subpopulations involved in this process. Inducing a regeneration process in airway epithelial tissue, which is normally characterized by a low turnover, accelerates proliferation and differentiation.
Rat tracheas were denuded of their surface epithelium by repeated cycles of freezing and thawing, then seeded with adult rat tracheal epithelial cells and implanted subacutanenously into immunodeficient nude mice [11]. Within a few days, the inoculated cells re-established an epithelial lining that was at first 'poorly differentiated' but then developed the features typical of the epithelium from which the cells originated. These poorly differentiated cells, which expressed markers of basal cells but not secretory or ciliated cells, seem to have a pivotal role in the regeneration-differentiation process. Secretory cells sorted by flow cytometry from the rat trachea seem to have a greater colony-forming efficiency than basal cells, and hence could be stem cells [12]. Conversely, in other studies, basal cells elutriated from rabbit trachea acted as basal cells and gave rise to secretory and ciliated cell types in the host trachea [7].
Submucosal gland cells might also be important in the renewal of the airway epithelium. The group of S Randell and J Dorin [13] found a distinct population of cells expressing high levels of keratin gene and protein in the ciliated ducts of the murine trachea. Because injury is needed to recruit stem cells into division, they damaged the tracheal epithelium and analysed stem cell divisions by injecting bromodeoxyuridine during injury and repair. At 3 and 6 days after injury, bromodeoxyuridine-positive epithelial cells were present along the entire tracheal length in all cells (whether luminal, intermediate or basal cells). By 3 months after injury, the surface epithelium adjacent to gland openings contained bromodeoxyuridine-positive basal cells, suggesting the presence of a stem cell niche in the ciliated ducts. After the removal of surface epithelium, cells migrated from glands to repopulate the tracheal epithelial surface. These results are in agreement with those of Engelhardt's group, which has shown in the newborn ferret that the expression of Lef1 marks early submucosal gland progenitor cells [14].
All these studies in vivo suggest that several categories of stem cell and progenitor cell, including columnar, basal and ciliated duct cells, can participate in airway epithelium regeneration and renewal. Nevertheless, histological differences exist between human airways and those of other animal species, raising doubts as to the relevance of the latter as models. Mouse tracheal epithelium is composed mainly of ciliated and Clara cells, the latter being present only in human distal airways, and only a few submucosal gland cells are identified at the upper tracheal level in mice.
Human airway xenograft models of maturation and regeneration
A first approach to identify and trace progenitors of human airway epithelium was adapted by Engelhardt et al [15] and Zepeda et al [16] from the animal model in vivo described previously by Shimizu et al [11]. They introduced dissociated human airway epithelial cells into a recipient rat trachea depleted of its own epithelium, which was then grafted into a partly xenotolerant nude mouse. Submucosal gland progenitor cells were identified within the airway surface epithelium; clonal analysis revealed that more than one airway progenitor cell is involved in the initial stage of gland development, and that several stem cell subsets can be responsible for airway epithelial regeneration [17].
Human fetal airway xenografts in SCID mice
We have described another model of human airway development in vivo relying on the transplantation of embryonic and fetal lung rudiments into xenotolerant SCID mice [18]. Proximal or distal airway primordia grew rapidly in SCID mice and differentiated fully after 6–12 weeks into tracheal or pulmonary structures, including a pseudostratified ciliated and secretory surface epithelium, submucosal glands and cartilage rings as well as alveolar structures and interstitium. Irrespective of initial stages of development, fragments of human fetal tracheas implanted subcutaneously into SCID mice developed as closed fluid-filled xenografts, lined on their whole inner surface with a pseudostratified and secretory epithelium. The presence of airway fluid inside the lumen of these tracheal grafts resulted from surface cell and submucosal gland secretion and from transepithelial active transport of ions and water. The bioelectric properties of these human tracheal grafts implanted in SCID mice were stable over several months and showed that the mature and well-differentiated lining epithelium acted as a selective barrier to ion transport [19]. Xenografts were similar to post-natal normal airways with respect to transepithelial potential difference, short-circuit current and transepithelial resistance as well as to responses to amiloride, forskolin and extracellular ATP. A lower baseline electrogenic ion transport activity, similar to that described in CF postnatal airways, was observed in CF fetal grafts [19].
This surrogate model of uninfected human airways might be relevant to a characterization of the early phase of inflammation in CF airways [20]. Before any infection, we observed an inflammatory imbalance, characterized by a higher intraluminal content of interleukin-8 and significant accumulation of leucocytes in the subepithelial region of the CF airways grafts. No histological abnormality was observed until these CF tissue grafts were challenged with Pseudomonas aeruginosa. After intraluminal infection, rapid and massive transepithelial migration of leucocytes occurred in CF airway grafts, associated with epithelial exfoliation facilitating the access of bacteria to adherence sites on exposed basal cells and basal lamina. One limitation of this model remains that the xenograft is not exposed to air and probably mimics the prenatal rather than the postnatal human airway environment.
Humanized SCID (SCID-hu) mice as an assay for airway epithelium progenitor cells
In one of the latest developments of the model [21], human airway grafts in SCID mice were repopulated with allogeneic epithelial cells. First, we seeded host grafts, from which native epithelium had been eliminated by several rounds of freezing and thawing, with total epithelial cells dissociated enzymically from developed airways. The recovery of a fully differentiated mucociliary epithelium ensued in all cases, whereas autonomous regeneration did not occur in control unseeded grafts. We confirmed the donor origin of newly formed epithelia in sex-mismatched combinations of host and donor tissues.
In the same experimental setting we then used as a donor tissue the endodermal pouch dissociated from the 5–7-week embryonic lung rudiment, which is a homogenous population of respiratory epithelium stem cells. Such early Anlagen also replenished the denuded host grafts with the full spectrum of surface epithelial cells and glands [21]. These experimental results demonstrate that candidate airway epithelial stem cells can be assayed functionally in SCID-hu mice. The search for molecular markers discriminating such progenitors is being actively pursued.
Human adult airway epithelial regeneration in a humanized nude mouse model
We recently explored [22] regeneration and maturation in the adult human airway epithelium, adapting the tracheal xenografts in nude mice initially developed by Engelhardt et al [15]. Epithelial cells dissociated from human nasal polyps were seeded into the lumen of rat tracheas denuded of their own epithelium by successive cycles of freezing and thawing. The rat tracheas, tied at their distal end to sterile polyethylene tubings, were inoculated with the human adult epithelial cells and implanted subcutaneously in the flanks of recipient nude mice. We analysed, in terms of cell proliferation and the differentiation and integrity of the epithelial barrier, the sequence of events involved in the regeneration of the human airway epithelium, which were partly similar to those described in epithelium regeneration after airway injury. At 3 days after implantation in nude mice, tracheas were partly repopulated with a flattened non-ciliated and poorly differentiated untight epithelium. By the end of the first week, cell proliferation produced on the entire surface of the host rat trachea a squamous-type epithelium that was stratified into multiple layers and tightly sealed.
This squamous epithelium phenotype, which represents a highly protective phenotype previously described after injury, does in fact reflect a protective dynamic regenerative process. During the following weeks, cell proliferation decreased markedly and the epithelium became progressively columnar, secretory and ciliated but was still partly untight, although it was already polarized. We also confirmed that in normal airway epithelium, expression of the CF transmembrane conductance regulator protein (CFTR) was related to epithelium differentiation and was detected at the apical domain of ciliated cells only when the epithelium was fully differentiated. Glandular submucosal structures were visible in xenografts 4 weeks old.
This chimaeric model has the main advantage of reconstituting a human adult airway epithelium exposed to the air environment in the same way as in adult human airways. We are currently analysing the cellular and molecular mechanisms involved in interactions between epithelial cells and bacteria during airway epithelial regeneration. This humanized nude (nu-hu) airway graft is a novel model for studying the inflammatory response of airway epithelium to bacterial virulence factors, oxidants or allergens, and might therefore be very useful in assaying anti-inflammatory molecules in vivo. Another important future pharmacological application of this air-opened humanized airway graft will be in assaying molecules able to activate epithelium regeneration in respiratory diseases such as chronic bronchitis, asthma and CF. Ultimately, this xenochimaera might be of benefit in the analysis of recombinant viral vectors to target progenitor cells for surface epithelium.
References
Puchelle E, Zahm JM, Tournier JM, de Bentzmann S: Airway epithelial injury and repair. Eur Respir Res 1997, 43:136–141.
Basbaum C, Jany B: Plasticity of the airway epithelium. Am J Physiol 1990, 259:L38-L46.
Puchelle E, Zahm JM: Repair processes of the airway epithelium. In Environmental Impact on the Airways. From Injury to Repair. Edited by Chretien J, Dusser D. New York: Dekker; 1996, 157–182.
Keena KP, Combs JW, McDowell EM: Regeneration of hamster tracheal epithelium after mechanical injury. Virchows Arch B Cell Pathol 1982, 41:193–214.
Ramphal R, Small PM, Shands JW, Fischlschweiger W, Small PA: Adherence of Pseudomonas aeruginosa to tracheal cells injured by influenza infection or by endotracheal incubation. Infect Immun 1990, 27:614–619.
Inayama Y, Hook GER, Brody AR, Cameron G, Jetten A, Gilmore L, Gray T, Nettesheim P: The differentiation potential of tracheal basal cells. Lab Invest 1988, 58:706–717.
Inayama Y, Hook GER, Brody AR, Jetten A, Gilmore L, Gray T, Mahler J, Nettesheim P: In vitro and in vivo growth and differentiation of clones of tracheal basal cells. Am J Pathol 1989, 134:539–549.
Ford J, Terzaghi-Howe M: Basal cells are the progenitors of primary tracheal epithelial cell cultures. Exp Cell Res 1992, 198:69–77.
Hicks W, Winston J, Lwebuga-Mukasa J: Isolation and characterization of basal cells form human upper respiratory epithelium. Exp Cell Res 1997, 237:357–363.
Johnson NF, Hubbs AF: Epithelial progenitor cells in the rat trachea. Am J Respir Cell Mol Biol 1990, 3:579–585.
Shimizu T, Nettesheim P, Ramaekers FC, Randell SH: Expression of 'cell-type-specific markers' during rat tracheal epithelial regeneration. Am J Respir Cell Mol Biol 1992, 7:30–41.
Liu JY, Nettesheim P, Randell SH: Growth and differentiation of tracheal epithelial progenitor cells. Am J Physiol 1994, 266:L296-L307.
Borthwick DW, Krantz T, Dorin JP, Randell SH: A potential stem cell niche in the ciliated ducts of murine submucosal glands. Pediatr Pulmonol 1998, Suppl 17:283.
Duan D, Sehgal A, Yao J, Engelhardt JF: Lef1 transcription factor expression defines airway progenitor cell targets for in utero gene therapy of submucosal gland in cystic fibrosis. Am J Respir Cell Mol Biol 1998, 18:750–758.
Engelhardt JF, Yankaskas JR, Wilson JM: In vivo retroviral gene transfer into human bronchial epithelia of xenografts. J Clin Invest 1992, 90:2598–2607.
Zepeda ML, Chinoy MR, Wilson JM: Characterization of stem cells in human airway capable of reconstituting a fully differentiated bronchial epithelium. Somatic Cell Mol Genet 1995, 21:61–73.
Engelhardt JF, Schlossberg H, Yankaskas JR, Dudus L: Progenitor cells of the adult human airway involved in submucosal gland development. Development 1995, 121:2031–2046.
Peault B, Tirouvanziam R, Sombardier MN, Chen S, Perricaudet M, Gaillard D: Gene transfer to human fetal pulmonary tissue developed in immunodeficient SCID mice. Hum Gene Ther 1994, 5:1131–1137.
Tirouvanziam R, Desternes A, Saari A, Puchelle E, Peault B, Chinet T: Bioelectric properties of human cystic fibrosis and non cystic fibrosis fetal tracheal xenografts in SCID mice. Am J Physiol 1998, 274:C875-C882.
Tirouvanziam R, de Bentzmann S, Hubeau C, Hinnrasky J, Jacquot J, Peault B, Puchelle E: Inflammation and infection in naive human cystic fibrosis airway grafts. Am J Respir Cell Mol Biol 2000, 23:121–127.
Delplanque A, Coraux C, Tirouvanziam R, Khazaal I, Puchelle E, Ambros P, Gaillard D, Peault B: Epithelial stem cell-mediated development of the human respiratory mucosa in SCID mice. J Cell Sci 2000, 113:767–778.
Dupuit F, Gaillard D, Hinnrasky J, Mongodin E, de Bentzmann S, Copreni E, Puchelle E: Differentiated and functional human airway epithelium regeneration in tracheal xenografts. Am J Physiol Lung Cell Mol Physiol 2000, 278:L165-L76.
Acknowledgements
The work of the authors referred to in this article was funded in part by INSERM (Institut National de la Santé et de la Recherche Médicale), AFLM (Association Française de Lutte contre la Mucoviscidose) and AFM (Association Française contre les Myopathies).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Puchelle, E., Peault, B. Human airway xenograft models of epithelial cell regeneration. Respir Res 1, 1 (2000). https://doi.org/10.1186/rr21
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/rr21