Abstract
Introduction
The inducible nitric oxide synthase (iNOS) plays a crucial role in early sepsis-related microcirculatory dysfunction. Compared to a catecholamine therapy we tested effects of a specific iNOS-inhibitor (1400W) on the microcirculatory function in the brain.
Methods
Seventy SD-rats (280-310 g) were divided into 1 control and 6 sepsis groups. Sepsis groups received 1 or 5 mg/kg lipopolysaccharide (LPS) intravenously to induce a moderate or severe sepsis syndrome. Thirty minutes later rats were further randomized into subgroups receiving moderate volume therapy alone or additionally continuous norepinephrine (NE) or 1400W infusion. Separately, effects of 1400W on neurofunctional parameters were investigated in 3 rats without sepsis induction. Performing electric forepaw-stimulation evoked potentials (N2-P1 amplitude, P1-latency) and local hemodynamic responses were recorded with surface electrodes and laser Doppler over the somatosensory cortex at baseline and repeatedly after LPS administration. Cytokine levels (tumor necrosis factor-alpha (TNFα), interleukin-6 (IL6), interferon-gamma (IFNγ)) and cell destruction markers (neuron-specific enolase (NSE), S-100 calcium binding protein B (S100B)) were obtained at the end of experiments.
Results
During sepsis progression resting cerebral blood flow increased and functionally activated hemodynamic responses decreased in a dose-dependent manner. Whereas 1400W and NE improved blood pressure, only 1400W stabilized resting flow levels. However, both regimens were ineffective on the functionally coupled flow responses and destruction markers were similar between groups.
Conclusions
NE and 1400W appeared to be ineffective in mitigating the effects of sepsis on the neurovascular coupling. Other regimens are needed to protect the cerebral microcirculation under septic conditions.
Similar content being viewed by others
Introduction
Sepsis and systemic inflammatory response syndromes are the leading causes of mortality in intensive care units [1, 2]. Overt nitric oxide (NO) production by the inducible form of NO-synthases (iNOS) is assumed to play an important role in early sepsis-related vasoregulative failure [3, 4]. In response to inflammatory stimuli NO levels increase rapidly within minutes to hours [3, 4] leading to hypotension [5–7] and refractoriness to vasopressor catecholamines [8]. Animals treated with selective iNOS-inhibitors or transgenic mice deficient in iNOS showed less hypotension and increased microvascular reactivity under septic conditions [9–11].
Regarding the cerebral circulation NO is intimately involved in the adequate blood flow distribution under physiologic conditions [12–14]. The excessive 100- to 1000-fold increase in NO levels overrides the physiologic signals leading to a dissociation of the cerebral circulation. Although the overall perfusion is increased (cerebral hyperemia) [7, 15, 16] it comes to a dysregulation on the microcirculative level [16, 17]. As the brain is very dependent on an appropriate blood supply the microcirculatory failure was in part suggested to best explain the early occurrence of sepsis-associated delirium [17, 18].
Whereas catecholamines can restore the macrocirculation there is growing evidence that they do not prevent the occurrence of microcirculatory dysfunction [19] Therefore, inhibition of the iNOS might be an interesting therapeutic regimen in sepsis syndromes. In this study, we compared protective effects of a specific iNOS-inhibitor N-(3-(aminomethyl)benzyl)acetamidine (1400W) with those of norepinephrine (NE) on the cerebral microcirculation as evaluated by the neurovascular coupling mechanism. To make comparison between a moderate or severe sepsis syndrome 1 mg/kg or 5 mg/kg lipopolysaccharide doses were given.
Materials and methods
General preparation
All procedures performed on the animals were in strict accordance with the National Institutes of Health Guide for Care and Use of Laboratory Animals and approved by the local Animal Care and Use Committee.
Adult male SD-rats (weighing 280 to 310 g) were initially anesthetized with 1.5 to 3% isoflurane in a 7:3 nitrous oxide (N2O)/oxygen mixture of gases, tracheotomized, paralyzed with pancuronium bromide (0.2 mg/kg/h), and artificially ventilated (Harvard Rodent Ventilator; Harvard, South Natick, MA, USA). Arterial blood gas analyses and pH were measured repeatedly as needed and at least every 30 minutes (Blood gas analyzer model Rapidlab 348, Bayer Vital GmbH, Fernwald, Germany). Also, glucose and lactate levels were measured repeatedly (Glukometer Elite XL, Bayer Vital GmbH, Fernwald, Germany; Lactate pro, Arkray Inc. European Office, Düsseldorf, Germany). Glucose was kept in the physiologic range by injections of 0.5 ml 20% glucose as needed. The right femoral artery and vein were cannulated for blood pressure recording, blood sampling, and drug administration. Rectal body temperature was maintained at 37°C using a feedback-controlled heating pad.
The head of the animals was fixed in a stereotaxic frame, the apex of the skull was exposed, and the bone over the left parietal cortex was thinned with a saline-cooled drill to allow transcranial laser-Doppler flowmetry (LDF) [20]. The laser probe (BRL-100, Harvard Apparatus, Holliston, MA, USA) was placed 3.5 mm lateral and 1 mm rostral to the bregma in accordance with the coordinates of the somatosensory cortex; this location corresponds closely to the region of maximal hemodynamic response during contralateral forepaw stimulation [21–23]. The laser-Doppler signal and the systemic mean arterial blood pressure were recorded continuously and processed on a personal computer running a data acquisition software (Neurodyn, HSE, March-Hugstetten, Germany). As the laser Doppler measures flow changes rather than absolute values, resting LDF signals are given in arbitrary units. However, evoked signal changes can be used to assess flow changes and are given in percent-changes from baseline [21, 22].
Somatosensory stimulation was carried out with electrical pulses applied by small needle electrodes inserted under the skin of the right forepaw (PSM Module 676, HSE, March-Hugstetten, Germany). Electric brain activity was recorded monopolarily with an active calomel electrode at 0.5 mm behind the laser probe and an indifferent calomel electrode placed on the nasal bone. Signals were recorded and amplified (BPA Module 675, HSE, March-Hugstetten, Germany) and somatosensory evoked potentials (SEP) were averaged using the Neurodyn acquisition software (HSE, March-Hugstetten, Germany). Evoked potential amplitudes were calculated from the N2-P1-amplitude differences and the latency between the start of stimulation and occurrence of the P1-peak was obtained.
Approximately 60 minutes before the stimulation experiments, isoflurane/N2O anesthesia was discontinued and replaced by intravenous application of α-chloralose (80 mg/kg; Sigma-Aldrich Chemie GmbH, Taufkirchen, Germany). Supplementary doses of chloralose (30 mg/kg) were given every hour. During chloralose anesthesia, the animals were ventilated with a nitrogen/oxygen mixture of 1/1.
Neurovascular coupling measurement
Somatosensory activation was carried out by electrical stimulation of the right forepaw with rectangular pulses of 0.3 ms width and a repetition frequency of 2 Hz for 30 seconds. The stimulation current was kept constant at 1.5 mA so that systemic blood pressure changes did not occur [21–23]. Allowing a rest of 30 seconds after each stimulation train, activation-rest cycles were repeated 10 times to increase signal to noise ratio. Flow velocity responses were averaged and relative responses were calculated in relation to the resting phase, setting the resting phase to zero. The evoked flow velocity responses were calculated from the averaged relative flow velocity signals under conditions of stimulation.
Clinical chemistry
At the end of the experiments blood samples were drawn into tubes containing aprotinin (Trasylol, Bayer AG, Leverkusen, Germany), immediately centrifugated and separated, after which plasma was stored at -80°C until analyses. The neuron-specific enolase (NSE) levels were determined using an ELISA (NSE EIA kit; Hoffmann-La Roche, Basel, Switzerland). The S-100B protein was determined with an immunoluminometric assay (Sangtec 100 LIA; Sangtec Medical, Bromma, Sweden) using monoclonal antibodies specific for the beta subunit of the S-100 protein. Cytokine analysis were performed for IL-6, TNFα, interferon (IFN) γ using commercialized rat ELISA sets (BD Bioscience, Heidelberg, Germany).
Study design
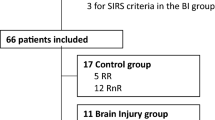
Each 10 rats were subjected to one of the following groups: control, 1 mg/kg LPS (LPS Escherichia coli, O111:B4, Sigma-Aldrich Chemie GmbH, Germany), 5 mg/kg LPS, 1 mg/kg LPS + 1400W, 1 mg/kg LPS + NE, 5 mg/kg LPS + 1400W, 5 mg/kg LPS + NE. LPS was dissolved in 0.5 ml 0.9% sodium chloride (NaCl). LPS was given within two to three minutes. The control group received 0.5 ml vehicle. A moderate volume therapy of 1 to 6 ml/kg/h 0.9% NaCl was allowed in all groups. Thirty minutes after sepsis induction 1400W was given as a bolus of 7.5 mg/kg followed by a continuous infusion at a rate of 7.5 mg/kg/h. NE was given in doses between 0.01 and 10 μg/kg/min to stabilize mean blood pressure in the lower physiologic range between 90 and 100 mmHg.
Prior to and then after LPS administration SEPs, evoked and resting cerebral blood flow velocity levels and blood pressure were measured up to 270 minutes.
In an additional group (n = 3), we investigated the effects of the same dose of 1400W without sepsis induction in healthy rats.
Statistics
If appropriate, a two-way analysis of variance was performed to assess differences within and between groups. In case of significance a Fischer post-hoc test was applied. If assumptions of normal distribution and equality of variances could not be assured, a nonparametric Friedman test was undertaken instead (Statview, SAS, Cary, NA, USA). The significance level was set to P < 0.05.
Results
No rat died from LPS injection. Table 1 shows the group averaged data for partial pressure of carbon dioxide, pH, glucose, lactate, and hemoglobin content. Partial pressure of oxygen levels remained in the range of 240 to 250 mmHg in all groups throughout experiments and therefore were not specified in the table. Table 2 indicates the group data for blood pressure together with the resting LDF signal, N2-P1 potential amplitude, P1 latency, and evoked flow velocity response. The cytokines as well as the cell destruction markers are given in Table 3.
In non-septic rats, 1400W did not result in changes in the following data: blood pressure (121 ± 11 vs.125 ± 6 mmHg; not significant), glucose levels (60 ± 9 vs.57 ± 6 mmol/L; not significant), resting cerebral blood flow (135 ± 25 vs. 142 ± 28; not significant), evoked flow responses (20 ± 7 vs. 20 ± 8%; not significant), SEP amplitudes (16 ± 6 vs.15 ± 4 μV; not significant), or P1-latencies (10 ± 2 vs.10 ± 1 ms; not significant).
General findings
With LPS-administration, rats developed signs of a severe sepsis syndrome characterized by a considerable drop in blood pressure (1 mg/kg LPS: 63 ± 10 mmHg; 5 mg/kg LPS: 56 ± 11 mmHg), occurrence of metabolic acidosis (1 mg/kg LPS: 7.48 ± 0.04; 5 mg/kg LPS: 7.46 ± 0.04), and an increase in the lactate levels (1 mg/kg LPS: 2.5 ± 0.8; 5 mg/kg LPS: 2.4 ± 0.7 mmol/l) as indicated in Table 1. Cytokine levels increased in all sepsis groups without differences between groups (Table 3). Resting flow levels were significantly induced in both LPS + NE groups by approximately 50%, whereas 1400W remained neutral (Table 2). Compared with non-treated groups NE improved blood pressure levels effectively in both groups (95 ± 17 mmHg and 92 ± 15 mmHg; both P < 0001 to non-treated groups). Not as effective as NE 1400W also stabilized blood pressure levels in both groups (82 ± 12 and 76 ± 12 mmHg; both P < 0.001 vs. non-treated animals).
Noteworthy is that only in the 1400W groups glucose substitutions were necessary to maintain adequate blood glucose levels. NE led to even higher glucose levels as compared with the 1 mg/kg or 5 mg/kg LPS groups.
Neurofunctional findings
Addressing neurofunctional parameters NE was shown to be most effective on N2-P1 amplitudes. Compared with the 1 mg/kg LPS group, evoked potential amplitudes were significantly higher throughout experiments (270 minutes: 16 ± 3 μV vs. 12 ± 4 μV; P < 0.05; Figure 1). In the 5 mg/kg group, NE prevented a progressive decline of amplitudes at the end of experiments (270 minutes: 14 ± 3 μV vs. 7 ± 2 μV; P < 0.001; Figure 2). No protective effects were seen on the P1-latencies or evoked flow velocity responses (Table 2).
Time course of group averaged N2-P1 amplitudes given as mean ± standard deviation for the 1 mg/kg lipopolysaccharide groups. Norepinephrine (NE) was protective on the potential amplitudes whereas selective inducible nitric oxide synthase (iNOS)-inhibition (N-(3-(aminomethyl)benzyl)acetamidine (1400W)) showed adverse effects. Statistical results are given as compared to the non-treated group; * P < 0.05. SEP = somatosensory evoked potentials.
Time course of group averaged N2-P1 amplitudes given as mean ± standard deviation for the 5 mg/kg lipopolysaccharide groups. Norepinephrine (NE) was protective on the potential amplitudes at the end of experiments whereas selective inducible nitric oxide synthase (iNOS)-inhibition (N-(3-(aminomethyl)benzyl)acetamidine (1400W)) showed again adverse effects from beginning of therapy. Sttistical results are given as compared with the non-treated group; * P < 0.05; *** P < 0.001.
1400W led to an early and progressive decline in evoked potential amplitudes, which exceeded changes seen in the 1 mg/kg or 5 mg/kg LPS groups (Figures 1 and 2). Similarly, P1-latencies increased to a higher extent as expected from non-treated LPS groups (Table 2). Evoked flow velocity responses dropped in relation to the decrease in evoked potential amplitudes indicating still intact coupling. This makes the possibility of an artifact in electrical recordings unlikely.
Discussion
The functionally coupled blood flow responses are decreased during early phases of sepsis, which could contribute to brain dysfunction (sepsis-associated delirium, septic encephalopathy) in sepsis. Neither 1400W nor NE improved the neurovascular coupling. However, interpretation of the effects of the iNOS-inhibition on the neurovascular coupling is hampered by the direct adverse effects of 1400W on SEP, which were only seen under septic conditions. In both LPS groups, potential amplitudes declined and latencies increased directly after administration of the iNOS-inhibitor. In non-septic rats neither 1400W nor other unspecific NO-inhibitors showed this effect [24, 25]. A second new finding was the strong glucose lowering effect of 1400W under septic conditions. From the literature a beneficial effect was anticipated because increased NO levels adversely interfere with the mitochondrial function and the intracellular glucose homeostasis [26, 27]. However, occurrence of mitochondrial respiratory chain enzyme dysfunction was shown to occur at later stages beginning six to eight hours after sepsis induction [28, 29]. Due to a tight glucose control in the present study simple hypoglycemia cannot explain our findings.
The effect of NE on evoked potential amplitudes cannot be taken as a clear indication for neuroprotection. An improvement of amplitudes is a direct effect of NE, which has been described even under non-septic conditions [30]. It was explained by a more focused activation of cortical neuronal fields. In line with this interpretation, the oxidative metabolism of the brain did not change in septic patients under NE treatment [31]. The lack of an effect on the cell destruction markers also points against a significant neuroprotective effect. Regarding the cerebral circulation, NE is neutral as long as the blood-brain barrier is intact and exerts vasoconstrictive effects in case of a barrier leakage [32, 33]. Therefore, the induced cerebral blood flow in the NE group could be best explained by the higher blood pressure levels. We also did not find an effect of NE on the neurovascular coupling. This is shown in Figure 3 which illustrates the relation between evoked potential amplitudes (x-axis) and resultant flow velocity changes (y-axis) from the beginning to end of experiments. Arrow 1 shows the typical initial uncoupling with a drop in evoked flow velocity responses but still intact evoked potential amplitudes. This response was not modified by NE as compared with non-treated groups. Arrow 2 shows the succeeding drop in evoked potential amplitudes, which were prevented in the NE group possibly due to a substance effect. The typical pattern of an initial uncoupling and succeeding drop in potentials was more pronounced in the 5 mg/kg groups as compared with the 1 mg/kg groups.
Graph of group averaged evoked potential amplitudes and evoked flow velocity responses to illustrate the temporal aspects of neurovascular dysfunction. With lipopolysaccharide (LPS) application it comes first to a disproportional high decline in evoked laser-Doppler responses in both LPS dose groups (arrow 1) before somatosensory evoked potential amplitudes declined (arrow 2). This constellation indicates early microcirculatory failure in the septic brain. Whereas norepinephrine (NE) did not modify the drop in hemodynamic responses (arrow 1) it was protective on the evoked potential amplitudes (absent (1 mg/kg) or diminished (5 mg/kg) component of arrow 2). LDF = laser-Doppler flowmetry; SEP = somatosensory evoked potentials.
Chloralose is a narcotic agent which allows neurophysiologic monitoring [34]. It results in a mild alkalosis which explains the higher initial pH levels.
We chose a classic catecholamine therapy, although immunomodulatory effects of some catecholamines were reported in the literature [35, 36]. We did not find a significant effect of NE on the cytokine level and also did not find significant effects on the gene expression levels of chemokines [37]. Our data are therefore in line with others who found epinephrine but not NE to modulate cytokine levels in a porcine model of endotoxic shock [38].
The cell destruction markers NSE and S-100 calcium binding protein B have been widely used to assess the prognosis and outcome of different disease processes [39–41]. A limitation occurs in case of a blood-brain barrier breakdown because serum levels then can considerably vary between individuals. A similar study excluded a blood-brain barrier breakdown for the first hours of a sepsis syndrome [33]. This is reflected by the narrow standard deviation of cell destruction markers.
Conclusions
Neurovascular coupling is decreased during early phases of sepsis. This could contribute to brain dysfunction in sepsis (sepsis-associated delirium). Neither NE nor 1400W considerably prevented the breakdown of the neurovascular coupling. However, further research is needed to clarify the direct adverse effects of 1400W on neuronal function, which occurs only under septic conditions.
Key messages
-
Microcirculatory dysfunction occurs early in the septic brain.
-
Besides its effects on blood pressure, norepinephrine does not prevent the occurrence of sepsis-related cerebral microcirculatory failure and the effect on evoked potential amplitudes seems to be a side effect of the agent.
-
Under septic conditions, 1400W stabilizes the blood pressure but shows a direct adverse effect on evoked potential amplitudes which does not appear under physiologic conditions. Due to this effect, interpretation of its effects on the neurovascular coupling is limited; however, a clear beneficial effect was lacking.
Abbreviations
- 1400W:
-
N-(3-(aminomethyl)benzyl)acetamidine
- ELISA:
-
enzyme-linked immunosorbent assay
- IFN:
-
interferon
- IL:
-
interleukin
- iNOS:
-
inducible nitric oxide synthase
- LDF:
-
laser-Doppler flowmetry
- LPS:
-
lipopolysaccharide
- NaCl:
-
sodium chloride
- NE:
-
norepinephrine
- NO:
-
nitric oxide
- NSE:
-
neuron specific enolase
- SEP:
-
somatosensory evoked potentials
- TNF:
-
tumor necrosis factor.
References
Hotchkiss RS, Karl IE: The pathophysiology and treatment of sepsis. New Engl J Med 2003, 348: 138-150. 10.1056/NEJMra021333
Parillo JE: Pathogenetic mechanisms of septic shock. New Engl J Med 1993, 328: 1471-1478. 10.1056/NEJM199305203282008
Tureen J: Effect of recombinant human tumor necrosis factor-alpha on cerebral oxygen uptake, cerebrospinal fluid lactate, and cerebral blood flow in the rabbit: role of nitric oxide. J Clin Invest 1995, 95: 1086-1091. 10.1172/JCI117755
Vincent JL: Microvascular endothelial dysfunction: a renewed appreciation of sepsis pathophysiology. Crit Care 2001, 5: S1-S5. 10.1186/cc1332
Rees DD: Role of nitric oxide in the vascular dysfunction of septic shock. Biochem Soc Trans 1995, 23: 1025-1029.
Rosselet A, Feihl F, Markert M, Gnaegi A, Perret C, Liaudet L: Selective iNOS inhibition is superior to norepinephrine in the treatment of rat endotoxic shock. Am J Respir Crit Care Med 1998, 157: 162-170.
Scott JA, Mehta S, Duggan M, Bihari A, McCormack DG: Functional inhibition of constitutive nitric oxide synthase in a rat model of sepsis. Am J Respir Crit Care Med 2002, 165: 1426-1432. 10.1164/rccm.2011144
Gray G, Schott C, Julou-Schaeffer G, Fleming I, Parratt JR, Stoclet JC: The effect of inhibitors of the L-arginine/nitric oxide pathway on endotoxin-induced loss of vascular responsiveness in anaesthetized rats. Br J Pharmacol 1991, 103: 1218-1244.
Hollenberg SM, Broussard M, Osman J, Parrillo JE: Increased microvascular reactivity and improved mortality in septic mice lacking inducible nitric oxide synthase. Circ Res 2000, 86: 774-779.
MacMicking JD, Nathan C, Hom G, Chartrain N, Fletcher DS, Trumbauer M, Stevens K, Xie QW, Sokol K, Hutchinson N, Chen H, Mudget JS: Altered responses to bacterial infection and endotoxic shock in mice lacking inducible nitric oxide synthase. Cell 1995, 81: 641-650. 10.1016/0092-8674(95)90085-3
Wei XQ, Charles IG, Smith A, Ure J, Feng GJ, Huang FP, Xu D, Muller W, Moncada S, Liew FY: Altered immune responses in mice lacking inducible nitric oxide synthase. Nature 1995, 375: 408-411. 10.1038/375408a0
Andresen J, Shafi NI, Bryan RM: Endothelial influences on cerebrovascular tone. J Appl Physiol 2006, 100: 318-327. 10.1152/japplphysiol.00937.2005
Iadecola C: Neurovascular regulation in the normal brain and in Alzheimer's disease. Nat Rev Neurosci 2004, 5: 347-360. 10.1038/nrn1387
Buerk DG, Ances BM, Greenberg JH, Detre JA: Temporal dynamics of brain tissue nitric oxide during functional forepaw stimulation in rats. Neuroimage 2003, 18: 1-9. 10.1006/nimg.2002.1314
Okamoto H, Ito O, Roman RJ, Hudetz AG: Role of inducible nitric oxide snythase and cyclooxygenase-2 in endotoxin.induced cerebral hyperemia. Stroke 1998, 29: 1209-1218.
Rosengarten B, Hecht M, Auch D, Ghofrani HA, Schermuly RT, Grimminger F, Kaps M: Microcirculatory dysfunction in the brain precedes changes in evoked potentials in endotoxin-induced sepsis syndrome in rats. Cerebrovasc Dis 2007, 23: 140-147. 10.1159/000097051
Ebersoldt M, Sharshar T, Annane D: Sepsis-associated delirium. Intensive Care Med 2007, 33: 941-950. 10.1007/s00134-007-0622-2
Green R, Scott LK, Minagar A, Conrad S: Sepsis associated encephalopathy (SAE): a review. Front Biosci 2004, 9: 1637-1641. 10.2741/1250
Pullamsetti SS, Maring D, Ghofrani HA, Mayer K, Weissmann N, Rosengarten B, Lehner M, Schudt C, Boer R, Grimminger F, Seeger W, Schermuly RT: Effect of nitric oxide synthase (NOS) inhibition on macro- and microcirculation in a model of rat endotoxic shock. Thromb Haemost 2006, 95: 720-727.
Dirnagl U, Kaplan B, Jacewicz M, Pulsinelli W: Continuous measurement of cerebral cortical blood flow by laser-Doppler flowmetry in a rat stroke model. J Cereb Blood Flow Metab 1989, 9: 589-596.
Ances BM, Detre JA, Takahashi K, Greenberg JH: Transcranial laser Doppler mapping of activation flow coupling of the rat somatosensory cortex. Neurosci Lett 1998, 257: 25-28. 10.1016/S0304-3940(98)00796-4
Lindauer U, Villringer A, Dirnagl U: Characterization of CBF response to somatosensory stimulation: model and influence of anesthetics. Am J Physiol 1993, 264: H1223-H1228.
Rosengarten B, Lutz H, Hossmann KA: A control system approach for evaluating somatosensory activation by laser-Doppler flowmetry in the rat cortex. J Neurosci Methods 2003, 130: 75-81. 10.1016/S0165-0270(03)00209-7
Lindauer U, Megow D, Schultze J, Weber JR, Dirnagl U: Nitric oxide synthase inhibition does not affect somatosensory evoked potentials in the rat. Neurosci Lett 1996, 216: 207-210. 10.1016/0304-3940(96)13044-5
Garvey EP, Oplinger JA, Furfine ES, Kiff RJ, Laszlo F, Whittle BJ, Knowles RG: 1400W is a slow, tight binding, and highly selective inhibitor of inducible Nitric-oxide synthase in vitro and in vivo. J Biol Chem 1997, 272: 4959-4963. 10.1074/jbc.272.8.4959
Jobgen WS, Fried SK, Fu WJ, Meininger CJ, Wu G: Regulatory role for the arginine-nitric oxide pathway in metabolism of energy substrates. J Nutr Biochem 2006, 17: 571-588. 10.1016/j.jnutbio.2005.12.001
Peres-Asensio FJ, Hurtado O, Burguete MC, Moro MA, Salom JB, Lizasoain I, Torregrosa G, Leza JC, Alborch E, Castillo J, Knowles RG, Lorenzo P: Inhibition of iNOS activity by 1400W decreases glutamate release and ameliorates stroke outcome after experimental ischemia. Neurobiol Dis 2005, 18: 375-384. 10.1016/j.nbd.2004.10.018
Comim CM, Rezin GT, Scaini G, Di-Pietro PB, Cardoso MR, Petronilho FC, Ritter C, Streck EL, Quevedo J, Dal-Pizzol F: Mitochondrial respiratory chain and creatine kinase activities in rat brain after sepsis induced by cecal ligation and perforation. Mitochondrion 2008, 8: 313-318. 10.1016/j.mito.2008.07.002
d'Avila JC, Santiago AP, Amancio RT, Galina A, Oliveira MF, Bozza FA: Sepsis induces brain mitochondrial dysfunction. Crit Care Med 2008, 36: 1925-1932. 10.1097/CCM.0b013e3181760c4b
Drouin C, Wang D, Waterhouse BD: Neurophysiological actions of methylphenidate in the primary somatosensory cortex. Synapse 2007, 61: 985-990. 10.1002/syn.20454
Moller K, Qvist T, Tofteng F, Sahl C, Sonderkaer S, Dethloff T, Knudsen GM, Larsen FS: Cerebral blood flow and metabolism during infusion of norepinephrine and propofol in patients with bacterial meningitis. Stroke 2004, 35: 1333-1339. 10.1161/01.STR.0000128418.17312.0e
Corday E, Williams JH Jr: Effect of shock and of vasopressor drugs on the regional circulation of the brain, heart, kidney and liver. Am J Med 1960, 29: 228-241. 10.1016/0002-9343(60)90020-6
Rosengarten B, Walberer M, Allendoerfer J, Mueller C, Schwarz N, Bachmann G, Gerriets T: LPS-induced endotoxic shock does not cause early brain edema formation - A MRI study in rats. Inflamm Res 2008, 57: 479-483. 10.1007/s00011-008-8042-5
Ueki M, Mies G, Hossmann KA: Effect of alpha-chloralose, halothane, pentobarbital and nitrous oxide anesthesia on metabolic coupling in somatosensory cortex of rat. Acta Anaesthesiol Scand 1992, 36: 318-322. 10.1111/j.1399-6576.1992.tb03474.x
Feinstein DL, Heneka MT, Gavrilyuk V, Gavrilyuk V, Dello Russo C, Weinberg G, Galea E: Noradrenergic regulation of inflammatory gene expression in brain. Neurochem Int 2002, 41: 357-365. 10.1016/S0197-0186(02)00049-9
Oberbeck R: Catecholamines: physiological immunomodulators during health and illness. Curr Med Chem 2006, 13: 1979-1989. 10.2174/092986706777584997
Wolff S, Klatt S, Wolff JC, Wilhelm J, Fink L, Kaps M, Rosengarten B: Endotoxin-induced gene expression differences in the brain and effects of iNOS inhibition and norepinephrine. Intensive Care Med 2009, 35: 730-739. 10.1007/s00134-009-1394-7
Bergmann M, Gornikiewicz A, Tamandl D, Exner R, Roth E, Függer R, Götzinger P, Sautner T: Continuous therapeutic epinephrine but not norepinephrine prolongs splanchnic IL-6 production in porcine endotoxic shock. Shock 2003, 20: 575-581. 10.1097/01.shk.0000095934.86703.83
Madl C, Grimm G, Kramer L, Yeganehfar W, Sterz F, Schneider B, Kranz A, Schneeweiss B, Lenz K: Early prediction of individual outcome after cardiopulmonary resuscitation. Lancet 1993, 341: 855-858. 10.1016/0140-6736(93)93061-5
Nguyen DN, Spapen H, Su F, Schiettecatte J, Shi L, Hachimi-Idrissi S, Huyghens L: Elevated serum levels of S-100β protein and neuron-specific enolase are associated with brain injury in patients with severe sepsis and septic shock. Crit Care Med 2006, 34: 1967-1974. 10.1097/01.CCM.0000217218.51381.49
Wunderlich MT, Wallesch CW, Goertler M: Release of neurobiochemical markers of brain damage is related to the neurovascular status on admission and the site of arterial occlusion in acute ischemic stroke. J Neurol Sci 2004, 227: 49-53. 10.1016/j.jns.2004.08.005
Acknowledgements
This project was funded by a Research Grant of the University Medical Centre Giessen and Marburg.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
BR drafted the manuscript, performed the experiments together with SK and SW. SW additionally investigated cytokines and cell destruction markers. RS designed the experiments with BR and helped with writing the paper. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Rosengarten, B., Wolff, S., Klatt, S. et al. Effects of inducible nitric oxide synthase inhibition or norepinephrine on the neurovascular coupling in an endotoxic rat shock model. Crit Care 13, R139 (2009). https://doi.org/10.1186/cc8020
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc8020