Abstract
Introduction
The purpose was to test the hypothesis that muscle perfusion, oxygenation, and microvascular reactivity would improve in patients with severe sepsis or septic shock during treatment with recombinant activated protein C (rh-aPC) (n = 11) and to explore whether these parameters are related to macrohemodynamic indices, metabolic status or Sequential Organ Failure Assessment (SOFA) score. Patients with contraindications to rh-aPC were used as a control group (n = 5).
Materials and methods
Patients were sedated, intubated, mechanically ventilated, and hemodynamically monitored with the PiCCO system. Tissue oxygen saturation (StO2) was measured using near-infrared spectroscopy (NIRS) during the vascular occlusion test (VOT). Baseline StO2 (StO2 baseline), rate of decrease in StO2 during VOT (StO2 downslope), and rate of increase in StO2 during the reperfusion phase were (StO2 upslope) determined. Data were collected before (T0), during (24 hours (T1a), 48 hours (T1b), 72 hours (T1c) and 96 hours (T1d)) and 6 hours after stopping rh-aPC treatment (T2) and at the same times in the controls. At every assessment, hemodynamic and metabolic parameters were registered and the SOFA score calculated.
Results
The mean ± standard deviation Acute Physiology and Chronic Health Evaluation II score was 26.3 ± 6.6 and 28.6 ± 5.3 in rh-aPC and control groups, respectively. There were no significant differences in macrohemodynamic parameters between the groups at all the time points. In the rh-aPC group, base excess was corrected (P < 0.01) from T1a until T2, and blood lactate was significantly decreased at T1d and T2 (2.8 ± 1.3 vs. 1.9 ± 0.7 mmol/l; P < 0.05). In the control group, base excess was significantly corrected at T1a, T1b, T1c, and T2 (P < 0.05). The SOFA score was significantly lower in the rh-aPC group compared with the controls at T2 (7.9 ± 2.2 vs. 12.2 ± 3.2; P < 0.05). There were no differences between groups in StO2 baseline. StO2 downslope in the rh-aPC group decreased significantly at all the time points, and at T1b and T2 (-16.5 ± 11.8 vs. -8.1 ± 2.4%/minute) was significantly steeper than in the control group. StO2 upslope increased and was higher than in the control group at T1c, T1d and T2 (101.1 ± 62.1 vs. 54.5 ± 23.8%/minute) (P < 0.05).
Conclusions
Treatment with rh-aPC may improve muscle oxygenation (StO2 baseline) and reperfusion (StO2 upslope) and, furthermore, rh-aPC treatment may increase tissue metabolism (StO2 downslope). NIRS is a simple, real-time, non-invasive technique that could be used to monitor the effects of rh-aPC therapy at microcirculatory level in septic patients.
Similar content being viewed by others
Introduction
During sepsis, the microcirculatory and mitochondrial dysfunction plays a key role in the development of severe sepsis, septic shock, and multiple organ failure [1]. This condition is characterized by microcirculatory perfusion heterogeneity, arteriovenous shunting, and impaired autoregulation mainly due to disturbed coagulation, inflammation, and leukocyte-endothelium interaction [1–3]. It is now well established in septic patients that restoring basic macrohemodynamic parameters, such as blood pressure, in itself does not lead to improved patient outcome, and that normalization of microcirculatory and mitochondrial function may be necessary as an endpoint [2, 4].
To this end, recombinant activated protein C (rh-aPC) has been used to restore the coagulative cascade, the inflammatory response, leukocyte adhesion and migration, and endothelial function. In previous studies, rh-aPC has been shown to decrease end-organ dysfunction and mortality if administered in the early stages of sepsis [5–7].
Near-infrared spectroscopy (NIRS) is a rapid, continuous, and non-invasive monitoring system of hemoglobin oxygen saturation in muscle and the brain, and has been used to assess the presence and extent of both circulatory and metabolic disorders in intensive care patients and trauma patients [8, 9]. The monitoring system uses near-infrared light (680 to 800 nm) to illuminate tissue, which is mainly absorbed by hemoglobin and myoglobin [10]. Due to the selected wavelength range and the high corresponding spectral absorbance by (de)oxyhemoglobin, the NIRS measurements are confined to vessels with a diameter <500 μm.
Using NIRS, oxyhemoglobin can be distinguished from deoxyhemoglobin because of their differing optical absorption spectra. The ratio of oxyhemoglobin concentration to deoxyhemoglobin concentration is used to calculate a parameter called tissue oxygen saturation (StO2), describing the oxygenation of the microvasculature in a certain volume of (muscular) tissue. In addition to steady-state StO2 values, NIRS can be used in combination with a vascular occlusion test (VOT), which consists of a baseline phase, an ischemia phase, a reperfusion phase, and a reactive hyperemia phase. Using this methodology in many studies of sepsis, it has been demonstrated in a variety of ways that, following a brief period of ischemia, there is an anomalous tissue reperfusion profile due to disturbed microcirculatory functioning [11, 12].
The purpose of the present study was to test the hypothesis that rh-aPC treatment corrects tissue perfusion and microcirculatory reperfusion in septic patients, evaluated with NIRS in combination with a VOT, and to explore whether the NIRS parameters are related to macrohemodynamic indices, metabolic status, and Sequential Organ Failure Assessment (SOFA) score.
Materials and methods
Patients
The study was designed as a prospective observational investigation. For the experimental group (rh-aPC group), we enrolled all patients admitted to the 12-bed polyvalent intensive care unit of the University Hospital of Ospedali Riuniti, Ancona, Italy with a diagnosis of severe sepsis or septic shock - based on the criteria of the International Sepsis Definitions Conference ACCP/SCCM [13] - that could receive rh-aPC treatment (continued infusion of 24 μg/kg/hour for 96 hours). We included patients with two or more sepsis-related organ failures (that is, cardiovascular, pulmonary or renal dysfunction, thrombocytopenia, metabolic acidosis with high lactates) or sepsis-correlated acute respiratory distress syndrome. Patients with absolute or relative contraindications to rh-aPC therapy were enrolled into the control group. At the onset of severe sepsis or septic shock, the Acute Physiology and Chronic Health Evaluation II score was calculated.
All patients were sedated, intubated, and mechanically ventilated. They were hemodynamically monitored by arterial femoral catheter with the PiCCO system (Pulsion, Munich, Germany). All patients received fluid challenge, and, if necessary, continuous infusion of inotropic (dobutamine) and vasopressor (norepinephrine) agents to maintain a normal cardiac index and intrathoracic blood volume index and to maintain the mean arterial pressure between 70 and 100 mmHg.
Near-infrared spectroscopy
StO2 was measured by a tissue spectrometer (InSpectra™ Model 325; Hutchinson Technology Inc., Hutchinson, MN, USA). The spectrometer consists of light detection circuitry and an optical cable that transmits light to tissues and receives scattered light from tissues. The maximum depth of the tissue volume sampled is estimated to be equal to the distance between the sending and receiving fibers of the probe (probe spacing). A probe spacing of 15 mm was used, with the probe placed on an adhesive surface on the skin of the volar surface of the forearm at the level of the brachio-radial muscle. The VOT was applied using a sphygmomanometer cuff around the same arm that was inflated to 60 mmHg above the systolic arterial pressure to obtain an arterial occlusion (stagnant ischemia) until StO2 decreased to 40%. StO2 was monitored continuously before (baseline) and during (ischemia) pneumatic compression and after cuff release (reperfusion).
Data were analyzed using InSpectra™ software to plot and measure the StO2 curve characteristics; that is, baseline StO2 (StO2 baseline), rate of decrease in StO2 during the VOT during the (StO2 downslope), and rate of increase in StO2 reperfusion phase (StO2 upslope). Data were collected before (T0), during (24 hours (T1a), 48 hours (T1b), 72 hours (T1c), and 96 hours (T1d)), and 6 hours (T2) after rh-aPC treatment (that is, 102 hours from T0), and at the same times in the controls. At all time points (except at 96 hours) the following measurements were obtained: mean arterial pressure, dose of norepinephrine, arterial blood lactate and base excess, cardiac index and intrathoracic blood volume index, and SOFA score.
Statistical analysis
Results are expressed as the mean ± standard deviation, and as the median (first to third interquartile range) for catecholamines. Parametric statistics were applied for all parameters-except for catecholamines, for which nonparametric statistics were utilized. A two-way analysis of variance test was used to assess differences between groups; a paired t test was applied to test differences between times within each group, while an unpaired t test with Welch correction when indicated was applied to test differences at each time between groups. The Friedman test was used to test significant differences during time within each group, the Wilcoxon test was used to test differences between each time point and T0, and the Mann-Whitney U test was used to test for differences between groups. P < 0.05 was considered statistically significant.
Results
We studied 11 patients (four female and seven male) with severe sepsis or septic shock who received rh-aPC therapy (continued infusion of 24 μg/kg/hour for 96 hours) and a control group of five patients (two female and three male) who could not receive rh-aPC because of contraindications. The patient characteristics are presented in Table 1. On admission to the intensive care unit, the mean Acute Physiology and Chronic Health Evaluation II score was 26.3 ± 6.6 for the rh-aPC group and 28.6 ± 5.3 for the control group, with a risk of death of 41.0 ± 22.9% and 57.6 ± 25.7%, respectively. The mortality rate was 36.4% in the rh-aPC group and 60% in the control group.
Four patients in the rh-aPC group (Table 1, Patients 2, 4, 9, and 11) and one patient in the control group (Table 1, Patient 4) presented severe sepsis/septic shock on intensive care unit admission, while the other patients developed sepsis after admission to the intensive care unit.
From the two-way analysis of variance test, significant differences between groups were found for StO2 downslope (P < 0.01), StO2 upslope, the SOFA score (P < 0.05) and the mean arterial pressure (P < 0.001).
The Friedman test showed that the norepinephrine and dobutamine rates significantly decreased only in the rh-aPC group (P < 0.01), and not in the control group (Table 2).
The SOFA score, compared with T0, was significantly lower at T1c and T1d (10.1 ± 2.3 vs. 8.8 ± 2.0 and 8.0 ± 2.3; P < 0.05) and at T2 (7.9 ± 2.2; P < 0.01) (Figure 1). At T2 the SOFA score was significantly reduced compared with the control group (7.9 ± 2.2 vs. 12.2 ± 3.2; P < 0.05). In the control group, no differences were found with respect to baseline values.
Sequential Organ Failure Assessment score before, during, and after recombinant activated protein C treatment. The Sequential Organ Failure Assessment (SOFA) score in the recombinant activated protein C (rh-aPC) group before, during, and after rh-aPC treatment, and in the control group at the same times. Data were collected before (T0), during (24 hours (T1a), 48 hours (T1b), 72 hours (T1c), and 96 hours (T1d)), and 6 hours (T2) after rh-aPC treatment (that is, 102 hours from T0). ANOVA, analysis of variance.
There were no significant differences in the macrohemodynamic parameters (cardiac index and intrathoracic blood volume index) at T0, during therapy, and at T2 (Table 2). The mean arterial pressure was no different at T0 between groups, while it was significantly increased during treatment only in the rh-aPC group (T2 93.8 ± 12.8 vs. T0 81 ± 10.9 mmHg) (Figure 2).
Mean arterial pressure before, during, and after recombinant activated protein C treatment. Mean arterial pressure (MAP) in the recombinant activated protein C (rh-aPC) group before, during, and after rh-aPC treatment, and in the control group at the same times. Data were collected before (T0), during (24 hours (T1a), 48 hours (T1b), 72 hours (T1c), and 96 hours (T1d)), and 6 hours (T2) after rh-aPC treatment (that is, 102 hours from T0). ANOVA, analysis of variance.
With regard to metabolic acidosis in the rh-aPC group, base excess was significantly corrected (P < 0.01) after 24 hours from T0 and remained corrected until T2 (Figure 3a). In the control group, base excess was significantly corrected at T1a, T1b, T1c, and T2 (P < 0.05) (Figure 3a). Blood lactate was significantly decreased in the rh-aPC group at T1d and T2 (2.8 ± 1.3 vs. 1.9 ± 0.7 mmol/l; P < 0.05) (Figure 3b).
Base excess and blood lactate before, during, and after recombinant activated protein C treatment. (a) Arterial base excess (BE) and (b) blood lactate in the recombinant activated protein C (rh-aPC) group before, during, and after rh-aPC treatment, and in the control group at the same times. Data were collected before (T0), during (24 hours (T1a), 48 hours (T1b), 72 hours (T1c), and 96 hours (T1d)), and 6 hours (T2) after rh-aPC treatment (that is, 102 hours from T0). ANOVA, analysis of variance; n.s., not significant.
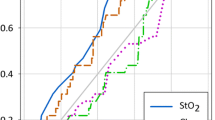
StO2 baseline was significantly higher at T1a, T1c and T2 (Figure 4), while in the control group it was significantly higher at T2. StO2 downslope decreased significantly at all the time points (Figure 5a) only in the rh-aPC group, and it was significantly steeper in the rh-aPC-treated patients than in the control patients at T1b and T2 (-16.5 ± 11.8 vs. -8.1 ± 2.4%/minute). StO2 upslope increased significantly in the rh-aPC group at T1b, T1c, T1d and T2 (Figure 5b), and was significantly higher than in the controls at T1c, T1d and T2 (101.1 ± 62.1 vs. 54.5 ± 23.8%/minute).
Baseline tissue oxygen saturation before, during, and after recombinant activated protein C treatment. Baseline tissue oxygen saturation (StO2 baseline) in the recombinant activated protein C (rh-aPC) group before, during, and after rh-aPC treatment, and in the control group at the same times. Data were collected before (T0), during (24 hours (T1a), 48 hours (T1b), 72 hours (T1c), and 96 hours (T1d)), and 6 hours (T2) after rh-aPC treatment (that is, 102 hours from T0). ANOVA, analysis of variance; n.s., not significant.
Tissue oxygen saturation increase and decrease before, during, and after recombinant activated protein C treatment. (a) Rate of decrease in tissue oxygen saturation (StO2 downslope) and (b) rate of increase in tissue oxygen saturation (StO2 upslope) in the recombinant activated protein C (rh-aPC) group before, during, and after rh-aPC treatment, and in the control group at the same times. Data were collected before (T0), during (24 hours (T1a), 48 hours (T1b), 72 hours (T1c), and 96 hours (T1d)), and 6 hours (T2) after rh-aPC treatment (that is, 102 hours from T0). ANOVA, analysis of variance.
Discussion
The present prospective observational study investigated the effects of rh-aPC treatment on the SOFA score, macrohemo-dynamic parameters, and metabolic acidosis in severe sepsis and septic shock. Additionally, and more importantly in the context of sepsis, the tissue oxygenation, metabolism, and microvascular reperfusion dynamics were assessed using NIRS in combination with a VOT to study any beneficial effects of rh-aPC therapy at the microcirculatory level. It was shown that rh-aPC treatment significantly lowered the SOFA score, increased the mean arterial pressure, and reduced the blood lactate concentration. Furthermore, rh-aPC had positive effects on the VOT-derived StO2 parameters; both and StO2 downslope StO2 upslope increased significantly, indicating raised oxygen consumption/metabolism and indicating improved microvascular reperfusion following ischemia.
Early goal-directed therapy focused on restoring macrohemodynamics has been shown to be insufficient in preventing cellular hypoxia and organ failure due to the heterogeneous nature of sepsis-related microcirculatory dysfunction. It has been shown that improvement in hemodynamic parameters with vasoconstrictors, such as norepinephrine, could make tissue perfusion worse [14], and several studies have demonstrated the positive effects of vasodilators on microcirculatory recruitment even in hemodynamically resuscitated septic patients [15]. rh-aPC treatment has been shown to improve end-organ function and to decrease mortality if started in the early stages of sepsis [5–7] by restoring the coagulative cascade, the inflammatory response, leukocyte adhesion and migration, and endothelial function. In addition to the anticoagulant, profibrinolytic [16], and anti-inflammatory effects and the antioxidant properties [17, 18], rh-aPC acts at the microcirculation level to enhance the proportion of perfused capillaries and improve local autoregulation [1, 19–21]. These studies were mostly carried out in animals. De Backer and co-workers [22] were the first to show the beneficial effects of rh-aPC on microcirculatory perfusion by direct observation of the sublingual microcirculation of septic patients using OPS imaging. To our knowledge, however, the direct effects of rh-aPC treatment on tissue oxygenation have not been studied before.
Many studies have shown the relevance of StO2 in the assessment of the metabolic and microcirculatory state in septic patients. Doerschug and colleagues [23], De Blasi and colleagues [10], Skarda and colleagues [24], and Pareznik and colleagues [25] all showed that tissue oxygen consumption was lower in septic patients than in nonseptic patients or healthy volunteers and that septic patients have slower tissue reoxygenation following ischemia. In addition, Creteur and colleagues [12] demonstrated that persistent alteration of StO2 resaturation correlated with worse outcome and multiorgan failure.
The steady-state tissue oxygenation (StO2 baseline) did not change as a result of rh-aPC treatment, which indicates that the balance between tissue oxygen delivery and consumption is unaltered by rh-aPC infusion. StO2 downslope, in contrast, increased significantly after starting the rh-aPC therapy, indicating increased cellular oxygen consumption. Additionally, StO2 upslope increased significantly due to rh-aPC treatment, which indicates the improved ability of the microcirculation to be reperfused after a brief period of ischemia. Microvascular function is therefore improved by rh-aPC treatment. This finding is also supported by the reduced SOFA score and lactate levels.
The present study has some limitations: firstly, the small number of patients - in particular in the control group, where patients affected by head trauma and intracranial hypertension could have an altered systemic hemodynamic; and secondly, because the NIRS technique itself has some limitations. StO2 downslope has been asserted to indicate the muscle oxygen consumption, but oxygen consumption cannot be directly measured as the amount of hemoglobin in the respective muscle blood volume is not known. The parameter being measured is the oxygen consumption rate extrapolated from the decrease in saturation of hemoglobin (StO2 decrease rate, %/minute), which is an index of the basic metabolism of the thenar muscle. Moreover, whether the concentration of hemoglobin affects the oxygen consumption rate is not known. One argument regarding the reperfusion rate is that NIRS does not measure blood flow and it must be assumed that an increase in StO2 reflects endothelium-dependent vasodilation. The extent to which comorbidites such as atherosclerosis, age, gender or mental stress may influence this parameter is not known. Regardless of these limitations, the ability to provide a non-invasive, reproducible estimate of the oxygen consumption rate of skeletal muscle at the bedside renders this technique potentially useful in clinical practice.
Conclusion
Treatment of septic patients with continuous infusion of rh-aPC may improve tissue oxygenation, cellular metabolism, and microvascular reactivity, and may significantly reduce the SOFA score and lactate levels. NIRS in combination with a VOT was able to detect microcirculatory and metabolic changes associated with sepsis and rh-aPC treatment.
Abbreviations
- NIRS:
-
near-infrared spectroscopy
- rh-aPC:
-
recombinant activated protein C
- SOFA:
-
Sequential Organ Failure Assessment
- StO2:
-
tissue oxygen saturation
- StO2 downslope:
-
rate of decrease in tissue oxygen saturation
- StO2 upslope:
-
rate of increase in tissue oxygen saturation
- VOT:
-
vascular occlusion test.
References
Ince C: The microcirculation is the motor of sepsis. Crit Care 2005,9(Suppl 4):13-19. 10.1186/cc3753
De Backer D, Creteur J, Preiser J, Dubois MJ, Vincent JL: Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care 2002, 166: 98-104. 10.1164/rccm.200109-016OC
Astiz ME, DeGent GE, Lin RY, Rackow EC: Microvascular function and rheologic changes in hyperdynamic sepsis. Crit Care Med 1995, 23: 265-271. 10.1097/00003246-199502000-00011
Trzeciak S, McCoy JV, Dellinger RP, Arnold RC, Rizzuto M, Abate NL, Shapiro NI, Parrillo JE, Hollenberg SM, Microcirculatory Alterations in Resuscitation and Shock (MARS) investigators: Early increases in microcirculatory perfusion during protocol-directed resuscitation are associated with reduced multi-organ failure at 24 h in patients with sepsis. Intensive Care Med 2008, 34: 2210-2217. 10.1007/s00134-008-1193-6
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ Jr, Recombinant Human Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study group: Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 2001, 344: 699-709. 10.1056/NEJM200103083441001
Vincent JL, Bernard GR, Beale R, Doig C, Putensen C, Dhainaut JF, Artigas A, Fumagalli R, Macias W, Wright T, Wong K, Sundin DP, Turlo MA, Janes J: Drotrecogin alfa (activated) treatment in severe sepsis from the global open-label trial ENHANCE: further evidence for survival and safety and implications for early treatment. Crit Care Med 2005, 33: 2266-2277. 10.1097/01.CCM.0000181729.46010.83
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banocloche J, Keh D, Marshall JC, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM: Surviving Sepsis Campaign Management Guidelines Committee: Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 2004, 32: 858-873. 10.1097/01.CCM.0000117317.18092.E4
Boushel R, Langberg H, Olesen J, Gonzales-Alonzo J, Bulow J, Kjaer M: Monitoring tissue oxygen availability with near infrared spectroscopy (NIRS) in health and disease. Scand J Med Sci Sports 2001, 11: 213-222. 10.1034/j.1600-0838.2001.110404.x
Ward KR, Ivatury RR, Barbee RW, Terner J, Pittman R, Filho IP, Spiess B: Near infrared spectroscopy for evaluation of the trauma patient: a technology review. Resuscitation 2006, 68: 27-44. 10.1016/j.resuscitation.2005.06.022
De Blasi RA, Palmisani S, Alampi D, Mercieri M, Romano R, Collini S, Pinto G: Microvascular dysfunction and skeletal muscle oxygenation assessed by phase-modulation near-infrared spectroscopy in patients with septic shock. Intensive Care Med 2005, 31: 1661-1668. 10.1007/s00134-005-2822-y
Knotzer H, Pajk W, Dunser MW, Majer S, Mayr AJ, Ritsch N, Friesenecker B, Hasibeder WR: Regional microvascular reactivity in patients with different degree of multiple organ dysfynction syndrome. Anesth Analg 2006, 102: 1187-1193. 10.1213/01.ane.0000198587.10553.c1
Creteur J, Carollo T, Soldati G, Buchele G, De Backer D, Vincent JL: The prognostic value of muscle StO 2 in septic patients. Intensive Care Med 2007, 33: 1549-1556. 10.1007/s00134-007-0739-3
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G: 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med 2003, 29: 530-538.
Jhanji S, Stirling S, Patel N, Hinds CJ, Pearse RM: The effect of increasing doses of norepinephrine on tissue oxygenation and microvascular flow in patients with septic shock. Crit Care Med 2009, 37: 1961-1966. 10.1097/CCM.0b013e3181a00a1c
Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemans-van Straaten HM, Zandstra DF: Nitroglycerin in septic shock after intravascular volume resuscitation. The Lancet 2002, 360: 1395-1396. 10.1016/S0140-6736(02)11393-6
Macias WL, Yan SB, Williams MD, Um SL, Sandusky GE, Ballard DW, Planquois JM: New insights into the protein C pathway: potential implications for the biological activities of drotrecogin alfa (activated). Crit Care 2005,9(Suppl 4):38-45. 10.1186/cc3747
Yamaji K, Wang Y, Liu Y, Abeyama K, Hashiguchi T, Uchimura T, Krishna Biswas K, Iwamoto H, Maruyama I: Activated protein C, a natural anticoagulant protein, has antioxidant properties and inhibits lipid peroxidation and advanced glycation end products formation. Thromb Res 2005, 115: 319-325. 10.1016/j.thromres.2004.09.011
Gierer P, Hoffmann JN, Mahr F, Menger MD, Mittlmeier T, Gradl G, Vollmar B: Activated protein C reduces tissue hypoxia, inflammation, and apoptosis in traumatized skeletal muscle during endotoxiemia. Crit Care Med 2007, 35: 1966-1971. 10.1097/01.CCM.0000275270.14835.2A
Hoffmann JN, Vollmar B, Laschke MW, Inthorn D, Fertmann J, Schildberg FW, Menger MD: Microhemodynamic and cellularmechanisms of activated protein action during endotoxemia. Crit Care Med 2004, 32: 1011-1017. 10.1097/01.CCM.0000120058.88975.42
Isobe H, Okajima K, Uchiba M, Mizutani A, Harada N, Nagasaki A, Okabe K: Activated protein C prevents endotoxin-induced hypotension in rats by inhibiting excessive production of nitric oxide. Circulation 2001, 104: 1171-1175. 10.1161/hc3501.093799
Marechal X, Favory R, Joulin O, Montaigne D, Hassoun S, Decoster B, Zerimech F, Neviere R: Endothelial glycocalyx damage during endotoxemia coincides with microcirculatory dysfunction and vascular oxidative stress. Shock 2008, 29: 572-576. 10.1097/SHK.0b013e318157e926
De Backer D, Verdant C, Chierego M, Koch M, Gullo A, Vincent JL: Effects of drotrecogin alfa activated protein C on microcirculatory alterations in patients with severe sepsis. Crit Care Med 2006, 34: 1-7.
Doerschug KC, Delsing AS, Schmidt GA, Haynes WG: Impairments in microvascular reactivity are related to organ failure in human sepsis. Am J Physiol Heart Circ Physiol 2007, 293: 1065-1071. 10.1152/ajpheart.01237.2006
Skarda DE, Mulier KE, Myers DE, Taylor JH, Beilman GJ: Dynamic near-infrared spectroscopy measurements in patients with severe sepsis. Shock 2007, 27: 345-353. 10.1097/01.shk.0000239779.25775.e4
Pareznik R, Knezevic R, Voga G, Podbregar M: Changes in muscle tissue oxygenation during stagnant ischemia in septic patients. Intensive Care Med 2006, 32: 87-92. 10.1007/s00134-005-2841-8
Acknowledgements
This article is part of Critical Care Volume 13 Supplement 5: Tissue oxygenation (StO2) in healthy volunteers and critically-ill patients. The full contents of the supplement are available online at http://ccforum.com/supplements/13/S5. Publication of the supplement has been supported with funding from Hutchinson Technology Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
AD and PP received a research grant from Eli-Lilly Italy. CI and RB received educational grants from Hutchinson Technology.
Rights and permissions
About this article
Cite this article
Donati, A., Romanelli, M., Botticelli, L. et al. Recombinant activated protein C treatment improves tissue perfusion and oxygenation in septic patients measured by near-infrared spectroscopy. Crit Care 13 (Suppl 5), S12 (2009). https://doi.org/10.1186/cc8010
Published:
DOI: https://doi.org/10.1186/cc8010