Abstract
Introduction
Anemia is one of the most common medical complications to be encountered in critically ill patients. Based on the results of clinical trials, transfusion practices across the world have generally become more restrictive. However, because reduced oxygen delivery contributes to 'secondary' cerebral injury, anemia may not be as well tolerated among neurocritical care patients.
Methods
The first portion of this paper is a narrative review of the physiologic implications of anemia, hemodilution, and transfusion in the setting of brain-injury and stroke. The second portion is a systematic review to identify studies assessing the association between anemia or the use of red blood cell transfusions and relevant clinical outcomes in various neurocritical care populations.
Results
There have been no randomized controlled trials that have adequately assessed optimal transfusion thresholds specifically among brain-injured patients. The importance of ischemia and the implications of anemia are not necessarily the same for all neurocritical care conditions. Nevertheless, there exists an extensive body of experimental work, as well as human observational and physiologic studies, which have advanced knowledge in this area and provide some guidance to clinicians. Lower hemoglobin concentrations are consistently associated with worse physiologic parameters and clinical outcomes; however, this relationship may not be altered by more aggressive use of red blood cell transfusions.
Conclusions
Although hemoglobin concentrations as low as 7 g/dl are well tolerated in most critical care patients, such a severe degree of anemia could be harmful in brain-injured patients. Randomized controlled trials of different transfusion thresholds, specifically in neurocritical care settings, are required. The impact of the duration of blood storage on the neurologic implications of transfusion also requires further investigation.
Similar content being viewed by others
Introduction
A key paradigm in the management of neurocritical care patients is the avoidance of 'secondary' cerebral insults [1–3]. The acutely injured brain is vulnerable to systemic derangements, such as hypotension, hypoxemia, or fever, which may further exacerbate neuronal damage [4–7]. Thus, critical care practitioners attempt to maintain a physiologic milieu that minimizes secondary injury, thereby maximizing the chance of a favorable functional and neurocognitive recovery.
Anemia is defined by the World Health Organization as a hemoglobin (Hb) concentration less than 12 g/dl in women and 13 g/dl in men [8]. It is one of the most common medical complications encountered in critically ill patients, including those with neurologic disorders. About two-thirds of patients have Hb concentrations less than 12 g/dl at the time of intensive care unit (ICU) admission, with a subsequent decrement of about 0.5 g/dl per day [9–12]. The etiology of ICU-acquired anemia is multifactorial. Systemic inflammation reduces red blood cell (RBC) development by blunting the production of erythropoietin and interfering with the ability of erythroblasts to incorporate iron [13–17]. RBC loss is accelerated by frequent phlebotomy, reduced RBC survival, and occasional hemorrhage. Large volumes of fluid used during resuscitation, with resultant hemodilution, may also contribute to early reductions in Hb levels [18–22].
Anemia can easily be corrected with the use of allogeneic RBC transfusions. The proportion of patients receiving blood during their ICU stay varies from 20 to 44%, and those who are transfused receive an average of as many as five units [10, 11, 23, 24]. However, two multi-center, randomized controlled trials (RCTs) and two large observational studies have shown the liberal use of blood transfusions, with the goal of maintaining relatively arbitrary Hb concentrations (e.g. 10 g/dl), to not only be ineffective at improving outcomes, but also potentially harmful [10, 11, 25, 26]. Still, because impaired oxygen (O2) delivery is thought to be an important factor in secondary brain injury, it remains uncertain whether these findings can be broadly applied to neurocritical care patients. Accordingly, it remains common practice for clinicians to set target Hb levels at a minimum of 9 to 10 g/dl in this setting [27–29].
Materials and methods
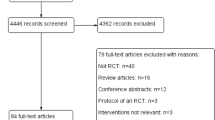
To describe the physiologic and clinical implications of anemia and transfusion in neurocritical care patients, we used the OVID interface to search MEDLINE from its inception until March 9, 2009. We combined the following MESH headings: (anemia OR blood transfusion OR hemodilution OR hematocrit OR hemoglobins) AND (stroke OR craniocerebral trauma OR subarachnoid hemorrhage OR cerebral hemorrhage OR cerebrovascular circulation OR cardiac surgical procedures OR coronary artery bypass). This search yielded 2137 English language publications dealing primarily with adults (>18 years old). Each abstract was reviewed, and both human and animal studies assessing the impact of anemia, hemodilution, or the use of RBC transfusions on a physiologic or clinical outcome were chosen for more detailed review. Relevant review articles and case reports were also included, and the references of selected papers were screened for additional publications. Clinical studies involving specific groups of neurocritical care patients were selected for inclusion in evidentiary tables.
Results and discussion
Physiologic implications of anemia
Cerebral blood flow and oxygen delivery
The amount of oxygen reaching specific organs is the product of local blood flow and the arterial oxygen content (CaO2). The latter is dependent on the Hb concentration and the degree to which it is saturated with O2 (SaO2), with a small amount of O2 also dissolved in blood. Thus, global systemic O2 delivery can be expressed by the following equation:

O2 delivery to the brain can be conceptualized using the same equation, but by substituting cerebral blood flow (CBF) for cardiac output (CO). Flow through the cerebral vasculature is determined by the cerebral perfusion pressure (CPP), the length and caliber of the vessels, and the viscosity of blood, as described by the Hagen-Poiseuille equation:

Regulation of CBF and cerebral O2 delivery in response to physiologic stressors is achieved largely by homeostatic variations in the caliber of cerebral vessels (the 'r' in the above equation; Figure 1).
Physiologic parameters influencing cerebral blood flow (a) The effects of mean arterial blood pressure (MAP) (solid line = normal autoregulation; dashed line = deranged autoregulation), (b) cerebral metabolic rate (CMRO2), (c) partial pressure of carbon dioxide (PCO2), (d) partial pressure of oxygen (PO2) and arterial oxygen content (CaO2) (solid curved line = PO2; dashed line = CaO2) are shown. CBF = cerebral blood flow.
CPP is the difference between mean arterial pressure and cerebral venous pressure; intracranial pressure is widely used as a surrogate for the latter. The response of the cerebral vasculature to changes in CPP is referred to as CBF autoregulation ('pressure-reactivity'). Cerebral arterioles vasoconstrict in response to raised CPP and vasodilate when there are reductions, thereby maintaining constant CBF (Figure 1a). Autoregulation is sometimes impaired in neurocritical care patients, such that CBF becomes directly dependent on CPP, making the brain more vulnerable to both hypo- and hyperperfusion [30–32].
There are numerous other stimuli that may modify cerebral vascular resistance and CBF. Both global and regional CBF are tightly coupled to metabolism. Thus, physiologic changes that lead to a reduction in cerebral metabolic rate (CMRO2) (e.g. hypothermia or sedation) will also proportionally reduce CBF (Figure 1b). In addition, CBF is influenced by variations in the partial pressures of carbon dioxide (PCO2; 'CO2-reactivity'), and to a lesser degree, O2 (PO2) (Figures 1c, d). CBF increases in response to a decrease in PO2, although this effect is probably minimal until the level approaches 60 mmHg [30].
In response to worsening anemia, neuronal O2 delivery is initially preserved both by the systemic cardiovascular response and mechanisms that are more specifically neuroprotective.
Cardiovascular response to anemia
A falling Hb concentration is sensed by aortic and carotid chemoreceptors, resulting in stimulation of the sympathetic nervous system, which in turn raises heart rate and contractility, thereby augmenting CO [33–35]. The reduction in blood viscosity results in a corresponding reduction in afterload, as well as enhanced flow through post-capillary venules, greater venous return, and increased preload [36–38]. Thus, stroke volume, CO, and blood pressure (as well as CPP) increase in response to isovolemic anemia. Tissues are further protected from falling O2 delivery because of their capacity to increase O2 extraction and maintain constant O2 consumption. In the brain, irreversible ischemia may not occur until the O2 extraction fraction (OEF) exceeds 75% [39–43]. Systemic anaerobic metabolism does not develop until the Hb concentration falls well below 5 g/dl in otherwise healthy individuals [44]. On the other hand, many neurocritical care patients have concomitant cardiac disease and left ventricular dysfunction which may prevent an appropriate increase in CO in response to sympathetic stimulation. This is commonly the case even in the absence of pre-existing heart disease; for example, among patients with acute 'high-grade' aneurysmal subarachnoid hemorrhage (SAH) (Hunt-Hess grades 3 to 5), more than one-third have regional left ventricular wall motion abnormalities detectable by echocardiography [45].
Cerebrovascular response to anemia
Apart from the increased flow produced by higher CPP and lower blood viscosity, anemia also induces cerebral vasodilatation [46–48]. When Hb (and therefore CaO2) falls, there appears to be a disproportionate increase in CBF in relation to other organs (Figure 1d) [49]. The mechanisms underlying this increase in vessel caliber are still being clarified, but include some of the same factors involved in CBF pressure-autoregulation; these have recently been reviewed in detail [46]. Importantly, anemia results in upregulation of nitric oxide (NO) production by perivascular neurons and vascular smooth muscle surrounding cerebral blood vessels. The importance of these pathways is supported by the observation that inhibition of NO synthase blunts hypoxia- and anemia-induced cerebral vasodilatation [50–52]. However, additional factors are undoubtedly involved [53–55]. Sympathetic β2 receptor stimulation is an example of one such mechanism that contributes to vasodilatation and maintenance of CBF [56]. Other biochemical mediators that are upregulated in the brain in response to anemia include vascular endothelial growth factor, hypoxia inducible factor 1α, and erythropoietin [46, 57]. Although it seems likely that these mediators are neuroprotective, it remains possible that they could also have harmful pathophysiologic effects [46].
Compensatory mechanisms eventually fail
As anemia worsens, the resultant increases in CBF and OEF eventually become insufficient to overcome the reduced CaO2 produced by a low Hb concentration (Figure 2). The point at which this threshold is reached is not clear and probably varies somewhat between patients. A sophisticated mathematical model based on animal data suggested that CMRO2 is well preserved in normal brain, even with severe reductions in Hb concentration. In contrast, penumbral brain appears to be much more vulnerable, with O2 delivery and CMRO2 progressively declining as Hb falls below 10 to 12 g/dl [58–62]. As with cerebral ischemia, impairment of the usual protective mechanisms induced by anemia has also been demonstrated as a result of brain trauma [63].
Effects of falling hemoglobin concentration on cerebral oxygen delivery. With mild hemodilution, it is theoretically possible that the resultant increase in cerebral blood flow (CBF) can raise overall O2 delivery. However, with further decrements in hemoglobin, the increment in CBF is insufficient to overcome the reduction in arterial oxygen content (CaO2).
A study of euvolemic hemodilution in healthy human volunteers confirmed that even profound anemia (Hb about 5 g/dl) was relatively well tolerated; however, subtle abnormalities in neurocognitive testing began to emerge when Hb concentrations fell below 7 g/dl [64, 65]. The co-existence of other physiologic stressors may also make anemia less tolerable; for example, experimental studies have found that cerebral O2 delivery is preserved in the presence of both severe anemia and hypotension individually, but not when they are both present [66, 67]. Additionally, anemia-induced cerebral vasodilatation appears to interfere with the usual response to variations in PCO2 [47, 68–70]. These observations raise concerns that relatively inadequate O2 delivery could occur at Hb levels well above 7 g/dl in critical care patients with cerebrovascular disease, pre-existing central nervous system pathology (e.g. an ischemic or 'traumatic' penumbra) or deranged regulation of CBF. Thus, there is strong physiologic rationale for believing that a restrictive transfusion threshold of 7 g/dl, although clearly safe in many critical care patients [25, 26], may not be without risk in neurocritical care patients.
Risks of red blood cell transfusion
Even if anemia is harmful, this does not necessarily prove that liberal use of allogeneic RBCs to normalize Hb concentrations is justified. Emerging data indicates that stored blood has important differences from patients' own blood. A number of changes occur over time as RBCs are being stored; some of these alterations could have important implications after transfusion, and they are collectively referred to as the 'storage lesion'. Biochemical changes include reductions in ATP, loss of membrane phospholipids, and oxidative damage to proteins. The consequence is a gradual change in RBC appearance from the usual biconcave discs to irreversibly deformed and stellate-shaped spheroechinocytes [71, 72]. Loss of RBC membrane function, as well as an increased tendency to adhere to endothelium, may interfere with microcirculatory flow [72, 73]. RBC 2-3-diphosphoglycerate levels become depleted to the point of being essentially undetectable after one week of storage. Although levels are usually restored within 24 to 72 hours after transfusion, the transiently increased binding affinity of Hb interferes with the release of O2 for use by tissues [74].
Thus, although blood transfusions are generally given with the intention of raising O2 delivery, the storage-induced changes may prevent RBCs from achieving their intended purpose. For example, studies using gastric tonometry parameters as a surrogate for mesenteric perfusion have not shown improvements following transfusion [75, 76]. Similarly, RBCs also appear to have little effect on skeletal muscle O2 tension in postoperative patients or on global O2 consumption in the critically ill [77, 78].
Transfusion-related acute lung injury is now the most common cause of transfusion-related mortality reported to the Food and Drugs Administration [79]. Transfusion may have immunosuppressive effects, which are thought to be due to concomitant white blood cell transmission. Several studies have suggested a link between the use of allogeneic RBCs and both nosocomial infections and acute respiratory distress syndrome [80–83]. Alternatively, RCTs, where well-matched groups were transfused with differing intensities, have not yet convincingly confirmed these associations [25, 26]. Furthermore, the risk of complications may be less since the implementation of universal leukoreduction in many jurisdictions [84].
It has been suggested that the use of fresher blood might further minimize the risks of transfusion, while also maximizing their physiologic effect. Results have been conflicting, and there is little data specifically in neurocritical care patients [71, 75, 76]. A recent animal study found fresh blood to be more effective at raising brain tissue oxygen tension (PbtO2) and preserving CBF in comparison to stored blood [85]. Alternatively, Weiskopf and colleagues performed isovolemic hemodilution to Hb concentrations of 55 to 74 g/L in healthy volunteers and then transfused them with autologous blood stored for either less than five hours or more than 14 days; neurocognitive test performance did not differ between the two groups [86].
Anemia and RBC transfusion in specific neurocritical care settings
The importance of ischemia in causing secondary brain injury appears to vary for different neurocritical care conditions. For example, cerebral vasospasm and delayed infarction are major causes of neurologic deterioration in the two weeks following a ruptured cerebral aneurysm [87, 88]. In contrast, the frequency and relevance of cerebral ischemia in the pathophysiology of traumatic brain injury (TBI) or intracerebral hemorrhage (ICH) continue to be debated [40, 89–91]. Accordingly, the significance of anemia and optimal transfusion thresholds may not be consistent from one condition to the next.
Lessons from cardiac surgery
A great deal of what is known about the neurologic effects of anemia has been reported in the cardiac surgical literature. A substantial proportion of patients undergoing cardiac surgery receive blood transfusions, even though large volume hemorrhage is comparatively less common [92]. Perioperative stroke occurs in 1 to 6% of patients and is strongly associated with greater morbidity and mortality [93, 94]. An even larger proportion (≥50%) develops at least transient neurocognitive dysfunction that is likely to be, at least in part, due to cerebral ischemia [95, 96]. Thus, the prevention and treatment of cerebral ischemia is of major concern in the perioperative period.
We identified 12 studies assessing the association between perioperative Hb concentrations and subsequent neurologic complications (Table 1). When defined as an Hb concentration less than 12.5 g/dl, about one-quarter of patients are anemic preoperatively [97]. Blood loss and hemodilution during cardiopulmonary bypass usually lead to nadir intraoperative Hb concentrations of 7.0 to 8.5 g/dl; levels at ICU admission are typically 8.5 to 9.5 g/dl [98]. Several, but not all, studies have suggested that the degree of Hb reduction is an independent predictor of stroke, delirium, neurocognitive dysfunction, and other adverse outcomes [97–108] (Table 1). Although it has not been proven with certainty that these relations are causative, it seems prudent to avoid major reductions in Hb as best as possible with relevant blood-conservation strategies [109–113].
A recent RCT involving 121 elderly patients undergoing coronary artery bypass compared two intraoperative hematocrit targets (15 to 18% vs. ≥ 27%) [102]. The study was terminated early because of high complication rates in both groups; however, a greater degree of postoperative neurocognitive dysfunction was observed among patients managed with more extreme hemodilution. In addition, although not necessarily directly applicable to adults, further evidence that excessive hemodilution may have harmful neurologic effects comes from the neonatal literature. Combined data from two RCTs suggested that hematocrit levels below 23.5% during cardiopulmonary bypass were associated with impaired psychomotor development at one year of age [114–116].
Whether using RBC transfusions to maintain higher perioperative Hb levels helps avoid neurologic complications remains uncertain. For example, although Karkouti and colleagues found nadir hematocrit levels during cardiopulmonary bypass to be a predictor of stroke in a multivariable analysis, the same was also true for the perioperative use of transfusions [105]. An association between transfusion and focal or global neurologic deficits has been confirmed in numerous other studies (Table 2) [117–125].
One study compared clinical outcomes, including the risk of perioperative stroke, between 49 Jehovah's Witnesses who underwent cardiac surgery without blood products and a matched control group of 196 patients, in whom RBC transfusions were used. No significant differences were observed; however, only nine patients in total experienced a stroke, such that this study lacked statistical power to detect a difference. The severity of anemia in Jehovah's Witness patients was not reported [123].
In a large, single-center, retrospective study, Koch and colleagues explored whether the association between RBCs and worse outcomes could be related to the duration of blood storage. Outcomes were compared among cardiac surgical patients depending on whether they were transfused with exclusively 'newer' (≤14 days old; median 11 days) or 'older' (>14 days old; median 20 days) blood during the perioperative period [126]. In-hospital mortality and postoperative complications, including sepsis, renal failure, and need for mechanical ventilation, were greater among patients receiving older blood. However, there was no significant difference in the incidence of stroke and coma.
In summary, there remains uncertainty concerning optimum Hb levels for neuroprotection of patients undergoing cardiac surgery. Many intensivists routinely employ a postoperative transfusion threshold of 7 g/dl, although this may not be the optimum Hb level for the avoidance of neurologic complications. By necessity, the recommendations of published consensus guidelines are relatively non-specific, and state that it is "not unreasonable to transfuse red cells in certain patients with critical noncardiac end-organ ischemia whose Hb levels are as high as 10 g/dl" [111]. Funding was recently secured in the UK for a multi-center RCT comparing transfusion triggers of 7.5 vs. 9 g/dl [92].
Traumatic brain injury
The majority of patients dying from severe TBI have histologic evidence of ischemic damage [127]. Early global CBF reductions occur in many patients, often to levels that are considered to be in the ischemic range [128, 129]. Reductions in both jugular venous O2 saturation (SjvO2) and PbtO2 are not only common, but their frequency and depth are predictive of worse outcomes [130–133]. However, the fall in CBF may be appropriate for a corresponding drop in metabolic rate [134, 135]. Recent studies using positron emission tomography (PET) have suggested that although ischemia does occur, it is less common than previously thought. Furthermore, much of the 'metabolic distress' detected by multimodal monitoring (SjvO2, PbtO2, and microdialysis parameters) is not necessarily attributable to classical ischemia [39, 134, 135].
On the other hand, there appears to be a great deal of regional heterogeneity in CBF and CMRO2 [136]. Even if the overall ischemic brain volume is relatively small, certain vulnerable regions may still benefit from enhanced O2 delivery [137]. As with cardiac surgical patients, relatively extreme reductions in Hb are likely to be deleterious. A recent animal model found that although isovolemic hemodilution to Hb concentrations of 5 to 7 g/dl resulted in an overall increase in CBF, it produced larger contusion volumes, more apoptosis, and lower PbtO2 [138].
Potentially beneficial physiologic effects of transfusion have been shown in four studies of patients with severe TBI [139–142], each of which demonstrated that PbtO2 increases following the administration of RBCs (Table 3) [139]. However, this increment was inconsistent, relatively small and often of questionable clinical importance. Of concern, in some cases there was even a reduction in PbtO2. It is possible that some of the variation in the cerebral effects of transfusion could be, in part, attributable to the variable age of transfused blood. Leal-Noval and colleagues recently found that only those patients having received RBCs less than 14 days old had a statistically significant improvement in PbtO2 one hour after transfusion [141]. Although these results are intriguing, they are too premature to influence clinical practice and require confirmation in larger studies. Just because PbtO2 rises, does not necessarily mean that CMRO2 has increased. On the contrary, Zygun and colleagues found no improvement in cerebral lactate to pyruvate ratio (LPR – a marker of ischemia and 'metabolic distress') in response to transfusion, despite an increment in PbtO2 [142].
In a retrospective study of 169 patients with TBI, Carlson and colleagues found nadir hematocrit levels to be associated with a worse Glasgow Outcome Scale at hospital discharge. However, the association between RBC transfusion and poor outcome was even stronger [143]. Other observational studies have reached similar conclusions (Table 4) [144–151]. Unfortunately, there are no large RCTs to guide practice at this time. The TRICC trial enrolled only 67 patients with severe TBI [150]. Although no statistically significant benefit from a liberal transfusion strategy was observed, this subgroup was too small to reach meaningful conclusions. Thus, the optimal use of RBCs in patients with severe TBI remains unclear. A recent survey found that practice across the USA is variable, and that the majority of clinicians believe a threshold of 7 g/dl to be too restrictive, especially in the presence of intracranial hypertension [27].
Subarachnoid hemorrhage
Narrowing of the cerebral vasculature (angiographic vasospasm) complicates about two-thirds of cases of SAH. Vasospasm most often emerges between days 3 and 14 after SAH and is the most important cause of secondary brain injury [87]. Evidence of cerebral infarction that was not present initially is observed in as many as 50 to 70% of survivors using magnetic resonance imaging (MRI) [152, 153]. Unlike other forms of stroke, the predictable risk of vasospasm and cerebral ischemia provides a unique opportunity for the provision of neuroprotection prior to the insult.
Three studies have assessed the association between daily Hb concentrations and eventual neurologic outcome [154–156]. Each of these demonstrated that patients with an unfavorable outcome consistently have lower Hb levels throughout much of the first two weeks in hospital (Table 5). The degree of decrement in Hb levels over time was also highly predictive of outcome [154]. Despite the use of multivariable analyses, there were numerous potentially confounding variables that could not be adjusted for. For example, patients who are 'sicker' tend to have more blood drawn for laboratory tests, have more invasive procedures performed, and tend to receive more intravenous fluids, all of which could contribute to lower Hb concentrations. Thus, the association between lower Hb and poor outcome has not conclusively been proven to be causative.
As in other settings, several studies have also shown a strong association between transfusion and unfavorable outcomes following SAH (Table 5) [28, 157–160]. One unconfirmed report suggested that the use of RBCs could contribute to the development of cerebral vasospasm, perhaps by promoting inflammation or depleting endogenous NO supplies [160]. A recent observational study found no difference in complications based on the transfusion of older (>21 days) compared with newer (≤21 days) units of blood, although this assessment was based on only 85 transfused patients [28].
Hemodilution, together with hypervolemia and hypertension, has been used as part of 'triple H therapy', a therapeutic strategy to improve CBF in patients with vasospasm [161]. One study used 133Xenon injections to assess global CBF in eight patients with SAH. As expected, isovolemic hemodilution from a mean Hb of 11.9 to 9.2 g/dl produced an increase in global CBF and a reduction in cerebral vascular resistance. However, the increase in CBF was not sufficient to overcome the reduction in CaO2, such that global O2 delivery fell and ischemic brain volume actually increased [162]. Complimentary findings were subsequently reported by Muench and colleagues, who used aggressive volume expansion on days 1, 3, and 7, which produced a concomitant reduction in Hb concentration ranging from of 1.3 to 2.0 g/dl. Although this intervention consistently produced a small increment in CBF, it actually caused a proportionally larger decline in PbtO2 (Table 3) [163].
More recently, Dhar and colleagues assessed the effects of transfusion in patients with SAH using PET [164]. PET scans were performed before and after the administration of one unit of RBCs to patients with pre-transfusion Hb concentrations less than 10 g/dl. Although no change in CMRO2 was observed, OEF dropped from 49 to 41%. Thus, it is possible that in vulnerable regions of the brain with relatively high OEF, RBC transfusions could help avoid irreversible infarction. Another recent study of 20 SAH patients found Hb concentrations less than 9 g/dl to be associated with lower PbtO2 and higher LPR [165].
In summary, there is now extensive data to suggest that even moderate degrees of anemia are associated with worse physiologic parameters and clinical outcomes in patients with SAH. However, it is not clear that the use of RBC transfusions can modify these associations. An adequately powered, RCT comparing different transfusion thresholds is urgently required, especially in light of the vulnerability of these patients to delayed cerebral ischemia and the frequency with which they develop anemia.
Ischemic stroke
Because of the known inverse relation between hematocrit and CBF, there has long been interest in the clinical use of hemodilution in the management of acute ischemic stroke [166]. Some studies have suggested that relatively high Hb concentrations may predispose to the development of strokes [167–173], as well as contribute to worse outcomes when cerebral ischemia occurs [174–177]. It is conceivable that increased viscosity could have a particularly deleterious effect on microvascular flow through the ischemic penumbra. Consistent with this notion, Allport and colleagues performed serial MRI scans in 64 stroke patients and found that a higher baseline hematocrit was independently associated with infarct growth and less chance of successful reperfusion [178].
The deleterious association with a higher hematocrit has, however, been inconsistent and largely observed at levels in excess of 45% (Table 6). Indeed, several studies have shown a U-shaped relation where low hematocrit levels are also associated with larger infarct size and worse outcomes [175, 177, 179–184]. The lowest risk of stroke and the best outcomes have generally been observed with mid-range hematocrit levels of about 42 to 45% [172, 175]. This range was also supported by a study using 133Xe to assess CBF in stroke patients, with the finding that cerebral O2 delivery was optimized at a hematocrit level of 40 to 45% [185]. Conversely, several animal studies have suggested that cerebral O2 delivery and neuroprotection are optimized at slightly lower hematocrit or Hb values, in the range of 30 to 36% and 10 to 12 g/dl, respectively [58, 186, 187]. Greater degrees of hemodilution consistently appear to be deleterious [188]. Some case reports have even described patients with relatively stenotic cerebral vessels who may have developed ischemic strokes directly attributable to anemia [189–191].
Several RCTs and a meta-analysis have not shown any clear benefit to using hemodilution as a therapeutic strategy in acute ischemic stroke [192]. However, there was a great deal of heterogeneity in the methodology of these studies (timing of treatment, specific type and dose of plasma expander, target hematocrit). Although each study deliberately produced reductions in hematocrit with the use of colloids and/or phlebotomy, the reductions were relatively modest, generally not beyond 37 to 38% [192–196].
More recently, several animal studies and phase II human trials have suggested that hemodilution with relatively high doses of albumin may reduce infarct size and enhance the efficacy of thrombolytic therapy [197–200]. It is likely that this effect was observed, in part, because of the unique properties of albumin, rather than only hemodilution. In a phase II dose-finding study, the reduction in hematocrit induced by the highest doses of albumin averaged 6 to 10% [198, 199].
In summary, there is currently no routine role for hemodilution in the management of acute ischemic stroke. Whether transfusing anemic stroke patients with Hb concentrations lower than 9 to 11 g/dl is beneficial has not been well evaluated.
Intracerebral hemorrhage
There has been controversy regarding the importance of cerebral ischemia in causing secondary brain injury after ICH. Early studies had suggested that an expanding intracerebral hematoma could cause mechanical compression and vasoconstriction of the surrounding vasculature, thereby producing a 'perihematomal penumbra' [201–203]. Imaging with PET, CT perfusion scans, and MRI have confirmed that the majority of patients with ICH have a surrounding rim of hypoperfusion [91, 204–206]. The biochemistry of this region appears to be similar to that of traumatic cerebral contusions [207]. However, OEF is not increased in the perihematomal tissues, suggesting that this hypoperfusion is due to reduced cerebral metabolism, rather than true ischemia [91]. Thus, mild reductions in Hb concentration are unlikely to have a major impact in contributing to neuronal death. Nevertheless, it remains uncertain whether perihematomal tissues tolerate anemia as well as healthy brain.
Use of hemoglobin-based blood substitutes
Hb-based blood substitutes (HBBS) have theoretical advantages over other fluids in the resuscitation of neurocritical care patients, because they have the potential to achieve the CBF-enhancing effects of hemodilution, while concomitantly maintaining, or even raising, CaO2. Several animal studies performed in the setting of experimental ischemic stroke, TBI, and SAH-induced vasospasm have supported this concept [208–221]. Alternatively, free Hb may also have numerous deleterious effects, probably mediated, in large part, by scavenging of NO [222]. Although not all products are identical, a recent meta-analysis of RCTs suggested that their use is associated with an increased risk of death and myocardial infarction [223]. One phase II RCT involving 85 patients with ischemic stroke reported worse neurological outcomes with the use of diaspirin cross-linked Hb [224]. Of the five RCTs involving trauma patients, none specifically assessed the subgroup of patients with TBI, although the largest study reported no statistically significant interaction between HBBS and admission Glasgow coma scale on mortality [225–229]. Two of the three RCTs in the setting of cardiac surgery reported the occurrence of perioperative stroke; there were no differences between HBBS-treated and control patients [230, 231]. Thus, although the use of HBSS in neurocritical care should be further investigated, there is currently no role for the routine use of these products.
Conclusions
Anemia is common in neurocritical care patients, is associated with worse outcomes, and should be avoided as much as possible with blood conservation strategies. Although Hb concentrations as low as 7 g/dl are well tolerated by most critically ill patients [25], there is ample data from animal studies, as well as human physiologic and observational studies to suggest that such a severe degree of anemia could be harmful in the brain-injured patient. Thus, in our practice, we frequently transfuse selected patients with Hb concentrations less than 8 to 9 g/dl. However, because allogeneic RBCs have multiple potentially deleterious effects, it cannot be assumed that the use of transfusions to 'correct' Hb levels alters the association between anemia and adverse outcomes. The impact of the duration of blood storage on the neurologic implications of transfusion requires further investigation. Unfortunately, existing guidelines provide little guidance to clinicians in deciding when to transfuse anemic stroke and neurocritical care patients [232–236]; clearly, RCTs are needed.
Key messages
-
Despite an increment in cerebral blood flow, even moderate reductions in Hb concentration lead to less overall cerebral oxygen delivery, resulting in lower PbtO2 and 'metabolic distress' (higher OEF and LPR).
-
Although the relation has not been proven with certainty to be causative, anemia is consistently associated with worse outcomes among neurocritical care patients.
-
Despite some beneficial physiologic effects (increased PbtO2 and reduced OEF), it remains uncertain whether transfusion can improve cerebral metabolism and help salvage tenuous 'penumbral' brain tissue, thereby improving neurologic recovery.
-
Although a transfusion threshold of 7 g/dl is safe in many general critical care patients, it remains unclear if this is also true in neurocritical care patients.
-
The duration of red blood cell storage may have implications on the cerebral consequences of transfusion.
Abbreviations
- CBF:
-
cerebral blood flow
- CaO2:
-
arterial oxygen content
- CMRO2:
-
cerebral metabolic rate
- CO:
-
cardiac output
- CO2:
-
carbon dioxide
- CPP:
-
cerebral perfusion pressure
- DO2:
-
oxygen delivery
- Hb:
-
hemoglobin
- HBBS:
-
hemoglobin-based blood substitutes
- ICH:
-
intracerebral hemorrhage
- ICU:
-
intensive care unit
- LPR:
-
lactate to pyruvate ratio
- MRI:
-
magnetic resonance imaging
- NO:
-
nitric oxide
- O2:
-
oxygen
- OEF:
-
oxygen extraction fraction
- PbtO2:
-
brain tissue oxygen tension
- PCO2:
-
partial pressure of carbon dioxide
- PET:
-
positron emission tomography
- PO2:
-
partial pressure of oxygen
- RBC:
-
red blood cell
- RCT:
-
randomized controlled trial
- SAH:
-
subarachnoid hemorrhage
- SaO2:
-
oxygen saturation
- SjvO2:
-
jugular venous oxygen saturation
- TBI:
-
traumatic brain injury.
References
Al Thanayan E, Bolton C, Hichici D, Savard M, Teitelbaum J, Young B, Zygun D: Neurocritical care in Canada: evolving streams in a new discipline. Can J Neurol Sci 2008, 35: 405-408.
Elf K, Nilsson P, Enblad P: Outcome after traumatic brain injury improved by an organized secondary insult program and standardized neurointensive care. Crit Care Med 2002, 30: 2129-2134. 10.1097/00003246-200209000-00029
Patel HC, Menon DK, Tebbs S, Hawker R, Hutchinson PJ, Kirkpatrick P: Specialist neurocritical care and outcome from head injury. Intensive Care Med 2002, 28: 547-553. 10.1007/s00134-002-1235-4
Miller JD, Sweet RC, Narayan R, Becker DP: Early insults to the injured brain. JAMA 1978, 240: 439-442. 10.1001/jama.240.5.439
Chesnut RM, Marshall LF, Klauber MR, Blunt BA, Baldwin N, Eisenberg HM, Jane JA, Marmarou A, Foulkes MA: The role of secondary brain injury in determining outcome from severe head injury. J Trauma 1993, 34: 216-222. 10.1097/00005373-199302000-00006
McHugh GS, Engel DC, Butcher I, Steyerberg EW, Lu J, Mushkudiani N, Hernandez AV, Marmarous A, Maas AI, Murray GD: Prognostic value of secondary insults in traumatic brain injury: results from the IMPACT study. J Neurotrauma 2007, 24: 287-293. 10.1089/neu.2006.0031
Henzler D, Cooper DJ, Tremayne AB, Rossaint R, Higgins A: Early modifiable factors associated with fatal outcome in patients with severe traumatic brain injury: a case control study. Crit Care Med 2007, 35: 1027-1031. 10.1097/01.CCM.0000259526.45894.08
Iron Deficiency Anemia Assessment, Prevention, and Control: A guide for programme managers[http://whqlibdoc.who.int/hq/2001/WHO_NHD_01.3.pdf]
Rodriguez RM, Corwin HL, Gettinger A, Corwin MJ, Gubler D, Pearl RG: Nutritional deficiencies and blunted erythropoietin response as causes of anemia of critical illness. J Crit Care 2001, 16: 36-41. 10.1053/jcrc.2001.21795
Vincent JL, Baron JF, Reinhart K, Gattinoni L, Thijs L, Webb A, Meier-Hellmann A, Nollet G, Peres-Bota D: Anemia and blood transfusion in critically ill patients. JAMA 2002, 288: 1499-1407. 10.1001/jama.288.12.1499
Corwin HL, Gettinger A, Pearl RG, Fink MP, Levy MM, Abraham E, MacIntyre NR, Shabot MM, Duh MS, Shapiro MJ: The CRIT Study: Anemia and blood transfusion in the critically ill – current practice in the United States. Crit Care Med 2004, 32: 39-52. 10.1097/01.CCM.0000104112.34142.79
Nguyen BV, Bota DP, Melot C, Vincent JL: Time course of hemoglobin concentrations in nonbleeding intensive care unit patients. Crit Care Med 2003, 31: 406-410. 10.1097/00003246-200301001-00001
Scharte M, Fink MP: Red blood cell physiology in critical illness. Crit Care Med 2003, 31: S651-657. 10.1097/01.CCM.0000098036.90796.ED
Rogiers P, Zhang H, Leeman M, Nagler J, Neels H, Mélot C, Vincent JL: Erythropoietin response in blunted in critically ill patients. Intensive Care Med 1997, 23: 159-162. 10.1007/s001340050310
van Iperen CE, Gaillard CA, Kraaijenhagen RJ, Braam BG, Marx JJ, Wiel A: Response of erythropoiesis and iron metabolism to recombinant human erythropoietin in intensive care unit patients. Crit Care Med 2000, 28: 2773-2778. 10.1097/00003246-200008000-00015
Darveau M, Denault AY, Blais N, Notebaert E: Bench-to-bedside review: iron metabolism in critically ill patients. Crit Care 2004, 8: 356-362. 10.1186/cc2862
Corwin HL, Krantz SB: Anemia of the critically ill: "Acute" anemia of chronic disease. Crit Care Med 2000, 28: 3099. 10.1097/00003246-200008000-00080
Walsh TS, Saleh EE: Anemia during critical illness. Br J Anesth 2006, 97: 278-291. 10.1093/bja/ael189
Smoller BR, Kruskall MS: Phlebotomy for diagnostic laboratory tests in adults. Patterns of use and effect on transfusion requirements. N Engl J Med 1986, 314: 1233-1235.
Tarpey J, Lawler PG: Iatrogenic anemia? A survey of venesection in patients in the intensive therapy unit. Anaesthesia 1990, 45: 396-398. 10.1111/j.1365-2044.1990.tb14785.x
Zimmerman JE, Seneff MG, Sn X, Wagner DP, Knaus WA: Evaluating laboratory usage in the intensive care unit: patient and institutional characteristics that influence frequency of blood sampling. Crit Care Med 1997, 25: 737-748. 10.1097/00003246-199705000-00006
Berezina TL, Zaets SB, Kozhura VL, Novoderzhkina IS, Kirsanova AK, Deitch EA, Machiedo GW: Morphologic changes of red blood cells during hemorrhagic shock replicate changes of aging. Shock 2001, 15: 467-470. 10.1097/00024382-200115060-00010
Walsh TS, Garrioch M, Maciver C, Lee RJ, MacKirdy F, McClelland DB, Kinsella J, Wallis C: Red cell requirements for intensive care units adhering to evidence-based transfusion guidelines. Transfusion 2004, 44: 1405-1411. 10.1111/j.1537-2995.2004.04085.x
French CJ, Bellomo R, Finfer SR, Lipman J, Chapman M, Boyce NW: Appropriateness of red blood cell transfusion in Australasian intensive care practice. Med J Aust 2002, 177: 548-551.
Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E: A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 1999, 340: 409-417. 10.1056/NEJM199902113400601
Lacroix J, Hebert PC, Hutchison JS, Hume HA, Tucci M, Ducruet T, Gauvin F, Collet JP, Toledano BJ, Robillard P, Joffe A, Biarent D, Meert K, Peters MJ: TRIPICU Investigators; Canadian Critical Care Trials Group; Pediatric Acute Lung Injury and Sepsis Investigators Network. Transfusion strategies for patients in pediatric intensive care units. N Engl J Med 2007, 356: 1609-1619. 10.1056/NEJMoa066240
Sena MJ, Rivers RM, Muizelaar JP, Battistella FD, Utter GH: Transfusion practices for acute traumatic brain injury: a survey of physicians at US trauma centers. Intensive Care Med 2009, 35: 480-488. 10.1007/s00134-008-1289-z
Kramer AH, Gurka MJ, Nathan B, Dumont AS, Kassell NF, Bleck TP: Complications associated with anemia and blood transfusion in patients with aneurismal subarachnoid hemorrhage. Crit Care Med 2008, 36: 2070-2075. 10.1097/CCM.0b013e31817c1095
Pendem S, Rana S, Manno EM, Gajic O: A review of red cell transfusion in the neurological intensive care unit. NeuroCrit Care 2006, 4: 63-67. 10.1385/NCC:4:1:063
Vavilala MS, Lee LA, Lam AM: Cerebral blood flow and vascular physiology. Anesthesiol Clin North America 2002, 20: 274-264. 10.1016/S0889-8537(01)00012-8
Marshall RS: The functional relevance of cerebral hemodynamics: why blood flow matters to the injured and recovering brain. Curr Opin Neurol 2004, 17: 705-709. 10.1097/00019052-200412000-00010
Udomphorn Y, Armstead WM, Vavilala MS: Cerebral blood flow and autoregulation after pediatric traumatic brain injury. Pediatr Neurol 2008, 38: 225-234. 10.1016/j.pediatrneurol.2007.09.012
Hatcher JD, Chiu LK, Jennings DB: Anemia as a stimulus to aortic and carotid chemoreceptors in the cat. J Appl Physiol 1978, 44: 696-702.
Chapler CK, Cain SM: The physiologic reserve in oxygen carrying capacity: studies in experimental hemodilution. Can J Physiol Pharmacol 1985, 64: 7-12.
Habler OP, Kleen MS, Podtschaske AH, Hutter JW, Tiede M, Kemming GI, Welte MV, Corso CO, Messmer KF: The effect of acute normovolemic hemodilution (ANH) on myocardial contractility in anesthetized dogs. Anesth Analg 1996, 83: 451-458. 10.1097/00000539-199609000-00002
Murray JF, Escobar E, Rapaport E: Effects of blood viscosity on hemodynamic responses in acute normovolemic anemia. Am J Physiol 1969, 216: 638-642.
Fowler NO, Holmes JC: Blood viscosity and cardiac output in acute experimental anemia. J Appl Physiol 1975, 39: 453-456.
Hebert PC, Linden P, Biro G, Hu LQ: Physiologic aspects of anemia. Crit Care Clin 2004, 20: 187-212. 10.1016/j.ccc.2004.01.001
Vespa PM: The implications of cerebral ischemia and metabolic dysfunction for treatment strategies in neurointensive care. Curr Opin Crit Care 2006, 12: 119-123.
Vespa P, Bergsneider M, Hattori N, Wu HM, Huang SC, Martin NA, Glenn TC, McArthur DL, Hovda DA: Metabolic crisis without brain ischemia is common after traumatic brain injury: a combined microdialysis and positron emission tomography study. J Cereb Blood Flow Metab 2005, 25: 763-774. 10.1038/sj.jcbfm.9600073
Senda M, Alpert NM, Mackay BC, Buxton RB, Correia JA, Weise SB, Ackerman RH, Dorer D, Buonanno FS: Evaluation of the 11CO 2 positron emission tomographic method for measuring brain pH. II. Quantitative pH mapping in patients with ischemic cerebrovascular diseases. J Cereb Blood Flow Metab 1989, 9: 859-873.
Coles JP, Fryer TD, Smielewski P, Rice K, Clark JC, Pickard JD, Menon DK: Defining ischemic burden after traumatic brain injury using 15O PET imaging of cerebral physiology. J Cereb Blood Flow Metab 2004, 24: 191-201. 10.1097/01.WCB.0000100045.07481.DE
Sakoh M, Ostergaard L, Rohl L, Smith DF, Simonsen CZ, Sorensen JC, Poulsen PV, Gyldensted C, Sakaki S, Gjedde A: Relationship between residual cerebral blood flow and oxygen metabolism as predictive of ischemic tissue viability: sequential multitracer positron emission tomography scanning of middle cerebral artery occlusion during the critical first 6 hours after stroke in pigs. J Neurosurg 2000, 93: 647-657. 10.3171/jns.2000.93.4.0647
Weiskopf RB, Viele MK, Feiner J, Kelley S, Liberman J, Noorani M, Leung JM, Fisher DM, Murray WR, Toy P, Moore MA: Human cardiovascular and metabolic response to acute, severe isovolemic anemia. JAMA 1998, 279: 217-231. 10.1001/jama.279.3.217
Kothaveale A, Banki NM, Kopelnik A, Yarlagadda S, Lawton MT, Ko N, Smith WS, Drew B, Foster E, Zaroff JG: Predictors of left ventricular regional wall motion abnormalities after subarachnoid hemorrhage. Neurocrit Care 2006, 4: 199-205. 10.1385/NCC:4:3:199
Hare GMT, Tsui AKY, McLaren AT, Ragoonanan TE, Yu J, Mazer CD: Anemia and cerebral outcomes: Many questions, fewer answers. Anesth & Analg 2008, 107: 1356-1370. 10.1213/ane.0b013e318184cfe9
Bruder N, Cohen B, Pellissier D, Francois G: The effect of hemodilution on cerebral blood flow velocity in anesthetized patients. Anesth Analg 1998, 86: 320-324. 10.1097/00000539-199802000-00020
Rebel A, Ulatowski JA, Kwansa H, Bucci E, Koehler RC: Cerebrovascular response to decreased hematocrit: effect of cell-free hemoglobin, plasma viscosity, and CO 2 . Am J Physiol Heart Circ Physiol 2003, 285: H1600-1608.
van Bommel J, Trouwborst A, Schwarte L, Siegemund M, Ince C, Henny C: Intestinal and cerebral oxygenation during severe isovolemic hemodilution and subsequent hyperoxic ventilation in a pig model. Anesthesiology 2002, 97: 660-670. 10.1097/00000542-200209000-00021
Hudetz AG, Wood JD, Kampine JP: 7-Nitroindazole impedes erythrocyte flow response to isovolemic hemodilution in the cerebral capillary circulation. J Cereb Blood Flow Metab 2000, 20: 220-224. 10.1097/00004647-200002000-00002
Hudetz AG, Shen H, Kampine JP: Nitric oxide from neuronal NOS plays critical role in cerebral capillary flow response to hypoxia. Am J Physiol 1998, 274: H982-989.
Hare GMT, Mazer CD, Mak W, Gorczynski RM, Hum KM, Kim SY, Wyard L, Barr A, Qu R, Baker AJ: Hemodilutional anemia is associated with increased cerebral neuronal nitric oxide synthase gene expression. J Appl Physiol 2003, 94: 2058-2067.
Plochl W, Liam BL, Cook DJ, Orszulak TA: Cerebral response to hemodilution during cardiopulmonary bypass in dogs: the role of nitric oxide synthase. Br J Anaesth 1999, 82: 237-243.
Ulatwoski JA, Bucci E, Nishikawa T, Razynska A, Williams MA, Takeshima R, Traystman RJ, Koehler RC: Cerebral O2 transport with hematocrit reduced by cross-linked hemoglobin transfusion. Am J Physiol 1996, 270: H466-475.
Todd MM, Farrell S, Wu B: Cerebral blood flow during hypoxemia and hemodilution in rabbits: different roles for nitric oxide? J Cereb Blood Flow Metab 1997, 17: 1319-1325. 10.1097/00004647-199712000-00007
Hare GM, Worrall JM, Baker AJ, Liu E, Sikich N, Mazer CD: Beta2 adrenergic antagonist inhibits cerebral cortical oxygen delivery after severe hemodilution in rats. Br J Anaesth 2006, 97: 617-623. 10.1093/bja/ael238
McLaren AT, Marsden PA, Mazer CD, Baker AJ, Stewart DJ, Tsui AK, Li X, Yucel Y, Robb M, Boyd SR, Liu E, Yu J, Hare GM: Increased expression of HIF-1alpha, nNOS, and VEGF in the cerebral cortex of anemic rats. Am J Physiol Regul Integr Comp Physiol 2007, 292: R403-414.
Dexter F, Hindman BJ: Effect of haemoglobin concentration on brain oxygenation in focal stroke: a mathematical modeling study. Br J Anaesth 1997, 79: 346-351.
Todd MM, Wu B, Maktabi M, Hindman BJ, Warner DS: Cerebral blood flow and oxygen delivery during hypoxemia and anemia: The role of arterial oxygen content. Am J Phys 1994, 267: H2025-2031.
Korosue K, Heros RC: Mechanism of cerebral blood flow augmentation by hemodilution in rabbits. Stroke 1992, 23: 1487-1492.
Cole DJ, Drummond JC, Patel PM, Marcantonio S: Effects of viscosity and oxygen content on cerebral blood flow in ischemic and normal rat brain. J Neurol Sci 1994, 124: 15-20. 10.1016/0022-510X(94)90004-3
Tu YK, Kuo MF, Liu HM: Cerebral oxygen transport and metabolism during graded isovolemic hemodilution in experimental global ischemia. J Neurol Sci 1997, 150: 115-122. 10.1016/S0022-510X(97)00111-1
Todd MM, Wu B, Warner DS: The hemispheric cerebrovascular response to hemodilution is attenuated by a focal cryogenic brain injury. J Neurotrauma 1994, 11: 149-160. 10.1089/neu.1994.11.149
Weiskopf RB, Kramer JH, Viele M, Neumann M, Feiner JR, Watson JJ, Hopf HW, Toy P: Acute severe isovolemic anemia impairs cognitive function and memory in humans. Anesthesiology 2000, 92: 1646-1652. 10.1097/00000542-200006000-00023
Weiskopf RB, Toy P, Hopf HW, Feiner J, Finlay HE, Takahashi M, Bostrom A, Songster C, Aminoff MF: Acute isovolemic anemia impairs central processing as determined by P300 latency. Clin Neurophysiol 2005, 116: 1028-1032. 10.1016/j.clinph.2004.12.009
Ge YL, Lv R, Zhou W, Ma XX, Zhong TD, Duan ML: Brain damage following severe acute normovolemic hemodilution in combination with controlled hypotension in rats. Acta Anaesthesiol Scand 2007, 51: 1331-1337.
Lee LA, Deem S, Glenny RW, Townsend I, Moulding J, An D, Treggiari MM, Lam A: Effects of anemia and hypotension on porcine optic nerve blood flow and oxygen delivery. Anesthesiology 2008, 108: 864-872. 10.1097/ALN.0b013e31816c8a30
Czinn EA, Salem MR, Crystal GJ: Hemodilution impairs hypocapnia-induced vasoconstrictor responses in the brain and spinal cord in dogs. Anesth Analg 1995, 80: 492-498. 10.1097/00000539-199503000-00010
Tu YK, Liu HM: Effects of isovolemic hemodilution on hemodynamics, cerebral perfusion, and cerebral vascular reactivity. Stroke 1996, 27: 441-445.
Kuwabara Y, Sasaki M, Hirakata H, Koga H, Nakagawa M, Chen T, Kaneko K, Masuda K, Fujishima M: Cerebral blood flow and vasodilatory capacity in anemia secondary to chronic renal failure. Kidney Int 2002, 61: 564-569. 10.1046/j.1523-1755.2002.00142.x
Tinmouth A, Fergusson D, Yee IC, Hebert PC: ABLE Investigators; Canadian Critical Care Trials Group. Clinical consequences of red cell storage in the critically ill. Transfusion 2006, 46: 2014-2017. 10.1111/j.1537-2995.2006.01026.x
Berezina TL, Zaets SB, Morgan C, Spillert CR, Kamiyama M, Spolarics Z, Deitch EA, Machiedo GW: Influence of storage on red blood cell rheological properties. J Surg Res 2002, 102: 6-12. 10.1006/jsre.2001.6306
Tsai AG, Cabrales P, Intaglietta M: Microvascular perfusion upon exchange transfusion with stored red blood cells in normovolemic anemic conditions. Transfusion 2004, 44: 1626-1634. 10.1111/j.0041-1132.2004.04128.x
Heaton A, Keegan T, Holme S: In vivo regeneration of red cell 2,3-diphosphoglycerate following transfusion of DPG-depleted AS-1, AS-3 and CPDA-1 red cells. Br J Haematol 1989, 71: 131-136. 10.1111/j.1365-2141.1989.tb06286.x
Marik PE, Sibbald WJ: Effect of stored-blood transfusion on oxygen delivery in patients with sepsis. JAMA 1993, 269: 3024-3029. 10.1001/jama.269.23.3024
Walsh TS, McArdle F, McLellan SA, Maciver C, Maginnis M, Prescott RJ, McClelland DB: Does the storage time of transfused red blood cells influence regional or global indexes of tissue oxygenation in anemic critically ill patients? Crit Care Med 2004, 32: 364-371. 10.1097/01.CCM.0000108878.23703.E0
Suttner S, Piper SN, Kumle B, Lang K, Rohm KD, Isgro F, Boldt J: The influence of allogeneic red blood cell transfusion compared with 100% oxygen ventilation on systemic oxygen transport and skeletal muscle oxygen tension after cardiac surgery. Anesth Analg 2004, 99: 2-11. 10.1213/01.ANE.0000120163.44315.47
Gramm J, Smith S, Gamelli RL, Dries DJ: Effect of transfusion on oxygen transport in critically ill patients. Shock 1996, 5: 190-193. 10.1097/00024382-199603000-00004
Goldman M, Webert KE, Arnold DM, Freedman J, Hannon J, Blajchman MA: TRALI Consensus Panel. Transfus Med Rev 2005, 19: 2-31. 10.1016/j.tmrv.2004.10.001
Schorr AF, Duh MS, Kelly KM, Kollef MH: Red blood cell transfusion and ventilator-associated pneumonia: A potential link? Crit Care Med 2004, 32: 666-674. 10.1097/01.CCM.0000114810.30477.C3
Gunst MA, Minei JP: Transfusion of blood products and nosocomial infection in surgical patients. Curr Opin Crit Care 2007, 13: 428-432. 10.1097/MCC.0b013e32826385ef
Gong MN, Thompson BT, Williams P, Pothier L, Boyce PD, Christiani DC: Clinical predictors of and mortality in acute respiratory distress syndrome: potential role of red cell transfusion. Crit Care Med 2005, 33: 1191-1198. 10.1097/01.CCM.0000165566.82925.14
Silverboard H, Aisiku I, Martin GS, Adams M, Rozycki G, Moss M: The role of acute blood transfusion in the development of acute respiratory distress syndrome in patients with severe trauma. J Trauma 2005, 59: 717-723.
Hebert PC, Fergusson D, Blajchman MA, Wells GA, Kmetic A, Coyle D, Heddle N, Germain M, Goldman M, Toye B, Schweitzer I, vanWalraven C, Devine D, Sher GD: Clinical outcomes following institution of the Canadian universal leukoreduction program for red blood cell transfusions. JAMA 2003, 289: 1941-1949. 10.1001/jama.289.15.1941
Rigamonti A, McLaren AT, Mazer CD, Nix K, Ragoonanan T, Freedman J, Harringon A, Hare GM: Storage of strain-specific rat blood limits cerebral tissue oxygen delivery during acute fluid resuscitation. Br J Anaesth 2008, 100: 357-364. 10.1093/bja/aem401
Weiskopf RB, Kramer JH, Viele M, Neumann M, Feiner JR, Watson JJ, Hopf HW, Toy P: Acute severe isovolemic anemia impairs cognitive function and memory in humans. Anesthesiology 2000, 92: 1646-1652. 10.1097/00000542-200006000-00023
Kassell NF, Torner JC, Haley EC Jr, Jane JA, Adams HP, Kongable GL: The International Cooperative Study on the Timing of Aneurysm Surgery. Part 1: Overall management results. J Neurosurg 1990, 73: 18-36. 10.3171/jns.1990.73.1.0018
Dorsch NW, King MT: A review of cerebral vasospasm in aneurysmal subarachnoid hemorrhage. Part 1: Incidence and effects. J Clin Neurosci 1994, 1: 19-26. 10.1016/0967-5868(94)90005-1
Diringer MN, Yundt K, Videen TO, Adams RE, Zazulia AR, Deibert E, Aiyagari V, Dacey RG Jr, Grubb RL Jr, Powers WJ: No reduction in cerebral metabolism as a result of early moderate hyperventilation following severe traumatic brain injury. J Neurosurg 2000, 92: 7-13. 10.3171/jns.2000.92.1.0007
Menon DK: Brain ischemia after traumatic brain injury: lessons from 15O 2 positron emission tomography. Curr Opin Crit Care 2006, 12: 85-89. 10.1097/01.ccx.0000216572.19062.8f
Zazulia AR, Diringer MN, Videen TO, Adams RE, Yundt K, Aiyagari V, Grubb RL Jr, Powers WJ: Hypoperfusion without ischemia surrounding acute intracerebral hemorrhage. J Cereb Blood Flow Metab 2001, 21: 804-810. 10.1097/00004647-200107000-00005
Reeves BC, Murphy GJ: Increased mortality, morbidity, and cost associated with red blood cell transfusion after cardiac surgery. Curr Opin Cardiol 2008, 23: 607-612. 10.1097/HCO.0b013e328310fc95
Roach GW, Kanchuger M, Mangano CM, Neuman M, Nussmeier N, Wolman R, Aggarwal A, Marschall K, Graham SH, Ley C: Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med 1996, 335: 1857-1863. 10.1056/NEJM199612193352501
McKhann GM, Grega MA, Borowicz LM Jr, Baumgartner WA, Selnes OA: Stroke and encephalopathy after cardiac surgery: an update. Stroke 2006, 37: 562-671. 10.1161/01.STR.0000199032.78782.6c
Newmann MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA: Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med 2001, 344: 395-402. 10.1056/NEJM200102083440601
Van Dijk D, Jansen EW, Hijman R, Nierich AP, Diephuis JC, Moons KG, Lahpor JR, Borst C, Keizer AM, Nathoe HM, Grobbee DE, DeJaegere PP, Kalkman CJ: Cognitive outcome after off-pump and on-pump coronary artery bypass graft surgery: a randomized trial. JAMA 2002, 287: 1405-1412. 10.1001/jama.287.11.1405
Karkouti K, Wijeysundera DN, Beattie WS, Reducing Bleeding in Cardiac Surgery (RBC) Investigators: Risk associated with preoperative anemia in cardiac surgery: a multicenter cohort study. Circulation 2008, 117: 478-484. 10.1161/CIRCULATIONAHA.107.718353
Bell ML, Grunwald GK, Baltz JH, McDonald GO, Bell MR, Grover FL, Shroyer ALW: Does preoperative hemoglobin independently predict short-term outcome after coronary artery bypass graft surgery? Ann Thorac Surg 2008, 86: 1415-1423. 10.1016/j.athoracsur.2008.07.088
Karkouti K, Wijeysundera DN, Yau TM, McCluskey SA, van Rensvurg A, Beattie WS: The influence of baseline hemoglobin concentration on tolerance of anemia in cardiac surgery. Transfusion 2008, 48: 666-672. 10.1111/j.1537-2995.2007.01590.x
Chang YL, Tsai YF, Lin PJ, Chen MC, Liu CY: Prevalence and risk factors for post-operative delirium in a cardiovascular intensive care unit. Am J Crit Care 2008, 17: 567-575.
Kulier A, Levin J, Moser R, Rumpold-Seitlinger G, Tudor IC, Snyder-Ramos SA, Moehnle P, Mangano DT: Impact of preoperative anemia on outcome in patients undergoing coronary artery bypass graft surgery. Circulation 2007, 116: 471-479. 10.1161/CIRCULATIONAHA.106.653501
Matthew JP, Mackensen GB, Phillips-Bute B, Stafford-Smith M, Podgoreanu MV, Grocott HP, Hill SE, Smith PK, Blumenthal JA, Reves JG, Newman MF, for the Neruologic Outcome Research Group (NORG) of the Duke Heart Center: Effects of extreme hemodilution during cardiac surgery on cognitive function in the elderly. Anesthesiology 2007, 107: 577-584. 10.1097/01.anes.0000281896.07256.71
Cladellas M, Bruguera J, Cmoin J, Vila J, de Jaime E, Marti J, Gomez M: Is pre-operative anemia a risk marker for in-hospial mortality and morbidity after valve replacement? Eur Heart J 2006, 27: 1093-1099. 10.1093/eurheartj/ehi830
Giltay EJ, Huijskes RV, Kho KH, Blansjaar BA, Rosseel PM: Psychotic symptoms in patients undergoing coronary artery bypass grafting and heart valve operation. Eur J Cardiothorac Surg 2006, 30: 140-147. 10.1016/j.ejcts.2006.03.056
Karkouti K, Djaiani G, Borger MA, Beattie WS, Fedorko L, Wijeysundera D, Ivanov J, Karski J: Low hematocrit during cardiopulmonary bypass is associated with increaed risk of perioperative stroke in cardiac surgery. Ann Thorac Surg 2005, 80: 1381-1387. 10.1016/j.athoracsur.2005.03.137
Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah A: Adverse effects of low hematocrit during cardiopulmonary bypass in the adult: should current practice be changed. J Thorac Cardiovasc Surg 2003, 125: 1438-1450. 10.1016/S0022-5223(02)73291-1
DeFoe GR, Ross CS, Olmstead EM, Surgenor SD, Fillinger MP, Groom RC, Forest RJ, Pieroni JW, Warren CS, Bogosian ME, Krumholz CF, Clark C, Clough RA, Weldner PW, Lahey SJ, Leavitt BJ, Marrin CA, Charlesworth DC, Marshall P, O'Connor GT: Lowest hematocrit on bypass and adverse outcomes associated with coronary artery bypass grafting. Ann Thorac Surg 2001, 71: 769-776. 10.1016/S0003-4975(00)02393-6
van Wermeskerken GK, Lardenoye JW, Hill SE, Grocott HP, Phillips-Bute B, Smith PK, Reves JG, Newman MF: Intraoperative physiologic variables and outcome in cardiac surgery: Part II. Neurologic outcome. Ann Thorac Surg 2000, 69: 1077-1083. 10.1016/S0003-4975(99)01443-5
Klein AA, Nashef SA, Sharples L, Bottrill F, Dyer M, Armstrong J, Vuylsteke A: A randomized controlled trial of cell salvage in routine cardiac surgery. Anesth & Analg 2008, 107: 1487-1495. 10.1213/ane.0b013e3181831e54
Carless PA, Henry DA, Moxey AJ, O'Connell DL, Brown T, Fergusson DA: Cell salvage for minimizing perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 2006, 4: CD001888.
Society of Thoracic Surgoeons Blood Conservation Guideline Task Force, Ferraris VA, Ferraris SP, Saha SP, Hessel EA, Haan CK, Royston BD, Bridges CR, Higgins RS, Despotis G, Brown JR, Society of Cardiovascular Anesthesiologists Special Task Force on Blood Transfusion, Spiess BD, Shore-Lesserson L, Stafford-Smith M, Mazer CD, Bennett-Guerrero E, Hill SE, Body S: Perioperative blood transfusion and blood conservation in cardiac surgery: the Society of Thoracic Surgeons and The Society of Cardiovascular Anesthesiologists clinical practice guidelines. Ann Thorac Surg 2007, 83: S27-86. 10.1016/j.athoracsur.2007.02.099
Taneja R, Fernandes P, Marwaha G, Cheng D, Bainbridge D: Perioperative coagulation management and blood conservation in cardiac surgery: a Canadian Survey. J Cardiothorac Vasc Anesth 2008, 22: 662-669. 10.1053/j.jvca.2008.02.005
Tinmouth AT, McIntyre LA, Fowlder RA: Blood conservation strategies to reduce the need for red blood cell transfusion in critically ill patients. CMAJ 2008, 178: 49-57.
Jonas RA, Wypij D, Roth SJ, Bellinger DC, Visconti KJ, du Plessis AJ, Goodkin H, Laussen PC, Farrell DM, Bartlett J, McGrath E, Rappaport LJ, Bacha EA, Forbess JM, del Nido PJ, Mayer JE Jr, Newburger JW: The influence of hemodilution on outcome after hypothermic cardiopulmonary bypass: results of a randomized trial in infants. J Thorac Cardiovasc Surg 2003, 126: 1765-1774. 10.1016/j.jtcvs.2003.04.003
Newburger JW, Jonas RA, Soul J, Kussman BD, Bellinger DC, Laussen PC, Robertson R, Mayer JE Jr, del Nido PJ, Bacha EA, Forbess JM, Pigula F, Roth SJ, Visconti KJ, du Plessis AJ, Farrell DM, McGrath E, Rappaport LA, Wypij D: Randomized trial of hematocrit 25% versus 35% during hypothermic cardiopulmonary bypass in infant heart surgery. J Thorac Cardiovasc Surg 2008, 135: 347-354. 10.1016/j.jtcvs.2007.01.051
Wypij D, Jonas RA, Bellinger DC, Del Nido PJ, Mayer JE Jr, Bacha EA, Forbess JM, Pigula F, Laussen PC, Newburger JW: The effect of hematocrit during hypothermic cardiopulmonary bypass in infant heart surgery: results from the combined Boston hematocrit trials. J Thorac Cardiovasc Surg 2008, 135: 355-360. 10.1016/j.jtcvs.2007.03.067
Brevig J, McDonald J, Zelinka ES, Gallagher T, Jin R, Grunemeier GL: Blood transfusion reduction in cardiac surgery: multidisciplinary approach at a community hospital. Ann Thorac Surg 2009, 87: 532-539. 10.1016/j.athoracsur.2008.10.044
Ngaage DL, Cowen ME, Griffin S, Guvendik L, Cale AR: Early neurological complications after coronary artery bypass grafting and valve surgery in octogenarians. Eur J Cardiothorac Surg 2008, 33: 653-659. 10.1016/j.ejcts.2008.01.017
Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD: Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation 2007, 116: 2544-2552. 10.1161/CIRCULATIONAHA.107.698977
Whitson BA, Huddleston SJ, Savik K, Shumway SJ: Bloodless cardiac surgery is associated with decreased morbidity and mortality. J Card Surg 2007, 22: 373-378. 10.1111/j.1540-8191.2007.00428.x
Norkiene I, Ringaitiene D, Misiureiene I, Samalavicuius R, Bubulis R, Baublys A, Uzdavinys G: Incidence and precipitating factors of delirium after coronary artery bypass grafting. Scadn Cardiovasc J 2007, 41: 180-185. 10.1080/14017430701302490
Koch CG, Li L, Duncan AI, Mihaljevic T, Cosgrove DM, Loop "FD, Starr NJ, Blackstone EH: Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 2006, 34: 1608-1616. 10.1097/01.CCM.0000217920.48559.D8
Stamou SC, White T, Barnett S, Boyce SW, Corso PJ, Lefrak EA: Comparisons of cardiac surgery outcomes in Jehovah's versus non-Jehovah's witnesses. Am J Cardiol 2006, 98: 1223-1225. 10.1016/j.amjcard.2006.05.055
Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Onnasch JF, Metz S, Falk V, Mohrt FW: Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg 2003, 75: 472-478. 10.1016/S0003-4975(02)04370-9
D'Ancona G, Saez de Ibarra JI, Baillot R, Mathieu P, Doyle D, Metras J, Desaulniers D, Dagenais F: Determinants of stroke after coronary artery bypass grafting. Eur J Cardiothorac Surg 2003, 24: 552-556. 10.1016/S1010-7940(03)00440-8
Koch CG, Li L, Sessler DI, Figueroa P, Hoeltge GA, Mihaljevic T, Blackstone EH: Duration of red-cell storage and complications after cardiac surgery. N Engl J Med 2008, 358: 1229-1239. 10.1056/NEJMoa070403
Graham DI, Ford I, Adams JH, Doyle D, Teasdale GM, Lawrence AE, McLellan DR: Ischemic brain damage is still common in fatal non-missile head injury. J Neurol Neurosurg Psychiatry 1989, 52: 346-350. 10.1136/jnnp.52.3.346
Bouma GJ, Muizelaar JP, Stringer WA, Choi SC, Fatouros P, Young HF: Ultra-early evaluation of reiongal cerebral blood flow in severely head-injured patients using xenon-enhanced computerized tomography. J Neurosurg 1992, 77: 360-368. 10.3171/jns.1992.77.3.0360
Marion DW, Darby J, Yonas H: Acute regional cerebral blood flow changes caused by severe head injuries. J Neurosurg 1991, 74: 407-414. 10.3171/jns.1991.74.3.0407
Gopinath SP, Robertson CS, Contant CF, Hayes C, Feldman Z, Narayan RK, Grossman RG: Jugular venous desaturation and outcome after head injury. J Neurol Neurosurg Psychiatry 1994, 57: 717-723. 10.1136/jnnp.57.6.717
Van Santbrink H, Maas AI, Avezaat CJ: Continuous monitoring of partial pressure of brain tissue oxygen in patients with severe head injury. Neurosurgery 1996, 38: 21-31. 10.1097/00006123-199601000-00007
Valadka AB, Gopinath SP, Contant CF, Uzura M, Robertson CS: Relationship of brain tissue PO2 to outcome after severe head injury. Crit Care Med 1998, 26: 1576-1581. 10.1097/00003246-199809000-00029
Brink WA, van Santbrink H, Steyerberg EW, Avezaat CJ, Suazo JA, Hogesteeger C, Jansen WJ, Koos LM, Vermeulen J, Maas AI: Brain oxygen tension in severe head injury. Neurosurgery 2000, 46: 868-876. 10.1097/00006123-200004000-00018
Diringer MN, Videen TO, Yundt K, Zazulia AR, Aiyagari V, Dacey RG Jr, Grubb RL, Powers WJ: Regional cerebrovascular and metabolic effects of hyperventilation after severe traumatic brain injury. J Neurosurg 2002, 96: 103-108. 10.3171/jns.2002.96.1.0103
Coles JP: Regional ischemia after head injury. Curr Opin Crit Care 2004, 10: 120-125. 10.1097/00075198-200404000-00008
Abate MG, Trivedi M, Fryer TD, Smielewski P, Chatfield DA, Williams GB, Aigbirhio F, Carpenter TA, Pickard JD, Menon DK, Coles JP: Early derangements in oxygen and glucose metabolism following head injury: the ischemic penumbra and pathophysiological heterogeneity. Neurocrit Care 2008, 9: 319-325. 10.1007/s12028-008-9119-2
Nortje J, Coles JP, Timofeev I, Fryer TD, Aigbirhio FI, Smielewsi P, Outtrim JG, Chatfield DA, Pichard JD, Hutchinson PJ, Gupta AK, Menon DK: Effect of hyperoxia on regional oxygenation and metabolism after severe traumatic brain injury: preliminary findings. Crit Care Med 2008, 36: 273-281. 10.1097/01.CCM.0000292014.60835.15
Hare GM, Mazer CD, Hutchison JS, McLaren AT, Liu E, Rassouli A, Ai J, Shaye RE, Lockwood JA, Hawkins CE, Sikich N, To K, Baker AJ: Severe hemodilutional anemia increases cerebral tissue injury following acute neurotrauma. J Appl Physiol 2007, 103: 1021-1029. 10.1152/japplphysiol.01315.2006
Smith MJ, Stiefel MF, Magge S, Frangos S, Bloom S, Gracias V, Le Roux PD: Packed red blood cell transfusion increases local cerebral oxygenation. Crit Care Med 2005, 33: 1104-1108. 10.1097/01.CCM.0000162685.60609.49
Leal-Noval SR, Rincon-Ferrari MD, Marin-Niebla A, Cayuela A, Arellano-Orden V, Marin-Caballos A, Amaya-Villar R, Ferrandiz-Millon C, Murillo-Cabeza F: Transfusion of erythrocyte concentrates produces a variable increment on cerebral oxygenation in patients with severe traumatic brain injury: a preliminary study. Intensive Care Med 2006, 32: 1733-1740. 10.1007/s00134-006-0376-2
Leal-Noval SR, Munoz-Gomez M, Aerllano-Orden V, Marin-Caballos A, Amaya-Villar R, Marin A, Puppo-Moreno A, Ferrandiz-Millon C, Flores-Cordero JM, Murillo-Cabezas F: Impact of age of transfused blood on cerebral oxygenation in male patients with severe traumatic brain injury. Crit Care Med 2008, 36: 1290-1296. 10.1097/CCM.0b013e3181692dfc
Zygun D, Nortje J, Hutchinson PJ, Timofeev I, Menon DK, Gupta AK: Effect of red blood cell transfusion on cerebral oxygenation and metaoblism following severe trauamtic brain injury. Crit Care Med 2009, 37: 1074-1078. 10.1097/CCM.0b013e318194ad22
Carlson AP, Schermer CR, Lu SW: Retrospective evaluation of anemia and transfusion in traumatic brain injury. J Trauma 2006, 61: 46-56. 10.1097/01.ta.0000231768.44727.a2
Steyerberg EW, Mushkuidani N, Perel P, Butcher I, Lu J, McHugh GS, Murray GD, Marmarou A, Robets I, Habbema JDF, Maas AIR: Predicting outcome after traumatic brain injury: development and validation of international validation of prognostic scores based on admission characteristics. PLoS Med 2008, 5: 1251-1261. 10.1371/journal.pmed.0050165
Duane TM, Mayglothling J, Grandhi R, Warrier N, Aboutanos MB, Wolfe LG, Malhotra AK, Ivatury RR: The effect of anemia and blood transfusions on mortality in closed head injury patients. J Surg Res 2008, 147: 163-167. 10.1016/j.jss.2008.02.044
Salim A, Hadjizacharia P, DuBose J, Brown C, Inaba K, Chan L, Margulies DR: Role of anemia in traumatic brain injury. J Am Coll Surg 2008, 207: 398-406. 10.1016/j.jamcollsurg.2008.03.013
George ME, Skarda DE, Watts CR, Pham HD, Beilman GJ: Aggressive red blood cell transfusion: no association with improved outcomes for victims of isolated traumatic brain injury. NeuroCrit Care 2008, 8: 337-343. 10.1007/s12028-008-9066-y
Van Beek JGM, Mushkudiani NA, Steyerberg EW, Butcher I, McHugh GS, Lu J, Marmarou A, Murrary GD, Maas AIR: Prognostic value of admission laboratory parameters in traumatic brain injury: results from the IMPACT Study. J Neurotrauma 2007, 24: 315-328. 10.1089/neu.2006.0034
Schirmer-Makalsen K, Vik A, Gisvold SE, Skandsen T, Hynne H, Klepstad P: Severe head injury: control of physiological variables, organ failure and complications in the intensive care unit. Acta Anaesthesiol Scand 2007, 51: 1194-1201.
McIntyre LA, Fergusson DA, Hutchison JS, Pagliarello G, Marshall JC, Yetisir E, Hare GM, Hébert PC: Effect of a liberal versus restrictive transfusion strategy on mortality in patients with moderate to severe head injury. NeuroCrit Care 2006, 5: 4-9. 10.1385/NCC:5:1:4
Robertson CS, Gopinath SP, Goodman JC, Contant CF, Valadka AB, Narayan RK: SjvO2 monitoring in head-injured patients. J Neurotrauma 1995, 12: 891-896. 10.1089/neu.1995.12.891
Bendel P, Koivisto T, Kononen M, Hanninen T, Huarskainen H, Saari T, Vapalahti M, Hernesniemi J, Vanninen R: MR imaging of the brain 1 year after aneurysmal subarachnoid hemorrhage: randomized study comparing surgical with endovascular treatment. Radiology 2008, 246: 543-552. 10.1148/radiol.2461061915
Shimoda M, Takeuchi M, Tominaga J, Oda S, Kumasaka A, Tsugane R: Asymptomatic versus symptomatic infarcts from vasospasm in patients with subarachnoid hemorrhage: serial magnetic resonance imaging. Neurosurgery 2001, 49: 1341-1348. 10.1097/00006123-200112000-00010
Kramer AH, Zygun DA, Bleck TP, Dumont AS, Kassell NF, Nathan B: Relationship between hemoglobin concentrations and outcomes across subgroups of patients with aneurysmal subarachnoid hemorrhage. NeuroCrit Care 2009, 10: 20-27. 10.1007/s12028-008-9137-0
Naidech AM, Drescher J, Ault ML, Shaibani A, Batjer HH, Alberts MJ: Higher hemoglobin is associated with less cerebral infarction, poor outcome, and death after subarachnoid hemorrhage. Neurosurgery 2006, 59: 775-779. 10.1227/01.NEU.0000232662.86771.A9
Naidech AM, Jovanovic B, Wartenberg KE, Parra A, Ostapkovich N, Connolly ES, Mayer SA, Commichau C: Higher hemoglobin is associated with improved outcome after subarachnoid hemorrhage. Crit Care Med 2007, 35: 2383-2389. 10.1097/01.CCM.0000284516.17580.2C
Tseng MY, Hutchinson PJ, Kirkpatrick PJ: Effects of fluid therapy following aneurismal subarachnoid hemorrhage: a prospective clinical study. Br J Neurosurg 2008, 22: 257-268. 10.1080/02688690701832100
Wartenberg KE, Schmidt JM, Claassen J, Temes RE, Frontera JA, Ostapkovich N, Parra A, Connolly ES, Mayer SA: Impact of medical complications on outcome after subarachnoid hemorrhage. Crit Care Med 2006, 34: 617-623. 10.1097/00003246-200612002-00426
DeGeorgia M, Deogaonkar A, Ondrejka J, Katzan I, Sabharwal V, Woo HH, Rasmussen P, Chow M, Mayberg M: Blood transfusionfollowing subarachnoid hemorrhage worsens outcome.[http://www.abstractonline.com/arch/RecordView.aspx?LookupKey=12345recordID=11885]
Smith MJ, Le Roux PD, Elliott JP, Winn HR: Blood transfusion and increased risk for vasospasm and poor outcome after subarachnoid hemorrhage. J Neurosurg 2004, 101: 1-7. 10.3171/jns.2004.101.1.0001
Sen J, Belli A, Albon H, Morgan L, Petzold A, Kitchen N: Triple-H therapy in the management of aneurysmal subarachnoid hemorrhage. Lancet Neurol 2003, 2: 614-621. 10.1016/S1474-4422(03)00531-3
Ekelund A, Reinstrup P, Ryding E, Andersson AM, Molund T, Kristiansson KA, Romner B, Brandt L, Saveland H: Effects of iso- and hypervolemic hemodilution on regional cerebral blood flow and oxygen delivery for patients with vasospasm after aneurysmal subarachnoid hemorrhage. Acta Neurochir 2002, 144: 703-712. 10.1007/s00701-002-0959-9
Muench E, Horn P, Bauhuf C, Roth H, Philipps M, Hermann P, Quintel M, Schmiedek P, Vajkoczy P: Effects of hypervolemia and hypertension on regional cerebral blood flow, intracranial pressure, and brain tissue oxygenation after subarachnoid hemorrhage. Crit Care Med 2007, 35: 1844-1851. 10.1097/01.CCM.0000275392.08410.DD
Dhar R, Zazulia A, Videen T, Diringer M: Red blood cell transfusion increases cerebral oxygen delivery after subarachnoid hemorrhage. NeuroCrit Care 2008, 9: S5.
Oddo M, Milby A, Chen I, Frangos S, Maloney-Wilensky E, Stiefel M, Kofke WA, Levine JM, Le Roux PD: Hemoglobin level and cerebral metabolism in patients with aneurysmal subarachnoid hemorrhage: a microdialysis study. Stroke 2009, 40: 1275-1281. 10.1161/STROKEAHA.108.527911
Grotta J, Ackerman R, Correia J, Fallick G, Chang J: Whole blood viscosity parameters and cerebral blood flow. Stroke 1982, 13: 296-301.
Tohgi H, Yamanouchi H, Murakami M, Kameyama M: Importance of the hematocrit as a risk factor in cerebral infarction. Stroke 1978, 9: 369-374.
Roh JK, Kang DW, Lee SH, Yoon BW, Chang KH: Significance of acute multiple brain infarction on diffusion-weighted imaging. Stroke 2000, 31: 688-694.
Arauz A, Murillo L, Cantu C, Barinagarrementeria F, Higuera J: Prospective study of single and multiple lacunar infarcts using magnetic resonance imaging: risk factors, recurrence, and outcome in 175 consecutive cases. Stroke 2003, 34: 2453-2458. 10.1161/01.STR.0000090351.41662.91
Longo-Mbenza B, Lelo Tshinkwela M, Mbuilu Pukuta J: Rates and predictors of stroke-associated case fatality in black Central African patients. Cardiovasc J Afr 2008, 19: 72-76.
Kannel WB, Gordon T, Wolf PA, McNamara P: Hemoglobin and the risk of cerebral infarction: the Framingham study. Stroke 1972, 3: 409-420.
Gagnon DR, Zhang TJ, Brand FN, Kannel WB: Hematocrit and the risk of cardiovascular disease – the Framingham study: a 34 year follow-up. Am Heart J 1994, 127: 674-682. 10.1016/0002-8703(94)90679-3
Wannamethee G, Perry IJ, Shaper AG: Hematocrit, hypertension and risk of stroke. J Intern Med 1994, 235: 163-168.
Sacco S, Marini C, Olivieri L, Pistoia F, Carolei A: Contribution of hematocrit to early mortality after ischemic stroke. Eur Neurol 2007, 58: 233-238. 10.1159/000107946
Diamond PT, Gale SD, Evans BA: Relationship of initial hematocrit level to discharge destination and resource utilization after ischemic stroke: a pilot study. Arch Phys Med Rehabil 2003, 84: 964-967. 10.1016/S0003-9993(03)00009-1
Harrison MJ, Pollock S, Kendall BE, Marshall J: Effect of hematocrit on carotid stenosis and cerebral infarction. Lancet 1981, 2: 114-115. 10.1016/S0140-6736(81)90298-1
Lowe GDO, Jaap AJ, Forbes CD: Relation of atrial fibrillation and high hematocrit to mortality in acute stroke. Lancet 1983, 1: 784-786. 10.1016/S0140-6736(83)91848-2
Allport LE, Parsons MW, Butcher KS, MacGregor L, Desmond PM, Tress BM, Davis SM: Elevated hematocrit is associated with reduced reperfusion and tissue survival in acute stroke. Neurology 2005, 65: 1382-1387. 10.1212/01.wnl.0000183057.96792.a8
Huang WY, Chen IC, Meng L, Weng WC, Peng TI: The influence of anemia on clinical presentation and outcome of patients with first-ever atherosclerosis-related ischemic stroke. J Clin Neurosci 2009, 16: 645-649. 10.1016/j.jocn.2008.08.014
Huang WY, Weng WC, Chien YY, Wu CL, Peng TI, Chen KH: Predictive factors of outcome and stroke recurrence in patients with unilateral atherosclerosis-related internal carotid artery occlusion. Neurol India 2008, 56: 173-178. 10.4103/0028-3886.41996
Nybo M, Kristensen SR, Mickley H, Jensen JK: The influence of anemia on stroke prognosis and its relation to N-terminal pro-brain natriuretic peptide. Eur J Neurol 2007, 14: 477-482. 10.1111/j.1468-1331.2006.01591.x
Bhatia RS, Garg RK, Gaur SPS, Kar AM, Shukla R, Agarwal A, Verma R: Predictive value of routine hematological and biochemical parameters on 30-day fatality in acute stroke. Neurol India 2004, 52: 220-223.
Wade JP, Taylor DW, Barnett HJ, Hachinksi VC: Hemoglobin concentration and prognosis in symptomatic obstructive cerebrovascular disease. Stroke 1987, 18: 68-71.
LaRue L, Alter M, Lai SM, Friday G, Sobel E, Levitt L, McCoy R, Isack T: Acute stroke, hematocrit, and blood pressure. Stroke 1987, 18: 565-569.
Kusonoki M, Kimura K, Nakamura M, Isaka Y, Yoneda S, Abe H: Effects of hematocrit variations on cerebral blood flow and oxygen transport in ischemic cerebrovascular disease. J Cereb Blood Flow Metab 1981, 1: 413-417.
Xiong L, Lei C, Wang Q, Li W: Acute normovolemic hemodilution with a novel hydroxyethylstarch (130/0.4) reduces focal cerebral ischemic injury in rats. Eur J Anaesthesiol 2008, 25: 581-588. 10.1017/S0265021508004067
Lee SH, Heros RC, Mullan JC, Korosue K: Optimum degree of hemodilution for brain protection in a canine model of focal cerebral ischemia. J Neurosurg 1994, 80: 469-475. 10.3171/jns.1994.80.3.0469
Reasoner DK, Ryu KH, Hindman BJ, Cutkomb J, Smith T: Marked hemodilution increases neurologic injury after focal cerebral ischemia in rabbits. Anesth Analg 1996, 82: 61-67. 10.1097/00000539-199601000-00011
Kim JS, Kang SY: Bleeding and subsequent anemia: a precipitant for cerebral infarction. Eur Neurol 2000, 43: 201-208. 10.1159/000008176
Bosel J, Ruscher K, Ploner CJ, Valdueza JM: Delayed neurological deterioration in a stroke patients with postoperative acute anemia. Eur Neurol 2005, 53: 36-38. 10.1159/000084261
Shahar A, Sadeh M: Severe anemia associated with transient neurological deficits. Stroke 1991, 22: 1201-1202.
Asplund K: Hemodilution for acute ischemic stroke. Cochrane Database Syst Rev 2002, 2: CD000103.
Italian Acute Stroke Study Group: Hemodilution in acute stroke: results from the Italian Hemodilution Trial. Lancet 1998, 13: 318-321.
Scandinavian Stroke Study Group: Multicenter trial of hemodilution in acute ischemic stroke: I. Results in the toal patient population. Stroke 1987, 18: 691-699.
Goslinga H, Eijzenbach V, Heuvelmans JH, Laan de Vries E, Melis VM, Schmid-Schoenbein H, Bezemer PD: Custom-tailored hemodilution with albumin and crystalloids in acute ischemic stroke. Stroke 1992, 23: 181-188.
Aichner FT, Fazekas F, Brainin M, Polz W, Mamoli B, Zeiler K: Hypervolemic hemodilution in acute ischemic stroke: the Multicenter Austrian Hemodilution Stroke Trial (MAHST). Stroke 1998, 29: 743-749.
Belayev L, Busto R, Zhao W, Clemens JA, Ginsberg MD: Effect of delayed albumin hemodilution on infarction volume and brain edema after transient middle cerebral artery occlusion in rats. J Neurosurg 1997, 87: 595-601. 10.3171/jns.1997.87.4.0595
Palesch YY, Hill MD, Ryckborst KJ, Tamariz D, Ginsberg MD: The ALIAS Pilot Trial: a dose-escalation and safety study of albumin therapy for acute ischemic stroke – II: neurologic outcome and efficacy analysis. Stroke 2006, 37: 2107-2114. 10.1161/01.STR.0000231389.34701.b5
Ginsberg MD, Hill MD, Palesch YY, Ryckborst KJ, Tamariz D: The ALIAS Pilot Trial: a dose-escalation and safety study of albumin therapy for acute ischemic stroke – I: physiological responses and safety results. Stroke 2006, 37: 2100-2106. 10.1161/01.STR.0000231388.72646.05
Shin DH, Moon GJ, Bang OY: Albumin therapy in acute stroke patients. J Neurol 2007, 254: 870-878. 10.1007/s00415-006-0456-9
Mayer SA, Rincon F: Management of intracerebral hemorrhage. Lancet Neurol 2005, 4: 662-672. 10.1016/S1474-4422(05)70195-2
Mendelow AD: Mechanisms of ischemic damage with intracerebral hemorrhage. Stroke 1993, 24: 115-119.
Siddique MS, Fernandes HM, Wooldridge TD, Fenwick JD, Slomka P, Mendelow AD: Reversible ischemia around intracerebral hemorrhage: a single-photon emission computerized tomography study. J Neurosurg 2002, 96: 736-741. 10.3171/jns.2002.96.4.0736
Schellinger PD, Fiebach JB, Hoffmann K, Becker K, Orakcioglu B, Kollmar R, Juttler E, Schramm P, Schwab S, Sartor K, Hacke W: Stroke MRI in intracerebral hemorrhage: is there a perihemorrhagic penumbra? Stroke 2003, 34: 1674-1679. 10.1161/01.STR.0000076010.10696.55
Rosand J, Eskey C, Chang Y, Gonzalez RG, Greenberg SM, Koroshetz WJ: Dynamic single-section CT demonstrates reduced cerebral blood flow in acute intracerebral hemorrhage. Cerebrovasc Dis 2002, 14: 214-220. 10.1159/000065681
Herweh C, Juttler E, Schellinger PD, Klotz E, Jenetzky E, Orakcioglu B, Sartor K, Schramm P: Evidence against a perihemorrhagic penumbra provided by perfusion computed tomography. Stroke 2007, 38: 2941-2947. 10.1161/STROKEAHA.107.486977
Nilsson OG, Polito A, Saveland H, Ungerstedt U, Norstrom CH: Are the primary supratentorial intracerebral hemorrhages surrounded by a biochemical penumbra? A microdialysis study. Neurosurgery 2006, 59: 521-528. 10.1227/01.NEU.0000227521.58701.E5
Aronowski J, Strong R, Grotta JC: Combined neuroprotection and reperfusion therapy for stroke. Effect of lubeluzole and diaspirin cross-linked hemoglobin in experimental focal ischemia. Stroke 1996, 27: 1571-1576.
Bowes MP, Burhop KE, Zivin JA: Diaspirin cross-linked hemoglobin improves neurological outcome following reversible but not irreversible CNS ischemia in rabbits. Stroke 1994, 25: 2253-2257.
Cole DJ, Drummon JC, Patel PM, Reynolds LR: Hypervolemic-hemodilution during cerebral ischemia in rat: effects of diaspirin cross-linked hemoglobin (DCLHb) on neurological outcome and infarct volume. J Neurosurg Anesthesiol 1997, 9: 44-50. 10.1097/00008506-199701000-00011
Mito T, Nemoto M, Kwansa H, Samepi K, Habeeb M, Murphy SJ, Bucci E, Koehler RC: Decreased damage from transient focal cerebral ischemia by transfusion of zero-link hemoglobin polymers in mouse. Stroke 2009, 40: 278-284. 10.1161/STROKEAHA.108.526731
Nemoto M, Mito T, Brinigar WS, Fronticelli C, Koehler RC: Salvage of focal cerebral ischemic damage by transfusion of high O 2 -affinity recombinant hemoglobin polymers in mouse. J Appl Physiol 2006, 100: 1688-1691. 10.1152/japplphysiol.01374.2005
Piper IR, Garrioch MA, Souter MJ, Andrews PJ, Thomson D: Effects of diaspirin cross-linked hemoglobin on post-traumatic cerebral persuion pressure and blood flow in a rodent model of diffuse brain injury. Br J Anaesth 1998, 80: 639-643.
Gibson JB, Maxwell RA, Schwiezter JB, Fabian TC, Proctor KG: Resuscitation from severe hemorrhagic shock after tramatic brain injury using saline, shed blood, or a blood substitute. Shock 2002, 17: 234-244. 10.1097/00024382-200203000-00013
Chappell JE, Shackford SR, McBride WJ: Effect of hemodilution with diaspirin cross-linked hemoglobin on intracranial pressure, cerebral perfusion pressure, and fluid reuirements after head injury and shock. J Neurosurg 1997, 86: 131-138. 10.3171/jns.1997.86.1.0131
Dudkiewicz M, Harpaul TA, Proctor KG: Hemoglobin-based oxygen carrying compound-201 as salvage therapy for severe neuro-and polytrauma (Injury Severity Score = 27–41). Crit Care Med 2008, 36: 2838-2848. 10.1097/CCM.0b013e318186f6b3
Stern S, Rice J, Philbin N, McGwin G, Arnaud F, Johnson T, Flournoy WS, Ahlers S, Pearce LB, McCarron R, Freilich D: Resuscitation with the hemoglobin-based oxygen carrier, HOBC-201, in a swine model of severe uncontrolled hemorrhage and traumatic brain injury. Shock 2009, 31: 64-79. 10.1097/SHK.0b013e3181778dc3
Rosenthal G, Morabito D, Cohen M, Roeytenberg A, Derugin N, Panter SS, Knodson MM, Maley G: Use of hemoglobin-based oxygen-carrying solution-201 to improve resuscitation parameters and prevent secondary brain injury in a swine model of traumatic brain injury and hemorrhage; laboratory investigation. J Neurosurg 2008, 108: 575-587. 10.3171/JNS/2008/108/3/0575
Kerby JD, Sainz JG, Zhang F, Hutchings A, Sprague S, Farrokhi FR, Son M: Resuscitation from hemorrhagic shock with HOBC-201 in the setting of traumatic brain injury. Shock 2007, 27: 652-656. 10.1097/01.shk.0000248584.10400.dc
Cole DJ, Reynolds LW, Nary JC, Drummond JC, Patel PM, Jacobsern WK: Subarachnoid hemorrhage in rats: effect of singular or sustained hemodilution with alpha-alpha diaspirin crosslinked hemoglobin on cerebral hypoperfusion. Crit Care Med 1999, 27: 972-977. 10.1097/00003246-199905000-00038
Cole DJ, Nary JC, Reynolds LW, Patel PM, Drummond JC: Experimental subarachnoid hemorrhage in rats: effect of intravenous alpha-alpha diaspitin crosslinked hemoglobin on hypoperfusion and neuronal death. Anesthesiology 1997, 87: 1486-1493. 10.1097/00000542-199712000-00028
Rother RP, Bell L, Hillmen P, Gladwin MT: The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin: a novel mechanism of human disease. JAMA 2005, 293: 1653-1662. 10.1001/jama.293.13.1653
Natanson C, Kern SJ, Lurie P, Banks SM, Wolfe SM: Cell-free hemoglobin-based blood substitutes and risk of myocardial infarction and death. JAMA 2008, 299: 2304-2312. 10.1001/jama.299.19.jrv80007
Saxena R, Wihnhoud AD, Carton H, Hacke W, Kaste M, Przybelski RJ, Stern KN, Koudstaal PJ: Controlled safety study of a hemoglobin-based oxygen carrier, DCLHb, in acute ischemic stroke. Stroke 1999, 30: 993-996.
Kerner T, Ahlers O, Veit S, Riou B, Saunders M, Pison U, for the European DCLHb Trauma Study Group: DCL-Hb for trauma patients with severe hemorrhagic shock: the European "On-Scene" Multicenter Study. Intensive Care Med 2003, 29: 378-385.
Sloan EP, Koenigsberg M, Gens D, Cipolle M, Runge J, Mallory MN, Rodman G, for the DCLHb Traumatic Hemorrhagic Shock Study Group: Diaspirin cross-linked hemoglobin (DCLHb) in the treatment of severe traumatic hemorrhagic shock: a randomized controlled efficacy trial. JAMA 1999, 282: 1857-1864. 10.1001/jama.282.19.1857
Gould SA, Moore EE, Hoyt DB, Burch JM, Haenel JB, Garcia J, DeWoskin R, Moss GS: The first randomized trial of human polymerized hemoglobin as a blood substitute in acute trauma and emergent surgery. J Am Coll Surg 1998, 187: 113-120. 10.1016/S1072-7515(98)00095-7
Przybelski RJ, Daily EK, Micheels J, Sloan E, Mols P, Corne L, Koenigerg MD, Bickell WH, Thompson DR, Harviel JD, Cohn SM: A safety assessment of diaspirin cross-linked hemoglobin (DCLHb) in the treatment of hemorrhagic, hypovolemic shock. Prehosp Disaster Med 1999, 14: 251-264.
Moore EE, Moore FA, Fabian TC, Bernard AC, Fulda GJ, Hoyt DB, Duane TM, Weireter LJ, Gomez GA, Ciplle MD, Rodman GH, Malangoni MA, Hides GA, Omert LA, Gould SA: Human polymerized hemoglobin for the treatment of hemorrhagic shock when blood is unavailable: the USA multicenter trial. J Am Coll Surg 2009, 208: 1-13. 10.1016/j.jamcollsurg.2008.09.023
Lamy ML, Daily EK, Brichant JF, Larbuisson RP, Demeyere RH, Vandermeersch EA, Lehot JJ, Parsloe MR, Berridge JC, Sinclair CJ, Baron JF, Przybelski RJ, for the DCLHb Cardiac Surgery Trial Collaborative Group: Randomized trial of diaspirin cross-linked hemoglobin solution as an alternative to blood transfusion after cardiac surgery. Anesthesiology 2000, 92: 646-656. 10.1097/00000542-200003000-00007
Hill SE, Gottshcalk LI, Grichnik K: Safety and preliminary efficacy of hemoglobin raffimer for patients undergoing coronary artery bypass surgery. J Cardiothorac Vasc Anesth 2002, 16: 695-702. 10.1053/jcan.2002.128416
Lindsay P, Bayley M, Hellings C, Hill M, Woddbury E, Phillips S: Canadian best practice recommendations for stroke care (updated 2008). CMAJ 2008, 179: S1-25.
Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks EF, American Heart Association; American Stroke Association Stroke Council; Clinical Cardiology Council; Cardiovascular Radiology and Intervention Council; Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke 2007, 38: 1655-1711. 10.1161/STROKEAHA.107.181486
Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons: Guidelines for the management of severe traumatic brain injury. J Neurotrauma 2007, 24: S1-106. 10.1089/neu.2006.0209
Bederson JB, Connolly ES, Batjer HH, Dacey RG, Dion JE, Diringer MN, Duldner JE, Harbaugh RE, Patel AB, Rosenwasser RH: Guidelines for the management of aneurysmal subarachnoid hemorrhage. Stroke 2009, 40: 994-1025. 10.1161/STROKEAHA.108.191395
Broderick J, Connolly S, Feldmann E, Hanley D, Kase C, Krieger D, Mayberg M, Morgenstern L, Ogilvy CS, Vespa P, Zuccarello M, American Stroke Association Stroke Council; High Blood Pressure Research Council; Quality of Care and Outcomes in Research Interdisciplinary Working Group: Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Stroke 2007, 38: 2001-2023. 10.1161/STROKEAHA.107.183689
Chang JJ, Youn TS, Benson D, Mattick H, Andrade BA, Harper MS, Moore CB, Madden CJ, Diaz-Arrastia RR: Physiologic and functional outcome correlates of brain tissue hypoxia in traumatic brain injury. Crit Care Med 2009, 37: 283-290. 10.1097/CCM.0b013e318192fbd7
Naidech AM, Bendok BR, Ault ML, Bleck TP: Monitoring with the Somanetics INVOS 5100C after aneurysmal subarachnoid hemorrhage. Neurocrit Care 2008, 9: 326-331. 10.1007/s12028-008-9077-8
Sahuquillo J, Poca MA, Garnacho A, Robles A, Coello F, Godet C, Triginer C, Rubio E: Early ischemia after severe head injury. Preliminary results in patients with diffuse brain injuries. Acta Neurochir 1993, 122: 204-214. 10.1007/BF01405530
Cruz J, Jaggi JL, Hoffstad OJ: Cerebral blood flow and oxygen consumption in acute brain injury with acute anemia: an alternative for the cerebral metabolic rate of oxygen consumption? Crit Care Med 1993, 21: 1218-1224.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AHK was responsible for the conception and design of the study, the analysis and interpretation of the data, and the drafting and revision of the manuscript. DAZ was responsible for the analysis and interpretation of data, and the revision of the manuscript. Both authors approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kramer, A.H., Zygun, D.A. Anemia and red blood cell transfusion in neurocritical care. Crit Care 13, R89 (2009). https://doi.org/10.1186/cc7916
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc7916