Abstract
Background
Little is known about the development of acute lung injury outside the intensive care unit. We set out to document the following: the association between predefined clinical conditions and the development of acute lung injury by using the American–European consensus definition; the frequency of lung injury development outside the intensive care unit; and the temporal relationship between antecedent clinical risk conditions, intensive care admission, and diagnosis of lung injury.
Methods
We conducted a 4-month prospective observational study in three Spanish teaching hospitals, enrolling consecutive patients who developed clinical conditions previously linked to lung injury, both inside and outside the intensive care unit. Patients were followed prospectively for outcomes, including the diagnosis of acute lung injury or acute respiratory distress syndrome.
Results
A total 815 patients were identified with at least one clinical insult; the most common were sepsis, pneumonia, and pancreatitis. Pulmonary risk conditions were observed in 30% of cases. Fifty-three patients (6.5%) developed acute lung injury; 33 of these (4.0%) met criteria for acute respiratory distress syndrome. Lung injury occurred most commonly in the setting of sepsis (46/53; 86.7%), but shock (21/59; 36%) and pneumonia (20/211; 9.5%) portended the highest proportional risk; this risk was higher in patients with increasing numbers of clinical risk conditions (2.2%, 14%, and 21% (P < 0.001) in patients with one, two, and three conditions, respectively). Median days (interquartile range) from risk condition to diagnosis of lung injury was shorter with pulmonary (0 (0 to 2)) versus extrapulmonary (3 (1 to 5)) (P = 0.029) risk conditions. Admission to the intensive care unit was provided to 9/20 (45%) patients with acute lung injury and to 29/33 (88%) of those with acute respiratory distress syndrome. Lung injury patients had higher mortality than others (acute lung injury 25.0%; acute respiratory distress syndrome 45.5%; others 10.3%; P < 0.001).
Conclusion
The time course from clinical insult to diagnosis of lung injury was rapid, but may be longer for extrapulmonary cases. Some patients with lung injury receive care and die outside the intensive care unit; this observation needs further study.
Similar content being viewed by others
Introduction
Conceptually, acute respiratory distress syndrome (ARDS) is an inflammatory lung injury involving both endothelial and epithelial layers of the alveolar-capillary membrane, with subsequent alveolar flooding and formation of a hyaline membrane, arising either from a direct (pulmonary) or indirect (extrapulmonary) insult [1–6]. In clinical practice and in research studies, this ARDS concept is most commonly captured by using the 1994 American–European Consensus Conference (AECC) definition [3, 7–9]. Acute lung injury (ALI) is defined as the acute onset of hypoxemia (PaO2/FiO2 (partial pressure of arterial oxygen/fractional concentration of inspired oxygen) ≤ 300 mmHg) and bilateral infiltrates on frontal chest X-ray, in the absence of left atrial hypertension. ARDS comprises the severe end of the ALI spectrum, defined with the same criteria, except that the hypoxemia threshold is 200 mmHg [3].
In recent years several multicentre observational studies have examined ARDS epidemiology in terms of incidence, risk factors, and associations with mortality [7, 9–16]. All of these studies, however, examined antecedent clinical insults from the perspective of patients with ALI or ARDS, reporting the proportion of cases that were due, for example, to pneumonia or sepsis. Studies examining these associations from the perspective of patients at risk of ALI/ARDS are both less prevalent and less recent, all reporting data collected in the early 1980s [17–19]. Because of the time at which they were performed, none of these studies was able to use current clinical definitions for ALI/ARDS or other clinical entities such as sepsis syndrome [20]. In addition, all of the studies outlined above identified patients who were admitted to an intensive care unit (ICU) [7, 9–15, 17–19]. As suggested in a recent editorial, it may be reasonable to assume that most patients with ARDS need treatment in an ICU, but many patients with milder ALI may not receive care in an ICU for medical or non-medical reasons; little is known about these patients [21].
We therefore performed a prospective observational study with the following objectives: to document the association between predefined clinical conditions and the development of ALI/ARDS by using the AECC definitions; to document the frequency of ALI/ARDS development outside the ICU; and to document the temporal relationship between antecedent clinical risk conditions, admission to the ICU, and diagnosis of ALI/ARDS.
Methods
Ethical considerations
The ethics committee at each participating hospital approved the study and waived the need for informed consent.
Patients
Patients were recruited from three hospitals in the south of the Comunidad de Madrid, Madrid, Spain, from 1 March to 30 June 2003. This study duration was chosen on the basis of resources available for data collection. These three general hospitals each have tertiary ICUs and residency training programs. They service adjacent, well-defined geographic areas; on the basis of 2001 census data they include a total of 573,149 individuals older than 18 years of age [22]. The usual practice in the Comunidad de Madrid is for patients to present to or be transferred to their geographically assigned hospital when acute care admission is required.
We screened patients who were admitted to an ICU or hospital ward and enrolled them if they were admitted with or developed one or more clinical conditions previously reported to be linked to the development of ARDS [3, 9, 19, 20, 23], defined by using standard definitions (see Tables 1, 2, 3 for details) [3, 24–27]. Patients with pneumonia, aspiration of gastric contents, pulmonary contusion, near-drowning, or inhalational injury were grouped as pulmonary cases; others were extrapulmonary. We excluded patients who were younger than 18 years, discharged from hospital alive within 48 hours of admission, transferred from another hospital with a pre-existing diagnosis of ALI/ARDS, or previously enrolled in the study cohort. In the medical–surgical ICUs and each at-risk ward area, all admitted patients were actively screened for the presence of these clinical conditions associated with ARDS by physician co-investigators, who reviewed admission records and patient charts and liaised with nurses and physicians on each ward to identify patients with these clinical risk conditions.
Cohort follow-up and data collection
Enrolled patients were followed daily for the development of ALI/ARDS [3]. In addition, until the development of ALI/ARDS, we continued to screen enrolled patients daily for the development of other clinical risk conditions. Screening for ALI/ARDS diagnosis was continued for 7 days unless another clinical insult developed, in which case follow-up was continued for a total of 14 days. When a diagnosis of ALI was made we continued to follow patients daily to document potential conversion to ARDS.
At the time of enrolment we recorded demographic data, the reason for admission to hospital, previous comorbidity status (McCabe score), whether their admission was medical or surgical, their location before admission (home, other acute hospital, or chronic hospital), and the presence of comorbidities. In addition, data on each patient was collected at up to four distinct time points (if they occurred and were separated by at least 12 hours): time of clinical insult identification (enrolment); time of admission to ICU; time of endotracheal intubation; and time of development of ALI/ARDS. At each of these time points we recorded as much of the following information as was available: severity of illness (simplified acute physiology score (SAPS) II); number of organ failures and multiple organ dysfunction (MODS) score; hemodynamic data (heart rate, mean arterial pressure, central venous pressure, pulmonary artery wedge pressure, pulmonary artery pressure, and cardiac index); ventilatory data (FiO2, respiratory rate, ventilator mode, tidal volume, positive end-expiratory pressure, peak inspiratory pressure, and inspiratory/expiratory ratio); and arterial blood gases. All enrolled patients were followed to capture relevant outcome data, including hospital mortality and length of hospital stay, and if applicable, mortality in ICU, the length of stay in the ICU, and the duration of mechanical ventilation.
Data coordination and quality assurance
We held monthly meetings between physicians at all centres, including the coordinating centre (Hospital Universitario de Getafe), to address issues or problems with definitions or enrolment. Case report forms were sent to the coordinating centre and were double-entered into a database. Blank fields or improbable values generated queries that were returned to each centre for correction. The coordinating centre selected a random 10% sample of surveyed patients at each hospital, and data were re-abstracted from the medical records by study personnel from one of the other hospitals to ensure validity.
Statistical analysis
Results are expressed as medians and interquartile range, or proportions with 95% confidence intervals (CI) as appropriate. We used the Mann–Whitney U test to compare continuous variables, and the χ2 test or Fisher's exact test to compare proportions, as appropriate. Two-tailed P values of less than 0.05 were used to indicate statistical significance. If patients initially presented with ALI and then went on to develop ARDS, we included them only in the ARDS group. Times to diagnosis of ALI/ARDS were compared by using a Kaplan–Meier survival analysis. All analyses were conducted with SPSS version 12.0 (SPSS Inc., Chicago, IL).
Results
Patients
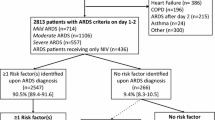
During the 4-month study period a total of 15,852 adults were admitted to the three hospitals, 815 (5.1%) of whom were enrolled after being identified with at least one clinical condition linked to ALI/ARDS; 108 (13.3%) received care in the ICU, whereas 707 (86.7%) were cared for only on another ward (Figure 1). Demographic information and data collected on the day that the clinical insult was identified are displayed in Table 1. Sepsis syndrome was the most clinical insult, seen in 86% of cases, with pneumonia being next most frequent at 29% (although these categories were not mutually exclusive).
ALI/ARDS risk by clinical insult
A total of 53 patients (6.5%; 95% CI 5.0 to 8.4%) developed ALI/ARDS, 20 (2.4%) with ALI and 33 (4.0%) with ARDS. Three of the 33 patients with ARDS initially presented with ALI and then went on to ARDS after 1 day in two cases, and after 4 days in the third patient. These rates correspond to incidences of 27.7, 10.5, and 17.3 cases per 100,000 population per year for ALI/ARDS, ALI, and ARDS, respectively. When only ICU cases are considered these rates are lower, at 19.9, 4.7, and 15.2 cases per 100,000 population per year, respectively.
By definition, patients with ARDS had worse hypoxemia than patients with ALI; patients with ARDS were also more likely to be diagnosed in the ICU and to be receiving mechanical ventilation at the time of diagnosis (Table 2). Figure 2a displays the proportion of patients with each antecedent clinical condition who went on to develop ALI or ARDS. The likelihood of developing ALI/ARDS was not equal between pulmonary and extrapulmonary risk conditions (37/244 (15.2%) versus 26/571 (4.6%); P < 0.001), nor among the mutually exclusive groupings risk conditions of shock 21/59 (35.6%), pneumonia without shock 20/211 (9.5%), and non-pulmonary sepsis without shock 6/432 (1.4%; P < 0.001). Examining only ICU patients (Figure 2b) leads to a much higher assessment of risk for each clinical insult. The frequency of ALI/ARDS also increased with the presence of an increasing number of clinical risk conditions (2.2%, 13.9%, and 20.8% for one, two, and three clinical conditions, respectively; P < 0.001).
Prevalence of ALI and ARDS by clinical risk condition. The proportion of patients with each clinical risk condition who went on to develop acute lung injury (ALI; blue columns) or acute respiratory distress syndrome (ARDS; red columns) is shown for all patients (a) and for only those admitted to the intensive care unit (b). In both panels the number of patients at risk with each clinical insult is displayed numerically below each category label.
ALI/ARDS timelines and outcomes
A diagnosis of ALI/ARDS was made after a median of 1 day (interquartile range 0 to 4 days) from the day of clinical insult in all patients (Figure 3a), and was not statistically different between patients with ALI and those with ARDS (Table 2). In contrast, patients who developed ALI/ARDS with pulmonary conditions did so more quickly than extrapulmonary patients (median 0 (interquartile range 0 to 2) versus 3 (1 to 5) days; P = 0.001; Figure 3b).
Time from clinical risk to diagnosis of ALI/ARDS. Kaplan–Meier curves displaying time from clinical risk condition to diagnosis of acute lung injury/acute respiratory distress syndrome (ALI/ARDS) are shown for all patients (a) and separated according to pulmonary (red line) versus extrapulmonary (blue line) risk conditions (b).
Patients with ARDS received ICU care significantly more frequently than patients with ALI (29/33 (88%) versus 9/20 (45%); P = 0.001), although the durations of ICU stay (ARDS 15 (7.5 to 36.5) versus ALI 7 (5.25 to 22.5) days; P = 0.16) and the times from ICU admission to diagnosis of ALI/ARDS (ARDS 1 (0 to 3.5) versus ALI 3 (0 to 4.5) days; P = 0.81) were not significantly different between these groups. Grouping together all patients with ALI/ARDS admitted to the ICU, Figure 4 shows the frequency histograms for the timing of ICU admission relative to development of the first clinical insult (upper panel), and diagnosis of ALI/ARDS relative to ICU admission (lower panel); on average, patients were admitted to the ICU on the day that their clinical insult developed, and they were diagnosed with ALI/ARDS 1 day later.
Timing of ICU admission relative to clinical risk and diagnosis of lung injury. Frequency histograms are shown for the timing of intensive care unit (ICU) admission relative to development of clinical risk condition (a), and diagnosis of acute lung injury (ALI)/acute respiratory distress syndrome (ARDS) relative to ICU admission (b), including together all patients with ALI and ARDS admitted to the ICU. Dx, diagnosis; IQR, interquartile range.
The relatively small number of ALI/ARDS cases makes it difficult to interpret outcome comparisons in these groups. Both ICU mortality and hospital mortality were numerically higher for patients with ARDS than for those with ALI, but these differences did not reach statistical significance (Table 3). Patients who developed either ALI or ARDS had higher hospital mortality rates than those who did not go on to develop lung injury (25.0% ALI; 45.5% ARDS; 10.3% no ALI/ARDS; P < 0.001). The mortality rate in patients with ALI admitted to the ICU was 22.2% (95% CI 6.3 to 54.7%); 27.3% (95% CI 9.8 to 56.6%) of patients with ALI who remained on the ward died (P = 0.60).
Discussion
The main findings of this study were as follows: a significant number of patients with ALI did not receive care in an ICU; when patients outside the ICU were included, the chance of developing ALI/ARDS with a given clinical insult was substantially lower than reported previously; and the time course from clinical insult to admission to the ICU and diagnosis of ALI/ARDS is rapid, but this process may take longer for extrapulmonary ALI/ARDS.
Although many studies have reported the frequency of antecedent clinical conditions as they occur in patients who develop ALI/ARDS [9, 11–15, 28, 29], very few have prospectively followed patients with these conditions to document the probability of developing ARDS [17–20]. These studies all used more stringent diagnostic criteria for ARDS, including more severe hypoxaemia and four-quadrant alveolar disease on a chest radiograph [19], reduced respiratory system compliance, and a pulmonary artery wedge pressure of 12 mmHg or less [18]. Because they were all conducted in the early 1980s, none of them examined current definitions for ALI or ARDS. In addition, the current definition of some clinical predispositions, notably sepsis syndrome and pneumonia, were unavailable at the time of these studies. We believe our study to be one of the first to expand surveillance outside the walls of the ICU, capturing at-risk patients on regular hospital wards. When we included all patients (ward and ICU), the risks for developing ALI and ARDS for a given clinical insult are significantly lower than reported previously. Undoubtedly this is due, at least in part, to the inclusion of patients with milder forms of these underlying conditions who seem less likely to develop ALI and ARDS. When we restrict our analysis to the ICU, we see similar rates for sepsis syndrome or shock, as Hudson and colleagues reported for their patients with septic shock (32% and 29% versus 41%) [19]. However, our rate of ARDS with pneumonia in the ICU was significantly higher than that reported by Fowler and colleagues (43% vs. 12%) [18], probably reflecting a less stringent ARDS definition and stricter ICU admission threshold in 2003 than in 1983.
Another important finding of this study is that more than half the patients with ALI (PaO2/FiO2 200 to 300 mmHg) were managed entirely outside the ICU. This has important implications for the accurate estimation of the true burden of disease in the population [7], but it also has meaning for clinicians. First, for clinicians managing patients on medical and surgical wards, it is important to realize that many patients with acute lung injury will be managed entirely outside the ICU. These patients with ALI will need different therapy from patients with cardiogenic pulmonary edema, for whom they may be mistaken. Second, for the intensivist, the question is whether these patients with ALI should be left on the ward, or whether their outcomes would be better if they received care in the ICU. In our study the death rates were not statistically different between patients with ALI who were admitted to the ICU and those who were not (22% versus 27%). Although the confidence intervals around these estimates are wide, they certainly do not suggest that these patients with ALI were kept on the floor because they were all going to do well. It is unknown whether admission to the ICU to receive therapies such as more vigorous resuscitation or non-invasive ventilation would change this outcome. We do not have a sufficient number of patients or enough information about their ward care to specifically address this question in our study. However, as many jurisdictions move to implement critical care outreach or medical emergency response teams [30, 31], the fact that there may be many patients with ALI on the hospital wards should be recognized, and such teams may facilitate their further study.
We found that, on average, patients progressed quickly from development of clinical insult, to ICU admission, to diagnosis of ALI/ARDS. The finding that most cases of ARDS occur quickly after the onset of the clinical predisposition is not new [18, 19]; however, we extend this knowledge in two ways. First, our finding that most patients entering the ICU do so on the day of developing their clinical insult is new, and it underscores the potential need for rapid intervention in these patients. Second, we observed a significantly longer time to ALI/ARDS development for extrapulmonary risk conditions compared with pulmonary risk conditions. This is In contrast with the findings of Hudson and colleagues, who showed fairly comparable times of ARDS onset for sepsis and aspiration [19]. This difference may be explained by the inclusion of patients with pneumonia in the sepsis category of the earlier study, and by a more liberal ARDS definition in our study, in which patients with direct lung injury already had a significant 'head start' in reaching the syndromic thresholds for ARDS. Finally, it is worth noting that relatively few patients initially diagnosed with ALI went on to develop ARDS (13%); this is a significantly lower proportion than the 55% conversion rate reported in a recent multicentre observational study [14]. The reasons for this difference are not clear; our patients with ARDS may have progressed more quickly for whatever reason, such that their movement through ALI was not captured in our once-daily screening.
Our study has several limitations. First, enrolment was limited to three hospitals in Madrid; local practice patterns (including thresholds for ICU admission) and case mix (including a lack of trauma patients, and the fact many non-ICU patients were quite elderly) may limit the generalizability of these results. Second, in this observational study we did not have a formal protocolized screening process for documenting ALI/ARDS. Chest X-rays and arterial blood gas measurements were performed when clinically indicated according to the treating physicians; we may therefore have missed some patients with ALI/ARDS, particularly on the wards in which these test are performed less frequently. Third, we enrolled patients over only a 4-month period. This has implications both in terms of missing seasonal variations in disease patterns and, importantly, in terms of the relatively small number of ALI/ARDS cases we were able to document, leading to imprecision in our point estimates, both for risk rates for different clinical conditions and mortality rates of ALI/ARDS. In addition, the accuracy of our incidence data may be questioned because of the short duration of the study and difficulties in accurately determining the population at risk (incidence denominator). Finally, we did not have the resources available to double-screen or perform other quality control measures on patients who were not already enrolled in the cohort. It is possible that we missed some patients with our defined clinical risk conditions, especially outside the ICU; however, the large number of patients at risk who were enrolled from the wards militates against this as a major flaw. In addition, our having missed patients entirely would have biased us toward underestimating the importance of ALI on the hospital wards and should not have had a large impact on our estimates of ALI/ARDS development rates and times.
Conclusion
We have observed that the time course from clinical insult to diagnosis of lung injury was rapid, but it was longer for extrapulmonary cases. The risk of ARDS was significantly lower than reported previously when patients outside the ICU were considered, but rates in ICU patients appeared similar. A significant number of patients with ALI received care outside the ICU; whether this is ideal requires further study.
Key messages
-
A significant number of patients with ALI did not receive care in an ICU; this observation needs further study.
-
When patients outside the ICU were included, the chance of developing ALI/ARDS with a given clinical insult was substantially lower than reported previously.
-
The time course from clinical insult to ICU admission and diagnosis of ALI/ARDS is rapid, but this process may take longer for extrapulmonary ALI/ARDS.
Abbreviations
- AECC:
-
American–European consensus conference
- ALI:
-
acute lung injury
- ARDS:
-
acute respiratory distress syndrome
- CI:
-
confidence interval
- FiO2:
-
fractional concentration of inspired oxygen
- ICU:
-
intensive care unit
- PaO2:
-
partial pressure of arterial oxygen.
References
Lesur O, Berthiaume Y, Blaise G, Damas P, Deland E, Guimond JG, Michel RP: Acute respiratory distress syndrome: 30 years later. Can Resp J 1999, 6: 71-86.
Ware LB, Matthay MA: The acute respiratory distress syndrome. N Engl J Med 2000, 342: 1334-1349. 10.1056/NEJM200005043421806
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy , LeGall JR, Morris A, Spragg R: Report of the American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. The Consensus Committee. Intensive Care Med 1994, 20: 225-232. 10.1007/BF01704707
Lyons WS: Advancing the concept of two distinct ARDSs. J Trauma Injury Infect Crit Care 2000, 48: 188. 10.1097/00005373-200001000-00039
Goodman LR, Fumagalli R, Tagliabue P, Tagliabue M, Ferrario M, Gattinoni L, Pesenti A: Adult respiratory distress syndrome due to pulmonary and extrapulmonary causes: CT, clinical, and functional correlations. Radiology 1999, 213: 545-552.
Gattinoni L, Pelosi P, Suter PM, Pedoto A, Vercesi P, Lissoni A: Acute respiratory distress syndrome caused by pulmonary and extrapulmonary disease: different syndromes? Am J Resp Crit Care Med 1998, 158: 3-11.
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD: Incidence and outcomes of acute lung injury. N Engl J Med 2005, 353: 1685-1693. 10.1056/NEJMoa050333
The Acute Respiratory Distress Syndrome Network: Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000, 342: 1301-1308. 10.1056/NEJM200005043421801
Bersten AD, Edibam C, Hunt T, Moran J: Incidence and mortality of acute lung injury and the acute respiratory distress syndrome in three Australian States. Am J Respir Crit Care Med 2002, 165: 443-448.
Goss CH, Brower RG, Hudson LD, Rubenfeld GD, ARDS Network: Incidence of acute lung injury in the United States. Crit Care Med 2003, 31: 1607-1611. 10.1097/01.CCM.0000063475.65751.1D
Luhr OR, Antonsen K, Karlsson M, Aardal S, Thorsteinsson A, Frostell CG, Bonde J: Incidence and mortality after acute respiratory failure and acute respiratory distress syndrome in Sweden, Denmark, and Iceland. The ARF Study Group. Am J Resp Crit Care Med 1999, 159: 1849-1861.
Monchi M, Bellenfant F, Cariou A, Joly LM, Thebert D, Laurent I, Dhainaut JF, Brunet F: Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Resp Crit Care Med 1998, 158: 1076-1081.
Ferguson ND, Frutos-Vivar F, Esteban A, Anzueto A, Alia I, Brower RG, Stewart TE, Apezteguia C, Gonzalez M, Soto L, et al.: Airway pressures, tidal volumes and mortality in patients with the acute respiratory distress syndrome. Crit Care Med 2005, 33: 21-30. 10.1097/01.CCM.0000150652.91411.66
Brun-Buisson C, Minelli C, Bertolini G, Brazzi L, Pimentel J, Lewandowski K, Bion J, Romand JA, Villar J, Thorsteinsson A, et al.: Epidemiology and outcome of acute lung injury in European intensive care units. Results from the ALIVE study. Intensive Care Med 2004, 30: 51-61. 10.1007/s00134-003-2022-6
Roupie E, Lepage E, Wysocki M, Fagon JY, Chastre J, Dreyfuss D, Mentec H, Carlet J, Brun-Buisson C, Lemaire F, et al.: Prevalence, etiologies and outcome of the acute respiratory distress syndrome among hypoxemic ventilated patients. SRLF Collaborative Group on Mechanical Ventilation. Societe de Reanimation de Langue Francaise. Intensive Care Med 1999, 25: 920-929. 10.1007/s001340050983
Roca O, Sacanell J, Laborda C, Pérez M, Sabater J, Burgueño MJ, Domínguez L, Masclans JR: Estudio de cohortes sobre incidencia de SDRA en pacientes ingresados en UCI y factores pronósticos de mortalidad. Medicina Intensiva 2006, 30: 6-12.
Pepe PE, Potkin RT, Reus DH, Hudson LD, Carrico CJ: Clinical predictors of the adult respiratory distress syndrome. Am J Surg 1982, 144: 124-130. 10.1016/0002-9610(82)90612-2
Fowler AA, Hamman RF, Good JT, Benson KN, Baird M, Eberle DJ, Petty TL, Hyers TM: Adult respiratory distress syndrome: risk with common predispositions. Ann Int Med 1983, 98: 593-597.
Hudson LD, Milberg JA, Anardi D, Maunder RJ: Clinical risks for development of the acute respiratory distress syndrome. Am J Resp Crit Care Med 1995, 151: 293-301.
Hudson LD, Steinberg KP: Epidemiology of acute lung injury and ARDS. Chest 1999, 116: 74S-82S. 10.1378/chest.116.suppl_1.74S-a
Quartin AA, RM HS: Acute lung injury: is the intensive care unit the tip of the iceberg? Crit Care Med 2003, 31: 1860-1861. 10.1097/01.CCM.0000063444.28173.79
Instituto Nacional de Estadistica: Censo de Población y Viviendas 2001[http://ccforum.com/content/11/5/R96]
Stewart TE, Meade MO, Cook DJ, Granton JT, Hodder RV, Lapinsky SE, Mazer CD, McLean RF, Rogovein TS, Schouten BD, et al.: Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome. Pressure- and Volume-Limited Ventilation Strategy Group. N Engl J Med 1998, 338: 355-361. 10.1056/NEJM199802053380603
Bone RC, Sibbald WJ, Sprung CL: The ACCP-SCCM consensus conference on sepsis and organ failure. Chest 1992, 101: 1481-1483. 10.1378/chest.101.6.1481
Cook DJ, Walter SD, Cook RJ, Griffith LE, Guyatt GH, Leasa D, Jaeschke RZ, Brun-Buisson C: Incidence of and risk factors for ventilator-associated pneumonia in critically ill patients. Ann Int Med 1998, 129: 433-440.
Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ: Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med 1995, 23: 1638-1652. 10.1097/00003246-199510000-00007
Grossman RF, Fein A: Evidence-based assessment of diagnostic tests for ventilator-associated pneumonia. Chest 2000, 117: 177S-181S. 10.1378/chest.117.4_suppl_2.177S
Doyle RL, Szaflarski N, Modin GW, Wiener-Kronish JP, Matthay MA: Identification of patients with acute lung injury. Predictors of mortality. Am J Resp Crit Care Med 1995, 152: 1818-1824.
Zilberberg MD, Epstein SK: Acute lung injury in the medical ICU: comorbid conditions, age, etiology, and hospital outcome. Am J Resp Crit Care Med 1998, 157: 1159-1164.
Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, Finfer S, Flabouris A: Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet 2005, 365: 2091-2097. 10.1016/S0140-6736(05)66733-5
Ball C, Kirkby M, Williams S: Effect of the critical care outreach team on patient survival to discharge from hospital and readmission to critical care: non-randomised population based study. BMJ 2003, 327: 1014-1016. 10.1136/bmj.327.7422.1014
Acknowledgements
We thank Dr Ted Marras, Dr Matthew Stanbrook, and Dr Brian Kavanagh for their insightful critiques of earlier versions of this manuscript. This work was funded by Red Gira G03/063 and Red Respira C03/11, Instituto de Salud Carlos III, Madrid, Spain, and by an unrestricted grant from Eli Lilly, Spain. NDF was supported by a Canadian Institutes of Health Research and Canadian Lung Association Post-Doctoral Fellowship at the time of this study, and is currently supported by a Canadian Institutes of Health Research RCT Mentoring Award. None of the funding agencies had any influence on the design, implementation, interpretation, or reporting of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
NDF, FFV, and AE conceived the study. All authors contributed to the study design and interpretation of the data. FFV, FG, TH, OP, AA, GG, AA, and IR participated in the acquisition of the data. NDF performed the data analysis and wrote the first draft of the manuscript, which was then revised for intellectually important content by all authors. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ferguson, N.D., Frutos-Vivar, F., Esteban, A. et al. Clinical risk conditions for acute lung injury in the intensive care unit and hospital ward: a prospective observational study. Crit Care 11, R96 (2007). https://doi.org/10.1186/cc6113
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc6113