Abstract
Introduction
Several studies have shown a correlation between body mass index (BMI) and both the development of critical illness and adverse outcomes in critically ill patients. The goal of our study was to examine this relationship prospectively with particular attention to the influence of concomitant diabetes mellitus (DM).
Methods
We analyzed data from 15,408 participants in the Atherosclerosis Risk in Communities (ARIC) study for this analysis. BMI and the presence of DM were defined at baseline. We defined 'acute organ failure' as those subjects who met a standard definition with diagnostic codes abstracted from hospitalization records. Outcomes assessed included the following: risk of the development of acute organ failure within three years of the baseline examination; in-hospital death while ill with acute organ failure; and death at three years among all subjects and among those with acute organ failure.
Results
At baseline, participants with a BMI of at least 30 were more likely than those in lower BMI categories to have DM (22.4% versus 7.9%, p < 0.01). Overall, BMI was not a significant predictor of developing acute organ failure. The risk for developing acute organ failure was increased among subjects with DM in comparison with those without DM (2.4% versus 0.7%, p < 0.01). Among subjects with organ failure, both in-hospital mortality (46.5% versus 12.2%, p < 0.01) and 3-year mortality (51.2% versus 21.1%, p < 0.01) was higher in subjects with DM.
Conclusion
Our findings suggest that obesity by itself is not a significant predictor of either acute organ failure or death during or after acute organ failure in this cohort. However, the presence of DM, which is related to obesity, is a strong predictor of both acute organ failure and death after acute organ failure.
Similar content being viewed by others
Introduction
Obesity is one of the major health problems in our society and its prevalence is rising worldwide [1, 2]. Currently, about 130 million US adults, 65% of the population, are overweight or obese. In addition, an increasing proportion of children in the USA are either overweight or obese, and this number has almost doubled over the past two decades [1].
Excess body weight increases the risk of hypertension, coronary artery disease, stroke, sleep apnea, and certain cancers [3–6]. Several population studies have described an association between body mass index (BMI) and mortality as a U-shaped curve, demonstrating increased mortality in the lowest and highest BMI distribution, even when controlling for age, smoking, and history of other comorbidities [7–11]. Obesity is also strongly associated with an increased risk of diabetes [12].
However, the influence of BMI on morbidity and mortality in critically ill patients is still controversial [13, 14]. Retrospective analysis of 63,646 patients from a multi-institutional intensive care unit database showed increased mortality in underweight patients (BMI ≤ 20) but not in overweight or obese patients [15].
By contrast, Goulenok and colleagues demonstrated, in a prospective study of critically ill patients, that a higher BMI was associated with increased mortality [16]. The authors did not include diabetes as an independent variable in the analysis and could not explain the results even though the infection rate and the duration of mechanical ventilation were not increased in the obese group. Studies of critically ill patients who are morbidly obese (BMI > 40) have shown more complications and higher mortality but have not controlled for diabetes mellitus (DM) [17, 18].
The relationship between obesity and diabetes, and particularly the modifying effect of the latter, in the development of acute organ failure, critical illness, and subsequent mortality is not well defined. A better understanding of this relationship may help to improve interventions and therefore outcomes in this commonly seen group of patients.
The goals of this analysis were to examine the effect of BMI in the development of acute organ failure and subsequent mortality in a large, population-based, prospective cohort. We also wished to determine the role of DM in modifying the effect of obesity.
Materials and methods
Study population
The Atherosclerosis Risk in Communities (ARIC) study is a prospective, population-based study of the natural history and etiology of cardiovascular disease. The ARIC population is a probability sample of 15,792 men and women aged from 44 to 66 years from four US communities (Suburban Minneapolis, Minnesota; Washington County, Maryland; Forsyth County, North Carolina, and Jackson, Mississippi) originally studied in 1986 to 1989 [19]. The cohort population reflects the demographic sample of the community except Jackson, where only African-Americans were included. Participants underwent baseline clinical examination, BMI measurement, and pulmonary function testing, and provided information on their medical and smoking history and educational background. The study was approved by institutional review boards at the clinical sites, and informed consent was obtained from all participants.
Subjects
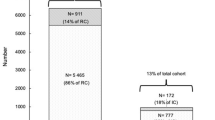
We restricted this analysis to participants for whom there was complete baseline data on variables important to this analysis, including BMI, DM status, lung function testing, and smoking history. We excluded 208 subjects for whom there were missing data on diabetes status, 131 subjects for whom there were missing data on lung function, and 45 subjects for whom there were missing data on other key variables, resulting in 15,408 participants in our analytic cohort.
Hospitalization summaries, including International Classification of Disease, Ninth Revision (ICD-9) codes for the discharge diagnoses and procedures performed, and disposition were available for all study participants. In addition, data from death certificates were also available.
Definitions of variables
Acute organ failure
We identified these subjects as those who were hospitalized and developed acute organ dysfunction as defined by Martin and colleagues [20] using ICD-9 codes (sepsis was not required as part of this definition). Diagnostic codes for organ dysfunction in these systems were included: respiratory, cardiovascular, renal, hepatic, hematologic, metabolic, and neurologic. Although one would assume that most inpatients who develop 'acute organ failure' would be critically ill and admitted to an intensive care unit, the site of in-hospital treatment was not available in the database.
Body mass index
Weight and height were measured, and BMI, calculated as weight (in kilograms) divided by the square of the height (in meters) was defined at baseline. Each group was further divided into four BMI subgroups, as follows: underweight (defined as BMI ≤ 20 kg/m2), normal (defined as a BMI of 21 to 24 kg/m2), overweight (defined as a BMI of 25 to 29 kg/m2) and obese (defined as BMI ≥ 30 kg/m2). These are commonly accepted standard subgroups except that we did adjust the underweight group, generally defined as BMI ≤ 18.5, to increase the sample size in this group and provide more stable estimates [1].
Diabetes status
We classified subjects as having DM at the baseline examination if they had any of the following: a positive response to the question 'Has a doctor ever told you that you had diabetes (sugar in the blood)?'; a report of taking medication for 'diabetes or high blood sugar' in the two weeks before the survey; a fasting blood sugar of 126 or higher. We were not able to distinguish between types 1 and 2 DM.
Lung function
We used a modification of the criteria developed by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) [21] to classify subjects according to their GOLD stages of chronic obstructive pulmonary disease (COPD): GOLD stage 3 or 4 (forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) < 0.70 and FEV1 < 50% predicted), GOLD stage 2 (FEV1/FVC < 0.70 and FEV1 ≥ 50 to < 80% predicted), GOLD stage 1 (FEV1/FVC < 0.70 and FEV1 ≥ 80%), restricted (FEV1/FVC ≥ 0.70 and FVC < 80% predicted), GOLD stage 0 (presence of respiratory symptoms in the absence of any lung function abnormality), and no lung disease. Bronchodilator response was not evaluated in this survey, so the classification is based on the 'pre-bronchodilator' level. We used data from asymptomatic never-smokers with no lung disease, stratified by race and sex, to develop internal prediction equations to determine normal values for lung function.
Other variables
Respondents with positive responses to the questions 'Have you ever smoked cigarettes?' and 'Do you now smoke cigarettes?' were classified as 'ever smokers' and 'current smokers', respectively. Education level was categorized as less than high school, completion of high school, or more than high school. Baseline age was grouped into four strata: 44 to 49 years, 50 to 54 years, 55 to 59 years, and 60 to 66 years.
Outcome variables
The primary outcomes of interest were the risk of the development of acute organ failure within three years of the baseline examination, in-hospital mortality related to any acute organ failure during that period, and all-cause mortality at three years.
Analysis
All analyses were conducted with SAS version 8.2 (SAS Institute, Cary, NC, USA), SUDAAN version 8.0 (RTI, Research Triangle Park, NC, USA) and SPSS version 10 (SPSS Inc, Chicago, IL, USA). Multivariable logistic regression models were developed for the outcomes of any hospitalization with acute organ failure, death at three years, and in-hospital death among those with acute organ failure. Models were adjusted for age, sex, race, smoking status, education level, BMI, diabetes status, and lung function status.
Cox proportional hazard regression models were developed with the SUDAAN procedure SURVIVAL to account for differential follow-up in ARIC participants. Time of follow-up was used as the underlying time metric. For deaths, the exit date was the date of death reported on the death certificate and, for survivors, the exit date was the date on which the participant was last known to be alive. Plots of the log-log survival curves for each covariate were used to show that the proportional-hazards assumptions were met. Age, sex, race, smoking status, education level, BMI, diabetes status, and lung function status were included in the adjusted models, and the models were evaluated for interactions.
Results
A total of 15,792 adults aged 44 to 66 years participated in the ARIC study. We excluded 384 subjects with missing data either on diabetes status, lung function or other key variables, resulting in 15,408 subjects in our analytic cohort.
The demographic characteristics of the cohort population at baseline and their outcomes are shown in Table 1. About one-third of the study population (29.9%) had an ideal body weight (BMI 21 to 24), 39.3% were overweight (BMI 25 to 29) and 27.5% were obese (BMI ≥ 30). This distribution reflects the US population well, with an estimated prevalence of about 30% obese and 35% overweight [1]. The mean BMIs of the cohort by BMI category was 18.9 (BMI < 20), 22.9 (BMI = 20 to 24), 27.3 (BMI = 25 to 29), and 34.5 (BMI ≥ 30).
Overall, 1,830 (11.9%) of all participants had DM. Participants with DM were more likely than those without DM to have a BMI of 30 or more (52% versus 24%, p < 0.01). The prevalence of DM increased with increasing BMI: 4.4% for BMI < 20, 4.9% for BMI = 20 to 24, 10% for BMI = 25 to 29, and 22.4% for BMI ≥ 30. Of the 1,830 subjects classified as having DM, 636 (43%) were classified solely on the basis of a fasting blood sugar of more than 126 mg/dl.
The development of acute organ failure among participants with different BMI subgroups was almost identical: 0.9% of subjects with ideal body weight developed acute organ failure, in comparison with 0.8% and 0.9% for overweight and obese subjects, respectively. BMI subgroups had similar mortality at the 3-year follow-up (Table 1). Within three years 5.4% of subjects with diabetes, in contrast with 1.6% of subjects without diabetes, died (Table 1).
Risk factors for developing acute organ failure within three years of the baseline evaluation and death within three years are displayed in Table 2. The significant risk factors for acute organ failure included older age, male sex, DM, and lower levels of lung function. These same factors, along with smoking, black race, and a lower educational level, predicted death within three years. The presence of DM was among the strongest independent predictors for the risk of acute organ failure, with a threefold increased risk (odds ratio 3.2; 95% confidence interval 2.1 to 4.7), and for all-cause mortality at 3 years (odds ratio 2.7; 95% confidence interval 2.1 to 3.5).
Table 3 displays the risk of the development of acute organ failure, in-hospital mortality among those with acute organ failure, and mortality at three years among those with acute organ failure by DM status. Subjects with DM were both more likely to develop a organ failure (2.4% versus 0.7%, p < 0.01) and to die during that hospitalization (46.5% versus 12.2%, p < 0.01) than were subjects without DM.
Time to the development of acute organ failure is presented in Figure 1, stratified by BMI (Figure 1a) and by DM status (Figure 1b). Cox proportional-hazards models in Table 4 show that in comparison with subjects without DM with BMIs of 21 to 24, subjects with DM had about a threefold higher risk of developing acute organ failure. Although the confidence intervals were wide because of sample size, a similar trend for a higher risk of in-hospital mortality was also noted among subjects with DM.
Discussion
The results of this large prospective cohort study of middle-aged adults in the USA suggest that the development of acute organ failure and death after acute organ failure is more related to the presence of DM than to an increased BMI. Our definition of acute organ failure is, we believe, a surrogate for critical illness, in that these events occurred in the setting of a hospitalization. Our results do not support the contention that obesity itself is a risk factor for increased mortality in patients with acute organ failure. It brings up a new perspective on this still controversial subject of obesity, critical illness, and mortality. In addition, our findings did not confirm increased mortality in overweight or obese critically ill patients without DM.
Previous studies have shown that a low BMI is a significant predictor of higher hospital mortality [9, 11]. This increased risk among patients with low BMIs has also been demonstrated in critically ill patients, although these data are limited [15, 22]. Our data suggested that subjects with low BMI developed organ failure earlier (Figure 1 and Table 4) and had a higher risk of in-hospital death, although the confidence intervals were wide and did not reach significance.
Conversely, other epidemiological studies have shown that high BMI is associated with higher all-cause mortality rates [8, 9]. In one large prospective cohort study the mortality rate for overweight non-smoking men was 3.9 times higher then for non-smoking men of ideal weight [9]. Some authors have postulated that obesity may not be a risk factor with regard to subsequent mortality in critically ill individuals, but rather that it could have a beneficial role of 'nutritional reserve' in the face of critical illness [15].
The relationship between an increased BMI and DM has been well established [12, 23, 24]. Our data, similarly, showed that subjects with BMIs ≥ 30 had a fourfold higher prevalence of DM than subjects with BMIs of 20 to 24. Weight gain, which frequently precedes the onset of diabetes, is also considered to be a risk factor for this disease [25, 26]. Both increased insulin secretion and insulin resistance result from obesity, and hyperglycemia and insulin resistance are the hallmarks of diabetes. Hyperglycemia has been shown to increase the release of pro-inflammatory mediators such as IL-6, IL-8, and TNF, which are important in inflammation [27]. In addition, high glucose levels have been shown to have deleterious effects on optimal macrophage and neutrophil function [28]. These negative effects of hyperglycemia are responsible for the increased risk of infection, cardiovascular diseases, organ dysfunction, and certain cancers, as has been shown recently [29–31].
Our findings suggest that DM and associated hyperglycemia with insulin resistance, rather than obesity itself, is responsible for the development of acute organ failure and subsequent adverse outcomes in this middle-aged US population. This hypothesis can be further supported by recent and consistent evidence suggesting that the outcomes in critically ill patients are improved by both tight glucose control and insulin therapy with its anti-inflammatory properties [32–34].
This study has several limitations. First, the accuracy of ICD-9-CM (the clinical modification of ICD-9) coding in identifying specific medical conditions is unproven [35], yet it is increasingly used for epidemiologic purposes [20]. In critical illness, the sensitivity and specificity of the diagnostic code for sepsis were estimated to be 87.7% and 98.8%, respectively. However, the use of ICD-9 codes for epidemiologic estimates may underestimate true incidence [36].
Second, we have focused on patients who were hospitalized and developed acute organ dysfunction, although we acknowledge that definitions in critical care population are not well validated. For example, some patients who had chronic organ failure might have been captured with our definition, and others might have developed organ failure and died without being hospitalized.
Third, we did not subcategorize patients who were morbidly obese (BMI > 40) because of the small sample size (about 3%). At the time of the study, morbid obesity was not as significant problem as it has become over the past 15 years. It seems that increased mortality and increased risk of multiple complications in a morbidly obese population are more obvious, as shown in several retrospective studies, and should therefore be studied separately [14, 17, 18, 37].
Fourth, patients were enrolled in this trial in 1986 to 1989, and both treatment for diabetes and treatment of acute organ failure may have changed in the years since then. However, it is noteworthy that is that in the USA the proportion of diabetic patients who are 'well controlled', on the basis of hemoglobin A1C levels, has not improved over the past two decades [38].
Fifth, our definition of DM might not have included all subjects with this disease, in that we did not perform glucose tolerance testing or other confirmatory testing. However, this potential misclassification would have biased our results towards not finding an effect in the DM population.
Finally, we included only three years of follow-up in this analysis. This was done to focus on the short-term risk of BMI and DM on acute organ failure. Over the long term, patients with high BMIs are more likely to develop DM and would in all likelihood have an increased risk of acute organ failure and critical illness subsequently.
Conclusion
Results of this study indicate that the presence of DM, rather than an increased BMI, accounts for a higher risk of acute organ failure and associated mortality. These findings call for further investigation to determine the mechanisms that underlie this complex relationship between obesity, diabetes, and critical illness. It will help to optimize care, which will result in improved outcomes and a decrease in the associated health care costs currently being expended in this growing population of patients.
Key messages
-
In this middle-aged cohort, diabetics had a threefold higher incidence of organ failure over three years than non-diabetics.
-
After adjusting for diabetes, BMI did not predict organ failure in this cohort.
-
Among patients with organ failure in this cohort, diabetics had more than twice the risk of in-hospital death than non-diabetics.
-
After adjusting for diabetes, an increased BMI did not predict in-hospital death among patients with organ failure in this cohort.
Abbreviations
- ARIC:
-
ARIC = Atherosclerosis Risk in Communities
- BMI:
-
BMI = body mass index
- DM:
-
DM = diabetes mellitus
- FEV:
-
FEV1 = forced expiratory volume in 1 second
- FVC:
-
FVC = forced vital capacity
- GOLD:
-
GOLD = Global Initiative for Chronic Obstructive Lung Disease
- ICD:
-
ICD-9
- International Classification of Disease:
-
Ninth Revision
- IL:
-
IL = interleukin
- TNF:
-
TNF = tumor necrosis factor.
References
Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM: Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA 2004, 291: 2847-2850. 10.1001/jama.291.23.2847
Daviglus ML, Liu K, Yan LL, Pirzada A, Manheim L, Manning W, Garside DB, Wang R, Dyer AR, Greenland P, et al.: Relation of body mass index in young adulthood and middle age to Medicare expenditures in older age. JAMA 2004, 292: 2743-2749. 10.1001/jama.292.22.2743
Bray GA: Medical consequences of obesity. J Clin Endocrinol Metab 2004, 89: 2583-2589. 10.1210/jc.2004-0535
Stein CJ, Colditz GA: The epidemic of obesity. J Clin Endocrinol Metab 2004, 89: 2522-2525. 10.1210/jc.2004-0288
Cossrow N, Falkner B: Race/ethnic issues in obesity and obesity-related comorbidities. J Clin Endocrinol Metab 2004, 89: 2590-2594. 10.1210/jc.2004-0339
Petrelli JM, Calle EE, Rodriguez C, Thun MJ: Body mass index, height, and postmenopausal breast cancer mortality in a prospective cohort of US women. Cancer Causes Control 2002, 13: 325-332. 10.1023/A:1015288615472
Landi F, Onder G, Gambassi G, Pedone C, Carbonin P, Bernabei R: Body mass index and mortality among hospitalized patients. Arch Intern Med 2000, 160: 2641-2644. 10.1001/archinte.160.17.2641
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr: Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med 1999, 341: 1097-1105. 10.1056/NEJM199910073411501
Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, Hennekens CH, Speizer FE: Body weight and mortality among women. N Engl J Med 1995, 333: 677-685. 10.1056/NEJM199509143331101
Singh PN, Lindsted KD: Body mass and 26-year risk of mortality from specific diseases among women who never smoked. Epidemiology 1998, 9: 246-254. 10.1097/00001648-199805000-00002
Singh PN, Lindsted KD, Fraser GE: Body weight and mortality among adults who never smoked. Am J Epidemiol 1999, 150: 1152-1164.
Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC: Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care 1994, 17: 961-969.
Garrouste-Org , Troche G, Azoulay E, Caubel A, de LA, Cheval C, Montesino L, Thuong M, Vincent F, Cohen Y, et al.: Body mass index. An additional prognostic factor in ICU patients. Intensive Care Med 2004, 30: 437-443. 10.1007/s00134-003-2095-2
El-Solh A, Sikka P, Bozkanat E, Jaafar W, Davies J: Morbid obesity in the medical ICU. Chest 2001, 120: 1989-1997. 10.1378/chest.120.6.1989
Tremblay A, Bandi V: Impact of body mass index on outcomes following critical care. Chest 2003, 123: 1202-1207. 10.1378/chest.123.4.1202
Goulenok C, Monchi M, Chiche JD, Mira JP, Dhainaut JF, Cariou A: Influence of overweight on ICU mortality: a prospective study. Chest 2004, 125: 1441-1445. 10.1378/chest.125.4.1441
Nasraway SA Jr, Albert M, Donnelly AM, Ruthazer R, Shikora SA, Saltzman E: Morbid obesity is an independent determinant of death among surgical critically ill patients. Crit Care Med 2006, 34: 964-970. 10.1097/01.CCM.0000205758.18891.70
Yaegashi M, Jean R, Zuriqat M, Noack S, Homel P: Outcome of morbid obesity in the intensive care unit. J Intensive Care Med 2005, 20: 147-154. 10.1177/0885066605275314
The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators Am J Epidemiol 1989, 129: 687-702.
Martin GS, Mannino DM, Eaton S, Moss M: The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003, 348: 1546-1554. 10.1056/NEJMoa022139
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001, 163: 1256-1276.
Galanos AN, Pieper CF, Kussin PS, Winchell MT, Fulkerson WJ, Harrell FE Jr, Teno JM, Layde P, Connors AF Jr, Phillips RS, et al.: Relationship of body mass index to subsequent mortality among seriously ill hospitalized patients. SUPPORT Investigators. The Study to Understand Prognoses and Preferences for Outcome and Risks of Treatments. Crit Care Med 1997, 25: 1962-1968. 10.1097/00003246-199712000-00010
Hartz AJ, Rupley DC Jr, Kalkhoff RD, Rimm AA: Relationship of obesity to diabetes: influence of obesity level and body fat distribution. Prev Med 1983, 12: 351-357. 10.1016/0091-7435(83)90244-X
Carey VJ, Walters EE, Colditz GA, Solomon CG, Willett WC, Rosner BA, Speizer FE, Manson JE: Body fat distribution and risk of non-insulin-dependent diabetes mellitus in women. The Nurses' Health Study. Am J Epidemiol 1997, 145: 614-619.
Holbrook TL, Barrett-Connor E, Wingard DL: The association of lifetime weight and weight control patterns with diabetes among men and women in an adult community. Int J Obes 1989, 13: 723-729.
Colditz GA, Willett WC, Rotnitzky A, Manson JE: Weight gain as a risk factor for clinical diabetes mellitus in women. Ann Intern Med 1995, 122: 481-486.
Krogh-Madsen R, Moller K, Dela F, Kronborg G, Jauffred S, Pedersen BK: Effect of hyperglycemia and hyperinsulinemia on the response of IL-6, TNF-α, and FFAs to low-dose endotoxemia in humans. Am J Physiol Endocrinol Metab 2004, 286: E766-E772. 10.1152/ajpendo.00468.2003
Geerlings SE, Hoepelman AI: Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunol Med Microbiol 1999, 26: 259-265. 10.1111/j.1574-695X.1999.tb01397.x
Pozzilli P, Leslie RD: Infections and diabetes: mechanisms and prospects for prevention. Diabet Med 1994, 11: 935-941.
Almdal T, Scharling H, Jensen JS, Vestergaard H: The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population-based study of 13,000 men and women with 20 years of follow-up. Arch Intern Med 2004, 164: 1422-1426. 10.1001/archinte.164.13.1422
Jee SH, Ohrr H, Sull JW, Yun JE, Ji M, Samet JM: Fasting serum glucose level and cancer risk in Korean men and women. JAMA 2005, 293: 194-202. 10.1001/jama.293.2.194
Van den Berghe GH, Wouters PJ, Bouillon R, Weekers F, Verwaest C, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P: Outcome benefit of intensive insulin therapy in the critically ill: Insulin dose versus glycemic control. Crit Care Med 2003, 31: 359-366. 10.1097/01.CCM.0000045568.12881.10
Van den Berghe GH, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R: Intensive insulin therapy in the critically ill patients. N Engl J Med 2001, 345: 1359-1367. 10.1056/NEJMoa011300
Finney SJ, Zekveld C, Elia A, Evans TW: Glucose control and mortality in critically ill patients. JAMA 2003, 290: 2041-2047. 10.1001/jama.290.15.2041
Guevara RE, Butler JC, Marston BJ, Plouffe JF, File TM Jr, Breiman RF: Accuracy of ICD-9-CM codes in detecting community-acquired pneumococcal pneumonia for incidence and vaccine efficacy studies. Am J Epidemiol 1999, 149: 282-289.
Benesch C, Witter DM Jr, Wilder AL, Duncan PW, Samsa GP, Matchar DB: Inaccuracy of the International Classification of Diseases (ICD-9-CM) in identifying the diagnosis of ischemic cerebrovascular disease. Neurology 1997, 49: 660-664.
Bercault N, Boulain T, Kuteifan K, Wolf M, Runge I, Fleury JC: Obesity-related excess mortality rate in an adult intensive care unit: A risk-adjusted matched cohort study. Crit Care Med 2004, 32: 998-1003. 10.1097/01.CCM.0000119422.93413.08
Resnick HE, Foster GL, Bardsley J, Ratner RE: Achievement of American Diabetes Association clinical practice recommendations among U.S. adults with diabetes, 1999–2002: the National Health and Nutrition Examination Survey. Diabetes Care 2006, 29: 531-537. 10.2337/diacare.29.03.06.dc05-1254
Acknowledgements
The authors thank the staff and participants in the ARIC study for their important contributions. The ARIC study is conducted and supported by the National Heart Lung and Blood Institute (NHLBI) in collaboration with the ARIC Study Investigators. This manuscript was not prepared in collaboration with investigators of the ARIC study and does not necessarily reflect the opinions or views of the ARIC study or the NHLBI. The coauthors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The authors have no funding or support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
KS and RSM designed the study, interpreted the data analysis, and drafted the manuscript. DMM and GSM designed the study, performed and interpreted the data analysis, and drafted the manuscript. DED interpreted the data analysis and revised the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Slynkova, K., Mannino, D.M., Martin, G.S. et al. The role of body mass index and diabetes in the development of acute organ failure and subsequent mortality in an observational cohort. Crit Care 10, R137 (2006). https://doi.org/10.1186/cc5051
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc5051