Abstract
Introduction
The aim of this study was to assess the efficacy of arginine-vasopressin (AVP) as a rescue therapy in catecholamine-refractory septic and non-septic shock in extremely low birth weight (ELBW) infants with acute renal injury.
Methods
Prospective assessment of AVP therapy in three ELBW infants with catecholamine-refractory septic shock and acute renal injury (mean birth weight 600 ± 30 g) and three ELBW infants with non-septic shock and acute renal injury (mean birth weight 770 ± 110 g) at a University hospital. The main outcome measures were restoration of blood pressure with adequate organ perfusion and survival at discharge.
Results
In all three ELBW infants with catecholamine-resistant septic shock, systemic arterial blood pressure increased substantively with restoration of urine output after AVP administration (dosage, 0.035 to 0.36 U/kg/h; length, 70 ± 21 hours). In the three ELBW infants with non-septic shock, only a transient stabilization in mean arterial pressure with restoration of urine output was observed after AVP therapy (dosage, 0.01 to 0.36 U/kg/h; length, 30 ± 16 hours). The mortality rate was 1/3 in the sepsis group versus 3/3 in the non-septic group.
Conclusion
AVP may be a promising rescue therapy in catecholamine-resistant shock in ELBW infants with acute renal injury. Larger prospective clinical trials are warranted to assess the efficacy and safety of AVP as a pressor adjunct in septic versus non-septic shock in ELBW infants.
Similar content being viewed by others
Introduction
Hypotensive, catecholamine-refractory shock is an important cause of morbidity and mortality in critically ill neonates. There is general agreement that there is depressed vasoconstrictor sensitivity to catecholamines in septic shock that can lead to vasodilatation and severe hypotension. Concentrations of vasopressin in plasma are significantly depressed in sepsis while vasopressin secretion is commonly increased in cardiogenic shock [1]. Clinical data indicate that a low serum vasopressin/norepinephrine ratio can predict impending septic shock in adults [2]. Recent clinical studies demonstrated that arginine-vasopressin (AVP) administration is most beneficial in septic patients [3–9]. However, AVP may also be employed successfully in children with states of depressed cardiac function [10].
AVP acts via vascular V1 receptors and renal tubular V2 receptors. V1 receptor stimulation leads to arterial vasoconstriction, and V2 stimulation increases renal free water re-absorption. Although no human data are available on V1 and V2 receptor mechanisms in pre-terms, animal studies demonstrated that the V1-receptor contributes to renal and cardiovascular responses to exogenous AVP in utero at the last third of gestation [11, 12]. Here, we communicate our experience with AVP as a rescue therapy in six extremely low birth weight (ELBW) infants with catecholamine-refractory shock (three septic, three non-septic) and acute renal injury whose hypotension had not responded to prior fluid resuscitation, hydrocortisone therapy and high-dose catecholamine infusion.
Materials and methods
This study was performed at the Department of Neonatology and Paediatric Intensive Care, University Children's Hospital of Saarland, and was conducted in accordance with the policy of our Institutional Review Board and the Helsinki Declaration. Between February 2004 and November 2005, ELBW infants (≤ 1,000 g birth weight) with catecholamine-resistant septic or non-septic shock and acute renal injury were consecutively enrolled.
Definitions of sepsis and septic shock were based on those established by the Society of Critical Care Medicine consensus conference of 1992 and its revised version published in 2003 with modification for normal values in neonates [13, 14]. Non-septic shock was defined as cardio-circulatory failure with concomitant organ dysfunction (renal injury, hyperlactataemia) without an infectious etiology. Low cardiac output was defined as a shortening fraction ≤ 25%. Acute renal injury was based on the RIFLE classification, and included two criteria: glomerular filtration rate (two fold increase in serum creatinine) or urine output <0.5 ml/kg/h for at least six hours [15].
To maintain adequate systemic perfusion, all infants received norepinephrine (NE) and epinephrine (E) in a dose-up manner according to clinical judgements specific to each case, adequate volume resuscitation and hydrocortisone. Diuretic medication consisted of furosemide in varying dosage (0.5 to 2 mg/kg/h). AVP medication was started when patients developed catecholamine-resistant hypotension with inadequate tissue perfusion as demonstrated by acute renal injury and hyperlactataemia (>3 mmol/l). The AVP target dose was 0.01 to 0.12 U/kg/h. The dosage was adjusted according to the clinical course and included AVP bolus if the mean arterial blood pressure (MAP) was < 20 mmHg. After restoration of MAP and urine output, tapering of AVP was attempted.
Stenosis of the renal artery, renal vein thrombosis and post-renal causes for renal injury were excluded in all infants by ultrasonography. Serial echocardiography was performed in all infants to assess left ventricular function. All infants had an arterial line in place for invasive monitoring of arterial blood pressure. Daily laboratory monitoring included arterial blood gas analyses, serum lactate, complete blood count, serum chemistry and microbiological testing for infectious agents (bacterial, fungal, viral) as indicated.
Exclusion criteria to AVP administration included genetic disorders, malformations and diseases incompatible with life, birth weight and weight when included into this study > 1,000 g, sustained cardio-circulatory function by catecholamine administration, uncontrolled haemorrhage, prior hypersensitivity reaction to any constituent of AVP and failure to obtain parental informed consent. Infants with stenosis of the renal artery, renal vein thrombosis and post-renal causes of acute renal injury were also excluded as were infants with cardio-circulatory failure caused by an underlying cardiac pathology that required specific surgical intervention.
Main outcome measures were restoration of blood pressure with adequate organ perfusion and survival at discharge.
Results
Between February 2004 and November 2005 a total of six ELBW infants with catecholamine-resistant septic (two bacterial and one fungal infection) and non-septic shock (two cardiogenic and one circulatory failure secondary to primary disease) and acute renal injury were consecutively enrolled in this study. All infants completed the study protocol. Demographic and clinical details are summarized in Table 1.
AVP dosage was comparable between septic (0.035 to 0.36 U/kg/h) and non-septic (0.01 to 0.36 U/kg/h) infants. Infant 1 was given an initial bolus of AVP (0.025 U) because of severe hypotension (MAP < 20 mmHg). The overall length of AVP administration was 70 ± 21 hours in infants with sepsis versus 30 ± 16 hours in non-septic infants. These differences are due to the early deaths of two twins with cardiogenic shock
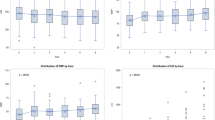
In all six infants, MAP substantially increased within two hours after AVP administration (Figures 1a and 2a). In infants with septic shock, the increase in MAP was paralleled by a moderate decrease in heart rate, while in non-septic shock, the heart rate increased (Figures 1a and 2a).
Cardiovascular parameters and urine output and serum lactate in ELBW infants with sepsis before and after initiation of arginine-vasopressin therapy. (a) Cardiovascular parameters: columns show mean arterial blood pressure (MAP; mmHg); lines show heart rate (beats per minute). Values given as mean ± standard deviation. (b) Urine output and serum lactate: columns show urine output (ml/kg body weight/h); lines show serum lactate (mmol/l). Values given as mean ± standard deviation.
Cardiovascular parameters and urine output and serum lactate in ELBW infants with sepsis before and after initiation of arginine-vasopressin therapy. (a) Cardiovascular parameters: columns show mean arterial blood pressure (MAP; mmHg); lines show heart rate (beats per minute). Values given as mean ± standard deviation. (b) Urine output and serum lactate: columns show urine output (ml/kg body weight/h); lines show serum lactate (mmol/l). Values given as mean ± standard deviation.
At the beginning of AVP medication, all six infants were oligo-anuric. In parallel with the rise in MAP, two hours after starting AVP urine output increased substantially in all six infants (Figures 1b and 2b). However, the rise in urine output was not as pronounced in the two twins with cardiogenic shock (approximately 3 ml/kg/h). Following restoration of MAP, a pronounced decrease in serum lactate was seen in infants 1 and 2 with septic shock while it remained unchanged in infant 3. On the contrary, serum lactate continued to increase despite AVP in the two twins with cardiogenic shock. In infant 6, a transient, non-sustained decrease in serum lactate concentration was noticed.
Possible adverse effects related to AVP medication are detailed in Table 1. No acute side effects were seen (for example, digital and splanchnic hypoperfusion, abdominal distension, bloody stools, necrotizing enterocolitis), or myocardial ischemia, or worsening of metabolic/lactic acidosis that could be related to AVP administration.
The mortality rate was 1/3 in infants with sepsis-induced catecholamine-refractory shock compared to 3/3 in non-septic shock infants.
Discussion
As reported in previous studies in children and adults [3–10], we demonstrated that AVP raised blood pressure in both septic and non-septic infants that was resistant to catecholamines (Figures 1a and 2a). Following restoration of tissue perfusion, a substantial increase in urine output was seen, which is in accordance with recent reports in children and adults with septic shock [3, 9, 16]. In our study, cardiovascular and renal changes induced by AVP were more pronounced and sustained in infants with septic shock, and associated with a fall in serum lactate (Figure 1b). The mortality rate in this group was 1/3. On the contrary, in non-septic infants, only a transient stabilization in cardiovascular and renal function could be achieved (Figure 2a,b). AVP administration did not have an impact on the poor prognosis of the three infants with non-septic catecholamine-resistant hypotension (mortality rate 3/3). The difference in survival rates between septic and non-septic infants cannot be related to the gestational age, birth weight or APGAR score. At the time of starting AVP, however, the three ELBW infants with non-septic catecholamine-resistant shock were in poorer clinical condition as shown by substantially higher serum lactate concentrations and the need for excessive catecholamines (Table 1).
There is still no clear concept of when to start VPA therapy in catecholamine-resistant (septic) shock. Recently, a large clinical study in adults with septic shock demonstrated the beneficial effects of initiating AVP therapy before NE requirements exceed 0.6 μg/kg/minute [17]. This is in accordance with our data, as the two surviving infants received NE and E in a dosage <0.6 μg/kg/minute prior to AVP medication (Table 1). Interestingly, a recent study in animals demonstrated that the combined infusion of NE and AVP improves hemodynamic variables compared with NE alone during sepsis, but not during cardiopulmonary resuscitation [18].
The differential effect of AVP can be related in part to its depletion in septic shock patients with hypersensitivity to exogenous AVP, whereas endogenous AVP release is increased in cardiogenic shock, causing a decreased response to exogenous AVP [1]. A low plasma AVP/NE ratio appears to be useful in predicting septic shock in adults [2]. In a recent study in children with meningococcal septic shock, however, AVP admission levels were appropriately elevated [19]. As we did not measure AVP serum levels, the above suggested mechanisms remain somewhat speculative. However, the prior administration of steroids in our study cohort might have affected endogenous AVP levels because cortisol suppresses the secretion of AVP in certain conditions [20]. Another limitation is the fact that systemic vascular resistances could not be determined in our ELBW infants, and thus it cannot be concluded with certainty that refractory shock was associated with vasoparalysis.
In most pediatric and adult clinical trials that assessed the efficacy of AVP in septic shock, terlipressin, an analogue of AVP with a longer duration of action (half-life of six hours versus six minutes for AVP), was given intermittently and not as a continuous infusion [4, 7, 21]. As hemodynamic profiles may change rapidly in children with septic shock – that is, transformation from hyperdynamic to hypodynamic shock with high systemic vascular resistance [21] – the use of AVP with a shorter time of action seems more appropriate. In one study in children with vasodilatory shock after cardiac surgery, AVP dosage ranged from 0.018 U/kg/h to 0.12 U/kg/h [10]. In another study in adults with vasodilatory septic shock, AVP was given at a rate of 2.4 U/h independent of body weight [6]. In our patients, AVP was administered as a continuous infusion, and titrated to the dosage that restored MAP and renal excretory function. In four infants, the mean dosage was in accordance with the above listed reports; AVP dosage escalation, which was in excess of standard dosage, was necessary in only two infants (non-survivors).
Major side effects of concern associated with AVP therapy are tissue hypoperfusion (mainly splanchnic) and a rebound phenomenon in vascular hyporeactivity with recurrent arterial hypotension [21, 22]. No immediate side effects were seen in the surviving infants. In one infant (patient 6), substantial tissue liver necrosis was seen on autopsy, which could be related to prolonged AVP medication. With NE and E medication being continued after cessation of AVP, no rebound of clinical significance in arterial hypotension was noticed in our study cohort.
Conclusion
This report adds further clinical experience on the use of AVP in catecholamine-refractory shock, indicating that it is also efficacious in ELBW infants. AVP may be a viable rescue therapy for ELBW infants in a refractory vasodilatatory state and acute renal injury when conventional therapies fail. To delineate the role of AVP in catecholamine-resistant shock in ELBW infants, further assessment of AVP safety and efficacy as a pressor adjunct in septic versus non-septic shock is warranted.
Key messages
-
AVP may be a viable rescue therapy for ELBW infants with intractable vasodilatation and acute renal injury to improve systemic arterial blood pressure and restore urine output when conventional inotropics fail.
-
Further evaluation of AVP in larger controlled clinical trials is warranted to assess its efficacy and safety in septic versus non-septic shock in ELBW infants.
Abbreviations
- AVP:
-
= arginine-vasopressin
- E:
-
Epinephrine
- ELBW:
-
= extremely low birth weight infants
- MAP:
-
= mean arterial blood pressure
- NE:
-
= norepinephrine
- PDA:
-
= persistant ductus arteriosus.
References
Landry DW, Levin HR, Gallant EM, Ashton RC Jr, Seo S, D'Alessandro D, Oz MC, Oliver JA: Vasopressin deficiency contributes to the vasodilation of septic shock. Circulation 1997, 95: 1122-1125.
Lin IY, Ma HP, Lin AC, Chong CF, Lin CM, Wang TL: Low plasma vasopressin/norepinephrine ratio predicts septic shock. Am J Emerg Med 2005, 23: 718-724. 10.1016/j.ajem.2005.02.055
Masutani S, Senzaki H, Ishido H, Taketazu M, Matsunaga T, Kobayashi T, Sasaki N, Asano H, Kyo S, Yokote Y: Vasopressin in the treatment of vasodilatory shock in children. Pediatr Int 2005, 47: 132-136. 10.1111/j.1442-200x.2005.02043.x
O'Brien A, Clapp L, Singer M: Terlipressin for norepinephrine-resistant septic shock. Lancet 2002, 359: 1209-1210. 10.1016/S0140-6736(02)08225-9
Liedel JL, Meadow W, Nachman J, Koogler T, Kahana MD: Use of vasopressin in refractory hypotension in children with vasodilatatory shock: Five cases and a review of the literature. Pediatr Crit Care Med 2002, 3: 15-18. 10.1097/00130478-200201000-00004
Tsuneyoshi I, Yamada H, Kakihana Y, Nakamura M, Nakano Y, Boyle WA 3rd: Hemodynamic and metabolic effects of low-dose vasopressin infusions in vasodilatatory septic shock. Crit Care Med 2001, 29: 673-675.
Matok I, Leibovitch L, Vardi A, Adam M, Rubinshtein M, Barzilay Z, Paret G: Terlipressin as a rescue therapy for intractable hypotension during neonatal septic shock. Pediatr Crit Care Med 2004, 5: 116-118. 10.1097/01.PCC.0000112521.93714.B8
Vasudevan A, Lodha R, Kabra SK: Vasopressin infusion in children with catecholamine-resistant septic shock. Acta Paediatr 2005, 94: 380-383.
Matok I, Vard A, Efrati E, Rubinshtein M, Vishne T, Leiboitch L, Adam M, Barzilay Z, Paret G: Terlipressin as a rescue therapy for intractable hypotension due to septic shock in children. Shock 2005, 23: 305-310. 10.1097/01.shk.0000158115.69704.11
Rosenzweig EB, Starc TJ, Chen JM, Culliane S, Timchak DM, Gersony WM, Landry DW, Galantowicz ME: Intravenous arginine-vasopressin in children with vasodilatatory shock after cardiac surgery. Circulation 1999, 100: II182-II186.
Erwin MG, Ross MG, Leake RD, Fisher DA: V1- and V2-receptor contributions to ovine fetal renal and cardiovascular responses to vasopressin. Am J Physiol 1992, 262: R636-643.
Shi L, Guerra C, Yao J, Xu Z: Vasopressin mechanism-mediated pressor responses caused by central angiotensin II in the ovine fetus. Pediatr Res 2004, 56: 756-762. 10.1203/01.PDR.0000141519.85908.68
Bone RC, Balk RA, Cerra FB, Dellinger RP, FEIN AM, Knaus WA, Schein RM, Sibbad WJ: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992, 101: 1644-1655.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen SM, Vincent JL, Ramsay G: SCCM/ESICM/ACCP/ATS/SIS International Sepsis Conference. Crit Care Med 2003, 31: 1250-1256. 10.1097/01.CCM.0000050454.01978.3B
Bellomo R, Ronco C, Kellum JA, Mehta R, Palevsky P, the ADQI workgroup: Acute renal failure-definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 2004, 8: R204-212. 10.1186/cc2872
Albanèse J, Leone M, Delmas A, Martin C: Terlipressin or norepinephrine in hyperdynamic septic shock: A prospective, randomized study. Crit Care Med 2005, 33: 1897-1902. 10.1097/01.CCM.0000178182.37639.D6
Luckner G, Dunser MW, Jochberger S, Mayr VD, Wenzel V, Ulmer H, Schmid S, Knotzer H, Pajk W, Hasibeder W, et al.: Arginine vasopressin in 316 patients with advanced vasodilatatory shock. Crit Care Med 2005, 33: 2659-2666. 10.1097/01.CCM.0000186749.34028.40
Prengel AW, Linstedt U, Zenz M, Wenzel V: Effects of combined administration of vasopressin, epinephrine, and norepinephrine during cardiopulmonary resuscitation in pigs. Crit Care Med 2005, 33: 2587-2591. 10.1097/01.CCM.0000186774.30674.15
Leclerc F, Walter-Nicolet E, Leteurtre S, Noizet O, Sadik A, Cremer R, Fourier C: Admission plasma vasopressin levels in children with meningococcal septic shock. Intensive Care Med 2003, 29: 1339-1344. 10.1007/s00134-003-1868-y
Papanek PE, Sladek CD, Raff H: Corticosterone inhibition of osmotically stimulated vasopressin from hypothalamic-neurohypophysial explants. Am J Physiol 1997, 272: R158-R162.
Berg RA: A long-acting vasopressin analog for septic shock: Brilliant idea or dangerous folly? Pediatr Crit Care Med 2004, 5: 188-189. 10.1097/01.PCC.0000121301.62216.0D
Wilson SJ, Mehta SS, Bellamy MC: The safety and efficacy of the use of vasopressin in sepsis and septic shock. Expert Opin Drug Saf 2005, 4: 1027-1039. 10.1517/14740338.4.6.1027
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SM was responsible for the conception and study design and data acquisition and analysis. SG was involved in data interpretation and drafting the manuscript. AB was responsible for data acquisition and interpretion of data. DW was responsible for data acquisition and drafting the manuscript. LG was involved in data interpretation and drafting the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Meyer, S., Gottschling, S., Baghai, A. et al. Arginine-vasopressin in catecholamine-refractory septic versus non-septic shock in extremely low birth weight infants with acute renal injury. Crit Care 10, R71 (2006). https://doi.org/10.1186/cc4917
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc4917