Abstract
Introduction
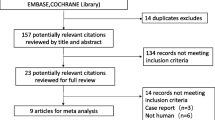
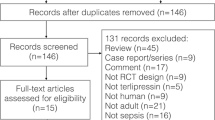
Refractory septic shock has dismal prognosis despite aggressive therapy. The purpose of the present study is to report the effects of terlipressin (TP) as a rescue treatment in children with catecholamine refractory hypotensive septic shock.
Methods
We prospectively registered the children with severe septic shock and hypotension resistant to standard intensive care, including a high dose of catecholamines, who received compassionate therapy with TP in nine pediatric intensive care units in Spain, over a 12-month period. The TP dose was 0.02 mg/kg every four hours.
Results
Sixteen children (age range, 1 month–13 years) were included. The cause of sepsis was meningococcal in eight cases, Staphylococcus aureus in two cases, and unknown in six cases. At inclusion the median (range) Pediatric Logistic Organ Dysfunction score was 23.5 (12–52) and the median (range) Pediatric Risk of Mortality score was 24.5 (16–43). All children had been treated with a combination of at least two catecholamines at high dose rates. TP treatment induced a rapid and sustained improvement in the mean arterial blood pressure that allowed reduction of the catecholamine infusion rate after one hour in 14 out of 16 patients. The mean (range) arterial blood pressure 30 minutes after TP administration increased from 50.5 (37–93) to 77 (42–100) mmHg (P < 0.05). The noradrenaline infusion rate 24 hours after TP treatment decreased from 2 (1–4) to 1 (0–2.5) µg/kg/min (P < 0.05). Seven patients survived to the sepsis episode. The causes of death were refractory shock in three cases, withdrawal of therapy in two cases, refractory arrhythmia in three cases, and multiorgan failure in one case. Four of the survivors had sequelae: major amputations (lower limbs and hands) in one case, minor amputations (finger) in two cases, and minor neurological deficit in one case.
Conclusion
TP is an effective vasopressor agent that could be an alternative or complementary therapy in children with refractory vasodilatory septic shock. The addition of TP to high doses of catecholamines, however, can induce excessive vasoconstriction. Additional studies are needed to define the safety profile and the clinical effectiveness of TP in children with septic shock.
Similar content being viewed by others
Introduction
Septic shock is a severe clinical condition with a complex pathophysiology and poor prognosis despite intensive therapy [1, 2]. In sepsis, a cascade of macrocirculatory and microcirculatory alterations may induce an inability to maintain vasoconstriction, and can lead to severe hypotension [3]. When hypotension becomes refractory to current intensive treatments, the prognosis of septic shock is very poor [4, 5].
Prompted by the desperate situation of patients who fail to respond to aggressive therapy with fluid expansion, vasopressors, inotropes, and other therapies, alternative or complementary vasoconstrictors have been used [3]. Vasopressin (AVP) has potent vasoconstrictive effects mediated via V1 receptors and has been shown effective in catecholamine-resistant hypotension due to septic shock [5–10].
Terlipressin (TP) is a synthetic analog of AVP with a similar pharmacodynamic profile, but with a significantly longer half-life, that has showed promising effects in some case reports of adult patients [11–16] and of children with refractory vasodilatory septic shock [4, 17–19]. On the other hand, concerns have been raised about possible adverse effects of these alternative pressor agents [20–22]. New clinical evidence is therefore needed to define the role of both AVP and TP in vasodilatory septic shock [4, 15, 22, 23].
In the present article, we report the results of the use of TP as a last-resource compassionate therapy in critically ill children with catecholamine-resistant hypotension due to septic shock.
Patients and methods
A prospective, multicenter, observational study was carried out in nine pediatric intensive care units (PICUs) in Spain, during a 12-month period (July 2004–June 2005). Indication of treatment was made by the responsible physician, and administrative authorization was obtained after fulfillment of the strict legal and ethical conditions for compassionate use of drugs required in our country [24]. Briefly, compassionate therapy permits the use of a non-licensed drug or a drug licensed for other indications, outside a clinical trial, in desperate clinical situations where the responsible doctor considers that no other therapeutic alternatives exist and after a specific informed consent process has been carried out.
Inclusion criteria included septic shock with refractory hypotension, defined by an inability to maintain a mean arterial pressure (MAP) above the third percentile for age despite fluid resuscitation and 'high catecholamine doses' (at least 1 µg/kg/min noradrenaline or adrenaline, associated with variable doses of dopamine and/or dobutamine), or evidence of adverse effects of catecholamines (ischemia, arrhythmias). Patients aged from one month to 15 years were eligible. Children with cardiac diseases were excluded.
Due to the lack of specific treatment recommendations, we decided to maintain the TP dosage used in previous pediatric cases [17]: 0.02 mg/kg every four hours by intravenous bolus for a maximum of 72 hours. The main objective of TP treatment was to improve survival of the episode; specific objectives were to achieve and maintain MAP values within the normal range for age and, when possible, to lessen the noradrenaline and adrenaline infusion rates.
Statistical analysis
Values are presented as the median (range). Nonparametric tests were used and intragroup comparisons were performed using the Wilcoxon test. P < 0.05 was considered statistically significant. The inotropic equivalent was calculated by means of a previously described formula [25].
Results
Sixteen children, with ages ranging from one month to 13 years, were included in the study. Patient characteristics are presented in Table 1. Sepsis was caused by Neisseria meningitides in eight cases and by Staphylococcus aureus in two cases; no bacteria were isolated in the remaining six children (sepsis was of nosocomial origin in three cases). At PICU admission, the median (range) Pediatric Logistic Organ Dysfunction score was 23.5 (12–52) and the median (range) Pediatric Risk of Mortality score was 24.5 (16–43). Seven patients already had signs of ischemia at the time TP treatment was considered (Table 1). Six patients had acute renal failure, four patients had coagulopathy, three patients had severe acidosis, two patients had rhabdomyolysis, two patients had acute respiratory distress syndrome, and one patient had refractory intracranial hypertension. Two children had been resuscitated from cardiac arrest (Table 1).
Prior to the start of TP treatment, 15 patients were being mechanically ventilated and ten patients were being treated with continuous renal replacement therapy. Corticosteroids were administered to eight children, and other treatments (antithrombin III, treatment of intracranial hypertension, plasmapheresis, fresh frozen plasma and activated C protein) were each used in one case, respectively. All patients received a combination of at least two catecholamines at high doses. The median (range) rates were 21.5 (10–52) µg/kg/min for dopamine (16 patients), 22.5 (5–40) µg/kg/min for dobutamine (12 patients), 2 (1–4) µg/kg/min for noradrenaline (14 patients), and 1.25 (0.4–4) µg/kg/min for adrenaline (12 patients). Three children also received milrinone, and another child also received digoxine.
TP was started 24 (4–168) hours after admission and was maintained for 24 (3–102) hours (Table 2). The hemodynamic variables and catecholamine infusion rates after TP therapy are summarized in Table 3.
The MAP significantly increased in all patients after TP administration, from 50.5 (37–93) mmHg pre TP administration, to 77 (42–100) mmHg 30 minutes after TP administration, and to 69.5 (41–104) mmHg 1 hour after TP administration (P < 0.05). The heart rate did not change significantly (Table 3).
Treatment with TP permitted a significant reduction in the noradrenaline infusion rate, from 2 (1–4) µg/kg/min pre TP administration, to 1 (0–2.6) µg/kg/min 12 hours after TP administration, and to 1 (0–2.5) µg/kg/min 24 hours later (P < 0.05) (Table 3).
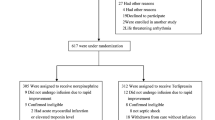
Seven patients showed signs of ischemia prior to TP administration; ischemia persisted or increased with TP treatment in three cases, and improved in four cases (Figure 1). The other nine patients had no signs of ischemia before TP therapy was started. In this subset of nine patients, five developed ischemia possibly related to TP treatment (Figure 1), one of which showed severe limb and intestinal ischemia.
The responsible physicians considered that TP treatment could be also related to other adverse effects: oliguria in two cases, rhabdomyolysis in two cases, hyperkalemia in one case, and hyperbilirrubinemia in another child (Table 2).
Seven patients survived the septic shock episode and nine children died. Causes of death were refractory shock in three cases, refractory arrhythmia in three cases, withdrawal of therapy in two cases, and multiorgan failure in one case (Table 2).
In an adolescent with severe cranial trauma and refractory intracranial hypertension, who developed a nosocomial sepsis with severe hypotension and acute renal failure, TP administration produced severe cutaneous and limb ischemia that was considered by the attending physician a direct factor contributing to death. One infant survived the shock episode but died two weeks later, due to intractable propionic acidemia.
In our patients, the Pediatric Risk of Mortality score or the Pediatric Logistic Organ Dysfunction score, age, sex, the time elapsed until the start of TP administration, the catecholamine infusion rate, the MAP, treatments with steroids, or the length of stay in the PICU were not associated with mortality. Four of the survivors developed sequelae. One patient suffered a major limb amputation, including both lower limbs (below knees) and both hands. Two children suffered the amputation of one finger, and another patient developed dysmetria and partial anopsy. The length of the PICU stay was 8 (1–51) days (Table 2).
Discussion
Septic shock is a very complex condition, characterized by circulatory failure. Its treatment has been based, in addition to antibiotic therapy, on aggressive volume resuscitation and cardiocirculatory support by means of the vasopressor and inotropic effects of catecholamines [1–3, 15, 26, 27]. Despite this approach and intensive care and monitoring, septic shock mortality and morbidity remain very high. New therapies are therefore urgently needed [26, 27].
AVP plasma concentrations are very high in cardiogenic or hypovolemic shock [1, 28]. In septic shock, however, a biphasic response has been recognized, with high levels in the early phase and inappropriately low AVP levels in established septic shock [1, 28, 29]. This evidence and the potent vasopressor effects of AVP prompted its use in vasodilatory septic shock. AVP has been effective in restoring the MAP and vascular tone in adult patients [5–9, 26] as well as in some pediatric case series [10, 30]. AVP has been also beneficial in the treatment of excessive vasodilation associated with cardiopulmonary bypass [31] and in postcardiotomy shock resistant to catecholamine therapy [32–34].
TP is a long-acting synthetic analog of AVP that has also demonstrated significant vasopressor effects in animal models [35, 36], in adult patients with norepinephrine-resistant septic shock [11, 13, 14, 16], and in a few pediatric cases with vasodilatory shock [4, 17–19]. A recently published trial comparing the short-time effects (only six hours) of noradrenaline and TP treatment in adult patients with hyperdynamic septic shock indicates that both drugs are effective in raising the MAP and improving renal function [16].
To our knowledge, results of randomized clinical trials to ascertain the effects of TP treatment, alone or in combination with noradrenaline or other catecholamines, in pediatric vasodilatory septic shock are lacking. The few case reports available [4, 17–19], however, suggest that TP has a possible role in intractable septic shock, an issue that should be explored.
We had previously reported the use of TP in four children with septic shock resistant to high doses of noradrenaline, combined with other catecholamines. In these patients TP therapy induced a rapid and sustained improvement in MAP, which allowed the lessening or even withdrawal of noradrenaline infusion, without related adverse effects. Two patients survived [17].
Matok and colleagues recently reported their retrospective experience with TP therapy in 14 children who suffered 16 septic shock episodes [4]. They observed significant improvements in respiratory and hemodynamic indices shortly after TP treatment. Adrenaline infusion was decreased or stopped in eight patients. Six patients survived. No reference to adverse effects was reported in this group of patients. Although all of the children were considered to be in an extreme state of septic shock, eight patients had undergone correction of congenital heart disease so a component of cardiogenic shock cannot be ruled out, and this fact could interfere with the interpretation of results.
The present study is the first prospective and observational study to report the clinical effects of TP administered as compassionate therapy in children with refractory hypotension due to septic shock. The patients were followed up until death or PICU discharge. To avoid bias, we have excluded patients with cardiac diseases. One-half of the patients had meningococcal purpura fulminans. Despite these differences in the patient characteristics analyzed, our results are comparable with those of Matok and colleagues [4]. We have also observed a significant increase in the MAP that permitted decreasing the noradrenaline infusion rate without changes in the heart rate (Table 3).
Noradrenaline and adrenaline, particularly at high doses, have potent vasoconstrictive effects that can lead to irreversible tissue ischemia [2, 26, 27]. Similar concerns arise when AVP and TP are considered for reversing severe vasodilation in septic shock [15, 21, 23]. When TP is used as a last-resource compassionate therapy, as in the present study, it is added to the previous treatment, which in this case included combinations of catecholamines in high doses. Such a synergy of effects with an increase of previous tissue perfusion insufficiency or its development could therefore be anticipated. In our series, seven patients had signs of ischemia before TP administration; interestingly, while ischemia persisted in three of them, it improved in four children (Figure 1). On the other hand, five out of nine patients without signs of ischemia developed skin and/or limb ischemia after adding TP to the catecholamine dose (Figure 1).
This heterogeneous response is intriguing. We can speculate that improvement of tissue perfusion improvement could be an indirect effect of restoring the MAP and that the development or worsening of ischemia could result from the addition of vasoconstrictive effects of catecholamines and TP or from a direct effect of TP administration. It also appears from our results that TP requirements may have great variability derived from multiple patient characteristics, and the dosage should be titrated according to clinical consequences (balance between positive and adverse effects). One potential strategy in this sense could be to administer a loading dose of TP followed by a goal-directed variable intravenous infusion rate [37].
Another point to be elucidated is the most adequate bolus dose of TP. Due to the lack of specific dosage recommendations, we decided to use the same dosage as that utilized in our previous study [17]: intermittent intravenous doses of 0.02 mg/kg every 4 hours for a maximum of 72 hours. This dose was based on arbitrary extrapolations from doses used for other indications in adults [38, 39] and it was considered a 'low dose'; nonetheless, a subset of patients developed ischemia. Further studies are therefore needed to ascertain the ideal dosage and schedule in children with vasodilatory septic shock. In this sense, a clinical tool to monitor vasoconstriction at tissue level could be very useful. Some case reports have been published in which gastric tonometry [20, 40], the ileal pCO2 gap [41], and the sublingual microcirculatory flow [42] have been used to monitor splanchnic and sublingual microvasculature after treatment with AVP or TP.
Our results indicate that TP may have a role in the therapy of refractory hypotension. TP administration might have influenced the final prognosis of our patients. Moreover, consider that nearly all of our patients had a desperate clinical situation and were treated with TP as a last resource. In our opinion, at least three children were treated in a near-death situation. In this condition, seven of 16 children survived the septic shock episode – a figure similar to that reported by Matok and colleagues [4]. On the other hand, in one case the attending physicians considered that TP was a major factor of the bad outcome, and in two patients they decided on withdrawal of therapy due to severe ischemia, multiple organ failure, and anticipation of non-acceptable sequelae. Only one of seven survivors had severe ischemic sequelae, with amputation of lower limbs below the knees and both hands; another two children suffered the amputation of one finger.
Our study has several limitations. Compassionate use of drugs permits the administration of nonproven therapies, outside clinical trials, in desperate cases; due to this fact, however, the treatment has a high risk of being a delayed, and therefore futile, treatment. It can be argued that if there is a rational indication for the treatment in the light of available evidence, then to have some chance of success TP therapy should be started before the clinical situation becomes so deteriorated that treatment is worthless.
Another drawback is the small number of patients included and the fact that they were gathered from nine different hospitals. This is justified by the fact that vasodilatory septic shock refractory to catecholamines is rare in children [2] and therefore multicenter studies are required. The number of cases precludes statistical analysis to detect factors that are correlated with clinical response, adverse effects, and prognosis.
Also, in order to evaluate the effects of TP administration in further detail, certain additional hemodynamic data, such as systemic vascular resistance, the cardiac index, or calorimetry measurements, could have been very useful. These data were unfortunately not available in most of our patients.
Conclusion
TP therapy is effective for reversing hypotension in children with catecholamine-resistant septic shock. This treatment may cause significant ischemic injury and it should be considered a last-resource treatment in the critical care setting. Our results nevertheless indicate that TP is a promising treatment, and they give support for future controlled clinical trials to assess the efficacy, safety, dosage, and indications of TP in pediatric vasodilatory septic shock.
Key messages
-
TP therapy is effective for reversing hypotension in children with catecholamine-resistant septic shock.
-
TP therapy permitted lowering of the high doses of noradrenaline needed in these patients.
-
TP therapy in combination with catecholamine vasopressors may cause significant ischemic injury.
-
Controlled clinical trials are needed to assess the efficacy, safety, dosage, and indications of TP therapy in pediatric vasodilatory septic shock.
Abbreviations
- AVP:
-
vasopressin
- MAP:
-
mean arterial pressure
- PICU:
-
pediatric intensive care unit
- TP:
-
terlipressin.
References
Landry D, Oliver J: The pathogenesis of the vasodilatory shock. N Engl J Med 2001, 345: 588-595. 10.1056/NEJMra002709
Carcillo JA, Fields AI: Clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit Care Med 2002, 30: 1365-1378. 10.1097/00003246-200206000-00040
Bracco D, Dubois MJ: Hemodynamic support in septic shock: is restoring a normal blood pressure the right target? Crit Care Med 2005, 33: 2113-2114. 10.1097/01.CCM.0000178285.97344.84
Matok I, Vard A, Efrati O, Rubinstein M, Vishne T, Leibovitch L, Adam M, Barzilay Z, Paret G: Terlipressin as rescue therapy for intractable hypotension due to septic shock in children. Shock 2005, 23: 305-310. 10.1097/01.shk.0000158115.69704.11
Malay MB, Ashton RCJ, Landry DW, Townsend RN: Low-dose vasopressin in the treatment of vasodilatory septic shock. J Trauma 1999, 47: 699-705.
Dünser MW, Mayr AJ, Ulmer H, Ritsch N, Knotzer H, Pajk W, Luckner G, Mutz NJ, Hasibeder WR: The effects of vasopressin on systemic hemodynamics in catecholamine-resistant septic and postcardiotomy shock: a retrospective analysis. Anesth Analg 2001, 93: 7-13. 10.1097/00000539-200107000-00003
Tsuneyoshi I, Yamada H, Kakihana Y, Nakamura M, Nakano Y, Boyla WA: Hemodynamic metabolic effects of low-dose vasopressin infusions in vasodilatory septic shock. Crit Care Med 2001, 29: 487-493. 10.1097/00003246-200103000-00004
Holmes CL, Walley KR, Chittock DR, Lehman T, Russell JA: The effects of vasopressin on hemodynamics and renal function in severe septic shock: a case series. Intensive Care Med 2001, 27: 1416-1421. 10.1007/s001340101014
Patel BM, Chittock DR, Russell JA, Walley KR: Beneficial effects of short-term vasopressin infusion during severe septic shock. Anesthesiology 2002, 96: 576-582. 10.1097/00000542-200203000-00011
Liedel JL, Meadow W, Nachman J, Koogle T, Kahana MD: Use of vasopressin in refractory hypotension in children with vasodilatory shock: five cases and review of the literature. Pediatr Crit Care Med 2002, 3: 15-18. 10.1097/00130478-200201000-00004
O'Brien A, Clapp L, Singer M: Terlipressin for norepinephrine-resistant septic shock. Lancet 2002, 359: 1209-1210. 10.1016/S0140-6736(02)08225-9
Fellahi JL, Benard P, Daccache G, Mourgeon E, Gerard JL: Vasodilatory septic shock refractory to catecholamines: is there a role for terlipressin? Ann Fr Anesth Reanim 2003, 22: 631-634. 10.1016/S0750-7658(03)00218-1
Leone M, Albanese J, Delmas A, Chaabane W, Garnier F, Martin C: Terlipressin in catecholamine-resistant septic shock patients. Shock 2004, 22: 314-319. 10.1097/01.shk.0000136097.42048.bd
Morelli A, Rocco M, Conti G, Orecchioni A, De Gaetano A, Cortese G, Coluzzi F, Vernaglione E, Pelaia P, Pietropaoli P: Effects of terlipressin on systemic and regional haemodynamics in catecholamine-treated hyperkinetic septic shock. Intensive Care Med 2004, 30: 597-604. 10.1007/s00134-004-2244-2
Delmas A, Leone M, Rousseau S, Albanese J, Martin C: Clinical review: vasopressin and terlipressin in septic shock patients. Crit Care 2005, 9: 212-222. 10.1186/cc2945
Albanèse J, Leone M, Delmas A, Martin C: Terlipressin or norepinephrine in hyperdynamic septic shock: a prospective, randomized study. Crit Care Med 2005, 33: 1897-1902. 10.1097/01.CCM.0000178182.37639.D6
Rodriguez-Núñez A, Fernández-Sanmartin M, Martinón-Torres F, González-Alonso N, Martinón-Sánchez JM: Terlipressin for catecholamine-resistant septic shock in children. Intensive Care Med 2004, 30: 477-480. 10.1007/s00134-003-2114-3
Matok I, Leibovitch L, Vardi A, Adam M, Rubinstein M, Barzilay Z, Paret G: Terlipressin as rescue therapy for intractable hypotension during neonatal septic shock. Pediatr Crit Care Med 2004, 5: 116-118. 10.1097/01.PCC.0000112521.93714.B8
Peters MJ, Booth RA, Petros AJ: Terlipressin bolus induces systemic vasoconstriction in septic shock. Pediatr Crit Care Med 2004, 5: 112-115. 10.1097/01.PCC.0000112366.62864.BD
Dünser MW, Mayr AJ, Tür A, Pajk W, Barbara F, Knotzer J, Ulmer H, Hasibeder WR: Ischemic skin lesions as a complication of continuous vasopressin infusion in catecholamine-resistant vasodilatory shock: incidence and risk factors. Crit Care Med 2003, 31: 1394-1398. 10.1097/01.CCM.0000059722.94182.79
Asfar P: Terlipressin in chronic hyperdynamic endotoxic shock: is it safe? Intensive Care Med 2003, 29: 154-155.
Westphal M, Bone HG, Van Aken H, Sielenkämper AW: Terlipressin for haemoynamic support in septic patients: a double-edged sword? Lancet 2002, 360: 1250-1251. 10.1016/S0140-6736(02)11253-0
Berg RA: A long-acting vasopressin analog for septic shock: brilliant idea or dangerous folly? Pediatr Crit Care Med 2004, 5: 188-189. 10.1097/01.PCC.0000121301.62216.0D
Ministry of Health: Royal Decree 223/2004, of February 6th, that regulates clinical trials with drugs. Volume 33. BOE (Official State Bulletin); 2004:5429-5443.
Chen Y, Yu H, Huang S, Chiu K, Lin T, Lai L, Lin F, Wang S, Chu S, Ko W: Experience and result of extracorporeal membrana oxygenation in treating fulminant myocarditis with shock: what mechanical support should be considered first? J Heart Lung Transplant 2005, 24: 81-87. 10.1016/j.healun.2003.09.038
Mullner M, Urbanek B, Havel C, Losert H, Waechter F, Gamper G: Vasopressors for shock. Cochrane Database Syst Rev 2004, 3: CD003709.
Holmes CL: Vasoactive drugs in the intensive care unit. Curr Opin Crit Care 2005, 11: 413-417. 10.1097/01.ccx.0000176696.70013.da
Landry DW, Levin HR, Gallant EM, Ashton RC, Seo S, D'Alesandro D, Oz MC, Oliver JA: Vasopressin deficiency contributes to the vasodilatation of septic shock. Circulation 1997, 95: 1122-1125.
Leclerc F, Walter-Nicolet E, Leteurtre S, Noizet O, Sadik A, Cremer R, Fourier C: Admission plasma vasopressin levels in children with meningococcal septic shock. Intensive Care Med 2003, 29: 1339-1344. 10.1007/s00134-003-1868-y
Vasudevan A, Lodha R, Kabra SK: Vasopressin infusion in children with catecholamine-resistant septic shock. Acta Paediatr 2005, 94: 380-383.
Argenziano M, Chen JM, Choudhri AF, Cullinane S, Garfein E, Weinberg AD, Smith CR, Rose EA, Landry DW, Oz MC: Management of vasodilatory shock after cardiac surgery: identification of predisposing factors and use of novel pressor agent. J Thorac Cardiovasc Surg 1998, 116: 973-980. 10.1016/S0022-5223(98)70049-2
Argenziano M, Chen JM, Cullinane S, Choudri AF, Rose EA, Smith CR, Edwards NM, Landry DW, Oz MC: Arginine vasopressin in the management of vasodilatory hypotension after cardiac transplantation. J Heart Lung Transplant 1999, 18: 814-817. 10.1016/S1053-2498(99)00038-8
Dunser MW, Mayr AJ, Satllinger A, Ulmer H, Ritsch N, Knotzer H, Pajk W, Mutz NJ, Hasibeder WR: Cardiac performance during vasopressin infusion in postcardiotomy shock. Intensive Care Med 2002, 28: 746-751. 10.1007/s00134-002-1265-y
Rosenzweig EG, Starc TJ, Chen JM, Cullinane S, Timchack DM, Gersony WM, Landry DW, Galantowicz ME: Intravenous arginine-vasopressin in children with vasodilatory shock after cardiac surgery. Circulation 1999, 100: II182-II186.
Scharte M, Meyer J, Van Aken H, Bone HG: Hemodynamic effects of terlipressin (a synthetic analog of vasopressin) in healthy and endotoxemic sheep. Crit Care Med 2001, 29: 1756-1760. 10.1097/00003246-200109000-00017
Ouattara A, Landi M, Le Manach Y, Lecomte P, Leguen M, Boccara G, Coriat P, Riou B: Comparative cardiac effects of terlipressin, vasopressin and norepinephrine on an isolated perfused rabbit heart. Anesthesiology 2005, 102: 85-92. 10.1097/00000542-200501000-00016
Zeballos G, López-Herce J, Fernández C, Brandstrup KB, Rodríguez-Núñez A: Rescue therapy with terlipressin by continuous infusion in a child with catecholamine-resistant septic shock. Resuscitation 2006, 68: 151-3. 10.1016/j.resuscitation.2005.06.016
Ioannou G, Doust J, Rockey DC: Terlipressin for acute esophageal variceal hemorrhage [Cochrane review]. Cochrane Database Syst Rev 2003, 1: CD002147.
Moreau R: Hepatorenal syndrome in patients with cirrhosis. J Gastroenterol Hepatol 2002, 17: 739-747. 10.1046/j.1440-1746.2002.02778.x
Van Haren FMP, Rozendaal FW, van der Hoeven JG: The effect of vasopressin on gastric perfusion in catecholamine-dependent patients in septic shock. Chest 2003, 124: 2256-2260. 10.1378/chest.124.6.2256
Sun Q, Dimopoulos G, Nguyen NC, Tu Z, Nagy N, Hoang AD, Rogiers P, De Backer D, Vincent JL: Low-dose vasopressin in the treatment of septic shock sheep. Am J Respir Crit Care Med 2003, 168: 481-486. 10.1164/rccm.200205-447OC
Boerma EC, Van der Voort PHJ, Ince C: Sublingual microcirculatory flow is impaired by the vasopressin-analogue terlipressin in a patient with catecholamine-resistant septic shock. Acta Anaesthesiol Scand 2005, 49: 1387-1390. 10.1111/j.1399-6576.2005.00752.x
Acknowledgements
This study received partial funding from Ferring, S.A., Madrid, Spain that consisted of the organization of two working meetings of the members of the RETSPED Working Group of the Spanish Society of Pediatric Intensive Care. José María Bellón, from the Preventive Service of Gregorio Marañón Hospital (Madrid), reviewed the statistical methods and contributed with helpful comments.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests. This study was partially supported by Ferring, S.A., Madrid, Spain (organization of two working meetings).
Authors' contributions
ARN conceived, designed, and coordinated the study, reviewed all necessary material, performed statistical analysis, and wrote the initial and successive drafts. JLH participated in the design of the study and critically reviewed the drafts. JGA and AH critically reviewed the drafts of the manuscript. CR assisted with study design and assessment of manuscript. ARN, JLH, JGA, AH, CR, and other members of the RETSPED Working Group of the Spanish Society of Pediatric Intensive Care (VM, CPC, ASG, JDLC, MTH, AM, and FMT) participated in the working meetings, discussed the design of the study, were in charge of the reported patients, and fulfilled the case records. All authors gave final approval of the version to be published.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Rodríguez-Núñez, A., López-Herce, J., Gil-Antón, J. et al. Rescue treatment with terlipressin in children with refractory septic shock: a clinical study. Crit Care 10, R20 (2006). https://doi.org/10.1186/cc3984
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc3984