Abstract
Introduction
Hospital-acquired pneumonia after surgery is one of the major causes of septic shock. The excessive inflammatory response appears to be responsible for the increased susceptibility to infections and subsequent sepsis. The primary aim of this study was to investigate immune parameters at the onset of pneumonia, before the development of subsequent septic shock. The secondary aim was to investigate the usefulness of these immune parameters in predicting progression from hospital-acquired pneumonia to septic shock.
Methods
This propective clinical study included 76 patients with the diagnosis of hospital-acquired pneumonia. Approval was obtained from the local institutional ethics committee and relatives of the patients gave informed consent. Of the 76 patients, 29 subsequently developed septic shock. All patients were included within 4 h of establishing the diagnosis of hospital-acquired pneumonia (first collection of blood samples and the analysis of immune mediators). In addition, we defined early (within 12 h of onset of septic shock) and late (within 72 to 96 h of onset) stages of septic shock for the collection of blood samples and the analysis of immune mediators. The immune parameters tumor necrosis factor-α, IL-1β, IL-6, IL-8 and IL-10 as well as the endothelial leucocyte adhesion molecule were analyzed.
Results
In the pneumonia group with subsequent septic shock, levels of IL-1β, IL-6, IL-8 and IL-10 were significantly increased before the onset of septic shock compared to patients without subsequent septic shock. This progression was best predicted by IL-1β, IL-6, IL-8 and IL-10 (area under the curve ≥ 0.8).
Conclusion
At the onset of hospital-acquired pneumonia, a significant relevant systemic cytokine mediated response had already been initiated. It might, therefore, be possible to identify patients at risk for septic shock with these predictive markers during early pneumonia. In addition, immune modulating therapy might be considered as adjuvant therapy.
Similar content being viewed by others
Introduction
Hospital-acquired pneumonia (HAP) is the most common nosocomial infection and its prevalence within the intensive care unit (ICU) setting ranges from 31% to 47% [1–4]. The mortality rate for HAP remains high at 20% to 50% [5–7]. HAP in surgical patients is especially characterized by the high frequency of early onset infections and the high proportion of Gram-negative bacteria and staphylococci isolated [8]. Mortality rates are between 19% and 45% for patients who contract postoperative pneumonia after major surgery [9]. A review by Friedman et al. [10] shows that incidents of HAP as a cause of septic shock have increased in the past decades and this has been accompanied by only a limited improvement in survival. In addition, the study of Martin et al. [11] shows that HAP as a cause of septic shock was associated with a poor outcome and significantly higher mortality (82%; p < 0.03) compared to wound infections and urinary tract infections.
Several studies indicate that a causal relationship exists between the surgical injury and the predisposition of these patients to develop infectious and septic complications [12, 13]. The excessive inflammatory response with alteration of cell-mediated immunity following major surgery appears to be responsible for the increased susceptibility to subsequent infection and sepsis [13]. In particular, the regulation of the inflammatory response in bacterial pneumonia is dependent on complex interactions between alveolar macrophages, polymorphonuclear leukocytes, immune cells and local production of both pro- and anti-inflammatory cytokines as well as vascular adhesion molecules [14–16]. The cytokines secreted by phagocytes in response to infection include tumor necrosis factor (TNF)-α, IL-1β, IL-6, IL-8 as well as IL-10 [14]. Interleukins are increasingly recognized as early mediators of the host inflammatory response to a variety of infectious agents. On one hand, cytokines can leak from the inflammatory sites in the lung as the normal compartmentalization of inflammation is lost during severe local infection [17, 18]. Alternatively, cytokines may be produced in the systemic compartment in response to bacterial products, such as endotoxin, that leak from the lungs into the circulation [19–21]. Parsons et al. [22] have provided the strongest evidence to date that IL-6, IL-8 and IL-10 are useful circulating markers for the intensitiy of the inflammatory response in the lungs and the prognosis of patients at the onset of lung injury. High elevated plasma levels of IL-6 and IL-8 have been associated with higher mortality rates [23–25].
To the best of our knowledge, no other study to date has investigated the systemic progression of HAP to septic shock with respect to the pattern of circulating cytokines in surgical patients.
The primary aim of this study was to investigate whether patients, within four hours of a HAP diagnosis, differed in their pro- and anti-inflammatory cytokine and adhesion molecule patterns before the development of septic shock. The secondary aim was to evaluate whether any of these markers had a predictive value for the progression of HAP to septic shock.
Materials and methods
This study was approved for an operative ICU. After receiving both the approval of the institutional ethics commitee and written informed consent from patients relatives or legal representatives, 76 patients were included. All patients were surgical patients (major abdominal, neurosurgical, trauma). The patients were allocated to two groups: HAP without septic shock and HAP with subsequent septic shock. HAP was diagnosed according to the criteria of the American Thoracic Society 1996 [2]. Patients were included within 4 h after the onset of HAP. Exclusion criteria were patients younger than 18 years old, acute myocardial ischemia, any corticosteroid therapy or chemotherapy, acute respiratory distress syndrome (ARDS), acute lung injury and heart insufficiency. A diagnosis of pneumonia was made if systemic signs of infection were present, new or worsening infiltrates were seen on the chest X-ray, and new onset of purulent sputum or a change of sputum with bacteriologic evidence in the endotracheal aspirate was found [26, 27]. Subsequent septic shock criteria were defined as outlined in the Consensus Conference 1992 [28]. In particular, we defined early (within 12 h of onset) and late (within 72 to 96 h of onset) stages of septic shock.
The collection of blood samples for the analysis of immune mediators, were drawn in all patients (with and without subsequent septic shock) at the time of HAP diagnosis within the first 4 h after onset. In patients with HAP and subsequent septic shock, blood samples were obtained at the early stage (within 12 h of onset) as well the late stage (within 72 to 96 h of onset) of subsequent septic shock.
All blood samples were collected in sterile tubes and centrifuged; the supernatants were stored in liquid nitrogen at -70°C. All mediators were analyzed at 23°C using a sandwich enzyme-linked immunosorbent assay (Quantikine™ Immunoassay Kit, R&D Systems, Minneapolis, MN, USA). Detection limits were: IL-1β, 0.1 pg/ml (intra- and interassay variation coefficients 3.0% and 12.5%, respectively); IL-6, 3 pg/ml (4.6%, 12.1%); IL-8, 8 pg/ml (5%, 11.1%); IL-10, 5 pg/ml (3.0%, 7.0%); TNF-α, 4.4 pg/ml (4.6%, 5.8%); E-selectin, 2 ng/ml (3.2%, 6.4%).
Routine laboratory parameters, including leucocytes, C-reactive protein (CRP), lactate and platelets, were determined two times a day. All patients were mechanically ventilated and received a continuous analgosedation with either propofol/fentanyl or midazolam/fentanyl. Basic patient characteristics, the microbiological etiology pneumonia, the Acute Physiology and Chronic Health Evaluation (APACHE) III score [29] and the Multiple Organ Failure (MOF) score [30] were documented. The researchers who performed the laboratory analyses were blinded to data collection, diagnosis of pneumonia and ICU outcome. Furthermore, the diagnosis of HAP made by clinicians on the ICU was seen and confirmed by two blinded researchers.
A radial artery catheter and a central-venous catheter were inserted as routine monitoring in all patients. A pulmonary artery catheter was inserted as routine cardiovascular monitoring for the 29 patients with subsequent septic shock. Arterial and mixed-venous blood gases were performed in all patients with septic shock to determine oxygen-transport related variables, in particular oxygen delivery and oxygen consumption via standard formulae. Volume resuscitation (crystalloids, colloids and blood transfusions) was performed to achieve an optimal left arterial pressure, which was estimated by the pulmonary capillary wedge pressure reaching the plateau value for left ventricular stroke work. If the cardiac index was <2.5 l/minute/m2, 3 to 10 ug/kg/minute dobutamine was administered to maintain the cardiac index between 3.0 and 3.5 l/minute/m2. If mean arterial pressure was below the level of 70 mmHg, norepinephrine was administered to obtain a mean arterial pressure between 70 and 90 mmHg [31]. Steroids were given in patients at the time of septic shock according to additive therapy, especially in patients who exhibited a poor response to the primary vasopressor agent [31].
Statistics
All data are expressed as median and 25/75 percentile. Statistical analysis between groups (HAP patients with and without subsequent septic shock) was performed using the Mann-Withney U test (intergroup analysis). The receiver operating curve was plotted to provide a graphical presentation of the relationship between sensitivity and specificity of the mediators covering all possible diagnostic cutoff levels. The area below the receiver operating curve (AUC) represents the probability of septic shock developing in a patient with pneumonia [32]. Statistical analysis of the pneumonia patients with subsequent septic shock (intragroup analysis) was performed using the Friedman test to show significant differences between pneumonia and early and late septic shock. When the global test revealed a significant difference, the Wilcoxon matched-pairs signed-rank test was then used to decide whether or not pneumonia and early and late septic shock differed locally. The Chi-square test was used to test statistical differences between dichotomous variables. A p < 0.05 was considered significant.
Results
Out of a total of 76 patients with HAP, 29 patients developed subsequent septic shock. Basic patient characteristics as well as the etiology of pneumonia (Gram-positive/Gram-negative) did not differ significantly between the two groups (Table 1). In the pneumonia group without septic shock, Gram-positive species were isolated from 18 patients (Staphylococcus aureus, Enterococcus faecium, Enterococcus faecalis), whereas Gram-negative species were isolated from 21 patients (Pseudomonas aeruginosa, Proteus mirabilis, Klebsiella pneumoniae, Enterobacter cloacae). In the pneumonia group with subsequent shock, eight patients had Gram-positive pulmonary infection (Staphylococcus aureus, Enterococcus faecium, Enterococcus faecalis), whereas Gram-negative species were isolated from 15 patients (Pseudomonas aeruginosa, Proteus mirabilis, Klebsiella pneumoniae, Enterobacter cloacae).
At the 'diagnosis of pneumonia', the clinical and laboratory findings did not significantly differ between the groups (Table 2). The time from admission to the ICU to the time of diagnosis of pneumonia did not differ between the groups (p < 0.37; Table 2). In the pneumonia group with subsequent septic shock, the time from diagnosis of pneumonia to the onset of early septic shock was 75 h (range 30 to 85 h), from early septic shock to late septic shock 78 h (range 17 to 103 h). None of the patients of the septic shock group had septic shock at the time of diagnosis of pneumonia. The progression from pneumonia to septic shock showed a significant increase in APACHE III and MOF scores as well in levels of leucocytes, although there was no significant increase in the levels of C-reactive protein, lactate and platelets (Table 3).
Immune modulating mediators and clinical parameters at the onset of pneumonia and during subsequent septic shock
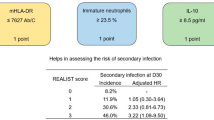
At the 'diagnosis of pneumonia', TNF-α, IL-1β, IL-6, IL-8, IL-10 and E-selectin were significantly increased in those patients who had subsequent septic shock, compared to patients with pneumonia without subsequent septic shock (Table 4). The AUC of IL-1β, IL-6, IL-8 and IL-10 ranged from 0.80 to 0.82 (Fig. 1a,b). In addition, routine laboratory parameters, such as levels of lactate, leucocytes and C-reactive protein as well as APACHE III and MOF scores, did not differ between the groups. The AUC of leukocytes and C-reactive protein ranged from 0.34 to 0.58 (Fig. 1c).
Predictive value of immune modulating parameters and conventional laboratory parameters at hospital-acquired pneumonia diagnosis. (a) Area under the receiver operating curve (AUC) for IL-6, IL-8 and IL-1β (*p < 0.05). (b) AUC for IL-10 (*p < 0.05). (c) AUC for C-reactive protein (CRP). Ns, not significant.
TNF-α and E-selectin increased significantly in 'early' septic shock. From 'early' to 'late' septic shock, significant decreases were observed in TNF-α, IL-1β, IL-6, and E-selectin (Table 3).
Hemodynamic and oxygen-related parameters in septic shock patients
None of the patients in both the non-septic and the septic shock group had pre-existing ARDS or fulfilled the criteria of ARDS at the diagnosis of pneumonia. None of the patients of either group had bilateral infiltrates in the chest X-ray as a radiomorphological correlate for the diagnosis of ARDS. The heart rate of patients with septic shock was significantly higher in the late phase of septic shock. In addition, oxygen consumption was significantly higher in early septic shock.
ICU stay and outcome in patients without and with septic shock
ICU stay did not differ between both groups. In contrast, the survival rate was significantly higher in patients without septic shock (Table 5). For 12 patients (5 patients without subsequent septic shock and 7 patients with subsequent septic shock), initial inappropriate antibiotic therapy was changed immediately according to the specific bacterial strains isolated. No significant differences in inflammatory parameters were found in these patients compared to patients who received initial adequate therapy.
Discussion
The most important result of this study was the detection of an already increased immune response with respect to circulating cytokines at the onset of HAP in all patients with subsequent septic shock compared to those without subsequent septic shock. In particular, IL-1β, IL-6, IL-8 and IL-10 were most predictive for the progression of septic shock (area under the curve ≥ 0.80). Furthermore, in our study, laboratory markers were not predictive for the progression of HAP to septic shock, which is in accordance with other clinical studies [11].
To the best of our knowledge, no other study to date has investigated the systemic progression of HAP to septic shock in surgical patients with respect to immune modulating cytokines, adhesion molecules, their systemic release and their possible predictive value.
In our study, increased serum levels of IL-1β, IL-6, IL-8 and IL-10 were found at the onset of HAP and had a predictive value (area under the curve ≥ 0.80) for the progression to septic shock. An increase in levels of IL-6 and IL-10 has been reported after different types of surgery [33, 34]. Furthermore, different early proinflammatory cytokine responses, as well as exaggerated increases in IL-10, are associated with later onset of infections [35, 34]. Brede et al. [35] demonstrated an immediate increase in plasma TNF-α levels in peritonitis patients, which was predictive for the development of subsequent septic shock. None of the patients had septic shock at the diagnosis of peritonitis, which is in accordance with our findings. In addition, Sander et al. [36] found decreased IL-6/IL-10 levels in patients immediately after surgery of the upper gastrointestinal tract, which was associated with an increased risk of postoperative infections. Spies et al. [37] reported an immediate increased IL-10 response, which was associated with the later onset of postoperative infections. Even if the above mentioned studies are not fully comparable to our study, the postoperative and early immediate increase of cytokines, especially IL-10, IL-1β, IL-8 and IL-6, might be explained as an exaggerated and imbalanced pro- and anti-inflammatory immune response after surgery.
In general, a clinical complication of HAP is the dissemination of bacteria from the pulmonary airspace into the bloodstream, resulting in bacteremia concurrent with the localized infection [38, 39]. In addition to direct bacterial phagocytosis, alveolar macrophages secrete a variety of cytokines and chemokines capable of activating blood neutrophils and monocytes in the pulmonary microenvironment [38]. Furthermore, inability to clear bacteria from the bloodstream can lead to a high exposure to endotoxin and subsequent septic shock [39, 40]. The cytokines secreted by phagocytes in response to infection include TNF-α, IL-1β, IL-6, IL-8 and IL-10 [14]. In accordance with our findings, Bonten et al. [23] showed that ventilator-associated pneumonia in patients with severe sepsis and septic shock was accompanied by increased levels of IL-6 and IL-8 at the time of diagnosis, and even two days after diagnosis, compared to control patients without ventilator-associated pneumonia. Furthermore, Meduri et al. [41] found a persistent elevation of the cytokines TNF-α, IL-1β, IL-6 and IL-10 after the diagnosis of adult respiratory distress syndrome, which predicted a poor outcome and severe sepsis and septic shock. In contrast, Friedland et al. [10] found that circulating levels of IL-6, IL-8 and IL-1β poorly correlated with the clinical severity of illness of ICU patients and only the presence of TNF-α in plasma was an independent predictor of mortality. However, it is difficult to make comparisons to the study of Friedland et al. [10] because of its heterogenous patient population (surgical and medical emergencies). In addition no differentiation with respect to the infectious focus was made in the study of Friedland et al. [10].
Experimental investigations documented a leakage of pro-inflammatory parameters from the infected lung [17], which caused increased systemic levels of pro- and anti-inflammatory cytokines in the circulation [17, 18]. In an experimental rabbit model, Kurahashi et al. [18] studied the pathogenesis of septic shock in Pseudomonas aeruginosa pneumonia with lung instillation of a cytotoxic PA 103, which caused a significant bacterial-induced alveolar epithelial injury and a progressive increase in the circulating pro-inflammatory cytokines TNF-α and IL-8. Pretreatment with systemic administration of anti-TNF-α serum or rh-IL-10 blocked the increase of pro-inflammatory mediators in the circulation and prevented hypotension and decreased cardiac output. Our impression is that this experimental setting indicates that systemic inflammation is already present at an early stage of infection and that specific immune parameters are related to the focus of infection and might thus be used to predict a worse outcome.
In our study, the outcome was significantly different between groups. Of 29 patients with subsequent septic shock, 13 (44.8%) died. This is in accordance with previous studies [3, 23, 42]. In the study of Bonten and coworkers [23], the mortality rate for ventilator-associated pneumonia patients with subsequent septic shock was 60%. Ibrahim et al. [3] studied 301 patients receiving mechanical ventilation. The mortality rate of patients who developed ventilator-associated pneumonia (45.5%) was significantly greater than the mortality rate of patients without ventilator-aquired pneumonia (32.2%, p < 0.004). Almiralli et al. [42] studied a total of 127 patients with community-aquired pneumonia (45.7%) and HAP (54.3%). Of the patients with HAP, 18.8% developed subsequent septic shock, which was associated with an increased mortality (66%). In addition, other predictive variables, such as a Simplified Acute Physiology II Score >12, mechanical ventilation and advanced age (>70 years) were associated with a 99% probability of a fatal outcome [42]. In contrast to the studies mentioned above, the APACHE III and MOF scores in our study were not predictive at the onset of HAP for the progression to subsequent septic shock. It is difficult, however, to compare these studies to our study because of their different patient populations and study designs.
A relationship between elevated levels of cytokines and both a clinical condition of severe sepsis or septic shock and mortality have been demonstrated repeatedly [20, 23]. It has been suggested that systemically stimulated immune parameters may predict a worse outcome [20, 23], which is in accordance with our study as progression from HAP to septic shock was associated with an early increase in the above mentioned cytokines prior to the development of septic shock. The subsequent decrease of nearly all immune modulating parameters during late septic shock may be considered as an immune breakdown, indicating an immune paralytic effect. This has been shown already in patients with peritonitis and subsequent septic shock [35]. The significant increase in MOF and APACHE III scores during early and late septic shock reflect the severity of septic shock and the development of multiple organ failure [43].
Limitations of the study
In this study, we did not perform a bronchial lavage procedure or determine cytokine levels in the bronchial lavage. This might be a limitation of this study, but direct examination of reliable respiratory tract samples cannot be relied upon solely [44]. Even if previous studies demonstrated elevated levels of IL-8 and IL-10 in the bronchial lavage of injured patients at the time of admission, which was associated with subsequent nosocomial pneumonia, this was not predictive for the development of subsequent septic shock [45]. The exact timing of HAP diagnosis was taken into consideration according to the precisely defined criteria of the American Thoracic Society 1996 [2] and is essential for timely administration of appropriate antibitiotic therapy [28, 44]. The sepsis definition is much more difficult and was performed according to the American College of Chest Physicians and Society of Critical Care Medicine 1992 [28]. Whereas it cannot be ruled out that 12 patients received inappropriate initial antibiotic therapy, no significant differences were observed for them with respect to outcome and inflammatory parameters.
Conclusion
In this study, a significant and clinically relevant systemic cytokine mediated response had already been initiated at the onset of HAP. This prestimulated response had a better predictive capacity for subsequent septic shock than conventional laboratory values. In HAP patients with subsequent septic shock, IL-1β, IL-6, IL-8 and IL-10 were superior predictive markers than TNF-α, E-selectin and conventional laboratory values and scores at the time of pneumonia diagnosis. It is possible, therefore, to identify patients at risk of septic shock in early pneumonia with these predictive markers.
Key messages
-
At the time of HAP diagnosis, TNF-α, IL-1β, IL-6, IL-8, IL-10 and E-selectin were significantly increased in pneumonia patients with subsequent septic shock compared to patients without subsequent septic shock.
-
In particular, IL-1β, IL-6, IL-8, and IL-10 were most predictive for the progression of septic shock (area under the curve ≥ 0.8).
-
Conventional laboratory markers as well as APACHE III and MOF scores were not predictive for subsequent septic shock.
-
At the time of HAP diagnosis, a significant and clinically systemic cytokine mediated response had already been initiated and had predictive capacity for subsequent septic shock.
-
In the clinical context, it might be possible to identify patients at risk of septic shock in early HAP with predictive markers.
Abbreviations
- ARDS:
-
acute respiratory distress syndrome
- AUC:
-
area under curve
- CRP:
-
C-reactive protein
- HAP:
-
hospital-acquired pneumonia
- ICU:
-
intensive care unit
- IL:
-
interleukin
- TNF:
-
tumor necrosis factor.
References
Vincent JL: Nosocomial infections in adult intensive care units. Lancet 2003, 361: 2068-2077. 10.1016/S0140-6736(03)13644-6
American Thoracic Society: Hospital-aquired pneumonia in adults: diagnosis, assessment of severity, initial antimicobial therapy, and preventive strategies. Am J Respir Crit Care Med 1996, 153: 1711-1725.
Ibrahim EH, Ward S, Sherman G, Schaiff R, Fraser VJ, Kollef MH: Experience with clinical guideline for the treatment of ventilator-associated pneumonia. Crit Care Med 2001, 29: 1109-1115. 10.1097/00003246-200106000-00003
Rodriguez JL, Gibbons JK, Bitzer LG, Dechert RE, Steinberg SM, Flint LM: Pneumonia: incidence, risk factors, and outcome in injured patients. J Trauma 1991, 31: 907-914.
McEachern R, Campbell GD Jr: Hospital-acquired pneumonia: epidemiology, etiology, and treatment. Infect Dis Clin North Am 1998, 12: 761-779.
Craig CP, Connelley S: Effect of intensive care unit nosocomial pneumonia on duration of stay and mortality. Am J Infect Control 1984, 12: 233-238. 10.1016/0196-6553(84)90114-7
Mayer J: Laboratory diagnosis of nosocomial pneumonia. Semin Respir Infect 2000, 15: 119-131.
Montarvers P, Veber B, Auboyer C, Dupont H, Gauzit R, Korinek A, Malledant Y, Martin C, Moine P, Pourriat JL: Diagnostic and therapeutic management of nosocomial pneumonia in surgical patients: Results of the Eole study. Crit Care Med 2002, 30: 368-375. 10.1097/00003246-200202000-00017
Ephgrave KS, Kleiman-Wexler R, Pfaller M, Booth B, Werkmeister L, Young S: Postoperative pneumonia: A prospective study of risk factors and morbidity. Surgery 1993, 114: 815-821.
Friedland JS, Porter JC, Daryanani S, Bland JM, Screaton NJ, Vesely MJ, Griffin GE, Bennett ED, Remick DG: Plasma proinflammatory cytokine concentrations, Acute Physiology and Chronic Health Evaluation (APACHE) III scores and survival in patients in an intensive care unit. Crit Care Med 1996, 24: 1775-1781. 10.1097/00003246-199611000-00003
Martin LF, Asher EF, Casey JM, Fry DE: Postoperative pneumonia. Determinants of mortality. Arch Surg 1984, 119: 379-383.
Roumen RM, Hendirks T, ven der Ven-Jongekrijg , Nieuwenhuijzen GA, Sauerwein RW, ven der Meer JW, Goris RJ: Cytokine patterns in patients after major surgery, hemorrhagic shock, and severe blunt trauma. Relation with subsequent adult repiratory distress syndrome and multiple organ failure. Ann Surg 1993, 218: 769-776.
Angele MK, Faist E: Clinical review: immunodepression in the surgical patient and increased susceptibility to infection. Crit Care 2002, 6: 298-305. 10.1186/cc1514
Strieter RM, Kunkel SL: Acute lung injury: the role of cytokines in the elicitation of neutrophils. J Investig Med 1994, 42: 640-651.
Baggiolini M, Dewald B, Moser B: Interleukine-8 and related chemotactic cytokines CXC and CC chemokines. Adv Immunol 1994, 55: 97-179.
Pilewski JM, Albelda SM: Adhesion molecules in the lung: an overview. Am Rev Respir Dis 1993, 148: S31-S37.
Tutor JD, Mason CM, Dobard E, Beckerman RC, Summer WR, Nelson S: Loss of compartmentalization of alveolar tumor-necrosis factor after lung injury. Am J Respir Crit Care Med 1994, 149: 1107-1111.
Kurahashi K, Kajikawa O, Sawa T, Ohara M, Gropper M, Frank D, Martin TR, Wiener-Kronisch JP: Pathogenesis of septic shock in Pseudomaonas aeruginosa pneumonia. J Clin Invest 1999, 104: 743-750.
Danner RL, Elin RJ, Hosseini JM, Wesley RA, Reilly JM, Parillo JE: Endotoxinemia in human septic shock. Chest 1991, 99: 169-175.
Martin TR, Rubenfeld GD, Ruzinski JT, Goodman RB, Steinberg KP, Leturcq DJ, Moriarty AM, Raghu G, Baughman RP, Hudson LD: Relationship between soluble CD14, lipopolysaccaride binding protein, and the alveolar inflammatory response in patients with acute respiratory distress syndrome. Am J Resp Crit Care Med 1997, 155: 937-944.
Martin TR: Cytokines and lung injury: searching for useful biomarkers. Crit Care Med 2005, 33: 230-232. 10.1097/01.CCM.0000150825.01762.90
Parsons PE, Eisner MD, Thompson BT, Matthay AU, Ancukiewicz M, Bernard GR, Wheeler AP, The NHLBI Acute Respiratory Distress Syndrome Clinical Trials Network: Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med 2005, 33: 1-6. 10.1097/01.CCM.0000149854.61192.DC
Bonten MJ, Froon A, Gaillard C, Greve JW, de Leeuw PW, Drent M, Stobberingh EE, Buurman WA: The systemic inflammatory response in the development of ventilator-associated pneumonia. Am J Respir Crit Care Med 1997, 156: 1105-1113.
Froon AH, Bonten MJ, Gaillard CA, Greve JW, Dentener MA, de Leeuw PW, Drent M, Stobberingh EE, Buurman WA: Prediction of clinical severity and outcome of ventilator-associated pneumonia. Comparison of simplified acute physiology score with systemic inflammatory mediators. Am J Respir Crit Care Med 1998, 158: 1026-1031.
Casey LC, Balk A, RC Bone: Plasma cytokine and endotoxin levels correlate with survival in patients with sepsis syndrome. Ann Intern Med 1993, 119: 771-778.
American Thoracic Society: Hospital-acquired pneumonia in adults: diagnosis, assessment of severity, initial antimicrobial therapy and preventive strategies. A consensus statement, American Thoracic Society 1995. Am J Respir Crit Care Med 1996, 153: 1711-1725.
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM.: CDC definitions for nosocomial infections, 1988. Am J Infect Control 1988, 16: 128-140. 10.1016/0196-6553(88)90053-3
American College of Chest Physicians and Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis Crit Care Med 1992, 20: 864-874.
Knaus WA, Wagner DP, Draper EA, Zimmermann JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A, et al.: The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalised adults. Chest 1991, 100: 1619-1636.
Lefering R, Goris RJ, Van Nieuwenhoven EJ, Neugebauer E: Revision of the multiple organ failure score. Langenbecks Arch Surg 2002, 387: 14-20. 10.1007/s00423-001-0269-3
Beale R, Hollenberg SM, Vincent JL, Parrillo JE: Vasopressor and inotropic support in septic shock: an evidence-based review. Crit Care Med 2004,32(11 Suppl):S455-S465. 10.1097/01.CCM.0000142909.86238.B1
Beck JR, Schultz EK: The use of the relative operating characteristic (ROC) curves in test performance evaluation. Arch Pathol Lab Med 1986, 110: 13-20.
Krohn CD, Reikeras O, Aasen AO: The cytokines IL-1β and IL-1 receptor antagonist, IL-2 and IL-2 soluble receptor-alpha, IL-6 and IL-6 soluble receptor, TNF-alpha and TNF soluble receptor I, and IL-10 in drained and systemic blood after orthopedic surgery. Eur J Surg 1999, 165: 101-109. 10.1080/110241599750007261
Kato M, Honda I, Suzuki H, Murakami M, Matsukawa S, Hashimoto Y: Interleukin-10 production during and after upper abdominal surgery. J Clin Anesth 1998, 10: 184-188. 10.1016/S0952-8180(97)00264-X
Katja B, Hartmut K, Pawel M, Stefan B, Kox WJ, Spies CD: The value of immune modulating parameters in predicting the progression from peritonitis to septic shock. Shock 2001, 15: 95-100.
Sander M, Irwin M, Sinha P, Naumann E, Kox WJ, Spies CD: Suppression of interleukin-6 to interleukin-10 ratio in chronic alcoholics: association with postoperative infections. Intensive Care Med 2002, 28: 285-292. 10.1007/s00134-001-1199-9
Spies CD, Kern H, Schroder T, Sander M, Sepold H, Lang P, Stangl K, Beherens S, Sinha P, Schaffartzik W, et al.: Myocardial ischemia and cytokine response are associated with subsequent onset of infections after noncardiac surgery. Anesth Analg 2002, 95: 9-18. 10.1097/00000539-200207000-00002
Jong G, Hsiue TR, Chen CR, Chang HY, Chen CW: Rapidly fatal outcome of bacteremic Klebsiella pnemoniae pneumonia in alcoholics. Chest 1995, 107: 214-217.
Moore T, Moore BB, Newstead MW, Standiford TJ: Gamma delta-T cells are critical for survival and early proinflammatory cytokine gene expression during murine Klebsiella pneumonia. J Immunol 2000, 165: 2643-2650.
Raetz CR: Biochemistry of endotoxins. Annu Rev Biochem 1990, 59: 129-170. 10.1146/annurev.bi.59.070190.001021
Meduri GU, Headley S, Kohler G, Stentz F, Tolley E, Umberger R, Leeper K: Persistent elevation of inflammatory cytokines predicts a poor outcome in ARDS. Plasma IL-1beta and IL-6 levels are consistent and efficient predictors of outcome over time. Chest 1995, 107: 1062-1073.
Almirall J, Mesalles E, Klamburg J, Parra O, Agudo A: Prognostic factors of pneumonia requiring admission to the intensive care unit. Chest 1995, 107: 511-516.
Schein M, Wittman DH, Holzheimer R, Condon RE: Hypothesis: compartmentalization of cytokines in intraabdominal infection. Surgery 1996, 119: 694-700.
Brun-Buisson C: Guidelines for treatment of hospital-acquired pneumonia. Semin Respir Crit Care Med 2002, 23: 457-470. 10.1055/s-2002-35717
Muehlstedt SG, Richardson CJ, West MA, Lyte M, Rodriguez JL: Cytokines and the pathogenesis of nosocomial pneumonia. Surgery 2001, 130: 602-609. 10.1067/msy.2001.117105
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
VvD participated in the study design, interpretation of the results, and was involved in writing and revising the manuscript critically for important intellectual content. KR was involved in acquisition of data. UR was involved in the statistical analysis of data and helped to draft the manuscript. OVH participated in the study design and helped in drafting the manuscript. All above mentioned authors read and approved the final manuscript. CS conceived the study, participated in the study design, interpretation of the results, and in writing of the article, revised the manuscript critically for important intellectual content, and gave final approval of the version to be published.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
von Dossow, V., Rotard, K., Redlich, U. et al. Circulating immune parameters predicting the progression from hospital-acquired pneumonia to septic shock in surgical patients. Crit Care 9, R662 (2005). https://doi.org/10.1186/cc3826
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc3826