Abstract
As interest in the use of activated recombinant factor VII (rFVIIa) in trauma grows, questions arise regarding how best to monitor rFVIIa therapy and when rFVIIa may be expected to improve hemostasis. Knowledge of the mechanisms of action may be combined with available data on laboratory monitoring and efficacy in various coagulopathic states in coming to clinically relevant conclusions. This review addresses the physiology of hemostasis, placing emphasis on how rFVIIa influences the process by both tissue factor dependent and tissue factor independent mechanisms. This is extended to a mechanistic consideration of how rFVIIa may function under acidotic, hypothermic, and hemodilutional and/or consumptive conditions of trauma related coagulopathy. When these considerations are viewed alongside the available clinical data, it becomes apparent that rFVIIa has potential to improve hemostasis during trauma coagulopathy, within limitations. Common laboratory procedures are discussed with reference to mechanisms of action of rFVIIa and the available clinical data. Although there is no single assay that can predict rFVIIa efficacy in trauma, the prothrombin time (PT) is recommended as a minimum. Although a shortened PT does not predict success, correction of PT into the normal range may be a better indicator. A nonresponding PT appears to indicate that rFVIIa alone will not lead to hemostasis, and that additional blood products and other measures must be applied. Once the patient is more stable, PT and thromboelastography are recommended.
Similar content being viewed by others
Introduction
In 1983, Hedner and Kisiel [1] reported the successful use of plasma derived activated factor VII (FVIIa) for the control of bleeding in two patients with factor VIII (FVIII) antibodies. This was followed by successful treatment in other patients [2]. However, the procedures required for purification of FVIIa from plasma precluded extensive use. The shortage was addressed when NovoNordisk Pharmaceuticals developed a method to produce recombinant human FVIIa (rFVIIa) using a transfected baby hamster kidney cell line [3]. The drug NovoSeven® (Novo Nordisk A/S, Bagsværd, Denmark) is now registered in many countries worldwide for the treatment of spontaneous and surgical bleeding in patients with inhibitors against FVIII or factor IX (FIX) [3]. Over 700,000 standard doses (90 μg/kg) have been administered for acquired and congenital hemophilia [4]. Recently, there has been growing interest in the use of rFVIIa to control hemorrhage in patients without hemophilia. There are numerous reports of rFVIIa use in patients under a variety of circumstances, including trauma [5], as reviewed by Grounds and Bolan in this supplement. As interest in the use of rFVIIa in trauma grows, questions arise pertaining to how best to monitor rFVIIa therapy and when rFVIIa may be expected to work. Regarding the use of rFVIIa in trauma, knowledge of the mechanism of action may be combined with available data on laboratory monitoring and efficacy in various coagulopathic states in coming to clinically relevant conclusions.
Cell based model of hemostasis
Over 40 years ago the cascade model of blood clotting was introduced [6], a model that was later expanded to include both the intrinsic and extrinsic (tissue factor [TF]) pathways. Over the years, observations such as the fact that factor XII deficiency does not result in a hemorrhagic disease and the identification of important links between the two pathways [7, 8] pointed to the importance of the TF pathway. By the 1990s it became clear that the TF pathway (extrinsic) of coagulation was of primary importance in normal hemostasis, and it became questionable whether the intrinsic pathway was relevant to in vivo hemostasis [9]. Lawson and coworkers [10] reported a model of TF initiated coagulation that described an initiation or lag phase, during which initiating enzymatic events result in the assembly of highly efficient enzyme complexes on phospholipid surfaces, followed by a propagation phase, during which an exponential burst of thrombin generation occurs. More recently, a cell based model has been proposed that differs from previous models primarily by emphasizing the cellular control of coagulation in vivo (Fig. 1) [11]. An understanding of this model is important in understanding the mechanism of action of rFVIIa. The cell based model includes three overlapping phases that describe events that take place on different cell surfaces: initiation, amplification, and propagation.
A cell-based model of coagulation. The three phases of coagulation occur on different cell surfaces: initiation on the tissue factor bearing cell; amplification on the platelet as it becomes activated; and propagation on the activated platelet surface. vWF, von Willebrand factor. Reproduced with permission from Hoffman and Monroe [11].
Initiation
TF is the primary physiologic initiator of coagulation [9] and is present in subendothelium and other tissues that are not normally exposed to blood [12, 13]. TF is also expressed on monocytes following trauma [14] and on endothelium in response to activation by inflammatory mediators [15]. It may also be present in plasma [16] and circulating microparticles under some circumstances [17].
The process begins when vascular damage exposes blood to subendothelium, which is rich in TF and collagen. Both FVIIa (which circulates as 1% of total FVII) and FVII bind to TF on subendothelial cells. The FVIIa/TF complex activates both factor X (FX) and FIX [10]. TF bound FVII is activated by this small amount of FXa, producing more TF/FVIIa in a feed forward manner. FXa also activates plasma factor V (FV) [18], allowing the formation of the prothrombinase complex (FXa/FVa/calcium) on the TF bearing cell surface and leading to the production a small amount of thrombin [10, 19].
Amplification
At the site of vascular injury, platelets adhere to the subendothelium and become partially activated. The small amount of thrombin produced during initiation fully activates platelets [20]. This enhances adhesion [21], causes release of FV from platelet α-granules, and induces a procoagulant configuration of cell membrane phospholipids and receptors [19]. On the activated platelet surface, thrombin produced during the initiation phase activates FV, FVIII, and factor XI (FXI) [20], which subsequently activates FIX to FIXa. The result is that the coagulation process has moved to the activated platelet surface, where the required components of the tenase complex (FIXa/FVIIIa/calcium) are assembled and ready to produce FXa, which will allow formation of the prothrombinase complex on the same surface in preparation for large scale production of thrombin [19].
Propagation
Small amounts of FIXa produced by the TF/FVIIa on the TF bearing cell diffuse to the surface of the activated platelet. This FIXa, along with FIXa produced by FXIa on the platelet, binds to the platelet surface and combines with FVIIIa, forming the tenase complex. The tenase complex converts FX to FXa, which then forms the prothrombinase complex in combination with FVa. The formation of these complexes makes possible the highly efficient generation of large amounts of thrombin from prothrombin [19]. The 'burst' of thrombin results in recruitment of more platelets as well as the production of fibrin polymers, activation of factor XIII, and other related events.
Localization of the procoagulant process
The coagulation process is localized to the site of vascular injury by several mechanisms [19]. The first is localized exposure of subendothelial elements. FVII and FVIIa have negligible enzymatic activity in the absence of TF. The binding of FVIIa to TF provides the enhanced FVIIa activity specifically where required. Binding and activation of platelets at the wound site, in close proximity to cells bearing the TF/FVIIa complex, provides the required procoagulant surface. Other mechanisms involve three key inhibitors of procoagulant enzymes and cofactors, antithrombin III, protein C, and tissue factor pathway inhibitor. FXa and thrombin that diffuse away from the protected surface of the cell are rapidly inactivated by antithrombin III [22]. Thrombin binds to thrombomodulin on adjacent undamaged endothelial surfaces. The thrombin/thrombomodulin complex activates protein C, which binds to a specific endothelial receptor and, with its cofactor protein S, inactivates FVa and FVIIIa, further controlling the spread of the coagulation process [23]. TF pathway inhibitor directly inhibits TF/FVIIa [24]. Other interactions among these enzymes and inhibitors are also involved. Additionally, endothelial cells possess a cell surface ADPase, which inhibits recruitment of platelets to bind to intact endothelium [25].
Mechanisms of action of activated recombinant factor VII
The normal ratio of FVII to FVIIa in the circulation is 100:1 (10 nmol/l and 0.10 nmol/l, respectively). Following rFVIIa administration the circulating total FVIIa (rFVIIa and native FVIIa) concentration is increased approximately 100-fold (to 3–20 nmol/l) such that the FVII:FVIIa ratio is approximately 1:1. It is generally agreed that rFVIIa acts by enhancing thrombin generation at the site of injury, but there is controversy over the exact mechanism(s) of action by which this is accomplished. Current knowledge of the action of rFVIIa comes primarily from work using systems of simulated or actual hemophilia conducted to study the ability of rFVIIa to enhance thrombin production by 'bypassing' FVIIIa or FIXa and the need for the tenase complex. It appears that there are two principal mechanisms by which rFVIIa acts [26]: a TF dependent and a TF independent mechanism.
In both mechanisms, rFVIIa augmented coagulation is initiated at the site of vascular injury by the interaction of rFVIIa with TF. This results in initial FX activation followed by thrombin generation. Along with the exposed subendothelium, this initial thrombin acts to recruit and activate platelets at the site of injury. At this point the mechanisms diverge.
Under the TF independent mechanism, rFVIIa binds with low affinity to the surface of activated platelets. This platelet bound rFVIIa then activates FX to FXa. Although the enzymatic efficiency of this reaction is low relative to that of the TF/rFVIIa complex, the pharmacologic concentration of rFVIIa offsets this inefficiency. Therefore, FXa production becomes independent of TF with the accumulation of platelets at the site of injury [19, 27]. Under the TF dependent mechanism, pharmacologic concentrations of rFVIIa result in an increased proportion of TF occupancy by (total) FVIIa (either FVIIa or rFVIIa), resulting in a higher concentration of TF/(r)FVIIa complex at the site of vascular damage [28]. The rFVIIa must bind to TF to enhance FXa production and ultimately thrombin generation [29, 30]. Under either mechanism, the remaining steps involve combination of FXa with FVa on the surface of activated platelets to form the prothrombinase complex, which converts prothrombin to thrombin. The mechanisms are not mutually exclusive, and it is possible that both play a role [26]. Data suggest that the response in nonhemophilic blood may be slightly different, involving the additional activity of rFVIIa activating FIX [31].
The localized generation of large amounts of thrombin as a result of rFVIIa may have the additional beneficial effects of enhancing platelet adhesion and aggregation [32] and making formed clots more resistant to fibrinolysis by increasing activation of thrombin activatable fibrinolysis inhibitor [33] and/or producing thinner and more tightly packed fibrin fibers [34].
Activated recombinant factor VII in trauma coagulopathy
With the rapidly expanding interest in the use rFVIIa in patients without hemophilia has come debate over whether rFVIIa may be considered a universal hemostatic agent [35, 36]. Both pro and con arguments in this debate acknowledge that hemorrhagic situations are not all the same. Even within the trauma setting a variety of situations exist, and the risks as well as potential efficacy may vary with the situation. With respect to the multifactorial coagulopathy associated with trauma, acidosis, hypothermia, hemodilution, and/or consumption of factors and platelets are important factors to consider [37].
Activated recombinant factor VII and acidosis
The coagulopathy associated with acidosis appears to involve changes in both enzymatic rates [38] and platelet function [39, 40]. In vitro, a reduction in pH from 7.4 to 7.0 reduces TF independent activity of rFVIIa by over 90% and TF dependent activity by over 60% [38]. Therefore, it is clear that reduced pH will result in some reduction in efficacy of rFVIIa. However, considering the fact that rFVIIa administration increases total circulating FVIIa levels by 100-fold, it is not clear at what level of acidosis the beneficial effect of rFVIIa would be nullified. The decrement in the TF independent mechanism is greater than the effect on the TF dependent mechanism. To the extent that one mechanism may be more important than the other in a given situation, the effects of pH may be variable. In addition to decrements in enzymatic efficiency, impaired platelet function during acidosis would also be expected to affect rFVIIa efficacy.
In one report [41] the clinical response to rFVIIa in trauma patients tended to decline at pH below 7.2 but the effect was only significant at or below 7.0. Dutton and coworkers [42] found that mean blood pH was 7.29 in the group of trauma patients who responded to rFVIIa whereas the pH in the nonresponders was 7.02 (P < 0.05). However, six out of 20 nonresponders had a pH greater than 7.10, while five patients with pH at or below 7.10 responded to rFVIIa therapy. In a case report of a trauma patient who had an arterial pH of 7.09 at the time of rFVIIa administration [43], the drug was deemed efficacious. In an early report of coagulopathic trauma patients [44], rFVIIa was also effective during acidosis.
Based on currently available information, pH cannot be used as an absolute guide as to whether rFVIIa therapy will be effective, but it can be expected that efficacy will be reduced as pH declines. It is clear that blood pH should be taken into account when considering use of rFVIIa for management of trauma coagulopathy, and the recommendation to correct pH to at least 7.2 before rFVIIa administration is a reasonable guideline [41].
Activated recombinant factor VII and hypothermia
It is well known that hypothermia decreases the activity of coagulation enzymes and impairs platelet function such that blood clotting is slowed. TF dependent activity of rFVIIa declines by 20% with a drop in temperature from 37°C to 33°C [38]. Interestingly, TF independent activity increases under the same experimental conditions [38]. With the assumption that both the TF dependent and TF independent activities of rFVIIa play a role, it seems possible that the TF independent mechanism may make rFVIIa somewhat resistant to decreases in temperature in terms of hemostatic effect. On the other hand, rFVIIa cannot be expected to be effective for all degrees of hypothermia. For the initiation of blood clotting (initiation phase) at the site of injury, formation of the TF/FVIIa complex and generation of a small amount of FXa by the TF dependent mechanism is required. Initiation by this mechanism would diminish with decreasing temperature. The other theoretical option is for platelets to adhere to the subendothelium and become sufficiently activated for rFVIIa to bind and activate FX by a TF independent mechanism. The limiting factor in this case could become the lack of platelet activation under hypothermic conditions [45]. Therefore, it appears that there will be a level of hypothermia at which rFVIIa is no longer effective.
rFVIIa appears to be effective at temperatures normally encountered in trauma, although this has not been fully studied. Martinowitz and Michaelson [41] reported efficacy in trauma patients with an average core temperature of 34.1°C. Similar findings were reported by others [46, 47]. In one study a hemostatic effect at a body temperature as low as 30°C was reported [44]. Two studies in swine [48, 49] also suggested efficacy in hypothermia, although a third swine study [50] failed to confirm those findings.
Based on currently available information, rFVIIa can be expected to be useful for the control of nonsurgical bleeding under hypothermic conditions encountered in trauma (e.g. 33°C), but loss of TF dependent activity and decreased platelet function will likely lead to reduced rFVIIa efficacy as temperature approaches 30°C.
Activated recombinant factor VII and hemodilution/ consumption
Examination of the model of blood coagulation and an inventory of the normal concentrations of coagulation factors makes it clear that the process is exquisitely balanced [22]. Changes in the concentrations of various components of the system can alter greatly thrombin generation and the clotting process as a whole [51]. Therefore, it is expected that sufficient dilution or consumption of various components of the coagulation system will result in coagulopathy. The potential for efficacy of rFVIIa will be eliminated when components other than FVIIa become rate limiting. For example, in the absence of FX or FV, rFVIIa does not shorten in vitro plasma clotting times [52]. There could also be a point when fibrinogen [37], prothrombin, or platelets become rate limiting. This notion is supported by data from 13 patients who were treated with rFVIIa for life threatening coagulopathy [53]. All patients received blood products before rFVIIa administration. However, patients who responded to treatment had a better coagulation status (as measured by fibrinogen and platelet concentrations, PT, and activated partial thromboplastin time [aPTT]) at the time of treatment than did nonresponders.
Nonetheless, rFVIIa does appear to improve hemostasis in the presence of hemodilution/consumption, within limits. The trauma cases reported to date have included patients who received crystalloid and colloidal fluids as well as blood products in various combinations. It is expected that all of these patients would have some degree of consumption and/or hemodilution. There have been a number of reports of successful use of rFVIIa for patients in consumptive states (disseminated intravascular coagulation or similar states) resulting from trauma or other causes [54–60]. In several cases in which hemodilution was clearly identified, rFVIIa was effective in controlling bleeding [43, 46, 60–62]. Two studies in swine [48, 49] also suggest efficacy in hemodilution, although a third study [50] failed to confirm those findings.
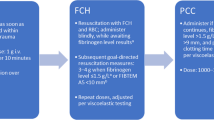
Further studies are needed to elucidate more fully the combinations of coagulopathic conditions under which rFVIIa will and will not be effective with regard to trauma. At the present time, to optimize the opportunity for rFVIIa to enhance hemostasis, it is recommended that factors and platelets be replaced to the extent possible before rFVIIa is used [37, 41, 57, 63]. As a guideline, platelets should be maintained at a minimum of 50,000/ μl and fibrinogen at a minimum of 50 mg/dl. Although the lower limits of pH and temperature under which rFVIIa may be effective are not clearly defined, efforts should be made to warm the patient and correct acidosis before administering rFVIIa treatment [41].
Laboratory monitoring of activated recombinant factor VII
There is currently no single laboratory test that is satisfactory for monitoring the clinical efficacy of rFVIIa [41, 64, 65]. By far the most commonly used tests have been the PT and the aPTT, but it has been suggested that the shortening of these two tests does not necessarily reflect clinical effectiveness [65]. A variety of other laboratory tests have been used to monitor or study the effects of rFVIIa under various conditions. When one is assessing the utility of a laboratory test in monitoring rFVIIa therapy, it is important to consider factors such as availability, turnaround time, and relevance of assay end-points to clinical outcomes, among others [66]. The following is a brief discussion of the potential applicability of selected laboratory tests in the trauma setting.
Plasma coagulation assays
Prothrombin time
The PT assay measures time to clot formation by the TF pathway. The assay is performed on a citrated plasma sample and takes only a few minutes to perform, although logistical considerations drive local turnaround times. The clotting reaction is initiated by adding TF and phospholipids (usually in the form of thromboplastin), and calcium. By the most common method, clot formation is detected by the change in turbidity as the fibrin mesh forms. Because PT specifically examines the TF pathway, it is sensitive to rFVIIa. Many studies have demonstrated that rFVIIa shortens PT when coagulation is normal and in coagulopathy due to trauma and many other nonhemophilic conditions. The maximal degree of PT shortening is limited not only by in vivo parameters but also by the concentration of TF and phospholipids present in the assay reagents, and by the settings of the instrument.
PT is sensitive to both temperature and pH. Standard PT assays are run at 37°C and the pH dictated by the reagents used. Therefore, the correction in PT may not reflect the actual status of the patient under coagulopathic conditions. Some automated instruments now perform PT at the patient's temperature, which assists in interpretation (perhaps future advances in instrumentation will account for patient pH).
Simple improvement (shortening) of the PT cannot be used as a reliable indicator of rFVIIa hemostatic efficacy in trauma. Both Dutton and coworkers [42] and Eikelboom and colleagues [67] noted that all patients treated with rFVIIa had improved PT, even those who did not respond in terms of hemostasis. There is some indication that the degree of shortening of PT may correlate with hemostatic efficacy. Although the PT shortened in all patients following rFVIIa, Dutton and coworkers [42] found that the post-rFVIIa PT was shorter in patients who responded hemostatically than in those who did not. Martinowitz and Michaelson [41] reported similar findings (Fig. 2). Although currently available data are limited, it appears that correction of the PT into or below the normal range may be a better indicator of expected rFVIIa hemostatic efficacy than a simple numeric reduction in PT.
Shortening of prothrombin time (PT) values before and after administration of activated recombinant factor VII (rFVIIa) was significant in both 'responders' (circles: P = 0.0001) and 'nonresponders' (triangles; P = 0.016). However, in the latter group the mean PT values before and after treatment were significantly higher. Reproduced with permission from Martinowitz and Michaelson [41].
Although there have been many reports of rFVIIa shortening PT, we know of only one report in which hemostasis was attained without a shortening in PT following rFVIIa administration [68]. Therefore, the PT may be useful in identifying patients in whom rFVIIa will not be expected to work. If PT is not shortened after rFVIIa administration, then replacement of one or more factors in addition to FVIIa may be indicated.
The PT assay is useful in monitoring rFVIIa treated patients after a damage control or definitive surgical procedure, or after re-dosing based on the clinical scenario. The time course of PT correction follows that of increased plasma FVII activity after rFVIIa treatment and is dose dependent [48, 49, 69–79]. As an alternative to the FVII assay (e.g. if this is not available), PT may be used to monitor duration of expected rFVIIa correction of coagulopathy.
In summary, a simple reduction in PT is not useful in identifying responders to rFVIIa but the lack of a reduction may identify nonresponders. A reduction in PT into the normal range may prove to be a better indicator of potential hemostatic effect. The PT can be useful in monitoring the duration of expected rFVIIa efficacy. Considering these factors, as well as the universality of the PT test, it is recommended that PT be used as a standard laboratory test in trauma patients receiving rFVIIa.
Activated partial thromboplastin time
This assay measures the time to clot formation by the intrinsic pathway and is performed using methods similar to the PT. The difference is that the clotting reaction is initiated by a source of celite or kaolin, a source of phospholipids (historically referred to as partial thromboplastin), and calcium. No TF is added. Often, rFVIIa treatment shortens aPTT. This phenomenon is due to TF independent activity of rFVIIa such that rFVIIa generates FXa independently of TF under the conditions of the assay [52, 80]. The aPTT is useful for monitoring rFVIIa efficacy in clinical hemophilia [81], but this is not necessarily so in other patients. In some cases aPTT has been shortened following rFVIIa administration in trauma patients, whereas in others it has not. Therefore, we do not consider the aPTT to be a useful assay for making clinical decisions regarding rFVIIa use in trauma.
Other standard plasma coagulation assays
It is not normally expected that rFVIIa treatment will affect thrombin time, fibrinogen concentration, or levels of coagulation factors, with the exception of FVII. However, it has been observed that administration of rFVIIa may interfere with results of some factor assays, producing artificially elevated levels [82]. With the exception of the FVII assay described below, the standard laboratory coagulation tests that are based on plasma clot formation (thrombin time, fibrinogen, clotting factors) are not useful in monitoring specifically the effectiveness of rFVIIa in trauma. Although rFVIIa treatment may interfere with the results of some of these assays, this phenomenon should not preclude monitoring of these parameters as necessary to assess overall patient status, for example to determine the need for blood products.
The most relevant of the standard factor assays for monitoring rFVIIa therapy is the FVII assay (factor VII clotting activity [FVII:C]). This assay does not measure specifically FVIIa or rFVIIa, but instead it measures total plasma FVII activity [83]. In a dose dependent manner, rFVIIa increases FVII activity in a sample far above normal levels [44, 48, 49, 69, 71–73, 75–79, 82, 84–86]. Therefore, the sample must be diluted by the laboratory in order to calculate an accurate value. The laboratory should be notified that this is expected. Although levels are related to the duration of PT correction, no study has demonstrated that FVII:C levels are predictive of hemostatic response to rFVIIa in trauma. The value of this assay in the management of rFVIIa in trauma is limited, but it can be used to confirm that the dose entered a patient's blood stream or to monitor the time course of FVII:C elevation.
Thrombin generation test
Thrombin generation tests have been used in research but clinical use has been very limited. In one version, the assay measures the amount of thrombin generated over time in platelet poor or platelet rich plasma by monitoring the change in flourescence as a fluorogenic substrate molecule is cleaved by thrombin. rFVIIa increases thrombin generation as detected using this method [87]. Issues related to availability and complexity currently limit the use of this assay. However, as automated versions become available, it may become a useful assay for monitoring rFVIIa therapy in trauma.
Whole blood clotting assays
Thromboelastography
Thromboelastography (TEG) is performed most commonly in North America using the Thromboelastograph (Haemoscope, Skokie, IL, USA). In other regions, a slight variation of this assay is performed using the roTEG Coagulation Analyzer (PentaPharm, Marburg, Germany). The same general principals hold for both instruments, although different nomenclature is used for the various clotting parameters. The nomenclature for the thromboelastograph is used for the purpose of this discussion.
TEG monitors changes in the viscoelastic properties of a forming clot. Either unaltered or citrated blood is delivered into a sample cup and clotting initiated spontaneously or using various agonists. A pin is suspended in the blood by a torsion wire and monitored for motion as the pin is repeatedly rotated through the blood in a 10 s cycle. Increased blood viscosity increases resistance to pin rotation and deflects the pin. The deflection is translated into output measured in millimeters of amplitude, which increases as blood viscosity increases. Various standard parameters are calculated, including reaction time (R), coagulation time (K), α angle, maximum amplitude (MA), time to reach MA (tMA), and per cent lysis at 30 or 60 min after MA. R reflects the time to initial clot formation. K reflects the time from R until a standardized level of clot firmness is reached (amplitude 20 mm). The α angle is a measure of the kinetics of clot development. MA reflects the maximum firmness of the clot. Per cent lysis measurements assess the rate of fibrinolysis. Recently, two additional TEG parameters – maximum velocity of clot formation (MaxVel) and time to reach MaxVel (tMaxVel) -were reported for both versions of the TEG instrument [77, 88]. These parameters appear more sensitive to rFVIIa than the standard kinetic parameters [88]. It is important to use dilute TF as the agonist to initiate clotting for best sensitivity [89, 90]. TEG has more traditionally been performed using agonists that initiate clotting via the intrinsic pathway, but these agonists yield variable results with rFVIIa and are not optimal for monitoring this drug.
The most consistent effect of rFVIIa on TF initiated TEG is a shortening of the R [42, 50, 77, 91–93], but this is not always observed [49]. Increased MaxVel, α-angle and MA, and decreased K have also been observed [42, 77, 90–92]. Hendriks et al. [92] reported no change in rate of fibrinolysis after rFVIIa treatment. The principal advantage of the TEG is that it can assess the rate of whole blood clot initiation, rate of clot development, maximum clot strength, and fibrinolysis in a single assay. Because it is a whole blood assay it accounts for the number and function of platelets, as well as other cellular and plasma phase components. TEG is not a standard instrument in many hospitals, and the assay normally takes about 1 hour to perform, even when the instrument is located in the operating room. However, it can be performed much more rapidly if one is interested only in R. These drawbacks notwithstanding, TEG using dilute TF to initiate clotting can be a useful and sensitive method to monitor rFVIIa therapy.
Other whole blood clotting assays
The activated clotting time (ACT) assay measures the time required for clot formation using whole blood, usually with clotting initiated via the intrinsic pathway. Although the ACT is commonly available, reports of use of the ACT after rFVIIa treatment are limited. One study reported a faster clot time in blood from pigs treated with rFVIIa [77]. Recently available modified ACT assays that use a TF reagent to initiate clotting may prove useful in monitoring rFVIIa treated patients. The platelet function analyzer (PFA) assesses primarily the ability of platelets to form a hemostatic plug and has been related to bleeding time [94]. In one study [95] PFA values before and after rFVIIa treatment was not related to efficacy in patients with platelet defects. Current data do not support the use of PFA as a standard parameter in monitoring rFVIIa therapy in trauma. The Hemodyne hemostasis analyzer (Hemodyne Inc., Richmond, VA, USA) monitors platelet contractile force over time and clot elasticity. Thrombin generation time can also be determined [96]. Although this assay offers some advantages over other whole blood assays and appears useful for rFVIIa monitoring, it is not widely available.
Recommendations for monitoring and interpretation of laboratory values
Recently, several articles have examined the issue of rFVIIa monitoring [66, 81, 89, 96]. Although numerous methods are available, the issue remains that there is no currently available single laboratory monitor that predicts rFVIIa efficacy [41, 64, 65]. There are factors related to trauma that make monitoring more problematic than for other patients. The most important of these is the issue of turnaround time. The rapidly changing status of the patient during the use of multiple blood products, colloids, and crystalloids during active resuscitation and ongoing hemorrhage is another factor, as is the uncertain half-life of a given dose of rFVIIa under these conditions. When a trauma patient has uncontrollable coagulopathic bleeding, it is usually not possible to wait for laboratory results before taking further action. Instead, empiric treatment with rFVIIa and direct observation must be used. Nonetheless, comparison of laboratory values after treatment with those before treatment can provide valuable information. Especially in cases in which continued bleeding may be obscured by packing, when intracranial hemorrhage is the target for hemostasis, or when rFVIIa treatment is administered under relatively more controlled circumstances, laboratory monitoring can be very useful.
The use of the PT is recommended. Although a simple shortening of PT does not predict hemostatic efficacy, correction of PT into the normal range may be a better indicator. It appears that a nonresponding PT indicates that rFVIIa alone will not lead to hemostasis, and that additional blood products and other measures must be applied. Once the patient is more stable, PT and TEG are recommended. FVII:C may also be useful in some situations. Other laboratory measurements, although useful for answering specific questions and monitoring overall patient status, are not necessary for basic rFVIIa monitoring in trauma.
Conclusion
Whether by a TF dependent or TF independent mechanism, or by a combination, it is agreed that the hemostatic efficacy of rFVIIa is due to its ability to increase thrombin generation in a localized manner at the site of vascular injury. Thrombin generation is dependent on the assembly and activity of key enzyme complexes on the membranes of activated platelets. Mechanistic considerations and available clinical reports are consistent with the concept that rFVIIa administration can improve hemostasis under conditions of acidosis, hypothermia, and hemodilution/consumption, within limits. Because of the effects of acidosis and hypothermia on enzymatic rates and platelet function, it is expected that extremes of acidosis and hypothermia will be reached at which rFVIIa can no longer be expected to function. Evidence for efficacy at least to a pH in the region of 7.2 and to a core temperature of 34°C is growing, although it is likely that the limits of efficacy are somewhat lower. When hemodilution/ consumption reaches a point at which a component other than FVIIa becomes rate limiting, rFVIIa efficacy will be impossible without replacement of other components, such as FV, FX, prothrombin, fibrinogen, and platelets. Current recommendations to give blood products and to attempt to correct acidosis and hypothermia before rFVIIa administration are consistent with the current understanding of rFVIIa mechanisms of action [37, 41, 63] but further research is needed to define more clearly the limitations of rFVIIa efficacy under the multifactorial coagulopathic conditions associated with trauma.
During active resuscitation and damage control procedures, laboratory monitoring may be too slow to permit its meaningful use in clinical decision making. There is currently no replacement for direct observation of hemostatic effect. Comparison of laboratory values after treatment with those before treatment can provide valuable information. Especially when continued bleeding may be obscured by packing, when intracranial hemorrhage is the target for hemostasis, or when rFVIIa treatment is administered under relatively more controlled circumstances, laboratory monitoring is essential. Although no laboratory test can predict the hemostatic efficacy of rFVIIa, the use of the PT is recommended. A shortened PT does not predict success, but correction of PT into the normal range may be a better indicator. A nonresponding PT appears to indicate that rFVIIa alone will not lead to hemostasis, and that additional blood products and other measures must be applied. Once the patient is more stable, PT and TEG are recommended. FVII:C may also be useful in some situations.
Abbreviations
- ACT:
-
ACT = activated clotting time
- aPTT:
-
aPTT = activated partial thromboplastin time
- FIX:
-
FIX = factor IX
- FV:
-
FV= factor V
- FVII:
-
C = factor VII clotting activity
- FVIII:
-
FVIII = factor VIII
- FX:
-
FX = factor X
- FXI:
-
FXI = factor XI
- PFA:
-
PFA = platelet function analyzer
- PT:
-
PT = prothrombin time
- rFVIIa:
-
rFVIIa = activated recombinant factor VII
- TEG:
-
TEG = thromboelastography
- TF:
-
TF = tissue factor.
References
Hedner U, Kisiel W: Use of human factor VIIa in the treatment of two hemophilia A patients with high-titer inhibitors. J Clin Invest 1983, 71: 1836-1841.
Hedner U, Bjoern S, Bernvil SS, Tengborn L, Stigendahl L: Clinical experience with human plasma-derived factor VIIa in patients with hemophilia A and high titer inhibitors. Haemostasis 1989, 19: 335-343.
Jurlander B, Thim L, Klausen NK, Persson E, Kjalke M, Rexen P, Jorgensen TB, Ostergaard PB, Erhardtsen E, Bjorn SE: Recombinant activated factor VII (rFVIIa): characterization, manufacturing, and clinical development. Semin Thromb Hemost 2001, 27: 373-384. 10.1055/s-2001-16890
Abshire T, Kenet G: Recombinant factor VIIa: review of efficacy, dosing regimens and safety in patients with congenital and acquired factor VIII or IX inhibitors. J Thromb Haemost 2004, 2: 899-909. 10.1111/j.1538-7836.2004.00759.x
Boffard KD, Riou B, Warren B, Choong PI, Rizoli S, Rossaint R, Axelsen M, Kluger Y, for the NovoSeven Trauma Study Group: Recombinant Factor VIIa as adjunctive therapy for bleeding control in severely injured trauma patients. J Trauma 2005, 59: 8-18.
Davie EW, Ratnoff OD: Waterfall sequence for intrinsic blood clotting. Science 1964, 145: 1310-1312.
Gailani D, Broze GJ Jr: Factor XI activation in a revised model of blood coagulation. Science 1991, 253: 909-912.
Osterud B, Rapaport SI: Activation of factor IX by the reaction product of tissue factor and factor VII: additional pathway for initiating blood coagulation. Proc Natl Acad Sci USA 1977, 74: 5260-5264.
Rapaport SI, Rao LV: The tissue factor pathway: how it has become a 'prima ballerina'. Thromb Haemost 1995, 74: 7-17.
Lawson JH, Kalafatis M, Stram S, Mann KG: A model for the tissue factor pathway to thrombin. I. An empirical study. J Biol Chem 1994, 269: 23357-23366.
Hoffman M, Monroe DM III: A cell-based model of hemostasis. Thromb Haemost 2001, 85: 958-965.
Drake TA, Morrissey JH, Edgington TS: Selective cellular expression of tissue factor in human tissues. Implications for disorders of hemostasis and thrombosis. Am J Pathol 1989, 134: 1087-1097.
Wilcox JN, Smith KM, Schwartz SM, Gordon D: Localization of tissue factor in the normal vessel wall and in the atherosclerotic plaque. Proc Natl Acad Sci USA 1989, 86: 2839-2843.
Utter GH, Owings JT, Jacoby RC, Gosselin RC, Paglieroni TG: Injury induces increased monocyte expression of tissue factor: factors associated with head injury attenuate the injury-related monocyte expression of tissue factor. J Trauma 2002, 52: 1071-1077.
Nawroth PP, Stern DM: Modulation of endothelial cell hemostatic properties by tumor necrosis factor. J Exp Med 1986, 163: 740-745. 10.1084/jem.163.3.740
Gando S: Disseminated intravascular coagulation in trauma patients. Semin Thromb Hemost 2001, 27: 585-592. 10.1055/s-2001-18864
Furie B, Furie BC: Role of platelet P-selectin and microparticle PSGL-1 in thrombus formation. Trends Mol Med 2004, 10: 171-178. 10.1016/j.molmed.2004.02.008
Monkovic DD, Tracy PB: Activation of human factor V by factor Xa and thrombin. Biochemistry 1990, 29: 1118-1128. 10.1021/bi00457a004
Hoffman M, Monroe DM III: The action of high-dose factor VIIa (FVIIa) in a cell-based model of hemostasis. Semin Hematol 2001, 38: 6-9. 10.1053/shem.2001.29504
Monroe DM, Hoffman M, Roberts HR: Transmission of a procoagulant signal from tissue factor-bearing cell to platelets. Blood Coagul Fibrinolysis 1996, 7: 459-464.
Diaz-Ricart M, Estebanell E, Lozano M, Aznar-Salatti J, White JG, Ordinas A, Escolar G: Thrombin facilitates primary platelet adhesion onto vascular surfaces in the absence of plasma adhesive proteins: studies under flow conditions. Haematologica 2000, 85: 280-288.
Mann KG: Biochemistry and physiology of blood coagulation. Thromb Haemost 1999, 82: 165-174.
Esmon CT: Protein C anticoagulant pathway and its role in controlling microvascular thrombosis and inflammation. Crit Care Med 2001, 29: S48-S51. 10.1097/00003246-200107001-00018
Broze GJ Jr: Tissue factor pathway inhibitor. Thromb Haemost 1995, 74: 90-93.
Marcus AJ, Broekman MJ, Drosopoulos JH, Islam N, Alyonycheva TN, Safier LB, Hajjar KA, Posnett DN, Schoenborn MA, Schooley KA, et al.: The endothelial cell ecto-ADPase responsible for inhibition of platelet function is CD39. J Clin Invest 1997, 99: 1351-1360.
Lisman T, De Groot PG: Mechanism of action of recombinant factor VIIa. J Thromb Haemost 2003, 1: 1138-1139. 10.1046/j.1538-7836.2003.00225.x
Monroe DM, Hoffman M, Oliver JA, Roberts HR: Platelet activity of high-dose factor VIIa is independent of tissue factor. Br J Haematol 1997, 99: 542-547. 10.1046/j.1365-2141.1997.4463256.x
van't Veer C, Mann KG: The regulation of the factor VII-dependent coagulation pathway: rationale for the effectiveness of recombinant factor VIIa in refractory bleeding disorders. Semin Thromb Hemost 2000, 26: 367-372. 10.1055/s-2000-8454
Butenas S, Brummel KE, Bouchard BA, Mann KG: How factor VIIa works in hemophilia. J Thromb Haemost 2003, 1: 1158-1160. 10.1046/j.1538-7836.2003.00181.x
Butenas S, Brummel KE, Paradis SG, Mann KG: Influence of factor VIIa and phospholipids on coagulation in 'acquired' hemophilia. Arterioscler Thromb Vasc Biol 2003, 23: 123-129. 10.1161/01.ATV.0000042081.57854.A2
Hoffman M, Monroe DM III, Roberts HR: Activated factor VII activates factors IX and X on the surface of activated platelets: thoughts on the mechanism of action of high-dose activated factor VII. Blood Coagul Fibrinolysis 1998,9(Suppl 1):S61-S65.
Lisman T, Adelmeijer J, Cauwenberghs S, Van Pampus EC, Heemskerk JW, De Groot PG: Recombinant factor VIIa enhances platelet adhesion and activation under flow conditions at normal and reduced platelet count. J Thromb Haemost 2005, 3: 742-751. 10.1111/j.1538-7836.2005.01227.x
Lisman T, Mosnier LO, Lambert T, Mauser-Bunschoten EP, Meijers JC, Nieuwenhuis HK, de Groot PG: Inhibition of fibrinolysis by recombinant factor VIIa in plasma from patients with severe hemophilia A. Blood 2002, 99: 175-179. 10.1182/blood.V99.1.175
He S, Blomback M, Jacobsson EG, Hedner U: The role of recombinant factor VIIa (FVIIa) in fibrin structure in the absence of FVIII/FIX. J Thromb Haemost 2003, 1: 1215-1219. 10.1046/j.1538-7836.2003.00242.x
Levi M: Recombinant factor VIIa: a general hemostatic agent? Not yet. J Thromb Haemost 2004, 2: 1695-1697. 10.1111/j.1538-7836.2004.00912.x
Roberts HR: Recombinant factor VIIa: a general hemostatic agent? Yes. J Thromb Haemost 2004, 2: 1691-1694. 10.1111/j.1538-7836.2004.00909.x
Armand R, Hess JR: Treating coagulopathy in trauma patients. Transfus Med Rev 2003, 17: 223-231. 10.1016/S0887-7963(03)00022-1
Meng ZH, Wolberg AS, Monroe DM III, Hoffman M: The effect of temperature and pH on the activity of factor VIIa: implications for the efficacy of high-dose factor VIIa in hypothermic and acidotic patients. J Trauma 2003, 55: 886-891.
Gende OA: Capacitative calcium influx and intracellular pH cross-talk in human platelets. Platelets 2003, 14: 9-14. 10.1080/0953710021000034465
Marumo M, Suehiro A, Kakishita E, Groschner K, Wakabayashi I: Extracellular pH affects platelet aggregation associated with modulation of store-operated Ca2+entry. Thromb Res 2001, 104: 353-360. 10.1016/S0049-3848(01)00374-7
Martinowitz U, Michaelson M: Guidelines for the use of recombinant activated factor VII (rFVIIa) in uncontrolled bleeding: a report by the Israeli Multidisciplinary rFVIIa Task Force. J Thromb Haemost 2005, 3: 640-648. 10.1111/j.1538-7836.2005.01203.x
Dutton RP, McCunn M, Hyder M, D'Angelo M, O'Connor J, Hess JR, Scalea TM: Factor VIIa for correction of traumatic coagulopathy. J Trauma 2004, 57: 709-718.
O'Neill PA, Bluth M, Gloster ES, Wali D, Priovolos S, DiMaio TM, Essex DW, Catanese CA, Strauss RA: Successful use of recombinant activated factor VII for trauma-associated hemorrhage in a patient without preexisting coagulopathy. J Trauma 2002, 52: 400-405.
Martinowitz U, Kenet G, Segal E, Luboshitz J, Lubetsky A, Ingerslev J, Lynn M: Recombinant activated factor VII for adjunctive hemorrhage control in trauma. J Trauma 2001, 51: 431-438.
Kermode JC, Zheng Q, Milner EP: Marked temperature dependence of the platelet calcium signal induced by human von Willebrand factor. Blood 1999, 94: 199-207.
Arnal D, Pineiro P, Garutti I, Olmedilla L, Sanz J, Lajara A: Recombinant activated factor VII used in a man with refractory bleeding from a stab wound injuring the liver and kidney [in Spanish]. Rev Esp Anestesiol Reanim 2004, 51: 284-288.
Martinowitz U, Zaarur M, Yaron BL, Blumenfeld A, Martonovits G: Treating traumatic bleeding in a combat setting: possible role of recombinant activated factor VII. Mil Med 2004, 169: 16-8.
Schreiber MA, Holcomb JB, Hedner U, Brundage SI, Macaitis JM, Hoots K: The effect of recombinant factor VIIa on coagulopathic pigs with grade V liver injuries. J Trauma 2002, 53: 252-257.
Martinowitz U, Holcomb JB, Pusateri AE, Stein M, Onaca N, Freidman M, Macaitis JM, Castel D, Hedner U, Hess JR: Intravenous rFVIIa administered for hemorrhage control in hypothermic coagulopathic swine with grade V liver injuries. J Trauma 2001, 50: 721-729.
Klemcke HG, Delgado A, Holcomb JB, Ryan KL, Burke A, Deguzman R, Scherer M, Cortez D, Uscilowicz J, Macaitis JM, et al.: Effect of recombinant FVIIa in hypothermic, coagulopathic pigs with liver injuries. J Trauma 2005, 59: 155-161.
Jones KC, Mann KG: A model for the tissue factor pathway to thrombin. II. A mathematical simulation. J Biol Chem 1994, 269: 23367-23373.
Telgt DS, Macik BG, McCord DM, Monroe DM, Roberts HR: Mechanism by which recombinant factor VIIa shortens the aPTT: activation of factor X in the absence of tissue factor. Thromb Res 1989, 56: 603-609. 10.1016/0049-3848(89)90268-5
Mayo A, Misgav M, Kluger Y, Geenberg R, Pauzner D, Klausner J, Ben-Tal O: Recombinant activated factor VII (NovoSeven): addition to replacement therapy in acute, uncontrolled and life-threatening bleeding. Vox Sang 2004, 87: 34-40. 10.1111/j.1423-0410.2004.00533.x
Chuansumrit A, Nuntnarumit P, Okascharoen C, Teeraratkul S, Suwansingh S, Supapannachart S: The use of recombinant activated factor VII to control bleeding in a preterm infant undergoing exploratory laparotomy. Pediatrics 2002, 110: 169-171. 10.1542/peds.110.1.169
Hoffman R, Mahajana A, Agmon P, Baruch Y, Brenner B: Successful use of recombinant activated factor VII (Novoseven) in controlling severe intra-abdominal bleeding after liver needle biopsy. Thromb Haemost 2002, 87: 346-347.
Kenet G, Walden R, Eldad A, Martinowitz U: Treatment of traumatic bleeding with recombinant factor VIIa. Lancet 1999, 354: 1879. 10.1016/S0140-6736(99)05155-7
Martinowitz U, Kenet G, Lubetski A, Luboshitz J, Segal E: Possible role of recombinant activated factor VII (rFVIIa) in the control of hemorrhage associated with massive trauma. Can J Anaesth 2002, 49: S15-S20.
Moscardo F, Perez F, de la Rubia J, Balerdi B, Lorenzo JI, Senent ML, Aznar I, Carceller S, Sanz MA: Successful treatment of severe intra-abdominal bleeding associated with disseminated intravascular coagulation using recombinant activated factor VII. Br J Haematol 2001, 114: 174-176. 10.1046/j.1365-2141.2001.02878.x
Segal S, Shemesh IY, Blumental R, Yoffe B, Laufer N, Mankuta D, Mazonr M, Zohar S, Schiff E, Martinovitz U: The use of recombinant factor VIIa in severe postpartum hemorrhage. Acta Obstet Gynecol Scand 2004, 83: 771-772. 10.1111/j.0001-6349.2004.00501.x
Tobias JD, Groeper K, Berkenbosch JW: Preliminary experience with the use of recombinant factor VIIa to treat coagulation disturbances in pediatric patients. South Med J 2003, 96: 12-16. 10.1097/01.SMJ.0000047629.79538.82
Tobias JD: Synthetic factor VIIa to treat dilutional coagulopathy during posterior spinal fusion in two children. Anesthesiology 2002, 96: 1522-1525. 10.1097/00000542-200206000-00039
Park P, Fewel ME, Garton HJ, Thompson BG, Hoff JT: Recombinant activated factor VII for the rapid correction of coagulopathy in nonhemophilic neurosurgical patients. Neurosurgery 2003, 53: 34-38. 10.1227/01.NEU.0000068830.54968.A8
Goodnough LT, Lublin DM, Zhang L, Despotis G, Eby C: Transfusion medicine service policies for recombinant factor VIIa administration. Transfusion 2004, 44: 1325-1331. 10.1111/j.1537-2995.2004.04052.x
Carr ME Jr, Martin EJ: Recombinant factor VIIa: clinical applications for an intravenous hemostatic agent with broad-spectrum potential. Exp Rev Cardiovasc Ther 2004, 2: 661-674. 10.1586/14779072.2.5.661
Roberts HR, Monroe DM, White GC: The use of recombinant factor VIIa in the treatment of bleeding disorders. Blood 2004, 104: 3858-3864. 10.1182/blood-2004-06-2223
Key NS, Nelsestuen GL: Views on methods for monitoring recombinant factor VIIa in inhibitor patients. Semin Hematol 2004, 41: 51-54. 10.1053/j.seminhematol.2003.11.011
Eikelboom JW, Bird R, Blythe D, Coyle L, Gan E, Harvey M, Isbister J, Leahy M, McIlroy D, Rahimpanah F, et al.: Recombinant activated factor VII for the treatment of life-threatening haemorrhage. Blood Coagul Fibrinolysis 2003, 14: 713-717. 10.1097/00001721-200312000-00004
Moisescu E, Ardelean L, Simion I, Muresan A, Ciupan R: Recombinant factor VIIa treatment of bleeding associated with acute renal failure. Blood Coagul Fibrinolysis 2000, 11: 575-577.
Bernstein DE, Jeffers L, Erhardtsen E, Reddy KR, Glazer S, Squiban P, Bech R, Hedner U, Schiff ER: Recombinant factor VIIa corrects prothrombin time in cirrhotic patients: a preliminary study. Gastroenterology 1997, 113: 1930-1937. 10.1053/gast.1997.v113.pm9247455
Chuansumrit A, Treepongkaruna S, Phuapradit P: Combined fresh frozen plasma with recombinant factor VIIa in restoring hemostasis for invasive procedures in children with liver diseases. Thromb Haemost 2001, 85: 748-749.
Erhardtsen E, Nony P, Dechavanne M, Ffrench P, Boissel JP, Hedner U: The effect of recombinant factor VIIa (NovoSeven) in healthy volunteers receiving acenocoumarol to an International Normalized Ratio above 2.0. Blood Coagul Fibrinolysis 1998, 9: 741-748.
Friederich PW, Henny CP, Messelink EJ, Geerdink MG, Keller T, Kurth KH, Buller HR, Levi M: Effect of recombinant activated factor VII on perioperative blood loss in patients undergoing retropubic prostatectomy: a double-blind placebo-controlled randomised trial. Lancet 2003, 361: 201-205. 10.1016/S0140-6736(03)12268-4
Girard P, Nony P, Erhardtsen E, Delair S, Ffrench P, Dechavanne M, Boissel JP: Population pharmacokinetics of recombinant factor VIIa in volunteers anticoagulated with acenocoumarol. Thromb Haemost 1998, 80: 109-113.
Jeffers L, Chalasani N, Balart L, Pyrsopoulos N, Erhardtsen E: Safety and efficacy of recombinant factor VIIa in patients with liver disease undergoing laparoscopic liver biopsy. Gastroenterology 2002, 123: 118-126. 10.1053/gast.2002.34164
Jeroukhimov I, Jewelewicz D, Zaias J, Hensley G, MacLeod J, Cohn SM, Rashid Q, Pernas F, Ledford MR, Gomez-Fein E, et al.: Early injection of high-dose recombinant factor VIIa decreases blood loss and prolongs time from injury to death in experimental liver injury. J Trauma 2002, 53: 1053-1057.
Lodge JP, Jonas S, Oussoultzoglou E, Malago M, Jayr C, Cherqui D, Anthuber M, Mirza DF, Kuhlman L, Bechstein WO, et al.: Recombinant coagulation factor VIIa in major liver resection: a randomized, placebo-controlled, double-blind clinical trial. Anesthesiology 2005, 102: 269-275. 10.1097/00000542-200502000-00006
Pusateri AE, Ryan KL, Delgado AV, Martinez RS, Uscilowicz JM, Cortez DS, Martinowitz U: Effects of increasing doses of activated recombinant factor VII on haemostatic parameters in swine. Thromb Haemost 2005, 93: 275-283.
Schreiber MA, Holcomb JB, Hedner U, Brundage SI, Macaitis JM, Aoki N, Meng ZH, Tweardy DJ, Hoots K: The effect of recombinant factor VIIa on noncoagulopathic pigs with grade V liver injuries. J Am Coll Surg 2003, 196: 691-697. 10.1016/S1072-7515(02)01835-5
Sondeen JL, Pusateri AE, Hedner U, Yantis LD, Holcomb JB: Recombinant factor VIIa increases the pressure at which rebleeding occurs in porcine uncontrolled aortic hemorrhage model. Shock 2004, 22: 163-168. 10.1097/01.shk.0000129202.76706.bd
Rao LV, Rapaport SI: Factor VIIa-catalyzed activation of factor X independent of tissue factor: its possible significance for control of hemophilic bleeding by infused factor VIIa. Blood 1990, 75: 1069-1073.
Shima M: Understanding the hemostatic effects of recombinant factor VIIa by clot wave form analysis. Semin Hematol 2004, 41: 125-131. 10.1053/j.seminhematol.2003.11.021
Meijer K, Hendriks HG, de Wolf JT, Klompmaker IJ, Lisman T, Hagenaars AA, Sloof MJ, Porte RJ, van der Meer J: Recombinant factor VIIa in orthotopic liver transplantation: influence on parameters of coagulation and fibrinolysis. Blood Coagul Fibrinolysis 2003, 14: 169-174. 10.1097/00001721-200302000-00008
Cid AR, Lorenzo JI, Haya S, Montoro JM, Casana P, Aznar JA: A comparison of FVII:C and FVIIa assays for the monitoring of recombinant factor VIIa treatment. Haemophilia 2001, 7: 39-41. 10.1046/j.1365-2516.2001.00478.x
Chuansumrit A, Suwannuraks M, Sri-Udomporn N, Pongtanakul B, Worapongpaiboon S: Recombinant activated factor VII combined with local measures in preventing bleeding from invasive dental procedures in patients with Glanzmann thrombasthenia. Blood Coagul Fibrinolysis 2003, 14: 187-190. 10.1097/00001721-200302000-00011
Potapov EV, Pasic M, Bauer M, Hetzer R: Activated recombinant factor VII for control of diffuse bleeding after implantation of ventricular assist device. Ann Thorac Surg 2002, 74: 2182-2183. 10.1016/S0003-4975(02)04105-X
Villar A, Aronis S, Morfini M, Santagostino E, Auerswald G, Thomsen HF, Erhardtsen E, Giangrande PL: Pharmacokinetics of activated recombinant coagulation factor VII (NovoSeven) in children vs. adults with haemophilia A. Haemophilia 2004, 10: 352-359. 10.1111/j.1365-2516.2004.00925.x
Hemker HC, Giesen P, AlDieri R, Regnault V, deSmed E, Wagenvoord R, Lecompte T, Beguin S: The calibrated automated thrombogram (CAT): a universal routine test for hyper- and hypocoagulability. Pathophysiol Haemost Thromb 2002, 32: 249-253. 10.1159/000073575
Sorensen B, Johansen P, Christiansen K, Woelke M, Ingerslev J: Whole blood coagulation thrombelastographic profiles employing minimal tissue factor activation. J Thromb Haemost 2003, 1: 551-558. 10.1046/j.1538-7836.2003.00075.x
Sorensen B, Ingerslev J: Thromboelastography and recombinant factor VIIa-hemophilia and beyond. Semin Hematol 2004, 41: 140-144. 10.1053/j.seminhematol.2003.11.024
Sorensen B, Ingerslev J: Whole blood clot formation phenotypes in hemophilia A and rare coagulation disorders. Patterns of response to recombinant factor VIIa. J Thromb Haemost 2004, 2: 102-110. 10.1111/j.1538-7836.2004.00528.x
Hendriks HG, van der Maaten JM, de Wolf J, Waterbolk TW, Slooff MJ, van der MJ: An effective treatment of severe intractable bleeding after valve repair by one single dose of activated recombinant factor VII. Anesth Analg 2001, 93: 287-289. 10.1097/00000539-200108000-00009
Hendriks HG, Meijer K, de Wolf JT, Porte RJ, Klompmaker IJ, Lip H, Sloof MJ, van der Meer J: Effects of recombinant activated factor VII on coagulation measured by thromboelastography in liver transplantation. Blood Coagul Fibrinolysis 2002, 13: 309-313. 10.1097/00001721-200206000-00006
Tanaka KA, Waly AA, Cooper WA, Levy JH: Treatment of excessive bleeding in Jehovah's Witness patients after cardiac surgery with recombinant factor VIIa (NovoSeven). Anesthesiology 2003, 98: 1513-1515. 10.1097/00000542-200306000-00034
Cariappa R, Wilhite TR, Parvin CA, Luchtman-Jones L: Comparison of PFA-100 and bleeding time testing in pediatric patients with suspected hemorrhagic problems. J Pediatr Hematol Oncol 2003, 25: 474-479. 10.1097/00043426-200306000-00009
Almeida AM, Khair K, Hann I, Liesner R: The use of recombinant factor VIIa in children with inherited platelet function disorders. Br J Haematol 2003, 121: 477-481. 10.1046/j.1365-2141.2003.04286.x
Gabriel DA, Carr M, Roberts HR: Monitoring coagulation and the clinical effects of recombinant factor VIIa. Semin Hematol 2004, 41: 20-24. 10.1053/j.seminhematol.2003.11.005
Acknowledgements
We thank Saulius Butenas, PhD and Dougald M Monroe, III, PhD for valuable discussions on the mechanisms of action of rFVIIa. The opinions or assertions expressed herein are the private views of the authors and are not to be construed as official or as reflecting the views of the US Department of the Army or the US Department of Defense.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Pusateri, A.E., Park, M.S. Mechanistic implications for the use and monitoring of recombinant activated factor VII in trauma. Crit Care 9 (Suppl 5), S15 (2005). https://doi.org/10.1186/cc3781
Published:
DOI: https://doi.org/10.1186/cc3781