Abstract
Introduction
The aim of the study was to determine whether the use of a nurses' protocol-directed weaning procedure, based on the French intensive care society (SRLF) consensus recommendations, was associated with reductions in the duration of mechanical ventilation and intensive care unit (ICU) length of stay in patients requiring more than 48 hours of mechanical ventilation.
Methods
This prospective study was conducted in a university hospital ICU from January 2002 through to February 2003. A total of 104 patients who had been ventilated for more than 48 hours and were weaned from mechanical ventilation using a nurses' protocol-directed procedure (cases) were compared with a 1:1 matched historical control group who underwent conventional physician-directed weaning (between 1999 and 2001). Duration of ventilation and length of ICU stay, rate of unsuccessful extubation and rate of ventilator-associated pneumonia were compared between cases and controls.
Results
The duration of mechanical ventilation (16.6 ± 13 days versus 22.5 ± 21 days; P = 0.02) and ICU length of stay (21.6 ± 14.3 days versus 27.6 ± 21.7 days; P = 0.02) were lower among patients who underwent the nurses' protocol-directed weaning than among control individuals. Ventilator-associated pneumonia, ventilator discontinuation failure rates and ICU mortality were similar between the two groups.
Discussion
Application of the nurses' protocol-directed weaning procedure described here is safe and promotes significant outcome benefits in patients who require more than 48 hours of mechanical ventilation.
Similar content being viewed by others
Introduction
The duration of weaning from mechanical ventilation (MV) represents a large proportion of the overall ventilation period [1]. The time from initiation of weaning to successful endotracheal extubation may account for as much as 40% of the overall ventilatory time [1]. A great number of studies have demonstrated that prompt recognition of reversal of respiratory failure using standardized procedures and daily screening may shorten the overall duration of MV [2–5]. However, those studies were mainly conducted by respiratory therapists in North American intensive care units (ICUs), whereas in Europe the respiratory therapist's roles are mainly assumed by nurses and physicians. Despite the accumulating evidence to support their routine use, the value of standardized weaning procedures continues to be of clinical and academic interest [6].
In October 2001, the French intensive care society (Société de Réanimation de Langue Francaise) organized a consensus conference to develop recommendations for MV weaning in the ICU [7]. The aim of the present prospective cohort study, which included a matched historical control group, was to determine whether a routine nurses' protocol-directed weaning procedure based on these recommendations and daily screening were efficient in terms of MV duration and ICU length of stay (LOS) in patients who required more than 48 hours of MV.
Methods
Study design
This prospective study was conducted in the 12-bed ICU of an 800-bed teaching hospital from January 2002 to February 2003. We employed a matched control group (1:1 matching) of patients identified from a historical database.
Selection of patients and controls
Screened patients were those who required more than 48 hours of MV and who satisfied eligibility criteria (see below) for a spontaneous breathing trial (SBT). Exclusion criteria were tracheostomy before ICU admission or within the first 48 hours of ICU management, and age under 18 years.
A computer-generated list of potential control individuals was obtained from a historical database of patients attending the same ICU (977 patients from 1999 to 2001). Controls were selected based on matching in terms of the following criteria: age (±5 years), sex, Simplified Acute Physiology Score (SAPS) II (±5 points; calculated within the first 24 hours of ICU admission), and admission diagnosis. The list of potential controls was reviewed for the best possible match, giving a ranking priority to SAPS II, followed by age, sex and then diagnosis.
Study protocol
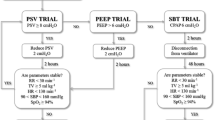
The study protocol was written according to the final recommendations of the Société de Réanimation de Langue Francaise's consensus conference on weaning. Patient eligibility for the weaning procedure was identified by daily screening by nurses. Screening was deemed to start immediately after ICU admission. The eligibility criteria for a SBT were the following: fractional inspired oxygen <50%; positive end-expiratory pressure <5 cmH2O; no vasopressor infusion; no sedative agent infusion; and response to simple orders. Physician approval for initiation of SBT was not required. A planned SBT duration of 90 min was employed, and SBTs were always performed using a T-piece. The SBT was terminated before 90 min had elapsed and considered a failure if any of the following criteria were satisfied: pulse oximetry <90%, a respiratory rate >35 breaths/min, a heart rate or a systolic arterial pressure variation >20%, or occurrence of patient agitation. All of these criteria for failure were specifically recorded. A SBT was considered to be successful when the patient could breathe spontaneously for 90 min. Physicians were asked to approve discontinuation of MV following a successful SBT. Extubation was therefore performed if cough was subjectively considered efficient, and if a leak test was considered positive (inspiratory and/or expiratory air leaks after cuff deflation). If the SBT was not well tolerated, then the failure criteria were specifically recorded and the patient returned to their prior ventilator settings and mode. Such patients were then subjected to screening the following day (Fig. 1).
Mechanical ventilation weaning protocol. Daily nurse screening identified patients eligible for weaning. A spontaneous breathing trial was considered to be successful when the patient could breathe spontaneously for 90 min without clinical intolerance. For such patients, physicians were then asked to approve discontinuation of mechanical ventilation. If the spontaneous breathing trial was not tolerated, then the patient was returned to their prior ventilator settings and screened the day after. FiO2, fractional inspired oxygen; PEEP, positive end-expiratory pressure; SpO2, pulse oximetry.
Pre-protocol weaning management (historical controls)
Before establishment of the nurse's protocol-directed weaning procedure, routine weaning from MV was 'physician directed', as in most European ICUs. Physician's individual preferences determined the mode of weaning (volume assisted controlled, pressure support ventilation, or T-piece). Weaning criteria were not monitored daily. The decision to extubate after a successful weaning procedure was also physician directed.
Definitions
All definitions were selected a priori before study analysis. Admission diagnosis was divided into four main groups: medicine, surgery, neurosurgery and acute exacerbations in chronic obstructive pulmonary disease. Ventilator-associated pneumonia was defined as the initiation of antibiotics and at least two of the following criteria: positive protected bronchoscopy cultures; fever or rising leucocyte count; and characteristic chest radiograph findings. The duration of ventilation was calculated as follows: (day of extubation + 1) - (day of intubation). Successful discontinuation of MV was defined as continuous independence from ventilator support for a period of at least 48 hours. Unsuccessful MV discontinuation was defined as need for noninvasive ventilation and/or reintubation within a 48 hour period. Criteria to initiate noninvasive ventilation following extubation were occurrence of clinical signs of acute respiratory failure, with or without hypercapnia.
Outcomes
The overall duration of MV and the ICU LOS were considered primary outcomes. Secondary outcomes were the overall incidence of ventilator-associated pneumonia, unsuccessful extubation rates and ICU mortality.
Statistical analysis
Categorical variables were expressed as percentage and continuous variables as mean ± standard deviation. P < 0.05 was considered statistically significant. Percentages were compared using χ2 tests, and means using Student's t-test. Kaplan–Meier curves were used to determine the probability of remaining ventilated during the overall ICU LOS; curves were compared using the log-rank test. When patients died before discontinuation of MV, matched data were censored within the analysis.
Results
Physiological variables
During the prospective study period 392 patients were admitted to our ICU, of whom 384 patients required ventilatory support. A total of 297 patients were mechanically ventilated through an endotracheal tube, of whom 204 required MV for longer than 48 hours. Among these 204 eligible patients, 100 were excluded from analysis because they died prior to initiation of any weaning procedure (85 patients) or because they were tracheostomized before admission or within the first 48-hour period (15 patients; Fig. 2). After 1:1 matching, 208 patients were finally included in the analysis: 104 patients in the prospective routine nurse's protocol-directed weaning procedure (cases) and 104 patients in the standard physician-directed weaning procedure (controls). Matching was successful for all parameters, and patient demographic variables were similar within groups (age 56 ± 18 years, sex ratio [male/female] 3/2; SAPS II = 49 ± 18). Admission diagnoses were similarly distributed within groups (Table 1).
Duration of mechanical ventilation and intensive care unit length of stay
All patients were under volume-assisted controlled or pressure support ventilation before entering the weaning procedure. The overall MV duration was 16.6 ± 13 days within cases, and 22.5 ± 21 days within controls (P = 0.02); this difference between groups is illustrated by Kaplan–Meier analysis in Fig. 3. The ICU LOS was 21.6 ± 14.3 days within cases and 27.6 ± 21.7 days within controls (P = 0.02). In subgroup analysis, the duration of MV and ICU LOS were shorter for medical patients (Table 2).
Kaplan–Meier curves of the risk for remaining mechanically ventilated in protocol-directed (cases) versus physician-directed weaning groups (controls). The protocol-directed weaning procedure allowed reduction in the overall duration of mechanical ventilation, whatever the patient's diagnosis. The overall mechanical ventilation duration was 16.6 ± 13 days in cases and 22.5 ± 21 days in controls (P = 0.02).
Outcomes
No significant differences in unsuccessful MV discontinuation rates were observed between groups (31% for cases versus 35% for controls; P = 0.81). Mortality was similar between the two groups (7% for cases versus 5% for controls; P = 0.92). A positive trend toward a decrease in ventilator-associated pneumonia rate was observed for the cases (20.2% versus 31%; P = 0.12; Table 3).
Discussion
The present study was designed to determine the clinical benefit of a nurse's protocol-directed weaning procedure in a broad range of ICU patients (including both medical and surgical patients) who had not been disconnected from the ventilator after 48 hours of MV. Our findings demonstrate the effectiveness of such a procedure performed on a routine basis. The nurse's protocol-directed weaning procedure reduced the duration of MV and the overall ICU LOS in patients who remained dependent on MV after a 48-hour period, without any increase in adverse events or in rate of unsuccessful extubation. Easily implemented, this protocol-directed weaning procedure synthesizes an approach that incorporates the following: daily screening by nursing staff and a single daily 90 min SBT with T-piece trial in selected patients. The criteria used in this procedure to screen patients for readiness for the weaning trial were very simple clinical criteria.
Some authors have demonstrated a key role for daily screening using predetermined criteria during the weaning process [2, 4]. In both of those studies, patients who satisfied the criteria were subjected to a 2 hour trial of CPAP while they remained attached to the mechanical ventilator circuit. How exactly a SBT should be performed remains subject to debate, and its optimal duration is not known, although there are data suggesting that it may be shortened [8–11]. For the routine procedure, we arbitrarily chose a 90 min duration and to perform the trial while the patient was disconnected from the ventilator, without adding any positive end-expiratory pressure.
The mean MV duration and ICU LOS found in this study differ significantly from those of previous studies [2, 3, 12]. In the study by Ely and coworkers [2] patients received MV for a median of 4.5 days, and in the study by Esteban and coworkers [10] patients were ventilated for a median of 5 days. Moreover, in the study by Ely and colleagues the ICU LOS was similar between groups. The main reasons for such a difference between our study and the previous ones are the higher mean SAPS II in our patients (49 ± 18 in both groups) and the selection of patients who survived and were not weaned from MV after a 48 hour period (i.e. patients whose conditions probably remained unstable for a long period and/or those who may be considered 'difficult to wean'). Therefore, we believe that we selected patients who may derive particular benefit from a decrease in the duration of MV.
The unsuccessful extubation rate also appears rather high in our patients as compared with previous studies (31% within cases versus 35% within controls) [10, 13–15]. However, this finding must be interpreted with caution because we considered unsuccessful extubation to be the need for any form of ventilatory assistance within a 48 hour period (either delivered noninvasively via face mask or invasively via an endotracheal tube), whereas in the vast majority of other studies unsuccessful extubation was considered just as need for endotracheal intubation. If we consider the reintubation rate alone, the incidence of extubation failure decreases to 21% in cases and 18% in controls. However, one may observe that, apart from earlier extubation, the failure rates were similar between the two groups (i.e. patients were not withdrawn too early, as compared with the 'standard' procedure).
Apart from the rather high mean SAPS II levels, the overall mortality rate in our study appears rather low in both groups (5%). However, in accordance with the analysis protocol we excluded patients who died before the predetermined weaning criteria were satisfied, and so this finding cannot be considered to be an adequate reflection of overall ICU mortality rate.
Case series with historical controls have advantages over randomized trials when the effects of routine daily procedures are studied. Indeed, it is easier for a broad range of nursing staff to institute a protocol throughout an entire ICU population than it is to limit it to specific monitored patients. Moreover, there is no risk for crossover effect, by which the staff may modify their behaviour toward control patients and thus blur the distinction between groups.
On the other hand the nonrandomized design of our study is a major limitation. First, only randomization can ensure comparability between cases and controls. Even if cases and controls were matched for age, sex, SAPS II and diagnosis on admission, selection bias cannot be fully excluded and might account for part of our results. Second, evolution of medical care during the study period might have influenced our results [16]. However, the use of sedatives and paralytics, and routine patient positioning and ventilatory settings did not fundamentally change over the period of interest (1999–2003). For example, patients with acute respiratory distress syndrome have been ventilated using a small tidal volume and an 'open lung approach' since publication of the study by Amato and coworkers [17].
Conclusion
This study demonstrates that a routine and simply applied nurse's protocol-directed weaning procedure was safe and promoted major clinical and outcome benefits for patients requiring MV over a 48 hour period. These benefits were obtained without increasing the average number of complications or the rate of unsuccessful extubation.
Key messages
-
A simply applied nurse's protocol-directed weaning procedure was safe and promoted major clinical and outcome benefits for patients.
-
Protocol-directed weaning procedure should be used in all ICUs.
Abbreviations
- ICU:
-
= intensive care unit
- LOS:
-
= length of stay
- MV:
-
= mechanical ventilation
- SAPS:
-
= Simplified Acute Physiology Score
- SBT:
-
= spontaneous breathing trial.
References
Esteban A, Alia I, Ibanez J, Benito S, Tobin MJ: Modes of mechanical ventilation and weaning. A national survey of Spanish hospitals. The Spanish Lung Failure Collaborative Group. Chest 1994, 106: 1188-1193.
Ely EW, Baker AM, Dunagan DP, Burke HL, Smith AC, Kelly PT, Johnson MM, Browder RW, Bowton DL, Haponik EF: Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med 1996, 335: 1864-1869. 10.1056/NEJM199612193352502
Horst HM, Mouro D, Hall-Jenssens RA, Pamukov N: Decrease in ventilation time with a standardized weaning process. Arch Surg 1998, 133: 483-488. discussion 488–489 10.1001/archsurg.133.5.483
Kollef MH, Shapiro SD, Silver P, St John RE, Prentice D, Sauer S, Ahrens TS, Shannon W, Baker-Clinkscale D: A randomized, controlled trial of protocol-directed versus physician-directed weaning from mechanical ventilation. Crit Care Med 1997, 25: 567-574. 10.1097/00003246-199704000-00004
Marelich GP, Murin S, Battistella F, Inciardi J, Vierra T, Roby M: Protocol weaning of mechanical ventilation in medical and surgical patients by respiratory care practitioners and nurses. Chest 2000, 118: 459-467. 10.1378/chest.118.2.459
MacIntyre N: Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest 2001, 120: 375S-396S. 10.1378/chest.120.6_suppl.375S
Richard C, Beydon L, Cantagrel S, Cuvelier A, Fauroux B, Garo B, Holzapfel L, Lesieur O, Levraut J, Maury E, et al.: 21st Consensus Conference on Intensive Care and Emergency Medicine: mechanical ventilation weaning [in French]. Réanimation 2001, 10: 697-698. 10.1016/S1164-6756(00)00080-3
Esteban A, Frutos F, Tobin MJ, Alia I, Solsona JF, Valverdu I, Fernandez R, de la Cal MA, Benito S, Tomas R, et al.: A comparison of four methods of weaning patients from mechanical ventilation. Spanish Lung Failure Collaborative Group. N Engl J Med 1995, 332: 345-350. 10.1056/NEJM199502093320601
Brochard L, Rauss A, Benito S, Conti G, Mancebo J, Rekik N, Gasparetto A, Lemaire F: Comparison of three methods of gradual withdrawal from ventilatory support during weaning from mechanical ventilation. Am J Respir Crit Care Med 1994, 150: 896-903.
Esteban A, Alia I, Tobin MJ, Gil A, Gordo F, Vallverdu I, Blanch L, Bonet A, Vazquez A, de Pablo R, et al.: Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1999, 159: 512-518.
Vallverdu I, Calaf N, Subirana M, Net A, Benito S, Mancebo J: Clinical characteristics, respiratory functional parameters, and outcome of a two-hour T-piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med 1998, 158: 1855-1862.
Marelich GP, Murin S, Battistella F, Inciardi J, Vierra T, Roby M: Protocol weaning of mechanical ventilation in medical and surgical patients by respiratory care practitioners and nurses: effect on weaning time and incidence of ventilator-associated pneumonia. Chest 2000, 118: 459-467. 10.1378/chest.118.2.459
Epstein SK, Ciubotaru RL, Wong JB: Effect of failed extubation on the outcome of mechanical ventilation. Chest 1997, 112: 186-192.
Esteban A, Alia I, Gordo F, Fernandez R, Solsona JF, Vallverdu I, Macias S, Allegue JM, Blanco J, Carriedo D, et al.: Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation. The Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1997, 156: 459-465.
Chan PK, Fischer S, Stewart TE, Hallett DC, Hynes-Gay P, Lapinsky SE, MacDonald R, Mehta S: Practising evidence-based medicine: the design and implementation of a multidisciplinary team-driven extubation protocol. Crit Care 2001, 5: 349-354. 10.1186/cc1068
Sacks H, Chalmers TC, Smith H Jr: Randomized versus historical controls for clinical trials. Am J Med 1982, 72: 233-240. 10.1016/0002-9343(82)90815-4
Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, et al.: Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 1998, 338: 347-354. 10.1056/NEJM199802053380602
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
JMT drafted the manuscript and participated in the design of the study. GP conceived the study and helped to draft the manuscript. GLG performed the statistical analysis. CGG collected data. AR colected data. JMB participated in the design of the study. EL participated in its design and coordination, and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Tonnelier, JM., Prat, G., Le Gal, G. et al. Impact of a nurses' protocol-directed weaning procedure on outcomes in patients undergoing mechanical ventilation for longer than 48 hours: a prospective cohort study with a matched historical control group. Crit Care 9, R83 (2005). https://doi.org/10.1186/cc3030
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc3030