Abstract
Introduction
The importance of accidental catheter removal (ACR) lies in the complications caused by the removal itself and by catheter reinsertion. To the best of our knowledge, no studies have analyzed accidental removal of various types of catheters in the intensive care unit (ICU). The objective of the present study was to analyze the incidence of ACR for all types of catheters in the ICU.
Methods
This was a prospective and observational study, conducted in a 24-bed medical/surgical ICU in a university hospital. We included all consecutive patients admitted to the ICU over 18 months (1 May 2000 to 31 October 2001). The incidences of ACR for all types of catheters (both per 100 catheters and per 100 catheter-days) were determined.
Results
A total of 988 patients were included. There were no significant differences in ACR incidence between the four central venous access sites (peripheral, jugular, subclavian and femoral) or between the four arterial access sites (radial, femoral, pedal and humeral). However, the incidence of ACR was higher for arterial than for central venous catheters (1.12/100 catheter-days versus 2.02/100 catheter-days; P < 0.001). The incidences of ACR/100 nonvascular catheter-days were as follows: endotracheal tube 0.79; nasogastric tube 4.48; urinary catheter 0.32; thoracic drain 0.56; abdominal drain 0.67; and intraventricular brain drain 0.66.
Conclusion
We found ACR incidences for central venous catheter, arterial catheter, endotracheal tube, nasogastric tube and urinary catheter that are similar to those reported in previous studies. We could not find studies that analyzed the ACR for thoracic, abdominal, intraventricular brain and cardiac surgical drains, but we believe that our rates are acceptable. To minimize ACR, it is necessary to monitor its incidence carefully and to implement preventive measures. In our view, according to establish quality standards, findings should be reported as ACR incidence per 100 catheters and per 100 catheter-days, for all types of catheters.
Similar content being viewed by others
Introduction
Use of catheters in critically ill patients is routine. In the European Prevalence of Infection in Intensive Care (EPIC) study [1], the following catheters were required in the management of critically ill patients: urinary catheter (75%), central venous catheter (64%), orotracheal tube (62%), arterial catheter (44%) and thoracic drain (14%). Use of catheters carries risks for complications such as nosocomial infection and accidental removal. Catheter-related infection has been studied extensively owing to the clinical and economic repercussions [2–7]. However, accidental catheter removal (ACR) has received little attention. There are considerable data on ACR of orotracheal tubes, but few reports have been published on ACR of vascular catheters and nasogastric tubes, and scarcely any on other drainage types (urinary, thoracic, abdominal, intraventricular brain or cardiac surgical drain). Furthermore, to the best of our knowledge, no studies have analyzed accidental removal of various types of catheters in the intensive care unit (ICU). The importance of ACR lies in the potentially life-threatening complications that can result from the removal itself and from catheter reinsertion. Among the complications of accidental removal of vascular catheters per se are interruption to vital drug therapy (such as inotropes/vasopressors) or renal replacement therapy, and haemorrhagic shock. Unplanned endotracheal extubation has been associated with serious complications such as arrhythmias, haemodynamic instability, aspiration pneumonia and death. ACR of thoracic drains can result in pneumothorax and/or haemothorax. Following ACR of an abdominal drain, blood and purulent fluids can accumulate, ultimately resulting in development of sepsis.
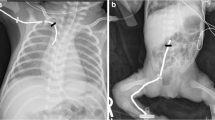
Hydrocephalus is a possible outcome following ACR of a catheter being used for intraventricular brain drainage, and ACR of a cardiac surgical drain can result in cardiac tamponade. Complications arising from subclavian or jugular venous catheter reinsertion include pneumothorax and/or haemothorax. Endotracheal reintubation can lead to nosocomial pneumonia, and reinsertion of new drains can result in haemorrhage or nosocomial infection.
The objective of the present study was to determine the incidence of ACR for all catheter types used in the ICU and to report the data in a standardized and comparable way, with a view to establishing quality standards.
Methods
An 18-month prospective study was performed that included all patients admitted to the 24-bed ICU of the Hospital Universitario de Canarias (Tenerife) between 1 May 2000 and 31 October 2001.
Interventions implemented to minimize the incidence of ACR were as follows. All patients were cared for by physicians who were board-certified in critical medicine and by nurses who were experienced in critical care. The ratio of nurses to patients was 1:2. Vital signs were recorded every hour. We standardized certain procedures, such as the method of securing endotracheal and nasogastric tubes, the use of sedation, and the use of hand and chest restraints. Active communication between staff and patients was encouraged. Unnecessary delays to elective removal of catheters and tubes were avoided; physicians and nurses were advised to be attentive and vigilant in order to minimize the likelihood of such delays. Housestaff were educated on the appropriate use of sedatives and analgesic agents. Appropriate sedation was considered to be present when patients were asleep but responsive to verbal or mild tactile stimulation. Sedation was prescribed when necessary, according to the physician's discretion. Both wrist and chest restraints were used when deemed necessary by the nursing staff. In agitated patients, nurses checked, at least once each shift, that the upper extremities were held adequately so that the patient's hands were more than 20 cm away from any catheter or tube. All central venous or arterial catheters and drains were sutured in place with 1/0 silk suture. The percutaneous entry sites of the catheters and drainages were examined and cared for, every 24 hours, by the ICU nurse assigned to the patient. Nasogastric tubes were secured to the nose using adhesive tape. The orotracheal route was preferred for endotracheal intubation. The endotracheal tubes were secured around the neck using adhesive tape, and the position of the tube at the teeth was noted at least once per shift, with the objective being to detect any short displacements and then correct the position of the tube. Two teams of staff collected the following data: age, sex, diagnosis, Acute Physiology and Chronic Health Evaluation (APACHE) II score, ICU admission and discharge dates, catheter placement and removal dates, and cause of catheter removal (planned or accidental).
The following three groups of catheters were studied: central venous catheters, including peripherally inserted central venous catheters, and jugular, subclavian and femoral access sites; arterial catheters, including radial, femoral, pedal and humeral arterial catheters; and nonvascular catheters, including endotracheal tube, nasogastric tube, urinary catheter, and thoracic, abdominal, intraventricular brain and cardiac surgical drains.
We considered ACR to be the unplanned removal of a catheter either by the patient or by the staff. The patient can cause ACR either by taking hold of the catheter in their hands or by making voluntary movements that lead directly the removal. The staff can be responsible for ACR as a consecuence of inappropriate handling.
To ensure that the recorded data were of good quality, the two teams of staff who collected the data reviewed the reports.
Statistical analysis was performed using SPSS 11.0 (SPSS Inc., Chicago, IL, USA) and LogXact 4.1 (Cytel Software, Cambridge, MA, USA) programs. Continuous variables are reported as mean with standard deviation, and categorical variables as percentages. ACR is reported as follows: percentage of catheters accidentally removed and number of accidental removals/100 catheter-days. Mean catheterization time was calculated by dividing the number of catheter-days by the number of catheterized patients. The incidence density of ACR, per 100 days of risk, between the different arterial and venous catheters was compared using Poisson distributions, and the Bonferroni correction was used to correct for multiple testing. According to Bonferroni's adjustment, P < 0.008 was considered statistically significant.
Results
A total of 988 patients were included, and 594 (60.12%) were male. The mean age of the patients was 55.63 ± 18.49 years (median 62 years, interquartile range 45–71 years), the mean APACHE II score was 13.65 ± 5.83 (median 14, interquartile range 10–18) and the mean length of ICU stay was 8.65 ± 12.34 days (median 4 days, interquartile range 2–11 days). A total of 142 (14.37%) patients died. Admission diagnoses were as follows: 491 (49.69%) heart surgery, 85 (8.60%) cardiological, 129 (12.14%) neurological, 117 (11.84%) trauma, 72 (7.29%) respiratory, 65 (6.58%) digestive and 29 (2.93%) intoxication.
Some type of central venous catheter was used in 890 of 988 patients (90.08%; Table 1). Of the 988 patients, a central venous catheter by peripheral access was employed in 257 (26.01%), jugular venous access in 618 (62.55%), subclavian venous catheterization in 321 (32.48%) and femoral venous catheterization in 111 (11.23%). No significant differences were found in the incidence of ACR between the various central venous catheters.
Some type of arterial catheter was used in 817 of 988 patients (82.69%; Table 2). Of the 988 patients, radial arterial catheterization was used in 753 (76.21%), femoral arterial access in 111 (11.23%), pedal arterial catheter in 27 (2.73%) and humeral arterial catheterization in 16 (1.62%). No significant differences were found in the incidence of ACR between the various arterial access catheters. The incidence of ACR was significantly higher in arterial than in central venous catheters (1.12/100 catheter-days versus 0.20/100 catheter-days; P < 0.001).
Data on nonvascular catheters are reported in the Table 3. Of the 988 patients, endotracheal intubation was necessary in 803 (81.27%), nasogastric tube in 861 (87.14%), urinary catheter in 874 (88.46%), drainage tube following cardiac surgery in 491 (49.69%), thoracic drain in 70 (7.08%), abdominal drain in 65 (6.57%) and intraventricular brain drainage tube in 68 (6.89%).
Discussion
Before we undertook the present study we conducted a survey of the literature, which revealed four studies on accidental removal of endotracheal tube, arterial catheter, central venous catheter and nasogastric tube [8–11], but in all of those studies there were certian limitations in the data on ACR. Specifically, accidental removal of urinary catheters was not studied in the studies apart from that by García and coworkers [9]; the various central venous and arterial catheters were not classified, except in the study conducted by Marcos and coworkers [8]; and other drains (e.g. thoracic, abdominal, intraventricular brain and cardiac surgical) were not mentioned. We could not find any studies that analyzed accidental removal of the various types of catheters in the ICU, or that reported data as a percentage of catheters accidentally removed and as ACR incidence density (number of accidental removals/100 catheter-days).
Our global ACR rates for the four central venous catheter sites (1.43% of catheters and 0.20/100 catheter-days) were similar to those published previously [8–13], which range between 0% and 7.5% of catheters and between 0 and 1.2/100 catheter-days.
Marcos and coworkers [8] analyzed accidental removal of various central venous catheters and found the following ACR incidences (presented per 100 catheters and per 100 catheter-days, respectively): subclavian 0%; jugular 5% and 1.4; femoral 15% and 1.9; and peripheral access 7.6% and 1.1. In the present study we found no differences in the incidence of ACR between the various central venous access sites. The discrepancy between our findings and those of Marcos and coworkers may be due to differences in sample sizes (72 patients in the study by Marcos and coworkers and 988 in the present study).
The previously reported ranges for global ACR incidence are 0–29% of catheters and 0–4.6/100 catheter-days [8–11]. Our global ACR findings for the four different arterial catheter sites (6.49% of catheters and 1.11/100 catheter-days) are within those ranges. In the study conducted by Marcos and coworkers [8], radial artery ACR occurred in 12% of catheters and in 1.8/100 catheter-days, and femoral artery ACR occurred in 21% of catheters. In the present study we did not find significant differences between the four arterial sites. Again, the discrepancy in findings between the present study and that conducted by Marcos and coworkers may be attributable to differences in sample sizes.
In accordance with other studies [8–10], we found a significantly higher ACR incidence for arterial catheters than for central venous catheters (1.12/100 catheter-days versus 0.20/100 catheter-days). We believe that this is attributable to the fact that the length of venous catheters inserted is greater than that of arterial catheters.
Our accidental endotracheal extubation rate was close to the lower limit reported in the literature [8–11, 14–23] (reported ranges 0–17% of tubes and 0–2.5 extubations/100 catheter-days). With respect to nasogastric tubes, previous studies [8–11] reported ACR incidences of 2–41% of tubes and 2.28–7.4/100 catheter-days; our rates were within those limits. In relation to the urinary catheter ACR, our incidences were similar to those reported in previous studies, namely 5% of catheters and 0.34/100 catheter-days [8–11]. We could not find studies that analyzed the ACR incidence of thoracic, abdominal, intraventricular brain and cardiac surgical drains, but we believe that our rates are acceptable.
Our study has two important limitations. The first is the absence of a multivariate analysis to control for possible confounders in the density incidence of ACR. The second limitation is that the study was observational, and the various vascular insertion sites were compared without randomization. Despite these limitations, we hope that we have made a contribution toward establishing quality standards with the results of the present study.
We believe that, to minimize ACR, it is necessary to monitor its incidence carefully and to implement preventive measures. Our preventive measures are similar to those employed by other investigators [8–10, 14, 23].
Conclusion
In conclusion, our ACR rates for central venous catheter, arterial catheter, endotracheal tube, nasograstric tube and urinary catheter are similar to those reported in previous studies. We could not find studies that analyzed the ACR incidence for thoracic, abdominal, intraventricular brain and cardiac surgery drains, but we believe that our rates are acceptable. We believe that to minimize ACR, it is necessary to monitor its incidence carefully and to implement preventive measures. It is necessary to analyze all types of catheter used and to report the data in a standardized and comparable manner, such as percentage of catheters accidentally removed and number of ACRs/100 catheter-days.
Key messages
In order to minimize ACR, it is necessary to monitor its incidence carefully and to implement preventive measures.
It is necessary to analyze all types of catheter used and to report the data in a standardized and comparable manner, such as percentage of catheters accidentally removed and number of ACRs/100 catheter-days.
We found that the incidence of accidental removal was not different between the various central venous access sites or between the various arterial access sites.
The incidence of accidental removal is higher for arterial than for central venous catheters.
Abbreviations
- ACR:
-
accidental catheter removal
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- ICU:
-
intensive care unit.
References
Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, Wolff M, Spencer RC, Hemmer M: The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA 1995, 274: 639-644. 10.1001/jama.274.8.639
Nyström B, Larsen SO, Dankert J: Bacteremia in surgical patients with intravenous devices: a European multicenter incidence study. The European Working Party on Control of Hospital Infections. J Hosp Infect 1983, 4: 338-349. 10.1016/0195-6701(83)90004-X
Vallés J, León C, Alvarez F, Working Group of Infectious Diseases: Nosocomial bacteremia in critically ill patients: a multicenter study evaluating epidemiology and prognosis. Clin Infect Dis 1996, 24: 387-395.
Collignon PJ: Intravascular catheter associated sepsis, a common problem: the Australian Study on Intravascular Catheter Associated Sepsis. Med J Aust 1994, 161: 374-378.
Moro ML, Vigano EF, Cozzi A: Risk factors for central venous catheter-related infections in surgical and intensive care units. The Central Venous Catheter Related Infections Study Group. Infect Control Hosp Epidemiol 1994, 15: 253-264.
Richet H, Hubert B, Nitemberg G, Andremont A, Buu-Hoy A, Ourba C, Veron M, Boisivon A, Bouvier AM: Prospective multicenter study of vascular-catheter-related complications and risk factors for positive central-catheter culture in intensive care unit patients. J Clin Microbiol 1990, 28: 2520-2525.
The National Nosocomial Infections Surveillance System: National Nosocomial Infections Surveillance (NNIS) System Report, Data Summary from October 1986–April Issued June 1998. Am J Infect Control 1998, 26: 522-533.
Marcos M, Ayuso D, González B, Carrión MI, Robles P, Muñoz M, de la Cal MA: Analysis of the accidental withdrawal of tubes, probes and catheters as a part of the program of quality control [in Spanish]. Enfermería Intensiva 1994, 3: 115-120.
García MP, López P, Eseverri C, Zazpe C, Asiain MC: Quality of care in intensive care units. Retrospective study on long-term patients [in Spanish]. Enfermería Intensiva 1998, 9: 102-108.
Carrión M, Ayuso D, Marcos M, Robles P, de la Cal MA, Alía I, Esteban A: Accidental removal of endotracheal and nasogastric tubes and intravascular catheters. Crit Care Med 2000, 28: 63-66. 10.1097/00003246-200001000-00010
Valls C, Sanz C, Jover C, Sola N, Sola M, Saez E, Ingles T, Delgado P, Cerezales J, Blasco M: Assistance quality program in intensive care units. Analysis of the effectiveness of correcting measures [in Spanish]. Enfermería Intensiva 1994, 5: 109-114.
Goni C, Perez A, Ruiz R, Carrascosa MC, Vazquez MS, Martinez A: Central venous access by the Seldinger technic in neonatology. Cir Pediatr 1999, 12: 165-167.
Fratino G, Mazzola C, Buffa P, Torre M, Castagnola E, Magillo P, Molinari AC: Mechanical complications related to indwelling central venous catheter in pediatric hematology/oncology patients. Pediatr Hematol Oncol 2001, 18: 317-324. 10.1080/088800101300312582
Coppolo DP, May JJ: Self-extubations: a 12-month experience. Chest 1990, 98: 165-169.
Vassal T, Anh NGD, Gabillet JM, Guidet B: Prospective evaluation of self-extubations in a medical intensive care unit. Intensive Care Med 1993, 19: 340-342.
Whelan J, Simpson SQ, Levy H: Unplanned extubation. Predictors of successful termination of mechanical ventilatory support. Chest 1994, 105: 1808-1812.
Giraud T, Dhainaut JF, Vaxelaure JF: Iatrogenic complications in adult Intensive Care Units: a prospective two-center study. Crit Care Med 1993, 21: 40-50.
Tindol GA, DiBenedetto RJ, Kosciuck L: Unplanned extubations. Chest 1994, 105: 1804-1807.
Rovira I, Heering CH, Zavala E, Mancebo J, Aldalia R, Alcón A: Incidence of unplanned extubation in a surgical intensive care unit [abstract]. Intensive Care Med 2001, 27: s269. 10.1007/s001340000796
Solsona JF, Marrugat J, Vázquez A, Miró G, Martínez R, Nolla J: Quality assurance in critically ill patients: recording of complications related to mechanical ventilation [in Spanish]. Medicina Intensiva 1998, 22: 91-95.
Betbesé AJ, Pérez M, Bak E, Ballús J, Net A, Mancebo J: Incidence and consequences of unplanned endotracheal extubation [in Spanish; abstract]. Medicina Intensiva 1994, 18: s46.
Miró G, Solsona JF, Marrugat J, Nolla J, Vázquez A, Alvarez F, Albert I: Self-extubation and mortality [abstract]. Medicina Intensiva 1995, 19: s76.
Chiang AA, Lee KC, Lee JC, Wei CH: Effectiveness of a continuous quality improvement program aiming to reduce unplanned extubation: a prospective study. Intensive Care Med 1996, 22: 1269-1271. 10.1007/s001340050250
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Lorente, L., Huidobro, M.S., Martín, M.M. et al. Accidental catheter removal in critically ill patients: a prospective and observational study. Crit Care 8, R229 (2004). https://doi.org/10.1186/cc2874
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc2874