Abstract
Background
Our aim was to examine whether serial blood lactate levels could be used as predictors of outcome.
Methods
We prospectively studied 44 high-risk, hemodynamically stable, surgical patients. Blood lactate values, mean arterial pressure, heart rate and urine output were obtained at patient admission to the study, at 12, 24 and 48 hours.
Results
The nonsurvivors (n = 7) had similar blood lactate levels initially (3.1 ± 2.3 mmol/l versus 2.2 ± 1.0 mmol/l, P = not significant [NS]), but had higher levels after 12 hours (2.9 ± 1.7 mmol/l versus 1.6 ± 0.9 mmol/l, P = 0.012), after 24 hours (2.1 ± 0.6 mmol/l versus 1.5 ± 0.7 mmol/l, P = NS) and after 48 hours (2.7 ± 1.8 mmol/l versus 1.9 ± 1.4 mmol/l, P = NS) as compared with the survivors (n = 37). Arterial bicarbonate concentrations increased significantly in survivors and were higher than in nonsurvivors after 24 hours (22.9 ± 5.2 mEq/l versus 16.7 ± 3.9 mEq/l, P = 0.01) and after 48 hours (23.1 ± 4.1 mEq/l versus 17.6 ± 7.1 mEq/l, P = NS). The PaO2/FiO2 ratio was higher in survivors initially (334 ± 121 mmHg versus 241 ± 133 mmHg, P = 0.03) and remained elevated for 48 hours. There were no significant differences in mean arterial pressure, heart rate, and arterial blood oxygenation at any time between survivors and nonsurvivors. The intensive care unit stay (40 ± 42 hours versus 142 ± 143 hours, P < 0.001) and the hospital stay (12 ± 11 days versus 24 ± 17 days, P = 0.022) were longer for nonsurvivors than for survivors. The Simplified Acute Physiology Score II score was higher for nonsurvivors than for survivors (34 ± 9 versus 25 ± 14, P = NS). The urine output was slightly lower in the nonsurvivor group (P = NS). The areas under the receiving operating characteristic curves were larger for initial values of Simplified Acute Physiology Score II and blood lactate for predicting death.
Conclusion
Elevated blood lactate levels are associated with a higher mortality rate and postoperative complications in hemodynamically stable surgical patients.
Similar content being viewed by others
Introduction
Acute hypoperfusion can be characterized by an imbalance between oxygen demand and oxygen delivery to the tissues. It has been proposed that organ damage in critical illness is due to inadequate oxygen delivery that fails to satisfy metabolic needs. Hypoperfusion is largely responsible for subsequent risk of multiple system organ failure. Experimentally and clinically, whenever the oxygen delivery is inadequate to maintain normal tissue oxygenation, blood lactate levels start to rise [1–6]. Blood lactate levels are closely related to outcome in critically ill patients [4, 6–11]. We have also shown, like other workers, that failure of serum lactate levels to reach normal values within a specific time during critical illness could be even more closely related to survival than the initial level [6, 11–14]. However, most studies have shown the prognostic value of blood lactate levels in patients with signs of clinical shock.
Resuscitation of surgical patients has traditionally been guided by the normalization of vital signs, such as blood pressure, urine output, and heart rate; and only when hemodynamic instability invasive monitoring is required. However, these endpoints have revealed the inadequacy of relying solely upon vital signs in resuscitation of critically ill patients [15]. The ideal marker of adequate resuscitation should be able to assess resolution of hypoperfusion. There have been few studies to date evaluating the prognostic value of occult hypoperfusion, defined as elevated blood lactate levels without signs of clinical shock in critically ill patients [16]. Several studies by the same group of investigators in trauma patients have shown that persistent occult hypoperfusion is associated with increased morbi-mortality, and early correction seems to improve outcome [7, 8, 16]. Polonen and colleagues have shown in cardiac surgical patients that a goal-oriented protocol targeting a normal blood lactate can shorten the length of stay [17]. In addition, Rivers and colleagues have shown that interventions targeted on hemodynamic endpoints can decrease the mortality of severe septic patients with elevated blood lactate levels [18].
There has not previously been a study examining the prognostic value of blood lactate values on the outcome of high-risk, hemodynamically stable, surgical patients. We therefore conducted the present study to examine whether serial blood lactate levels could be used as predictors of outcome in this population.
Patients and methods
Patients
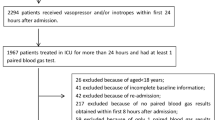
We prospectively studied 44 consecutive adult patients (30 male, 14 female) admitted to a general intensive care unit (ICU) after high-risk noncardiac surgery (Table 1). All high-risk surgical patients were admitted to the study if they showed two or more of the following inclusion criteria: major elective operation for removal of carcinoma that lasted at least 2 hours; elective repair of an abdominal aortic aneurysm; age > 70 years and evidence of limited physiologic reserve of one or more vital organs (creatinine > 2 mg/dl, cardiac ejection fraction < 50%); acute abdominal catastrophe (e.g. pancreatitis, peritonitis); and previous disease of a vital organ, defined as compensated or prior congestive cardiac failure, previous clinical indication of ischemic heart disease (previous myocardial infarction, ST–T depression during stress testing or Q-waves on electrocardiogram), cardiac arrhythmia with chronic use of antiarrhythmic drugs, chronic obstructive pulmonary disease as diagnosed by spirometric tests, or chronic liver disease Child B or Child C. The exclusion criteria were hemodynamic instability before or during surgery and during the first hour after admission to the ICU. Hemodynamic stability was defined as patients with no need for active resuscitation with fluids, pressors, or inotropes to keep urine output > 0.5 ml/kg per min, systolic arterial pressure > 90 mmHg, and heart rate < 120 beats/min.
All patients were treated following the same protocol used in our ICU. No patients needed hemodynamic monitoring with a pulmonary artery catheter.
Measurements and study protocol
The ethics committee of our institution approved the study. The study was conducted at the Central ICU of the Santa Casa de Porto Alegre Hospital. Demographic data were collected by the ICU staff and included age, type of surgery, duration of surgery, hospital mortality, and risk of death for each patient predicted from the Simplified Acute Physiology Score II (SAPS II) [19]. Blood gas values were determined using a commercial blood-gas analyzer (Ciba-Corning, San Diego, CA, USA). Blood lactate concentrations were measured by an enzymatic technique (Cobas Mira Plus; Roche, Indianapolis, IN, USA).
Blood lactate values, the mean arterial pressure, the heart rate and the urine output were obtained at patient's admission to the study, at 12, 24 and 48 hours. Blood arterial gases were obtained daily. SAPS II was recorded at admission. Other values recorded included demographic data, serum chemistries, surgery and ICU or hospital stay duration, and hospital mortality.
Statistical analysis
An unpaired Student t test was used to compare differences between groups at study admission. Changes over time were analyzed using a two-way analysis of variance for repeated measurements. Newman–Keuls' test was used for post-hoc comparisons. We determined the accuracies of the study variables by constructing their receiver operating characteristics curves. Statistical significance was accepted to correspond to P < 0.05. All data are presented as means ± standard deviation.
Results
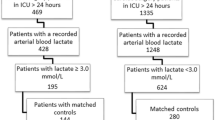
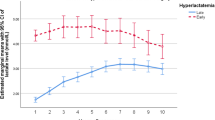
Clinical data for the 44 patients are summarized in Table 1. Twenty-nine survivors were discharged before 48 hours of ICU stay. Five patients died during the ICU stay, four of them dying from septic shock. Another two patients died after discharge from the ICU. Figure 1 shows the changes in arterial lactate and bicarbonate. The survivors' blood lactate levels decreased significantly with time, but levels remained stable in the nonsurvivor group. A significant difference for lactate concentrations was seen after 12 hours. Arterial bicarbonate levels increased significantly in survivors and were higher than in nonsurvivors up to 48 hours. No correlation was found between lactate and bicarbonate or base excess at any time.
The ICU stay and the hospital stay were longer for nonsurvivors. SAPS II was higher for nonsurvivors than for survivors (P = not significant). The PaO2/FiO2 ratio and the urine output tended to be lower, and the heart rate tended to be higher in nonsurvivors during time (Table 2). There were no significant differences in age or serum albumin at admission. The values for mean arterial pressure and arterial blood oxygenation parameters were statistically similar for survivors and nonsurvivors at any time.
Nine patients (seven nonsurvivors) developed complications such as severe sepsis, respiratory failure, abdominal fistula, and surgical wound infection.
Figure 2 represents the receiver operating characteristics curves for initial values of blood lactate and SAPS II. The area under the curve was larger for SAPS II and for blood lactate, both for predicting complications or death, than the other variables (Table 3).
Discussion
The search for the optimal marker of adequate resuscitation continues. Intensivists agreed that traditional markers, such as blood pressure or urine output, are not sufficient indicators of adequate global perfusion. It is important to find a reliable indicator of perfusion since most deaths in the ICU are secondary to multiple organ failure, an end product of persistent hypoperfusion [20].
The optimal marker of adequate resuscitation would possess a number of desirable qualities: accuracy, ease and rapidity of acquisition, reproducibility in a broad variety of clinical hypoperfusion states, consistent results among different providers, and rapidity of change in response to change in clinical condition or to resuscitation. The study is a prospective examination of blood lactate as one of the more widely used markers of hypoperfusion.
Lactate is a byproduct of anaerobic metabolism, elevated in hypoperfusion states when pyruvate cannot enter the Krebs cycle due to insufficient oxygen supply and it is shunted to lactate. In states of global hypoperfusion, lactate production exceeds its rate of metabolism and the blood lactate levels rise. Elevated blood lactate has been correlated strongly with mortality in many types of shock [4, 6–11, 21, 22]. The rapidity at which lactate is cleared from the blood during resuscitation better correlates with outcome, including mortality or organ failure, than a single measurement of lactate [6, 11–14].
Other markers of metabolic acidosis, such as base deficit or bicarbonate, have been used to evaluate resuscitation after trauma or septic shock [4, 13, 23, 24]. In these studies, blood lactate levels were also elevated. Serum lactate and base deficit do not appear to be always linked. Abnormalities in the acid–base environment from the administered base, alterations in the body's buffer base, renal dysfunction, and electrolyte abnormalities have all been postulated as causes of this observed uncoupling. It seems this is the case for base deficit or bicarbonate in several studies studying different populations of critically ill patients in a context of a completed clinically global resuscitation. In contrast, there is consistent evidence that significant hyperlactatemia and dangerous hypoperfusion can exist despite lack of acidosis [6, 8–10, 25]. In addition, the use of lactate as an endpoint of resuscitation is based on a substantial body of literature, including multiple prospective studies in trauma patients, in surgical patients, in septic patients, and in mixed populations of critically ill patients [8, 13, 18, 26].
Our hypothesis states that patients without signs of clinical shock can still be hypoperfused and are at risk for complications. We therefore studied high-risk surgical patients that have had a stable hemodynamic course during surgery and immediately after admission to the ICU. The results of this study indicate that the lactate level is superior to several clinical markers of shock or organ failure, including the heart rate, diuresis and the mean arterial pressure, or indices of metabolic acidosis. Lactate levels at admission (P = not significant) and after 12 hours (P = 0.012) separated survivors and nonsurvivors. In addition, persistent hyperlactetemia showed by the nonsurvivors at 48 hours correlates with a poor clinical outcome in accordance with previous observations. These data probably reflect a continuous and insufficient resuscitation. However, 29 survivors were discharged and one patient died before 48 hours, reducing the possibility to find statistically significant differences after 48 hours.
We found that both lactate and bicarbonate showed a similar course for survivors and for nonsurvivors with time. The receiver operating characteristics curves, however, showed that lactate was significantly superior to any metabolic or hemodynamic variable and was comparable with SAPS II as a predictor of mortality or morbidity at admission to the ICU. Similar to our previous results in septic patients, or other studies in trauma, the lactate level of surgical or burn patients was found to be a significant predictor of mortality, while base deficit or bicarbonate failed to achieve clinical significance [6, 8–10, 25]. Blood lactate levels, particularly when hemodynamic alterations are taken into consideration, seem to have a similar value in identifying survivors when compared with more sophisticated scores like SAPS II or Acute Physiology and Chronic Health Evaluation II. In addition, and at the bedside, lactate values may give better relevant clinical information of what is occurring with the patient over time.
Blood lactate concentrations are easily obtained and measured when compared with other monitoring variables, even before any invasive monitoring is available. Nevertheless, determinations of lactate concentrations have their limitations, especially in septic conditions when metabolic conditions can be complex (increased aerobic production, altered clearance in the liver and other organs, washout of accumulated lactate in the tissues, extracorporeal renal support with hemofiltration) [27–33]. Few patients in our study were septic or had liver dysfunction at admission to the study. None were actively resuscitated during the surgery and immediately after, and, finally, no patient was under extracorporeal renal support. Lung lactate production is significantly elevated in acute lung injury, particularly in septic conditions [34, 35]. The nonsurvivors had a lower (P = not significant) PaO2/FiO2 ratio than the survivors. We did not measure the lactate gradient across the lung to verify whether the nonsurvivors had an increased lactate production by the lungs. However, no correlation was found between lactate levels and the PaO2/FiO2 ratio, and all patients, including the nonsurvivors, had no evidence of diffuse lung inflammatory processes during the first 48 hours. It is thus probable that hyperlactatemia of our patients was mainly due to hypoperfusion.
This prospective study supports blood lactate levels as a marker of occult hypoperfusion. Blood lactate is reliable in predicting lethality in the early phase after high-risk surgery. Nonetheless, further studies are needed to demonstrate whether the identification and correction of hyperlactatemia may be beneficial in reducing morbidity and mortality in the stable surgical patient.
Key messages
-
Survival rates in high-risk surgical patients are associated with an adequate resuscitation
-
Adequate resuscitation cannot be based only on normalization of vital signs
-
Elevated blood lactate levels despite normal vital signs (occult hypoperfusion) are good markers of mortality in surgical patients
-
Resolution of persistent occult hypoperfusion may improve mortality rates in surgical patients
Abbreviations
- ICU:
-
intensive care unit
- NS:
-
not significant
- PaO2/FiO2:
-
partial pressure of arterial oxygen/inspired fraction of oxygen ratio
- SAPS II:
-
Simplified Acute Physiology Score II
References
Cain SM: Appearance of excess lactate in anesthetized dogs during anemic and hypoxic hypoxia.Am J Physiol 1965, 209:604–610.
Nelson DP, Beyer C, Samsel RW, Wood LD, Schumacker PT: Pathological supply dependence of O 2 uptake during bacteremia in dogs.J Appl Physiol 1987, 63:1487–1492.
Zhang H, Rogiers P, Friedman G, Preiser JC, Spapen H, Buurman WA, Vincent JL: Effects of nitric oxide donor SIN-1 on oxygen availability and regional blood flow during endotoxic shock.Arch Surg 1996, 131:767–774.
Bakker J, Coffernils M, Leon M, Gris P, Vincent JL: Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock.Chest 1991, 99:956–962.
Friedman G, De Backer D, Shahla M, Vincent JL: Oxygen supply dependency can characterize septic shock.Intensive Care Med 1998, 24:118–123.
Friedman G, Berlot G, Kahn RJ, Vincent JL: Combined measurements of blood lactate concentrations and gastric intramucosal pH in patients with severe sepsis.Crit Care Med 1995, 23:1184–1193.
Crowl AC, Young JS, Kahler DM, Claridge JA, Chrzanowski DS, Pomphrey M: Occult hypoperfusion is associated with increased morbidity in patients undergoing early femur fracture fixation.J Trauma 2000, 48:260–267.
Claridge JA, Crabtree TD, Pelletier SJ, Butler K, Sawyer RG, Young JS: Persistent occult hypoperfusion is associated with a significant increase in infection rate and mortality in major trauma patients.J Trauma 2000, 48:8–14.
Jeng JC, Jablonski K, Bridgeman A, Jordan MH: Serum lactate, not base deficit, rapidly predicts survival after major burns.Burns 2002, 28:161–166.
Husain FA, Martin MJ, Mullenix PS, Steele SR, Elliott DC: Serum lactate and base deficit as predictors of mortality and morbidity.Am J Surg 2003, 185:485–491.
McNelis J, Marini CP, Jurkiewicz A, Szomstein S, Simms HH, Ritter G, Nathan IM: Prolonged lactate clearance is associated with increased mortality in the surgical intensive care unit.Am J Surg 2001, 182:481–485.
Alves FA, Sant'Anna UL, Oliveira E, Weingartner R, Oliveira E, Friedman G: O valor prognóstico do curso hemodinâmico inicial de pacientes com falência circulatória.Revista Brasileira de Terapia Intensiva 1998, 10:68–75.
Abramson D, Scalea TM, Hitchcock R, Trooskin SZ, Henry SM, Greenspan J: Lactate clearance and survival following injury.J Trauma 1993, 35:584–588.
Bakker J, Gris P, Coffernils M, Kahn RJ, Vincent JL: Serial blood lactate levels can predict the development of multiple organ failure following septic shock.Am J Surg 1996, 171:221–226.
Scalea TM, Maltz S, Yelon J, Trooskin SZ, Duncan AO, Sclafani SJ: Resuscitation of multiple trauma and head injury: role of crystalloid fluids and inotropes.Crit Care Med 1994, 22:1610–1615.
Blow O, Magliore L, Claridge JA, Butler K, Young JS: The golden hour and the silver day: detection and correction of occult hypoperfusion within 24 hours improves outcome from major trauma.J Trauma 1999, 47:964–969.
Polonen P, Ruokonen E, Hippelainen M, Poyhonen M, Takala J: A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients.Anesth Analg 2000, 90:1052–1059.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M: Early goal-directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med 2001, 345:1368–1377.
Le Gall JR, Lemeshow S, Saulnier F: A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study.J Am Med Assoc 1993, 270:2957–2963.
Shoemaker WC, Appel PL, Kram HB: Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients.Chest 1992, 102:208–215.
Weil MH, Afifi AA: Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock).Circulation 1970, 41:989–1001.
Groeneveld AB, Kester AD, Nauta JJ, Thijs LG: Relation of arterial blood lactate to oxygen delivery and hemodynamic variables in human shock states.Circ Shock 1987, 22:35–53.
Davis JW, Parks SN, Kaups KL, Gladen HE, O'Donnell-Nicol S: Admission base deficit predicts transfusion requirements and risk of complications.J Trauma 1996, 41:769–774.
Rutherford EJ, Morris JA Jr, Reed GW, Hall KS: Base deficit stratifies mortality and determines therapy.J Trauma 1992, 33:417–423.
Mikulaschek A, Henry SM, Donovan R, Scalea TM: Serum lactate is not predicted by anion gap or base excess after trauma resuscitation.J Trauma 1996, 40:218–222.
Boyd O, Grounds RM, Bennett ED: A randomized clinical trial of the effect of deliberate perioperative increase of oxygen delivery on mortality in high-risk surgical patients.J Am Med Assoc 1993, 270:2699–2707.
Vary TC, Siegel JH, Nakatani T, Sato T, Aoyama H: Effect of sepsis on activity of pyruvate dehydrogenase complex in skeletal muscle and liver.Am J Physiol 1986, 250:E634-E640.
Preiser JC, Moulart D, Vincent JL: Dichloroacetate administration in the treatment of endotoxin shock.Circ Shock 1990, 30:221–228.
Curtis SE, Cain SM: Regional and systemic oxygen delivery/uptake relations and lactate flux in hyperdynamic, endotoxin-treated dogs.Am Rev Respir Dis 1992, 145:348–354.
Widnell CC, Baldwin SA, Davies A, Martin S, Pasternak CA: Cellular stress induces a redistribution of the glucose transporter.FASEB J 1990, 4:1634–1637.
Hargrove DM, Bagby GJ, Lang CH, Spitzer JJ: Adrenergic blockade does not abolish elevated glucose turnover during bacterial infection.Am J Physiol 1988, 254:E16-E22.
Woll PJ, Record CO: Lactate elimination in man: effects of lactate concentration and hepatic dysfunction.Eur J Clin Invest 1979, 9:397–404.
Leavy JA, Weil MH, Rackow EC: 'Lactate washout' following circulatory arrest.J Am Med Assoc 1988, 260:662–664.
Kellum JA, Kramer DJ, Lee K, Mankad S, Bellomo R, Pinsky MR: Release of lactate by the lung in acute lung injury.Chest 1997, 111:1301–1305.
De Backer D, Creteur J, Zhang H, Norrenberg M, Vincent JL: Lactate production by the lungs in acute lung injury.Am J Respir Crit Care Med 1997, 156:1099–1104.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Meregalli, A., Oliveira, R.P. & Friedman, G. Occult hypoperfusion is associated with increased mortality in hemodynamically stable, high-risk, surgical patients. Crit Care 8, R60 (2004). https://doi.org/10.1186/cc2423
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc2423