Abstract
Objective
An endotracheal tube (ETT) imposes work of breathing on mechanically ventilated patients. Using a bellows-in-a-box model lung, we compared the tube compensation (TC) performances of the Nellcor Puritan-Bennett 840 ventilator and of the Dräger Evita 4 ventilator.
Measurements and results
Each ventilator was connected to the model lung. The respiratory rate of the model lung was set at 10 breaths/min with 1 s inspiratory time. Inspiratory flows were 30 or 60 l/min. A full-length 8 mm bore ETT was inserted between the ventilator circuit and the model lung. The TC was set at 0%, 10%, 50%, and 100% for both ventilators. Pressure was monitored at the airway, the trachea, and the pleura, and the data were recorded on a computer for later analysis of the delay time, of the inspiratory trigger pressure, and of the pressure–time product (PTP). The delay time was calculated as the time between the start of inspiration and minimum airway pressure, and the inspiratory trigger pressure was defined as the most negative pressure level. The same measurements were performed under pressure support ventilation of 4 and 8 cmH2O.
The PTP increased according to the magnitude of inspiratory flow. Even with 100% TC, neither ventilator could completely compensate for the PTP imposed by the ETT. At 0% TC the PTP tended to be less with the Nellcor Puritan-Bennett 840 ventilator, while at 100% TC the PTP tended to be less with the Dräger Evita 4 ventilator. A small amount of pressure support can be equally effective to reduce the inspiratory effort compared with the TC.
Conclusion
Although both ventilators provided effective TC, even when set to 100% TC they could not entirely compensate for a ventilator and ETT-imposed work of breathing. The effect of TC is less than that of pressure support ventilation. Physicians should be aware of this when using TC in weaning trials.
Similar content being viewed by others
Introduction
Mechanically ventilated patients usually show significantly increased respiratory resistance [1–3]. Almost all ventilated patients are intubated and positive pressure ventilation is most commonly applied to assist patient effort. The endotracheal tube (ETT) constitutes a greater resistance than does the supraglotic airway [4]. Once the patient starts making efforts to breathe, resistance imposed by the ETT increases the resistive work of breathing (WOB) during both the inspiration and the expiration. It is prudent for physicians to recognize the importance of imposed WOB due to an ETT during the weaning process. In clinical practice, pressure support ventilation (PSV) is popular to compensate for an ETT. The pressure difference across the ETT changes proportionate to the gas flow. When a patient generates a high flow with a strong inspiratory effort, the pressure difference across the ETT can be considerably great, and PSV cannot compensate for imposed WOB due to the ETT. Sometimes 10 or 15cmH2O PSV is needed to compensate for WOB due to an ETT in a patient with high minute ventilation [5].
To alleviate the WOB due to tube resistance, two manufacturers have recently released ventilators that, by increasing pressure at the proximal end of the tube, are able to compensate for tube resistance [6–8]. This function is known as tube compensation (TC). The object of TC is to give the patients the feeling that they are not intubated from the viewpoint of WOB, and it is sometimes described as 'electric extubation'. If TC works in theory, WOB due to an ETT is compensated regardless of inspiratory efforts. However, new ventilatory modes are sometimes very good in theory but do not work in practice. The purpose of the study was to investigate whether TC worked both in normal and high inspiratory flow, and whether the TC performance of two sophisticated ventilators worked in the same manner.
Methods
Model lung and ventilators
To simulate spontaneous breathing we used a custom-built bellows-in-a-box model lung, details of which have been described elsewhere [8, 9] (Fig. 1). Briefly, a pair of bellows are set in a rigid box: one simulates the muscles and the other simulates the lungs. Negative pressure acts on the muscle compartment by the Venturi effect. The space between the box and the bellows simulates the pleural space. The source gas (O2 at 345 kPa) was connected to a custom-made pressure regulator and a proportional solenoid valve (SMC 315; SMC Co., Tokyo, Japan). The opening of the solenoid valve was controlled by a function generator (H3BF; Omron, Tokyo, Japan). The inspiratory flow, the inspiratory time, and the respiratory rate were controlled by setting the regulator on the model lung. The compliance of the model lung was adjusted to 46.8 ml/cmH2O.
The model lung was set for spontaneous breathing (respiratory rate, 10 breaths/min; inspiratory time, 1.0 s; peak inspiratory flow, 30 or 60 l/min). Two commercially available ventilators that incorporate TC functions, the Nellcor Puritan-Bennett 840 (NPB840) ventilator (Pleasanton, CA, USA) and the Dräger Evita 4 (DE4) ventilator (Lübeck, Germany), were connected to the model lung via a standard ventilator circuit (Dar SpA, Milandola, Italy) with full-length 8 mm bore ETT (Portex, Hythe, UK). Operating the TC function involves specifying the size and type of the tubes and then selecting the degree of TC. Compensation settings vary from 100% to 10% with the NPB 840 ventilator, and from 100% to 1% with the DE4 ventilator. To compare the actual TC performance of the two ventilators, TC was monitored on both machines at settings of 10%, 50%, and 100%. The tube length was the same for both machines and so is not considered significant to the comparative results. We did not shorten the tubes in the present study. PSV was originally developed to overcome the WOB imposed by ETTs, so we also carried out, with the same settings on the model lung, trials with PSV set at 4 and 8 cmH2O on either ventilator. The trigger sensitivity on both ventilators was set at 1 l/min. Settings for the rising time and the expiratory sensitivity were a support sensitivity of 0.2 s and an expiratory sensitivity of 25% for the NPB 840 ventilator, and a flow acceleration of 90% and an expiratory sensitivity of 25% for the DE4 ventilator.
Measurements
The airway pressure at the proximal end of the ETT (Paw), the pressure at the distal end of ETT (Ptr), and the pleural pressure (Ppl) were measured with differential pressure transducers (DP45; Validyne, Northridge, CA, USA). The flow at the airway opening was measured with a pneumotachometer (model 4700, 0-160 l/min: Hans-Rudolph Inc., Kansas City, MO, USA) connected to a differential pressure transducer (DP45; Validyne). The flowmeter was calibrated using a syringe with a plunger that was moved by a linear slider programmed to adjust flow to precisely 1 l/s. Accuracy was confirmed by the integration of flow signal for 1 s. Pressure transducers were calibrated at 10 cmH2O with a water manometer. The tidal volume (VT) was calculated by digital integration of flow data. All signals were led to an analogue–digital converter (DI-220; Dataq Instruments Inc., Akron, OH, USA) via amplifiers (CD19A High Gain Carrier Demodulator; Validyne), and were saved at 100 Hz/channel signal frequency on an IBM-compatible computer using WINDAQ (Dataq Instruments Inc.) data acquisition software. At each experimental setting, three breaths were analysed and average values were used.
Data analysis
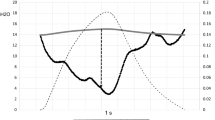
Figure 2 shows the measurements of the pressure–time product (PTP), the inspiratory delay time (DT), and the inspiratory trigger pressure (PI). The PTP is indicated by the area below the baseline pressure between the initiation of inspiration and the time for the pressure to return to the baseline. These calculations were performed for Paw, Ptr, and Ppl. The DT was calculated as the time between the start of inspiration and minimum airway pressure. During the inspiratory trigger, the PI was defined as the most negative pressure level.
Definition of measured parameters. Delay time (DT), the time elapsed from the beginning of inspiration to the bottom of the pressure cycle; inspiratory trigger pressure (PI), the pressure difference between the baseline and the bottom; pressure–time product (PTP), the area on the graph where the pressure is below the baseline.
Statistical analysis
The VT, the DT, the PI, and the PTP were analysed as dependent variables. For each variable, two-way analysis of variance was performed for TC, with PSV support levels and ventilators as the repeated measures. When statistical significance was indicated, it was further examined by post hoc analysis (Scheffé test). A statistics software package (STATISTICA 5.1; StatSofa Inc.,Tulsa, OK, USA) was used and significance was set at P < 0.05.
Results
Figure 3 shows pressure tracings for each ventilator during TC of 0% and 100%. At TC of 0% the NPB840 ventilator increased the Paw above baseline after triggering of the inspiratory effort, while the DE4 ventilator did not increase Paw above baseline during the entire inspiratory phase. The tracheal pressures of both ventilators were below baseline during the whole inspiration. At 100% TC, the tracheal pressure was close to baseline during the latter phase of inspiration with the NPB840 ventilator and at the end of inspiration with the DE4 ventilator.
Representative pressure tracings from 60 l/min inspiratory flow. Airway pressure (Paw), tracheal pressure (Ptr), and pleural pressure (Ppl) tracings at: (a) 0% tube compensation (TC) with the Nellcor Puritan-Bennett 840 ventilator, (b) 100% TC with the Nellcor Puritan-Bennett 840 ventilator, (c) 0% TC with the Dräger Evita 4 ventilator, and (d) 100% TC with the Dräger Evita 4 ventilator.
The PTPs were calculated with Paw, Ptr, and Ppl. A higher inspiratory flow resulted in greater PTPs for both ventilators. With 0%, 10%, and 50% TC there were no significant differences between PTPs. At 100% TC, both the PTPs calculated with Ptr and with Ppl decreased significantly compared with other settings. Figure 4 shows PTPs at each support level of TC for both ventilators. At all settings, 4 and 8 cmH2O PSV increased the VT by more than 10% (Table 1), although the VT did not increase more than 10% above the baseline VT in 10% TC and 50% TC but it did in 100% TC with DE4. The DT, at all experimental settings for both ventilators, did not differ significantly with increasing TC. The inspiratory flow did not significantly influence the DT, and consequently combined data for the DT at 30 and 60 l/min inspiratory flow are presented. Increases in TC, at any experimental settings, did not cause significant changes in the PI. As expected, the PI increased as inspiratory flow increased. Table 2 presents data only for 60 l/min inspiratory flow.
The pressure–time product (PTP) at each ventilator setting: (a) 30 l/min peak inspiratory flow, and (b) 60 l/min inspiratory flow. The numerals 0, 10, 50, and 100 under each graph represent tube compensation support levels of 0%, 10%, 50%, and 100%, respectively. The PTP was calculated from the airway pressure (Paw), the tracheal pressure (Ptr), and the pleural pressure (Ppl).
PTPs were larger with the DE4 ventilator than with the NPB840 ventilator at TC of 0%. At 0% and 10% TC the VT was significantly less with the DE4 ventilator than with the NPB840 ventilator, and at 50% and 100% TC the VT was significantly larger with the DE4 ventilator than with the NPB840 ventilator. On comparing these two ventilators, the DT did not vary significantly.
Discussion
There are two major findings of the present study. First, with both the DE4 and the NPB840 ventilators, PTPs during inspiration decreased as TC support increased. Second, at 0% TC the PTP calculated with Ptr was less with the NPB840 ventilator than that with the DE4 ventilator.
Invasive positive pressure ventilation requires an ETT, the presence of which imposes additional WOB according to bore and inspiratory flow [10, 11]. The burden is heavy enough to induce respiratory muscle fatigue. To compensate for the WOB imposed by the ETT, the most popular ventila-tory strategy is PSV. A PSV of 5-7 cmH2O for adult patients [12] and a PSV of 4-8 cmH2O for children [13] are reported to compensate for the imposed work. Ventilators with selectable TC settings have more recently been developed to compensate the WOB imposed by an ETT. At a setting of 100% TC it would be natural to assume that the ventilator was completely cancelling the extra burden imposed by the resistance of the small-bore tube. Despite being set to 100%, neither of the two ventilators tested was able to completely compensate for PTP calculated with Ppl.
Patients have to trigger the ventilator in patient-triggered ventilation modes. This effort requires significant WOB [14, 15]; the effort may even exceed the total WOB of healthy human beings. The technique of TC is also dependent on patient-triggered ventilation and trigger work is still necessary during TC. This is one of the major reasons why, with the tested ventilators, TC did not completely compensate ETT-imposed PTP calculated with Ppl.
As TC support increased, PTPs decreased. As already described, however, TC did not fully compensate for PTPs imposed by ETT resistance. This result raises doubts about the lower range of overall TC support that is actually provided in clinical situations. In clinical settings, because of secretions deposited inside the ETT or because of deformity of the ETT, or both, ETT resistance tends to increase the longer the intubation continues. In the present study, the ETT was allowed to assume a natural curve and was not subject to any twisting or deformation. Neither was a humidifier used. The ETT was kept dry, so neither condensation in, nor deformity of, the ETT could have impeded the ideal functioning of TC. Furthermore, 4 cmH2O PSV decreased PTPs by the same amount as 100% TC and raises the question whether TC technology yet provides any advantage over other ventilatory modes. PSV is a well known and widely practiced technique to alleviate WOB imposed by an ETT for mechanically ventilated patients [12]. As Fig. 3 shows, Paw was high at the beginning of inspiration and decreased as the inspiratory flow decreased with 100% TC. PSV is designed to keep Paw constant during the inspiratory effort of spontaneous breathing. This is one of the reasons why only a small amount of PSV was as effective as 100% TC. From the viewpoint of decreasing WOB, the clinical importance of TC may be doubtful.
Once triggered by the patient's breath, the ventilators deliver fresh gas according to the programming for the set ventilatory modes. Each manufacturer uses its own algorithms to control delivery of inspiratory gas. The technical strategies applied to deliver gas mean that different brands of ventilator will behave differently in practice. At 100% TC, the DE4 ventilator decreased PTPs more than did the NPB840 ventilator. This suggests that the ventilators use different TC algorithms and that neither of these algorithms is actually able to provide 100% compensation.
This is an in vitro study with a model lung, and our results should not be considered applicable to patients directly. TC is a mode to support inspiration, and we did not evaluate the expiratory WOB. We set the respiratory rate of simulated spontaneous breathing at 10 breaths/min to prevent air-trapping inside the bellows. However, in the clinical setting, the respiratory rate is not necessarily low enough to avoid air-trapping. Two levels of inspiratory efforts (30 and 60 l/min inspiratory flow of the model lung) were investigated, but they were constant during data acquisition. The inspiratory effort of patients differs breath by breath in clinical settings, and the effect was not evaluated in the present study. The respiratory mechanics of patients may also influence the performance of TC, and we did not evaluate this from the data of the present study. Positive end expiratory pressure could also affect TC performance. We therefore repeated the whole study at 5 cmH2O positive end expiratory pressure, and the data did not reveal any differences without positive end expiratory pressure. We presented the data at zero positive end expiratory pressure.
In conclusion, TC did not compensate for the PTPs imposed by ETT resistance. TC is a patient-triggered ventilation technique, and patients have to work to trigger the ventilator. TC cannot compensate for these triggering PTPs. A small amount of PSV was as effective as 100% TC. This inability restricts the usefulness of this new ventilator function. Before we can be confident of the clinical advantages of TC, more hands-on experience is needed.
Key message
-
The tube compensation function incorporated in two modern ventilators was investigated. The function did not compensate completely for that imposed by an endotracheal tube
Abbreviations
- DE4:
-
= Dräger Evita 4
- DT:
-
= delay time
- ETT:
-
= endotracheal tube
- NPB 840:
-
= Nellcor Puritan-Bennett 840
- aw:
-
Paw = airway pressure
- PI:
-
= inspiratory trigger pressure
- pl:
-
Ppl= pleural pressure
- PSV:
-
= pressure support ventilation
- PTP:
-
= pressure–time product
- tr:
-
Ptr = tracheal pressure
- TC:
-
= tube compensation
- T:
-
VT= tidal volume
- WOB:
-
= work of breathing.
References
Pelosi P, Cereda M, Foti G, Giacomini M, Pesenti A: Alterations of lung and chest wall mechanics in patients with acute lung injury: effects of positive end-expiratory pressure. Am J Respir Crit Care Med 1995, 152: 531-537.
Pesenti A, Pelosi P, Rossi N, Virtuani A, Brazzi L, Rossi A: The effects of positive end-expiratory pressure on respiratory resistance in patients with the adult respiratory distress syndrome and in normal anesthetized subjects. Am Rev Respir Dis 1991, 144: 101-107.
Mols G, Kessler V, Benzing A, Lichtwarck-Aschoff M, Geiger K, Guttmann J: Is pulmonary resistance constant, within the range of tidal volume ventilation, in patients with ARDS? Br J Anaesth 2001, 86: 176-182. 10.1093/bja/86.2.176
Straus C, Louis B, Isabey D, Lemaire F, Harf A, Brochard L: Comparison of the endotracheal tube and the upper airway to breathing workload. Am J Respir Crit Care Med 1998, 157: 23-30.
Fabry B, Haberthür C, Zappe D, Guttmann J, Kuhlen R, Stocker R: Breathing pattern and additional work of breathing in spontaneously breathing patients with different ventilatory demand during inspiratory pressure support and automatic tube compensation. Intensive Care Med 1997, 23: 545-552. 10.1007/s001340050371
Haberthür C, Elsasser S, Eberhard L, Stocker R, Guttmann J: Total versus tube-related additional work of breathing in ventilator-dependent patients. Acta Anaesthesiol Scand 2000, 44: 749-757. 10.1034/j.1399-6576.2000.440615.x
Guttmann J, Bernhard H, Mols G, Benzing A, Hofmann P, Haberthür C, Zappe D, Fabry B, Geiger K: Respiratory comfort of automatic tube compensation and inspiratory pressure support in conscious human. Intensive Care Med 1997, 23: 1119-1124. 10.1007/s001340050467
Fujino Y, Uchiyama A, Mashimo T, Nishimura M: Spontaneously breathing lung model comparison of work of breathing between automatic tube compensation and pressure support. Respir Care 2003, 48: 38-45.
Miyoshi E, Fujino Y, Mashimo T, Nishimura M: Performance of transport ventilator with patient-triggered ventilation. Chest 2000, 118: 1109-1115. 10.1378/chest.118.4.1109
Bolder PM, Healy TEJ, Bolder AR, Beatty PCW, Kay B: The extra work of breathing through adult endotracheal tubes. Anesth Analg 1986, 65: 853-859.
Shapiro M, Wilson K, Casar G, Bloom K, Teague RB: Work of breathing through different sized endotracheal tubes. Crit Care Med 1986, 14: 1028-1031.
Brochard L, Rua F, Lorino H, Lemaire F, Harf A: Inspiratory pressure support compensates for the additional work of breathing caused by the endotracheal tube. Anesthesiology 1991, 75: 739-745.
Takeuchi M, Imanaka H, Miyano H, Kumon K, Nishimura M: Effect of patient-triggered ventilation on respiratory workload in infants after cardiac surgery. Anesthesiology 2000, 93: 1238-1244. 10.1097/00000542-200011000-00017
Sassoon CS, Lodia R, Rheeman CH, Kuei JH, Light RW, Mahutte CK: Inspiratory muscle work of breathing during flow-by, demand-flow, and continuous-flow systems in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 1992, 145: 1219-1222.
Sassoon CS, Del Rosario N, Fei R, Rheeman CH, Gruer SE, Mahutte CK: Influence of pressure- and flow-triggered synchronous intermittent mandatory ventilation on inspiratory muscle work. Crit Care Med 1994, 22: 1933-1941.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Maeda, Y., Fujino, Y., Uchiyama, A. et al. Does the tube-compensation function of two modern mechanical ventilators provide effective work of breathing relief?. Crit Care 7, R92 (2003). https://doi.org/10.1186/cc2343
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc2343