Abstract
Introduction
Use of the Bair Hugger forced-air patient warming system during prolonged abdominal vascular surgery may lead to increased bacterial contamination of the surgical field by mobilization of the patient's skin flora.
Methods
This possibility was studied by analyzing bacterial content in air and wound specimens collected during surgery in 16 patients undergoing abdominal vascular prosthetic graft insertion procedure, using the Bair Hugger patient warming system. The bacterial colony counts from the beginning and the end of surgery were compared, and the data analyzed using the Wilcoxon matched pairs test.
Results
The results showed not only that there was no increase in bacterial counts at the study sites, but also that there was a decrease (P < 0.01) in air bacterial content around the patient and in the operating theatre after prolonged use of the patient warmer. No wound or graft infections occurred.
Conclusion
The use of this warming system does not lead to increased bacterial contamination of the operating theatre atmosphere, and it is unlikely to affect the surgical field adversely.
Similar content being viewed by others
Introduction
Forced-air patient warming systems, such as Bair Hugger (Augustine Medical Inc., Eden Prairie, MN, USA), were developed in the 1980s and are acknowledged as being the most clinically effective patient warming modality [1, 2]. The advantages of avoiding hypothermia for patients undergoing major surgical procedures are well established, and include decreased blood loss (with consequent reduction in blood product use) [3], wound infection [4], duration of intensive care and hospital stay [5, 6] and cardiac ischaemia [7, 8], and increased survival [6, 9, 10]. However, a potential disadvantage is the risk for bacterial contamination of the operating theatre environment. Prolonged exposure of the patient to the exhaust of the warming blanket could potentially mobilize their resident skin organisms into the theatre atmosphere, and thence into the surgical field, possibly increasing the risk for prosthetic material infection. This has not previously been investigated.
We studied whether use of the Bair Hugger patient warming system increased bacterial contamination of the operating theatre and the surgical wound during prolonged surgery.
Methods
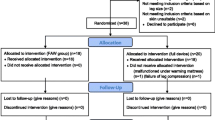
Sixteen consecutive patients undergoing aortic surgery with prosthetic graft insertion were prospectively studied. All vascular surgery was performed in a standard positive pressure theatre. The Bair Hugger upper body blanket (model 522) was used for all patients. Bacteria sampling sites are shown in Fig. 1. Air samples were taken using standard techniques from the theatre atmosphere (sites A1–A3) and around the axillae (sites B1 and B2), where the exhaust air emerged, using the Biotest RCS centrifugal air sampler and Biotest Hycon TC agar strips (Biotest UK Ltd, Solihull, West Midlands, UK). A total of 160 l of air was sampled in 4 min from each of these sites. Sterile swabs were used to take specimens from the warming unit and hose (site C) and immediately plated onto standard blood agar culture media. Further specimens were taken from the wound edges with touch plates of blood agar (site D). Two readings were taken from each site, one when the warming blanket was first applied at the start of the operation and again at the end of the operation. All the culture media were then incubated at 36°C for 24 hours. The number of bacterial colonies visible to the naked eye on each of the agar strips and culture plates were then counted by hand and recorded.
The duration of the operation was recorded. There were nine staff circulating in the operating theatre: three surgeons, two anaesthetists, one operating department assistant and three nurses. All patients had three doses of intravenous antibiotics perioperatively. The data were analyzed using the Wilcoxon matched pairs test [11].
Results
Twelve male and four female patients were included in the present study. Their mean age was 72.5 years (range 60–86 years). The mean duration of use of the warming blanket was 234 min (range 180–270 min). From each site, the number of bacterial colonies at the start of surgery was compared with that at the end of the operation.
Results are shown in Tables 1 and 2. All operating theatre air specimens (sites A1–A3) exhibited a decrease in colony counts at the end of surgery (mean reduction 36.4%). The exhaust air (sites B1 and B2) colony counts also decreased at the end of surgery, although the size of the reduction was much less (mean reduction 9.5%). In the Wilcoxon matched pairs test, the test statistic T equalled 0, because the rank difference was negative for all specimens from sites A1–A3, and B1 and B2. This indicates that there was a significant decrease in the colony counts at the end of surgery as compared with the beginning (P < 0.01). All filter (site C) and wound specimens (site D) were sterile.
None of the patients developed postoperative wound or prosthetic infections during a 6-month follow-up period.
In the present study bacteria were not typed; only the absolute numbers of colonies cultured were counted. Typing was to be done only if there was an increase in colony counts at the end of surgery, and this did not occur in any of the patients studied.
Discussion
As indicated above, the benefits of maintaining normothermia in surgical patients is well documented. It has been shown that the warming equipment itself does not cause bacterial dispersal [12] but the role of patient flora was not investigated and the study was not conducted in a true surgical setting. This remained a concern in our unit, especially because some bacteria in wound infections originated from the patients' skin [13]. The present study did not show any increase in the mobilization and dispersal of patient resident skin organisms. The exhaust air from beneath the surgical drapes, which had passed over the patient's skin, showed a decrease in the number of bacterial counts at the end of surgery, and this demonstrated that there was no increase in air contamination associated with the Bair Hugger patient warming system. Furthermore, it indicated that the warm air stream did not force circulation of the patients' skin organisms. If the Bair Hugger were affecting the atmosphere adversely, then the room air counts would also be expected to increase rather than decrease. In fact, the colony numbers in room air and system exhaust were reduced and this was consistent.
Although the study was not designed to evaluate other causes of bacterial presence in the operating theatre, we feel that the higher count at the beginning of surgery in room air may be due to the unrestricted movement of personnel in and out of the operating room, with opening and closing of doors, leading to increased air flow and turbulence. Toward the end of surgery, movement of staff is much less and this may explain the fall in bacterial counts seen as the air turbulence decreases [14, 15].
Conclusion
We conclude that the use of the Bair Hugger patient warming system during prolonged abdominal surgery does not lead to increased bacterial contamination of the operating theatre atmosphere, and it is therefore unlikely to cause contamination of the surgical field.
Key messages
-
Forced-air warming does not force patient's resident skin organisms into and contaminate the operating theatre atmosphere
-
Such systems are unlikely to increase the incidence of wound and prosthetic infections
References
Sessler DI: Consequences and treatment of perioperative hypothermia. Anesth Clin North Am 1994, 12: 425-456.
Mahoney CB, Odom J: Maintaining intraoperative normothermia: a meta-analysis of outcomes with costs. AANA J 1999, 67: 155-164.
Schmied H, Kurz A, Sessler DI, Kozek S, Reiter A: Mild intraoperative hypothermia increases blood loss and allogenic transfusion requirements during total hip arthroplasty. Lancet 1996, 347: 289-292. 10.1016/S0140-6736(96)90466-3
Leaper DJ, Melling AG: Antibiotic prophylaxis in clean surgery: clean non-implant wounds. J Chemother 2001,13(spec no 1):96-101.
Kurz A, Sessler DI, Lenhardt R: Perioperative normothermia to reduce the incidence of surgical wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med 1996, 334: 1209-1215. 10.1056/NEJM199605093341901
Tryba M, Leban J: Does active warming of severely injured trauma patients influence perioperative morbidity? Anesthesiology 1996,85(suppl 3A):A283.
Frank SM, Fleisher LA, Breslow MJ, Higgins MS, Olson KF, Kelly S, Beattie C: Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. JAMA 1997, 277: 1127-1134. 10.1001/jama.277.14.1127
Frank SM, Christopherson R: Unintentional hypothermia is associated with postoperative myocardial ischaemia. Anesthesiology 1993, 78: 468-476.
Uebelen R, Schultze K: Unintended decreasing body temperature: a stepchild of perioperative care and outcome consequence. Br J Anaesth 1998,80(suppl 1):A26.
Bush H Jr, Hydo LJ, Fisher D: Hypothermia during elective abdominal aortic aneurysm repair: the high price of avoidable morbidity. J Vasc Surg 1995, 21: 392-402.
Bland M: Introduction to Medical Statistics 3 Edition Oxford: Oxford University Press 2000.
Avidan MS, Jones N, Ing R, Khoosal M, Lundgren C, Morrell DF: Convection warmers- not just hot air. Anaesthesia 1997, 52: 1073-1076.
Bitkover CY, Marcusson E, Ransjo U: Spread of coagulase-negative staphylococci during cardiac operations in a modern operating room. Ann Thorac Surg 2000, 69: 1110-1115. 10.1016/S0003-4975(99)01432-0
Gosden PE, MacGowan AP, Bannister GC: Importance of air quality and related factors in the prevention of infection in orthopaedic implant surgery. J Hosp Infect 1998, 39: 173-180.
Pittet D, Ducel G: Infectious risk factors related to operating rooms. Infect Control Hosp Epidemiol 1994, 15: 456-462.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Huang, J.K., Shah, E.F., Vinodkumar, N. et al. The Bair Hugger patient warming system in prolonged vascular surgery: an infection risk?. Crit Care 7, R13 (2003). https://doi.org/10.1186/cc1888
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc1888