Abstract
Introduction
Dehydroepiandrosterone (DHEA) and its sulphate (DHEAS) are pleiotropic adrenal hormones with immunostimulating and antiglucocorticoid effects. The present study was conducted to evaluate the time course of DHEAS levels in critically ill patients and to study their association with the hypothalamic–pituitary–adrenal axis.
Materials and method
This was a prospective observational clinical and laboratory study, including 30 patients with septic shock, eight patients with multiple trauma, and 40 age- and sex-matched control patients. We took serial measurements of blood concentrations of DHEAS, cortisol, tumour necrosis factor-α and IL-6, and of adrenocorticotrophic hormone immunoreactivity over 14 days or until discharge/death.
Results
On admission, DHEAS was extremely low in septic shock (1.2 ± 0.8 mol/l) in comparison with multiple trauma patients (2.4 ± 0.5 μmol/l; P < 0.05) and control patients (4.2 ± 1.8; P < 0.01). DHEAS had a significant (P < 0.01) negative correlation with age, IL-6 and Acute Physiology and Chronic Health Evaluation II scores in both patient groups. Only during the acute phase did DHEAS negatively correlate with dopamine. Nonsurvivors of septic shock (n = 11) had lower DHEAS levels (0.4 ± 0.3 μmol/l) than did survivors (1.7 ± 1.1 μmol/l; P < 0.01). The time course of DHEAS exhibited a persistent depletion during follow up, whereas cortisol levels were increased at all time points.
Conclusion
We identified extremely low DHEAS levels in septic shock and, to a lesser degree, in multiple trauma patients as compared with those of age- and sex-matched control patients. There appeared to be a dissociation between DHEAS (decreased) and cortisol (increased) levels, which changed only slightly over time. Nonsurvivors of sepsis and patients with relative adrenal insufficiency had the lowest DHEAS values, suggesting that DHEAS might be a prognostic marker and a sign of exhausted adrenal reserve in critical illness.
Similar content being viewed by others
Introduction
Dehydroepiandrosterone (DHEA) and its sulphate (DHEAS) are the most abundant steroids secreted by the adrenal cortex [1]. The concentration of DHEA in the blood oscillates in parallel with cortisol, in response to levels of adrenocorticotrophic hormone (ACTH), but without feedback control at the hypothalamic–pituitary level.
The physiological role and biological actions of DHEA(S) are not well known but studies in humans suggest a positive impact on sense of well-being [2], and DHEA has recently been recognized as a potent modulator of the immune response [1]. DHEA improved host defences by restoring immune cell function and reversed susceptibility to infection [3].
Serum DHEA(S) concentration was low in patients with primary adrenal insufficiency, and short-term oral DHEA replacement improved the clinical condition of these patients [2,4]. Functional or relative adrenal insufficiency frequently occurs in critically ill patients, with possible fatal consequences, although diagnostic criteria for this entity still pose problems [5]. We hypothesize that the serum DHEAS level has utility as a diagnostic tool and a prognostic marker in such patients. Furthermore, low serum concentrations of DHEAS might be a more sensitive marker of hypothalamic–pituitary–adrenal (HPA) hypofunction than is glucocorticoid secretion.
The present study was conducted to evaluate the time course of DHEAS levels (an immunostimulator) as compared with those of cortisol (an immunosuppressor), ACTH (an inducer of DHEAS) and cytokines (stimulators of the HPA axis) in patients with critical illness and in age- and sex-matched control patients.
Materials and method
Study design
This was a prospective, observational, clinical and laboratory study conducted in a 20-bed medical/surgical/neurosurgical intensive care unit.
Patients
Approval for the study was obtained from our institutional Human Subjects Research Committee, and written informed consent from first-degree relatives was mandatory. Thirty-eight consecutive patients who were admitted to the intensive care unit with septic shock (n = 30) or severe multiple trauma (Injury Severity Score >20; n = 8) were included in the study within 6 hours after admission. Exclusion criteria were as follows: age under 18 years; use of corticosteroids, DHEA or other drugs that affect the HPA axis; pre-existing adrenal insufficiency or known abnormalities of the HPA axis; and presence of diabetes mellitus or congestive heart failure. Age- and sex-matched control patients (n = 40) were patients without acute medical illness who were admitted to the medical department for routine diagnosis and treatment.
Data collection
In patients with septic shock or multiple trauma, Acute Physiology and Chronic Health Evaluation (APACHE) II and Sequential Organ Failure Assessment scores, and intensive care unit mortality were used to assess the severity of disease. In addition, use of dopamine (cumulative dose in milligrams per day) was recorded.
We obtained serial blood samples for measurement of serum cortisol and DHEAS, and plasma ACTH, IL-6 and tumour necrosis factor (TNF)-α once a day between 0700 and 0800 h. Follow up was conducted for 14 days, or until death or discharge from the intensive care unit. Blood samples were stored at -70°C until use.
Immunoreactive DHEAS, cortisol, ACTH, TNF-α and IL-6 concentrations were measured using commercially available chemiluminescent enzyme immunoassays with the Immulite Automated Immunoassay System (Diagnostic Products Corp, Los Angeles, CA, USA).
In patients with clinical suspicion of (relative) adrenal insufficiency (unexplained hypotension and resistance to inappropriately high doses of vasoactive drugs) a low-dose ACTH (1 μg) stimulation test was performed. A normal cortisol response was defined as greater than 550 nmol/l after stimulation and an increase of 150 nmol/l or more [6].
Statistical analysis
Values are expressed as means ± SD. Qualitative data were analysed using the χ2 test. Groups were compared using the Kruskal-Wallis test, with Dunn's test for multiple comparisons. The Spearman rank order correlation coefficient (rs) was used to evaluate relations for individual data. P < 0.05 was considered statistically significant. All analyses were performed using a statistical software package (SPSS 9.0.1; SPSS Inc, Chicago, IL, USA).
Results
The clinical and laboratory characteristics of the patients and control groups on admission are summarized in Table 1. On admission, patients with septic shock had significantly lower DHEAS levels (1.2 ± 0.8 mol/l) than did those with multiple trauma (2.4 ± 0.5 mol/l, P < 0.05) and control patients (4.2 ± 1.8 μmol/l, P < 0.01). There was a significant negative correlation between DHEAS and age (rs = -0.55, P < 0.01) in the patient groups (pooled), but there was no significant difference in DHEAS concentrations between male and female patients. We found a negative correlation between DHEAS and dopamine only during the acute phase (septic shock: rs = -0.60; trauma: rs = -0.55; P < 0.01). Also, the correlation between DHEAS and IL-6 (septic shock: rs = -0.61, P < 0.01; trauma: rs = 0.47, P < 0.05) was more pronounced during the acute phase. These correlations were lost during prolonged illness (after 5 days).
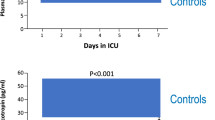
The time course of DHEAS during the observation period of 14 days is shown in Fig. 1. In both septic and trauma patients, DHEAS concentrations were consistently lower than those in control patients over time. In contrast, cortisol levels were persistently elevated at all time points, in both septic and trauma patients. On admission, nonsurvivors of septic shock (n = 11) had lower DHEAS levels (0.4 ± 0.3 mol/l) than did survivors (1.7 ± 1.1 mol/l, P < 0.01). In addition, DHEAS was inversely correlated with APACHE II (rs = -0.52, P < 0.01) and Sequential Organ Failure Assessment (rs = -0.45, P < 0.05) scores.
In eight septic patients there was clinical suspicion of (relative) adrenal insufficiency, which was confirmed by a blunted response to low-dose ACTH in four cases. The patients with adrenal insufficiency had lower DHEAS levels at the time of testing (0.35 ± 0.3 mol/l) than did those with 'normal' adrenal function (1.3 ± 0.8 mol/l, P < 0.05).
Discussion
We found a clear dissociation between high blood levels of cortisol and extremely low levels of DHEAS in critically ill patients in both the acute and prolonged phases. Parker and coworkers [7] demonstrated such a divergence in adrenal steroid secretion; in that study serum cortisol was increased in adult men with burn injuries, whereas serum DHEAS was reduced. Luppa and coworkers [8] studied serum androgens in a large group of critically ill patients and also found markedly decreased DHEAS levels in both males and females, mainly in those patients with a prolonged clinical course. These data indicate a shift in adrenal steroid synthesis away from mineralocorticoids and androgens and toward excessive cortisol production. The dissociation between blood levels of cortisol and DHEAS appears to be a contradiction because both hormones are synthesized and secreted mainly by the adrenal cortex. However, DHEAS is produced mainly in the zona reticularis of the adrenal cortex, possibly indicating that a differential alteration in the cortical zone is responsible for DHEAS deficiency during severe critical illness.
The sustained hypercortisolism, as opposed to the marked DHEAS depletion, during severe critical illness could theoretically result in an imbalance between immunosuppressive and immunostimulatory pathways, and may therefore play a role in susceptibility to infectious complications [1].
Interestingly, we found the lowest DHEAS and the highest cortisol levels in nonsurvivors and the most severely ill patients, indicating that the DHEAS : cortisol ratio might be a prognostic indicator for outcome of critical illness, in particular septic shock. Interpretation of cortisol levels measured in seriously ill patients is difficult. Serum cortisol levels that are regarded as high in control individuals may be inappropriately low in patients who are severely ill. We recently showed that functional or relative adrenal insufficiency can be present in critically ill patients despite 'high' initial serum cortisol levels [5]. By using the low-dose ACTH stimulation test and Thorn test, we demonstrated the relative lack of adrenocortical response to extra stimulation by ACTH in some critically ill patients, because their HPA axis is already maximally stimulated. In the present study the low-dose ACTH test identified four patients out of eight with a clinical suspicion for relative adrenal insufficiency. These patients had very low serum concentrations of DHEAS, which may also be a sign of limited adrenocortical reserve arising during the course of critical illness [6].
In both septic and trauma patients we found a similar degree of stimulation of the HPA axis; however, patients with septic shock were more severely ill than were patients with multiple trauma, as reflected by their APACHE II scores, and TNF-α and IL-6 levels. One could argue that this also indicates a state of exhausted adrenal reserve.
We found a relation between dopamine use and DHEAS levels, but only during the acute phase. Therefore, acute depletion of DHEAS might reflect the liberal use of dopamine [9]. In addition, we found a negative correlation between IL-6 and DHEAS during the acute phase. In healthy persons, serum IL-6 correlated inversely with DHEAS, and DHEA administration led to inhibition of IL-6 secretion from monocytes, indicating a functional link between DHEAS and IL-6 [10]. IL-6 can act synergistically with ACTH on the adrenal glands to release cortisol [11]. Therefore, IL-6 may be an important regulator of DHEAS in (acute) critical illness. However, the dopamine dosage and IL-6 levels decreased significantly over time whereas DHEAS concentrations remained low, suggesting different mechanisms for the prolonged DHEAS depletion during critical illness.
We found a negative correlation between age and DHEAS concentrations. DHEAS concentrations exhibit a biphasic time course following the onset of adrenarche, reaching a peak between the ages 20 and 30 years, and with the greatest decline occurring by age 50–60 years [12,13]. This dramatic age-related reduction might be caused by a specific defect in the desmolase activity in the reticular zone of the adrenal gland. Most of patients studied here, including control patients, were aged approximately 50–60 years.
In conclusion, we found extremely low DHEAS levels in virtually all critically ill patients, in both septic shock and multiple trauma. DHEAS depletion was associated with a worse outcome and represents a prognostic marker. Acute depletion of DHEAS is probably related to the use of dopamine and high IL-6 levels. The prolonged depletion of DHEAS might reflect an exhausted adrenal adaptation. Whether DHEA should be administered in DHEAS-deficient states remains to be elucidated. However, theoretically, beneficial effects on immunity, susceptibility for infections and well-being may be expected.
Key messages
Critically ill patients exhibit a remarkable depletion in DHEAS in both acute and chronic phases, suggesting an exhausted adrenal adaptation
There is a clear dissociation between DHEAS (decreased) and cortisol (increased) levels in critically ill patients, indicating a disturbed balance between immunostimulatory and immunosuppressive factors
DHEAS appears to be a prognostic marker, because nonsurvivors of septic shock have extremely low DHEAS levels
The acute depletion of DHEAS is probably related to the use of dopamine and the high IL-6 levels during the acute phase of critical illness
The prolonged depletion of DHEAS during critical illness is unexplained, but supports the hypothesis of an exhausted neuroendocrine system, and necessitates an interventional study with substitution doses of DHEA, considering the expected beneficial effects on immunity and well-being
Abbreviations
- ACTH:
-
ACTH = adrenocorticotrophic hormone
- APACHE:
-
APACHE = Acute Physiology and Chronic Health Evaluation
- DHEA(S):
-
DHEA(S) = dehydroepiandrosterone (sulphate)
- HPA:
-
HPA = hypothalamic–pituitary–adrenal
- IL:
-
IL = interleukin
- TNF:
-
TNF = tumour necrosis factor.
References
Ebeling P, Koivisto VA: Physiological importance of dehydroepiandrosterone. Lancet 1994, 343: 1479-1481. 10.1016/S0140-6736(94)92587-9
Arlt W, Callies F, van Vlijmen JC, Koehler I, Reincke M, Bidling-maier M, Huebler D, Oettel M, Ernst M, Schulte HM, Allolio B: Dehydroepiandrosterone replacement in women with adrenal insufficiency. N Engl J Med 1999, 341: 1013-1020. 10.1056/NEJM199909303411401
Oberbeck R, Dahlweid M, Koch R, van Griensven M, Emmendörfer A, Tscherne H, Pape HC: Dehydroepiandrosterone decreases mortality and improves cellular immune function during polymicrobial sepsis. Crit Care Med 2001, 29: 380-384. 10.1097/00003246-200102000-00029
Achermann JC, Silverman BL: Dehydroepiandrosterone replacement for patients with adrenal insufficiency. Lancet 2001, 357: 1381-1382. 10.1016/S0140-6736(00)04617-1
Beishuizen A, Vermes I, Hylkema BS, Haanen C: Relative eosinophilia and functional adrenal insufficiency in critically ill patients. Lancet 1999, 353: 1675-1676. 10.1016/S0140-6736(99)01346-X
Beishuizen A, Thijs LG: Relative adrenal failure in intensive care: an identifiable problem requiring treatment? Best Pract Res Clin Endocrinol Metab 2001, 15: 513-531. 10.1053/beem.2001.0167
Parker LN, Levin ER, Lifrak ET: Evidence for adrenocortical adaptation to severe illness. J Clin Endocrinol Metab 1985, 60: 947-952.
Luppa P, Munker R, Nagel D, Weber M, Engelhardt D: Serum androgens in intensive-care patients: correlations with clinical findings. Clin Endocrinol (Oxf) 1991, 34: 305-310.
Van den Berghe G, de Zegher F, Wouters P, Schetz M, Verwaest C, Ferdinande P, Lauwers P: Dehydroepiandrosterone sulphate in critical illness: effect of dopamine. Clin Endocrinol (Oxf) 1995, 43: 457-463.
Straub RH, Konecna L, Hrach S, Rothe G, Kreutz M, Scholmerich J, Falk W, Lang B: Serum dehydroepiandrosterone (DHEA) and DHEA sulfate are negatively correlated with serum interleukin-6 (IL-6), and DHEA inhibits IL-6 secretion from mononuclear cells in man in vitro: possible link between endocrinosenescence and immunosenescence. J Clin Endocrinol Metab 1998, 83: 2012-2017.
Mastorakos G, Chrousos GP, Weber JS: Recombinant interleukin-6 activates the hypothalamic–pituitary–adrenal axis in humans. J Clin Endocrinol Metab 1993, 77: 1690-1694.
Kroboth PD, Salek FS, Pittenger AL, Fabian TJ, Frye RF: DHEA and DHEA-S: a review. J Clin Pharmacol 1999, 39: 327-348. 10.1177/00912709922007903
Baulieu E-E: Dehydroepiandrosterone (DHEA): a fountain of youth? J Clin Endocrinol Metabol 1996, 81: 3147-3151.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Rights and permissions
About this article
Cite this article
Beishuizen, A., Thijs, L.G. & Vermes, I. Decreased levels of dehydroepiandrosterone sulphate in severe critical illness: a sign of exhausted adrenal reserve?. Crit Care 6, 434 (2002). https://doi.org/10.1186/cc1530
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc1530