Abstract
Introduction
The objective of this systematic review and meta-analysis was to determine the effect of renal replacement therapy (RRT), delivered as hemofiltration vs. hemodialysis, on clinical outcomes in patients with acute kidney injury (AKI).
Methods
MEDLINE, EMBASE and CENTRAL databases and conference abstracts were searched to June 2012 for parallel-group or crossover randomized and quasi-randomized controlled trials (RCTs) evaluating hemofiltration vs. hemodialysis in patients with AKI. Two authors independently selected studies and abstracted data on study quality and outcomes. Additional information was obtained from trial authors. We pooled data using random-effects models.
Results
Of 6,657 citations, 19 RCTs (10 parallel-group and 9 crossover) met inclusion criteria. Sixteen trials used continuous RRT. Study quality was variable. The primary analysis included three parallel-group trials comparing similar doses of hemofiltration and hemodialysis; sensitivity analyses included trials comparing combined hemofiltration-hemodialysis or dissimilar doses. We found no effect of hemofiltration on mortality (risk ratio (RR) 0.96, 95% confidence interval (CI) 0.73 to 1.25, P = 0.76; three trials, n = 121 (primary analysis); RR 1.10, 95% CI 0.88 to 1.38, P = 0.38; eight trials, n = 540 (sensitivity analysis)) or other clinical outcomes (RRT dependence in survivors, vasopressor use, organ dysfunction) compared to hemodialysis. Hemofiltration appeared to shorten time to filter failure (mean difference (MD) -7 hours, 95% CI (-19,+5), P = 0.24; two trials, n = 50 (primary analysis); MD -5 hours, 95% CI (-10, -1), P = 0.01; three trials, n = 113 (including combined hemofiltration-hemodialysis trials comparing similar doses); MD -6 hours, 95% CI (-10, -1), P = 0.02; five trials, n = 383 (sensitivity analysis)). Data primarily from crossover RCTs suggested that hemofiltration increased clearance of medium to larger molecules, including inflammatory cytokines, compared to hemodialysis, although almost no studies measured changes in serum concentrations. Meta-analyses were based on very limited data.
Conclusions
Data from small RCTs do not suggest beneficial clinical outcomes from hemofiltration, but confidence intervals were wide. Hemofiltration may increase clearance of medium to larger molecules. Larger trials are required to evaluate effects on clinical outcomes.
Similar content being viewed by others
Introduction
Severe acute kidney injury (AKI) occurs in approximately 6% of patients admitted to an intensive care unit (ICU) [1] and in up to 19% of patients with vasopressor-dependent septic shock [2]. For such individuals, mortality is approximately 60% [1], and survivors are at increased risk of requiring permanent renal replacement therapy (RRT) [3]. Two multicenter randomized controlled trials (RCTs) [4, 5] and two meta-analyses [6, 7] have demonstrated that increasing the dose of RRT above 20 to 25 mL/kg/h of effluent flow for continuous renal replacement therapy (CRRT) or increasing intermittent dialysis frequency beyond alternate days does not improve survival.
In addition to dose, the mode of clearance is also a modifiable component of the RRT prescription that may affect patient outcomes. Convective clearance and diffusive clearance, delivered by hemofiltration and hemodialysis, respectively, can be provided by all continuous and some intermittent RRT machines. Despite similar clearance of small molecules, hemofiltration is reported to achieve higher clearance of medium-sized to larger molecules compared to hemodialysis [8]. Consequently, it is postulated that hemofiltration might benefit critically ill patients with AKI by better clearing large toxic inflammatory cytokines [9]. In the absence of a large, suitably-powered, randomized trial demonstrating the superiority of one mode over the other, practice surveys have shown variability in mode selection among countries and regions [10–15]. Therefore, our objective was to conduct a systematic review and meta-analysis of all RCTs comparing the effects of convective clearance (using hemofiltration) to diffusive clearance (using hemodialysis) in patients with AKI on clinically important outcomes.
Materials and methods
Literature search
We searched OVID versions of MEDLINE, EMBASE Classic and EMBASE and the Cochrane Central Register of Controlled Trials (from inception to June 2012) without language restrictions using a previously described search strategy [6]. We also searched abstracts from critical care and nephrology professional society conferences, including: Society of Critical Care Medicine (2004 to 2012), European Society of Intensive Care Medicine (2001 to 2011), International Symposium of Intensive Care and Emergency Medicine (2004 to 2012), American Thoracic Society (2004 to 2012), American College of Chest Physicians (2003 to 2011), American Society of Nephrology (2003 to 2011), and the European Renal Association - European Dialysis and Transplant Association (2002 to 2012). We also searched bibliographies of included studies and personal files. Two reviewers independently reviewed all citations and retrieved the full text of any citation considered potentially relevant by either reviewer. We attempted to contact selected authors of included studies for clarification of methods and to obtain additional data, where required.
Study selection
Two unblinded reviewers assessed full-text reports and included studies meeting the following criteria: (1) design: either parallel-group (patients assigned to only one treatment) or cross-over (each patient received both treatments in random order) randomized or quasi-randomized (for example, assigning patients in alternating fashion or by hospital registry number) controlled trial, (2) population: adult or post-neonatal pediatric patients with AKI requiring RRT, (3) intervention: hemofiltration compared to hemodialysis, with both modes applied using continuous or intermittent RRT; trials comparing continuous to intermittent RRT were excluded, (4) outcomes: all-cause mortality (primary outcome) or other clinically important outcomes (see below) for the parallel-group trials; or group-specific filter duration, or clearance or plasma concentration measurements of cleared substances for both parallel-group and crossover trials. We also included trials of hemodiafiltration (that is, combined dialysis-filtration) compared to either hemodialysis or hemofiltration in sensitivity analyses as explained below.
Data abstraction and validity assessment
Two unblinded reviewers independently abstracted data from included trials, including study population (number of centers, age, gender, illness acuity proportion with oliguria and sepsis, baseline creatinine and urea), RRT methods (modality, dose, duration of and criteria for starting/stopping study RRT), outcomes (mortality, RRT duration, RRT dependence in survivors, hemodynamics (for example, vasopressor doses), evolution of organ dysfunction, filter duration, measured clearances and plasma concentrations of metabolites) and study quality (including method of sequence generation and allocation concealment, intention-to-treat analysis, loss to follow-up for the outcome of mortality, and early trial stopping for efficacy before the planned enrollment was completed). For the crossover trials we also assessed whether carry-over effects and washout periods were addressed and whether paired data analyses were performed [16]. Disagreements between reviewers regarding study selection and data abstraction that remained after author contact were resolved by consensus.
Data analysis
Our primary outcome was all-cause hospital mortality and, if not available, then mortality at 90, 60, 30 or 28 days after randomization, at ICU discharge or after stopping RRT (in descending order of preference). Secondary outcomes included RRT dependence among survivors at the latest time point available (with the same preferred order of time point as for the mortality analysis), RRT duration until renal recovery or death, filter duration, clearance of selected solutes and plasma concentration measurements.
Binary outcomes are reported as risk ratios (RR) and continuous outcomes using weighted mean differences (MD, a measure of absolute change) or ratio of means (RoM, a measure of relative change) [17]. We used Review Manager 5.1 (The Cochrane Collaboration, Oxford, England, UK) to calculate pooled outcome measures. We considered (two-sided) P <0.05 as statistically significant and reported individual trial and summary results with 95% confidence intervals (CIs). We used random-effects models, which incorporate between-trial heterogeneity and give wider confidence intervals when heterogeneity is present, to pool data. We assessed statistical heterogeneity among trials using I2, the percentage of total variability across studies due to heterogeneity rather than chance [18, 19], and used published thresholds to ascribe low (I2 = 25 to 49%), moderate (I2 = 50 to 74%), and high (I2 ≥75%) heterogeneity [19]. Continuous variables are expressed as mean ± standard deviation, unless otherwise indicated. Because the crossover trials generally did not report within-patient differences, we used the unpaired group-specific means to pool data, recognizing that this approach reduces the statistical power to detect differences [20].
For each outcome, the primary analysis included only trials in which one group was treated only with hemofiltration and the other group only with hemodialysis, with both groups receiving RRT providing similar (that is, within 20%) small-molecule clearances. In assessing equivalency of doses, we determined whether trial authors adjusted for the reduced dose of hemofiltration that results from blood dilution by pre-filter replacement fluid, where applicable. In sensitivity analyses for each outcome, we included data from trials in which doses differed by greater than 20% between the convection and diffusion groups, and from trials comparing combined filtration-dialysis modes to either filtration or dialysis. For trials in which one group was treated with combined filtration-dialysis, this group was considered either as filtration (if compared to a dialysis-only group) or dialysis (if compared to a filtration-only group).
To assess for publication bias we planned to visually examine a funnel plot of study precision versus treatment effect on mortality for evidence of asymmetry, assuming ≥5 trials in the analysis.
Because this study reports an analysis of published data, ethical approval was not required.
Results
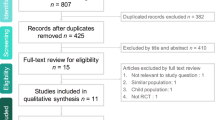
Study flow
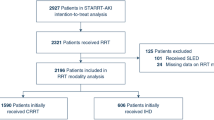
Our search strategy identified 6,657 citations, 6,324 from Medline, EMBASE Classic and EMBASE and 333 from the Cochrane Central Register of Controlled Trials. We retrieved 41 articles for detailed evaluation, of which 19 studies met criteria for inclusion [21–39] and 22 were excluded [40–61] (Figure 1). They included 10 parallel-group trials [21–30] and 9 crossover trials [31–39]. Among the parallel-group trials, authors of 9 included trials [21, 23–30] provided additional methodological or clinical data, and the author of the 10th trial [22] informed us that no additional information was available. In addition, authors of two studies informed us either that the vast majority of enrolled randomized patients did not have renal failure [40], or that it was not a randomized controlled trial [41] (reference [62] is the full paper for the abstract reference [41]), leading to exclusion of these studies.
Description of included studies (Table 1)
Enrolled patients had high illness severity. The mean or median acute physiology and chronic health evaluation (APACHE) II score [63] was ≥20 or simplified acute physiology score (SAPS) II [64] was ≥60, as reported in 8 of 10 parallel-group trials [21–27, 29] and 3 of 9 crossover trials [37–39]. One parallel-group trial reported only the mean sequential organ failure assessment (SOFA) [65] score of 16 [30]. Where reported, the vast majority of patients required mechanical ventilation or vasopressors [21, 23, 25, 29–32, 35, 36]. AKI was defined by abnormal biochemistry (serum creatinine or urea) or a complication of oliguria (such as volume overload, hyperkalemia, acidosis or uremic symptoms) in 7 of 10 parallel-group trials [21, 23–26, 29, 30] and 3 of 9 crossover trials [34, 35, 38]. The remaining nine trials enrolled patients with AKI requiring RRT without reporting specific AKI criteria [22, 27, 28, 31–33, 36, 37, 39]. Five trials explicitly excluded patients with chronic kidney disease, defined by pre-morbid creatinine or creatinine clearance [23, 25, 26, 29] or recent dialysis [30],
Description of RRT interventions (Table 2)
Seven of the 10 parallel-group trials used continuous RRT [21, 22, 24–27, 30–39], 1 trial used intermittent RRT [23] and 2 trials used sustained low efficiency RRT provided in sessions of eight hours each day [28, 29]. Only three parallel-group trials, all using CRRT, (n = 24 [24], n = 20 [25], n = 78 [30]) compared exclusively hemofiltration to exclusively hemodialysis at similar small-molecule doses. Of these, one trial allocated patients to higher (2.5 L/h) or lower (1 L/h) dose continuous veno-venous hemofiltration (CVVH) or continuous veno-venous hemodialysis (CVVHD) in a 2 × 2 factorial design [24]. In six of the remaining seven parallel-group trials, patients treated with hemofiltration (n = 20 [21], n = 206 [26], n = 96 [27]) or hemodialysis (n = 13 [22], n = 39 [23], n = 60 [29]) were compared to a group treated with hemodiafiltration (hemofiltration and hemodialysis). Hemodiafiltration recipients received higher doses, except in three trials where doses in the two treatment arms were similar, although not corrected for lower clearance due to pre-filter addition of replacement fluid [23, 27, 29]. The seventh trial, which used sustained low efficiency RRT and was reported only in abstract form, randomized patients into three groups: two similar-dose groups of hemodialysis (n = 6) and hemodiafiltration (n = 5) and a lower-dose group of hemofiltration (n = 6) [28]. Only one parallel-group trial was multi-centered [30].
All crossover trials were single-centered, used CRRT, and included few randomized patients (median 11.5 patients (range, 5 to 31)) [31–39]. Six of nine crossover trials [31, 33, 34, 36–38] compared hemofiltration and hemodialysis at similar doses. Of these, only three trials reported post-filter addition of replacement fluid [33, 37] or appropriately adjusted the rate of pre-filter replacement fluid to compare similar clearances [38]. Patients in one of these three trials [37] received three treatments (post-filter hemofiltration, pre-filter hemofiltration and hemodialysis) in random order. In another trial [31], patients received hemofiltration and three doses of hemodialysis in random order. For this trial, we excluded the two higher dose hemodialysis groups and retained the two matched-dose hemofiltration and hemodialysis groups.
In the remaining three crossover trials, hemofiltration was compared to a mixture of hemofiltration and hemodialysis at either higher [32, 35] or lower [39] doses. In one of these trials [32], patients were crossed over twice and received their initial treatment a second time; only data from the first two treatments were included.
One parallel-group trial used different fixed doses based on weight ranges [26] while two others used weight-based dosing [27, 30]. The parallel-group trials with sustained low efficiency RRT used fixed doses for the hemodialysis and hemodiafiltration groups [29] and weight-based dosing for the hemofiltration group [28]. One crossover trial used weight-based dose prescriptions for both interventions [38], while another used it only for hemofiltration [39]. The remaining trials used either fixed doses [22–25, 31, 33, 34, 36, 37] or dose ranges not directly related to patient weight [21, 32, 35].
Among the parallel-group trials, RRT was discontinued at the clinicians' discretion [21–23, 25, 27, 29], after a fixed duration [24, 28], or when protocol-defined criteria were met [26, 30]. The mean duration of RRT ranged from 2 to 8 days in four parallel-group CRRT trials [24, 25, 27, 30] and just over 20 days in the parallel-group with intermittent therapy [23]. Among the crossover trials, patients were crossed over after a fixed time: 24 h for most trials [32, 34–37] and 0.5 h for one trial [33]. Two trials crossed patients over after filter clotting or failure [38, 39]. One trial did not report when patients were crossed over [31].
Study quality (Table 3)
In the parallel-group trials that provided these data, all patients were analyzed according to the group to which they were initially assigned, and withdrawal of randomized patients from the mortality analysis either did not occur [26, 27] or comprised ≤5% of randomized patients [21, 23, 30]. Caregiver blinding was not practical in any trial, given the nature of the intervention. Four trials reported [21, 23, 26, 30] concealed allocation. In three trials reporting mortality [24, 25, 27] the authors informed us that they allocated patients to interventions in an alternating manner. The author of one trial informed us that the trial stopped early for benefit [26]. This trial was included only in the sensitivity analyses due to the use of differing doses and a mixture of hemofiltration and hemodialysis. Quality measures shown in Table 3 were generally not reported for the crossover trials, although in two crossover trials, authors reported that 3/13 (23%) [34] and 14/45 (31%) [39] patients were not crossed over to the other treatment. Carryover effects were generally ignored, which may have been reasonable given that the impact of clearance mode on solute removal should manifest relatively quickly [8], and subsequent clearance and concentration measurements were collected over a period of 12 to 24 hours after crossover in most trials. The trial with the shortest measurement period (30 minutes) provided a 10-minute equilibration period after crossover prior to data collection [33]. For one other trial [37], we included data collected over 12 hours but not starting until 12 hours after crossover. Most crossover trials reported using paired analyses [33–37, 39], but none provided individual patient data or mean within-patient difference data. Therefore, we were restricted to using group-specific means to perform meta-analyses, as discussed in the Methods.
Clinical outcomes
The three parallel group trials that compared similar doses of hemofiltration to hemodialysis were included in the primary analysis and reported either ICU [24, 25] or hospital [30] mortality. Five additional parallel-group trials comparing similar [23, 27, 29] or different [21, 26] doses of hemodiafiltration to either hemodialysis or hemofiltration reported mortality data and were included in the sensitivity analysis. They reported hospital [21, 23], 28-day [27, 29], or 90-day [26] mortality. We did not identify differences in pooled mortality in the primary (RR 0.96, 95% CI 0.73 to 1.25, P = 0.76; three trials, 121 patients) or sensitivity (RR 1.10, 95% CI 0.88 to 1.38, P = 0.38; eight trials, 540 patients) analyses (Figure 2). Statistical heterogeneity was absent (I2 = 0%) and moderate (I2 = 50%), respectively. Visual inspection of the funnel plot for the sensitivity analysis did not suggest publication bias.
Dialysis dependence in survivors was not different between groups (primary analysis: RR 1.33, 95% CI 0.35 to 5.08, P = 0.67; two trials [25, 30], 37 surviving patients; sensitivity analysis: RR 0.95, 95% CI 0.44 to 2.04, P = 0.89; four trials [25–27, 30], 177 surviving patients), with no statistical heterogeneity (I2 = 0%). Two trials reported no differences in SOFA scores 72 hours after starting therapy (primary analysis: RoM 1.02, 95% CI 0.89 to 1.16, P = 0.79; one trial, 63 patients [30]; sensitivity analysis: RoM 1.00, 95% CI 0.61 to 1.64, P = 0.99; two trials, 124 patients [27, 30]). One trial reported lower SOFA scores in the hemofiltration group primarily between four and seven days, driven primarily by the cardiovascular component (reflecting lower vasopressor requirements); however, this decrease was not statistically significant [30]. Another trial reported no difference in norepinephrine doses or changes in the multi-organ dysfunction score (MODS) [66] or APACHE II score between continuous hemofiltration and hemodialysis groups over the first 72 hours [24]. One parallel-group trial, comparing intermittent hemodiafiltration to hemodialysis, reported similar improvements in MODS between groups over 10 days [23], and another comparing sustained low efficiency dialysis to diafiltration reported similar improvements in blood pressure between groups over three days [29].
Pooled data from two small crossover trials using similar dose CVVH vs. CVVHD [34, 38] suggest that hemofiltration may shorten the time to filter failure, although only the RoM result achieved statistical significance (MD -7.3 hours, 95% CI -19.4 to +4.9, P = 0.24, I2 = 38%; RoM 0.67, 95% CI 0.45 to 0.99, P = 0.04, I2 = 7%; n = 50). Incorporating the results of one parallel-group trial using similar dose CVVH vs. hemodiafiltration (CVVHDF) [27] produced a pooled result that was significant for both effect measures (MD -5.4 hours, 95% CI -9.6 to -1.3 hours, P = 0.01; RoM 0.70, 95% CI 0.56 to 0.88, P = 0.003; I2 = 0% in both analyses; n = 113). Recognizing that higher dose may also affect filter life, two other trials comparing non-equivalent doses in the two treatment arms demonstrated shorter time to filter clotting in the higher dose group. One crossover trial comparing higher dose CVVH to CVVHDF [39] demonstrated an even greater decrease in filter life in the CVVH group, and one parallel group trial comparing lower dose CVVH to CVVHDF [26] demonstrated a non-statistically significant shorter time to filter clotting in the higher-dose group (Figure 3). Including the data from trials with non-equivalent doses in the two treatment arms in the pooled analysis resulted in a similar shortened time to filter failure in the hemofiltration group (MD -5.6 hours, 95% CI -10.4 to -0.9 hours, P = 0.02; RoM 0.69, 95% CI 0.50 to 0.95, P = 0.02; five trials, 383 patients), with higher heterogeneity (I2 = 51 to 66%). All these trials used unfractionated heparin anti-coagulation and pre-filter replacement fluid except for one trial that used a mixture of pre- and post-filter replacement to keep the filtration fraction <20% [38]. This reduction in filter survival time of about one-third is equivalent to a 50% increase in filters required for hemofiltration compared to hemodialysis.
Clearances of small and large molecules (Table 4)
Few molecules were examined in more than one study, and analyses included few patients. In general, small molecule clearance (for example, urea, phosphate and creatinine) was similar between hemofiltration and hemodialysis, whereas hemofiltration achieved higher clearance of larger molecules (up to around 20 kiloDaltons (kDa)). Pooled data from two studies [24, 34] showed similar clearance of interleukin (IL)-6 between modes, but statistical heterogeneity was high. Single studies also found that hemofiltration delivered significantly higher clearances of protein and albumin (using a high (60 kDa) cut-off filter) [24], and almost all amino acids in one study examining pediatric patients receiving amino acid supplementation [36].
The impact of clearance mode on serum concentrations of various solutes of interest was reported even less frequently. One crossover trial [34] found the concentration of tumor necrosis factor (TNF) α (but not IL-6, IL-10, SL-selectin, and endotoxin) to be significantly lower in the patients during hemofiltration. A second crossover trial [35] found no differences in concentrations of mediators of endothelial activation. One parallel-group trial [25] measured a larger decrease in IL-6 and smaller increase in TNFα concentration in the hemofiltration group, but these cytokines were only measured in one patient treated with hemofiltration and two patients treated with hemodialysis. Finally, the crossover trial of pediatric patients receiving amino acid supplementation [36] reported lower serum concentrations of amino acids in association with higher clearances in the hemofiltration group.
Discussion
This systematic review and meta-analysis highlights the paucity of data from randomized controlled trials comparing hemofiltration to hemodialysis in the treatment of AKI. Considering clinical outcomes of hemofiltration in parallel-group RCTs, there was no indication of improved mortality or organ dysfunction, although confidence intervals were wide. Our meta-analysis suggests that hemofiltration shortens filter life by about five to six hours (or one-third of total mean filter time). Based primarily on crossover RCTs, we found that hemofiltration increases the clearance of medium to larger molecules compared to hemodialysis. Almost no studies determined whether the enhanced middle-molecule clearance attributed to hemofiltration actually led to lower serum concentrations.
The trials reporting on filter failure rates used primarily pre-filter addition of replacement fluid. Comparing pre-filter to post-filter addition, one trial [37] included in this meta-analysis and other studies [67–69] have demonstrated that replacement fluid requirements are about 15 to 20% higher to achieve similar small molecule clearance rates at doses of around 20 mL/kg/h. Our finding of a 33% shorter time to filter failure with hemofiltration, combined with its higher fluid requirements to achieve similar small molecule clearance, implies that hemofiltration may consume more resources than hemodialysis. This hypothesis merits further evaluation in a formal cost analysis.
Comparing the published practice survey data in different countries and regions [10–15] (summarized in Figure 4), it appears that physicians tend to use a mode with at least some hemofiltration (that is, either CVVH or CVVHDF), perhaps anticipating additional benefit associated with hemofiltration. However, the small number of trials, randomized patients and events does not support this belief. A well-designed and adequately powered trial would be necessary to establish the superiority of hemofiltration.
Distribution of mode of RRT used in different countries/regions based on practice surveys. Abbreviations: CRRT, continuous renal replacement therapy; CVVH, continuous venovenous hemofiltration; CVVHD, continuous venovenous hemodialysis; CVVHDF, continuous venovenous hemodiafiltration; ICU, intensive care unit; MD, medical doctor; NZ, New Zealand; RRT, renal replacement therapy; UK, United Kingdom; US, United States.
Strengths of our review include methods to minimize bias, such as a comprehensive literature search, duplicate data abstraction, consideration of important clinical outcomes, and inclusion of additional methodological or clinical information from authors. The primary limitation is the small number and size of RCTs comparing pure hemofiltration to pure hemodialysis at similar doses. Sensitivity analyses, including trials whose arms also varied with respect to dose, gave similar results, as expected given recent large trials [4, 5] and meta-analyses [6, 7] that found similar outcomes with different RRT doses. In addition, trials varied in the modality of RRT used, timing of initiation, and types of filters and blood flows, although recent meta-analyses have not found differential outcomes based on these factors [70–73]. We did not consider comparisons of blood clearance modes with peritoneal dialysis [74, 75], which is used in some areas of the world to treat acute kidney failure. Finally, heterogeneity may have been underestimated because these tests are underpowered when there are few trials. Although hemofiltration is of particular interest in patients with sepsis, in whom pro-inflammatory mediators are increased, there was insufficient data to conduct a subgroup analysis in these patients. In addition, we did not examine the role of hemofiltration vs hemodialysis in patients with sepsis who have not yet developed AKI [40] or the role of hemofiltration compared to no RRT [76–79].
Conclusions
Pooled data from a few randomized trials suggest that hemofiltration increases the clearance of medium to larger molecules without improving clinical outcomes, though confidence intervals are wide. Hemofiltration may also reduce filter life. This latter finding, together with the increased replacement fluid requirements to achieve equivalent small-molecule clearance when pre-filter replacement is used, suggests that hemofiltration may be more expensive than hemodialysis. Our findings support the need for additional pilot data [80] to evaluate the impact of hemofiltration vs. hemodialysis on intermediate outcomes, such as vasopressor requirements, that may serve as valid surrogates for important clinical outcomes that could subsequently be evaluated in a large definitive trial.
Key messages
-
Few randomized controlled trials have compared hemofiltration vs hemodialysis for the treatment of acute kidney injury.
-
Pooling the results from these trials does not suggest beneficial clinical outcomes of hemofiltration vs hemodialysis, but confidence intervals are wide.
-
Compared to hemodialysis, hemofiltration may increase clearance of medium to larger molecules, but may also shorten the time to filter failure.
-
Additional pilot trials are needed to evaluate the impact of hemofiltration vs. hemodialysis on intermediate outcomes, such as vasopressor requirements, that may serve as valid surrogates for important clinical outcomes that could subsequently be evaluated in a large definitive trial.
Abbreviations
- AKI:
-
acute kidney injury
- APACHE:
-
acute physiology and chronic health evaluation
- CI:
-
confidence interval
- CRRT:
-
continuous renal replacement therapy
- CVVH:
-
continuous veno-venous hemofiltration
- CVVHD:
-
continuous veno-venous hemodialysis
- CVVHDF:
-
continuous veno-venoous hemodiafiltraion
- HD:
-
hemodialysis
- HF:
-
hemofiltration
- I 2 I 2 :
-
heterogeneity measure
- ICU:
-
intensive care unit
- IL:
-
interleukin
- kDa:
-
kiloDalton
- MD:
-
mean difference
- MODS:
-
multi-organ dysfunction score
- RCT:
-
randomized controlled trial
- RoM:
-
ratio of means
- RR:
-
relative risk
- RRT:
-
renal replacement therapy
- SAPS:
-
simplified acute physiology score
- SOFA:
-
sequential organ functional assessment
- TNF:
-
tumor necrosis factor
References
Uchino S, Kellum J, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C, for the Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators: Acute Renal Failure in Critically Ill Patients: A multinational, multicenter study. JAMA. 2005, 294: 813-818. 10.1001/jama.294.7.813.
Bagshaw SM, Lapinsky S, Dial S, Arabi Y, Dodek P, Wood G, Ellis P, Guzman J, Marshall J, Parrillo JE, Skrobik Y, Kumar A, the Cooperative Antimicrobial Therapy of Septic Shock (CATSS) Database Research Group: Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med. 2009, 35: 871-881. 10.1007/s00134-008-1367-2.
Wald R, Quinn RR, Luo J, Li P, Scales DC, Mamdani MM, Ray JG, for the University of Toronto Acute Kidney Injury Research Group: Chronic dialysis and death among survivors of acute kidney injury requiring dialysis. JAMA. 2009, 302: 1179-1185. 10.1001/jama.2009.1322.
The RENAL Replacement Therapy Study Investigators: Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med. 2009, 361: 1627-1638.
The VA/NIH Acute Renal Failure Trial Network: Intensity of renal support in critically ill patients with acute kidney injury. N Eng J Med. 2008, 359: 7-20.
Van Wert R, Friedrich JO, Scales DC, Wald R, Adhikari NKJ: High-dose renal replacement therapy for acute kidney injury: systematic review and meta-analysis. Crit Care Med. 2010, 38: 1360-1369. addendum Crit Care Med 2010, 38:2424-2425
Jun M, Heerspink HJL, Ninomiya T, Gallagher M, Bellomo R, Myburgh J, Finfer S, Palevsky PM, Kellum JA, Perkovic V, Cass A: Intensities of renal replacement therapy in acute kidney injury: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2010, 5: 956-963. 10.2215/CJN.09111209.
Brunet S, Leblanc M, Geadah D, Parent D, Courteau S, Cardinal J: Diffusive and convective solute clearances during continuous renal replacement therapy at various dialysate and ultrafiltration flow rates. Am J Kidney Dis. 1999, 34: 486-492. 10.1016/S0272-6386(99)70076-4.
Ronco C, Tetta C, Mariano F, Wratten ML, Bonello M, Bordoni V, Cardona X, Inguaggiato P, Pilotto L, d'Intini V, Bellomo R: Interpreting the mechanisms of continuous renal replacement therapy in sepsis: the peak concentration hypothesis. Artif Organs. 2003, 27: 792-801. 10.1046/j.1525-1594.2003.07289.x.
Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten H, Ronco C, Kellum JA: Continuous renal replacement therapy: a worldwide practice survey. The beginning and ending supportive therapy for the kidney (B.E.S.T. kidney) investigators. Intensive Care Med. 2007, 33: 1563-1570. 10.1007/s00134-007-0754-4.
Renal Study Investigators: Renal replacement therapy for acute kidney injury in Australian and New Zealand intensive care units: a practice survey. Crit Care Resusc. 2008, 10: 225-230.
Gatward JJ, Gibbon GJ, Wrathall G, Padkin A: Renal replacement therapy for acute renal failure: a survey of practice in adult intensive care units in the United Kingdom. Anaesthesia. 2008, 63: 959-966. 10.1111/j.1365-2044.2008.05514.x.
Overberger P, Pesacreta M, Palevsky PM, for the VA/NIH Acute Renal Failure Trial Network: Management of Renal Replacement Therapy in Acute Kidney Injury: a survey of practitioner prescribing practices. Clin J Am Soc Nephrol. 2007, 2: 623-630. 10.2215/CJN.00780207.
Flores FX, Brophy PD, Symons JM, Fortenberry JD, Chua AN, Alexander SR, Mahan JD, Bunchman TE, Blowey D, Somers MJG, Baum M, Hackbarth R, Chand D, McBryde K, Benfield M, Goldstein SL: Continuous renal replacement therapy (CRRT) after stem cell transplantation. A report from the prospective pediatric CRRT Registry Group. Pediatr Nephrol. 2008, 23: 625-630. 10.1007/s00467-007-0672-2.
Zwillman M, Adhikari NK, Meade MO, Hladunewich M, Piquette D, Friedrich JO: Survey of continuous renal replacement therapy in Canadian intensive care units [Abstract]. Inten Care Med. 2006, 32: S161-
Mills EJ, Chan A-W, Wu P, Vail A, Guyatt GH, Altman DG: Design, analysis, and presentation of crossover trials. Trials. 2009, 10: 27-10.1186/1745-6215-10-27.
Friedrich JO, Adhikari NK, Beyene J: The ratio of means method as an alternative to mean differences for analyzing continuous outcome variables in meta-analysis: a simulation study. BMC Med Res Methodol. 2008, 8: 32-10.1186/1471-2288-8-32.
Higgins JP, Thompson SG: Quantifying heterogeneity in a meta-analysis. Stat Med. 2002, 21: 1539-1558. 10.1002/sim.1186.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG: Measuring inconsistency in meta-analyses. BMJ. 2003, 327: 557-560. 10.1136/bmj.327.7414.557.
Elbourne DR, Altman DG, Higgins JPT, Curtin F, Worthington HV, Vail A: Meta-analyses involving cross-over trials: methodological issues. Int J Epidemiol. 2002, 31: 140-149. 10.1093/ije/31.1.140.
Davenport A, Will EJ, Davidson AM: Improved cardiovascular stability during continuous modes of renal replacement therapy in critically ill patients with acute hepatic and renal failure. Crit Care Med. 1993, 21: 28-338.
Alamartine E, de Filippis JP, Toulon J, Berthoux F: On-line continuous venovenous hemodiafiltration: a technique for the control of ultrafiltration and convection during continuous renal replacement therapy. Ren Fail. 1994, 16: 707-714. 10.3109/08860229409044900.
Pettila V, Tiula E: Intermittent hemodiafiltration in acute renal failure in critically ill patients. Clin Nephrol. 2001, 56: 324-331.
Morgera S, Slowinski T, Melzer C, Sobottke V, Vargas-Hein O, Volk T, Zuckermann-Becker H, Wegner B, Műller JM, Baumann G, Kox WJ, Bellomo R, Neumayer H-H: Renal replacement therapy with high-cutoff hemofilters: impact of convection and diffusion on cytokine clearances and protein status. Am J Kidney Dis. 2004, 43: 444-453. 10.1053/j.ajkd.2003.11.006.
Daud KM, Leong GB, Visvanathan R: Acute dialytic support for the critically ill: continuous venovenous haemodialysis versus continuous venovenous haemofiltration. Int Med J. 2006, 13: 37-42.
Saudan P, Niederberger M, De Seigneux S, Romand J, Pugin J, Perneger T, Martin PY: Adding a dialysis dose to continuous hemofiltration increases survival in patients with acute kidney failure. Kidney Int. 2006, 70: 1312-1317. 10.1038/sj.ki.5001705.
Chang JW, Lee HK, Yang WS, Kim SB, Park S-K, Lee SK, Park JS: No difference in clearance and survival between continuous hemodiltration and hemodiafiltration at the same net effluent in patients with acute renal failure [Abstract]. Crit Care Med. 2009, 37 (Suppl): A473-
Ratanarat R, Rugsasuk S, Chanchairujira T, Athirakul K, Vasuvattakul S: Effect of prolonged intermittent renal replacement therapy on phosphate kinetics in critically ill patients with acute kidney injury [Abstract]. J Am Soc Nephrol. 2009, 20: 602A-
Ratanarat R, Chaipruckmalakarn T, Laowahutanont N, Larpparisuth N, Vasuvattakul S: Efficacy and hemodynamic outcome of prolonged intermittent renal replacement therapy (PIRRT) in critically ill patients: a preliminary report. J Med Assoc Thai. 2012, 95 (Suppl 2): S265-S271.
Wald R, Friedrich JO, Bagshaw SM, Burns KEA, Garg AX, Hladunewich MA, House AA, Lapinsky S, Pannu NI, Richardson RM, Thorpe K, Adhikairi N: The optimal mode of renal replacement therapy in acute kidney injury (OMAKI): a pilot randomized controlled trial of CVVH vs. CVVHD [Abstract]. J Am Soc Nephrol. 2011, 22: 10B-
Maher ER, Hart L, Levy D, Scoble JE, Baillod RA, Sweny P, Varghese Z, Moorhead JF: Comparison of continuous arteriovenous haemofiltration and haemodialysis in acute renal failure [Letter]. Lancet. 1988, 1: 129-
Alarabi AA, Taube A, Danielson BG, Wikstroem B: Continuous ateriovenous haemodialysis and haemofiltration in intensive care acute renal failure patients. Int Urol Nephrol. 1992, 24: 657-664. 10.1007/BF02551303.
Jeffrey RF, Khan AA, Prabhu P, Todd N, Goutcher E, Will EJ, Davison AM: A comparison of molecular clearance rates during continuous hemofiltration and hemodialysis with a novel volumetric continuous renal replacement system. Artif Organs. 1994, 18: 425-428. 10.1111/j.1525-1594.1994.tb02228.x.
Kellum JA, Johnson JP, Kramer D, Palevsky P, Brady JJ, Pinsky MR: Diffusive vs. convective therapy: effects on mediators of inflammation in patients with severe systemic inflammatory response syndrome. Crit Care Med. 1998, 26: 1995-2000. 10.1097/00003246-199812000-00027.
Garcia-Fernandez N, Lavilla FJ, Rocha E, Purroy A: Haemostatic changes in systemic inflammatory response syndrome during continuous renal replacement therapy. J Nephrol. 2000, 13: 282-289.
Maxvold NJ, Smoyer WE, Custer JR, Bunchman TE: Amino acid loss and nitrogen balance in critically ill children with acute renal failure: a prospective comparison between classic hemofiltration and hemofiltration with dialysis. Crit Care Med. 2000, 28: 1161-1165. 10.1097/00003246-200004000-00041.
Wynckel A, Cornillet J, Bene B, Stolz A, Lepouse C, Paris B, Chanard J: Improved removal of small proteins using continuous venovenous hemofiltration to treat acute renal failure. ASAIO J. 2004, 50: 81-84. 10.1097/01.MAT.0000104823.48673.BD.
Ricci Z, Ronco C, Bachetoni A, D'amico G, Rossi S, Alessandri E, Rocco M, Pietropaoli P: Solute removal during continuous renal replacement therapy in critically ill patients: convection versus diffusion. Crit Care. 2006, 10: R67-10.1186/cc4903.
Davies HT, Leslie G, Pereira SM, Webb SA: A randomized comparative crossover study to assess the affect on circuit life of varying pre-dilution volume associated with CVVH and CVVHDF. Int J Artif Organs. 2008, 31: 221-227.
Li Y, Hu ZJ, Li CX, Cui Y, Dai QC, Guo JP: A clinical study on different modalities of blood purification for the treatment of sepsis [Chinese]. Chin Crit Care Med. 2009, 21: 369-370.
Marchionna N, Floris M, Brendolan A, Nalesso F, Zanella M, Ronco C: Solutes removal during continuous renal replacement therapy in critically ill patients with a new high polysulfone-based hemofilter (CUREFLO®): convection vs. diffusion [Abstract]. J Am Soc Nephrol. 2010, 21: 893A-
Raja R, Karmer M, Goldstein S, Caruana R, Lerner A: Comparison of continuous arteriovenous hemofiltration and continuous arteriovenous dialysis in critically ill patients. ASAIO Trans. 1986, 435-436.
Zobel G, Ring E, Zobel V: Continuous arteriovenous renal replacement systems for critically ill children. Ped Nephrol. 1989, 3: 140-143. 10.1007/BF00852895.
Bellomo R, Ernest D, Parkin G, Boyce N: Clearance of vancomycin during continuous arteriovenous hemodiafiltration. Crit Care Med. 1990, 18: 181-183. 10.1097/00003246-199002000-00011.
Hirasawa H, Sugai T, Ohtake Y, Oda S, Shiga H, Matsuda K, Kitamura N: Continuous hemofiltration and hemodiafiltration in the management of multiple organ failure. Contrib Nephrol. 1991, 93: 42-46.
Valtonen M, Tiula E, Neuvonen PJ: Effect of continuous venovenous haemofiltration and haemodiafiltration on the elimination of fluconazole in patients with acute renal failure. J Antimicrob Chemother. 1997, 40: 695-700. 10.1093/jac/40.5.695.
Meloni C, Morosetti M, Turani F, Palombo G, Meschini L, Zupancich E, Taccone-Gallucci M, Di Giulio S, Casciani CU: Cardiac function and oxygen balance in septic patients during continuous hemofiltration. Blood Purif. 1998, 16: 140-146. 10.1159/000014327.
Booth M, Fox C, Dobb G: Energy losses associated with continuous venovenous haemodiafiltration in intensive care patients [Abstract]. Br J Anaesth. 1995, 74 (Suppl 1): 109-
Favre H, Blanc E, Emonet S, Claeysen D: Treatment of acute renal insufficiency with continuous veno-venous haemofiltration; importance of precise fluid balance control [French] [Abstract]. Schweiz Med Wochenschr. 1996, 126 (Suppl 81): 17-
Cole L, Bellomo R, Baldwin I: A randomized, prospective, crossover study of the hemodynamic effects of high-volume hemofiltration in patients with septic shock [Conference Proceedings]. Blood Purif. 1998, 16: 113-114.
Dilek K, Ersoy A, Gűllűlű M, Aslanhan I, Emir G, Dalkỷlỷç E, Karabulut Y, Usta M, Ilcol Y, Yavuz M, Yurtkuran M: Crush syndrome developing acute renal failure in the Marmar earthquake: the comparison of the effects of different hemodialysis approaches on renal functions and mortality rates [Abstract]. Nephol Dial Transplant. 2000, 15: A82-10.1093/ndt/15.1.82.
Lins RL, Elseviers MM, Van der Niepen P, Hoste E, Malbrain ML, Damas P, Devriendt J, SHARF investigators: Intermittent versus continuous renal replacement therapy for acute kidney injury patients admitted to the intensive care unit: results of a randomized clinical trial. Nephol Dial Transplant. 2009, 24: 512-518.
Zhao SP, Wu J, Ai YH, Sun B, Xu DM, Guo QL: Comparison of clinical efficacy between continuous veno-venous hemofiltration (CVVH) and CVVH combined with hemoperfusion for the treatment of multiple organ dysfunction syndrome [Chinese]. Chin Crit Care Med. 2009, 21: 373-374.
Lui P, He YZ, Zhang XG, Li G, Wang HC, Lu XX, Zhang CG, Meng QY: Studying the therapic effects of hemoperfusion with continuous venovenous hemofiltration on the patients with acute paraquat poisoning] [Chinese]. Chin J Industrial Hygiene Occupat Dis. 2011, 29: 266-269.
Guo JP, Hu ZJ, Li CX, Li Y, Cui Y, Jia CM: Clinical comparison of efficiency in clearance of interleukin-8 and life of filtrator with continuous venous blood filtration using different proportion of pre- and post-dilution of filtration fluid] [Chinese]. Chin Crit Care Med. 2011, 23: 189-190.
Hubsher J, Olshan AR, Schwartz AB, Zoranski B, DeClement F, Bendlin A, Hensell D, Brezin JH, Krevolin LE, Chinitz JL: Continuous arteriovenous hemofiltration for the treatment of anasarca and acute renal failure in severely burned patients. ASAIO Trans. 1986, 32: 401-404. 10.1097/00002480-198609000-00002.
Schetz M: Removal of cytokines in septic patients using continuous veno-venous hemodiafiltration. Crit Care Med. 1994, 22: 715-716. author reply 719-721
Wakabayashi Y, Kamijou Y, Soma K, Ohwada T: Removal of circulating cytokines by continuous haemofiltration in patients with systemic inflammatory response syndrome or multiple organ dysfunction syndrome. Br J Surg. 1996, 83: 393-394. 10.1002/bjs.1800830331.
Hirayama Y, Hirasawa H, Oda S, Shiga H, Nakanishi K, Matsuda K, Nakamura M, Hirano T, Moriguchi T, Watanabe E, Nitta M, Abe R, Nakada T: The change in renal replacement therapy on acute renal failure in a general intensive care unit in a university hospital and its clinical efficacy: a Japanese experience. Ther Apher Dial. 2003, 7: 475-482. 10.1046/j.1526-0968.2003.00094.x.
Davenport A, Will EJ, Davison AM: Effect of renal replacement therapy on patients with combined acute renal and fulminant hepatic failure. Kidney Int Suppl. 1993, 43: S245-S251.
Davenport A, Will EJ, Davison AM: Continuous vs. intermittent forms of haemofiltration and/or dialysis in the management acute renal failure in patients with defective cerebral autoregulation at risk of cerebral oedema. Contrib Nephrol. 1991, 93: 225-233.
Floris M, Marchionna N, Clementi A, Kim JC, Cruz DN, Nalesso F, Zanella M, Garzotto F, de Cal M, Virzì GM, Brendolan A, Ronco C: Evaluation of a new polysulfone hemofilter for continuous renal replacement therapy. Blood Purif. 2011, 32: 133-138. 10.1159/000325221.
Knaus WA, Draper EA, Wagner DP, Zimmermann JE: APACHE II: a severity of disease classification system. Crit Care Med. 1985, 13: 818-829. 10.1097/00003246-198510000-00009.
Le Gall JR, Lemeshow S, Saulnier F: A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993, 270: 2957-2963. 10.1001/jama.1993.03510240069035. [Erratum, JAMA 1994, 271:1321.]
Ferreira FL, Bota DP, Bross A, Melot C, Vincent JL: Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001, 286: 1754-1758. 10.1001/jama.286.14.1754.
Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ: Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995, 23: 1638-1652. 10.1097/00003246-199510000-00007.
Troyanov S, Cardinal J, Geadah D, Parent D, Courteau S, Caron S, Leblanc M: Solute clearances during continuous venovenous haemofiltration at various ultrafiltration flow rates using multiflow-100 and HF1000 filters. Nephol Dial Transplant. 2003, 18: 961-966. 10.1093/ndt/gfg055.
Parakininkas D, Greenbaum LA: Comparison of solute clearance in three modes of continuous renal replacement therapy. Pediatr Crit Care Med. 2004, 5: 269-274. 10.1097/01.PCC.0000123554.12555.20.
Nurmohamed SA, Jallah BP, Vervloet MG, Beishuizen A, Groeneveld ABJ: Predilution versus postdilution continuous venovenous hemofiltration: no effect on filter life and azotemic control in critically ill patients on heparin. ASAIO J. 2011, 57: 48-52. 10.1097/MAT.0b013e318201a599.
Pannu N, Klarenbach S, Wiebe N, Manns B, Tonelli M, Alberta Kidney Disease Network: Renal replacement therapy in patients with acute renal failure: a systematic review. JAMA. 2008, 299: 793-805. 10.1001/jama.299.7.793.
Bagshaw SM, Berthiaume LR, Delaney A, Bellomo R: Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: a meta-analysis. Crit Care Med. 2008, 36: 610-617. 10.1097/01.CCM.0B013E3181611F552.
Seabra VF, Balk EM, Liangos O, Sosa MA, Cendoroglo M, Jaber BL: Timing of renal replacement therapy initiation in acute renal failure: a meta-analysis. Am J Kidney Dis. 2008, 52: 272-284. 10.1053/j.ajkd.2008.02.371.
Wu M-Y, Hsu Y-H, Bai C-H, Lin Y-F, Wu C-H, Tam K-W: Regional citrate versus heparin anticoagulation for continuous renal replacement therapy: a meta-analysis of randomized controlled trials. Am J Kidney Dis. 2012, 59: 810-818. 10.1053/j.ajkd.2011.11.030.
Phu NH, Hien TT, Mai NTH, Chau TTH, Chuong LV, Loc PP, Winearls C, Farrar J, White N, Day N: Hemofiltration and peritoneal dialysis in infection-associated acute renal failure in Vietnam. N Engl J Med. 2002, 347: 895-902. 10.1056/NEJMoa020074.
George J, Varma S, Kumar S, Thomas J, Gopi S, Pisharody R: Comparing continuous venevenous hemodiafiltration and periotoneal dialysis in critically ill patients with acute kidney injury: a pilot study. Perit Dial Int. 2011, 31: 422-429. 10.3747/pdi.2009.00231.
Payen D, Mateo J, Cavaillon JM, Fraisse F, Floriot C, Vicaut E, Hemofiltration and Sepsis Group of the College National de Reanimation et de Medecine d'Urgence des Hopitaux extra-Universitaires: Impact of continuous venovenous hemofiltration on organ failure during the early phase of severe sepsis: a randomized controlled trial. Crit Care Med. 2009, 37: 803-810. 10.1097/CCM.0b013e3181962316.
Sander A, Armbruster W, Sander B, Daul AE, Lange R, Peters J: Hemofiltration increases IL-6 clearance in early systemic inflammatory response syndrome but does not alter IL-6 and TNF alpha plasma concentrations. Intensive Care Med. 1997, 23: 878-884. 10.1007/s001340050425.
Laurent I, Adrie C, Vinsonneau C, Cariou A, Chiche JD, Ohanessian A, Spaulding C, Carli P, Dhainaut JF, Monchi M: High-volume hemofiltration after out-of-hospital cardiac arrest: a randomized study. J Am Coll Cardiol. 2005, 46: 432-437. 10.1016/j.jacc.2005.04.039.
Honore PM, Jamez J, Wauthier M, Lee PA, Dugernier T, Pirenne B, Hanique G, Matson JR: Prospective evaluation of short-term, high-volume isovolemic hemofiltration on the hemodynamic course and outcome in patients with intractable circulatory failure resulting from septic shock. Crit Care Med. 2000, 28 (11): 3581-3587. 10.1097/00003246-200011000-00001.
Arnold DM, Burns KE, Adhikari NK, Kho ME, Meade MO, Cook DJ, McMaster Critical Care Interest Group: The design and interpretation of pilot trials in clinical research in critical care. Crit Care Med. 2009, 37 (1 Suppl): S69-74.
Hozo SP, Djulbegovic B, Hozo I: Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005, 5: 13-10.1186/1471-2288-5-13.
Acknowledgements
We are grateful to Eric Alarmartine [22], Jai Won Chang [27], Kamaliah Bt. Mohd Daud [25], Andrew Davenport [21], Yong Li [40], Stanislao Morgera [24], Ville Pettila [23], Ranistha Ratanarat [28], Claudio Ronco [41, 62] and Patrick Saudan [26] for providing additional data from their trials or for informing us that no additional data were available. We also thank Jennifer Tsang for assistance with translation of Chinese articles [40, 53–55]. We appreciate the thoughtful advice of Michelle Hladunewich, David Klein, Stephen Lapinsky and Robert Richardson from the Toronto Acute Kidney Injury Research Group. This study received no specific funding. Jan Friedrich and Karen Burns hold Clinician Scientist Awards with the Canadian Institutes of Health Research (CIHR). Sean Bagshaw holds a Canada Research Chair in Critical Care Nephrology and a Clinician Scientist Award from Alberta Innovates - Health Solutions (AI-HS). Neither CIHR nor AI-HS had any involvement in the design and conduct of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
JF and NA acquired and analyzed the data. JF wrote the first draft of the manuscript. All authors were involved with the conception and design of the study, interpretation of the data, and critical revision of the manuscript for important intellectual content. All authors have read and approved the manuscript for publication.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Friedrich, J.O., Wald, R., Bagshaw, S.M. et al. Hemofiltration compared to hemodialysis for acute kidney injury: systematic review and meta-analysis. Crit Care 16, R146 (2012). https://doi.org/10.1186/cc11458
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc11458