Abstract
Introduction
Protocols for the delivery of analgesia, sedation and delirium care of the critically ill, mechanically ventilated patient have been shown to improve outcomes but are not uniformly used. The extent to which elements of analgesia, sedation and delirium guidelines are incorporated into order sets at hospitals across a geographic area is not known. We hypothesized that both greater hospital volume and membership in a hospital network are associated with greater adherence of order sets to sedation guidelines.
Methods
Sedation order sets from all nonfederal hospitals without pediatric designation in Washington State that provided ongoing care to mechanically ventilated patients were collected and their content systematically abstracted. Hospital data were collected from Washington State sources and interviews with ICU leadership in each hospital. An expert-validated score of order set quality was created based on the 2002 four-society guidelines. Clustered multivariable linear regression was used to assess the relationship between hospital characteristics and the order set quality score.
Results
Fifty-one Washington State hospitals met the inclusion criteria and all provided order sets. Based on expert consensus, 21 elements were included in the analgesia, sedation and delirium order set quality score. Each element was equally weighted and contributed one point to the score. Hospital order set quality scores ranged from 0 to 19 (median = 8, interquartile range 6 to 14). In multivariable analysis, a greater number of acute care days (P = 0.01) and membership in a larger hospital network (P = 0.01) were independently associated with a greater quality score.
Conclusions
Hospital volume and membership in a larger hospital network were independently associated with a higher quality score for ICU analgesia, sedation and delirium order sets. Further research is needed to determine whether greater order-set quality is associated with improved outcomes in the critically ill. The development of critical care networks might be one strategy to improve order set quality scores.
Similar content being viewed by others
Introduction
In the ICU setting, mechanical ventilation is common, resource intensive and associated with pain, anxiety and delirium [1, 2]. Protocols and order sets (the mechanism by which a protocol is implemented) have been developed to optimize the care of mechanically ventilated patients [3]. In fact, analgesia and sedation protocols improve the duration of mechanical ventilation, the length of ICU stay, and survival in the setting of clinical trials [4–7]. However, the implementation of these protocols and their content are variable. Recent surveys showed that just over 70% of American academic ICUs had sedation protocols and only 40% of Canadian intensivists used a daily spontaneous awakening trial, an intervention shown to decrease the duration of mechanical ventilation [5, 8–10].
Clinical practice guidelines for mechanically ventilated patients have been developed by international professional organizations based on the analgesia, sedation and delirium treatment literature [11, 12]. Ideally, these guidelines and the professional literature itself would help hospitals develop order sets that would then be used in their ICUs to deliver evidence-based patient care. There is significant variation in order set development and guideline implementation, however, suggesting that this knowledge translation process is neither seamless nor uniform [9, 13].
Order set creation and knowledge translation are complex and incompletely understood processes [14–16]. Provider work load, lack of resources, variability in interpretation, and lack of familiarity with the guidelines have all been cited as reasons for incomplete knowledge translation [3, 13]. Using a structure-process-outcome model of quality improvement, we sought to identify hospital-level predictors of ICU analgesia, sedation and delirium order set quality - a structure quality element [17]. As an established relationship between volume and outcome exists in medicine, we hypothesized that higher-volume hospitals and hospitals that are members of a hospital network would be more likely to have higher-quality order sets with greater adherence to published guidelines [18–21]. We chose to look at hospital networks because some have described a potential role for the regionalization of critical care and our own experience has highlighted the fact that hospitals in a network tend to share protocols and order sets within their networks [22, 23].
Materials and methods
Hospital sample
We conducted a cross-sectional study of all nonfederal, nonpediatric acute care hospitals in Washington State between December 2010 and June 2011. Hospitals were identified using the Washington State Department of Health hospital database as well as the Washington State Hospital Association hospital list. Representatives of ICU leadership in each hospital were interviewed to determine whether their hospital provided ongoing care (defined as care for > 24 hours) for mechanically ventilated patients. All interviews were completed by telephone by one investigator (CRD). We excluded hospitals that transferred patients requiring ongoing mechanical ventilation, even if they provided short-term care to postoperative ventilated patients and those patients requiring stabilization prior to transfer.
A total of 101 hospitals were identified (Figure 1). Of these, 85 were nonfederal, nonpediatric acute care hospitals. Thirty hospitals did not provide ongoing care for ventilated patients and were excluded. Twenty-nine of the 30 acute care hospitals (97%) that did not provide ongoing mechanical ventilation were critical access hospitals, which by definition have 25 beds or fewer. Fifty-five hospitals provided ongoing care for ventilated patients. A member of the ICU leadership team at each of these hospitals was interviewed to determine whether the hospital possessed an order set or protocol that could be used to provide analgesia, sedation or delirium treatment for ICU patients. Fifty-one of the 55 hospitals (93%) reported that they had an order set or protocol. All provided a copy of their order sets and/or protocols and were included in the study sample. The four hospitals that provided ongoing care to mechanically ventilated patients but did not have an order set for analgesia, sedation or delirium treatment were excluded from the analysis. These four excluded hospitals had a median of 52 acute care beds and 21,132 acute care days in 2009, and one was a critical access hospital. Hospitals with multiple ICUs were queried about the existence of multiple order sets in their various ICUs, but all reported using the same analgesia, sedation and delirium protocol in all of their ICUs.
The Human Subjects Division of the University of Washington reviewed the study and determined it not to be human subject research and therefore exempt.
Variable definitions and abstraction
Hospital characteristics - including acute care and ICU bed numbers, acute care and ICU days, critical access status and hospital governance structure - were obtained from the Washington State Department of Health database for 2009. The ICU leadership team at each hospital was interviewed to ascertain the number of ICUs at the hospital, the availability of computerized provider order entry (CPOE), whether resident physicians provided care in the ICU, and whether the ICU was open or closed. A closed ICU was defined as one where all patients had their care transferred to, or directed by, an intensivist-led team [24]. A hospital network was defined as an entity that operated two or more hospitals in Washington State or an adjoining metro area. The hospital's membership in a larger hospital network was determined by review of the 2008 American Hospital Association hospital data file and a structured web search, and was confirmed via the ICU leadership interview. The chosen reference date for membership in a hospital network and the presence of CPOE was 1 January 2011.
The ICU leadership team was asked for an electronic or faxed copy of the order set or protocol that they used to provide analgesia, sedation and/or delirium management for mechanically ventilated patients. If more than one protocol was used to provide analgesia, sedation and delirium care (for example, a separate delirium protocol) then all relevant protocols were obtained and analyzed as one.
Development of an analgesia, sedation and delirium quality score
The 2002 American College of Critical Care Medicine, American Society of Health-System Pharmacists and American College of Chest Physician clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult were reviewed to generate a list of possible components that a high-quality analgesia, sedation and delirium protocol could contain (Table 1) [11]. Twenty-four proposed quality elements were found to be unique indicators of order set quality (10 items pertaining to analgesia, 10 items to sedation, and four items pertaining to delirium). Two potentially significant elements were not addressed by the 2002 guidelines: a daily spontaneous awakening trial for each eligible patient, and a paired daily spontaneous awakening trial and spontaneous breathing trial for all eligible patients. We felt that these elements were important enough to merit consideration for inclusion in the quality score even though they were not included in the 2002 guidelines. We purposely did not included elements related to specific medications or assessment tools.
A web-based survey was then sent to a convenience sample of 20 North American ICU directors and experts - individuals who have been academically active in ICU analgesia, sedation and delirium work - asking them to rate the importance of the 24 potential quality elements on the following four-point scale: 1 = very important (all high-quality critical care analgesia, sedation and delirium order sets should contain this element); 2 = somewhat important (a high-quality critical care analgesia/sedation order set would most probably contain this element, but some high-quality order sets may not contain it); 3 = not important/optional (a high-quality critical care analgesia/sedation order set may or may not contain this element); and 4 = drop/do not include (a high-quality critical care analgesia, sedation and delirium order set would not contain this element).
Of the 20 experts in ICU analgesia, sedation and delirium, 15 (75%) completed the survey and their responses were used to create a quality score. The mean (standard deviation) scores are shown in Table 1. All elements with a mean rating that the element would more likely than not be included in a high-quality order set were included in our score. Two items that were rated so as not to be included were: scheduled opioid doses or a continuous infusion are given preferentially over an as-needed regimen; and a patient-controlled analgesia device is preferred to deliver opioids if the patient is able to understand and operate the device.
To score the order sets and compute the quality score, composite survey questions with an 'and' or an 'or' conjunction were separated into two elements for abstraction. For example, 'pain is regularly assessed and documented' was abstracted as two separate items. The element 'the QT interval is monitored in patients receiving antipsychotics' was excluded from the final quality score as not all hospitals had antipsychotics as part of their orders and therefore may not require this quality element. Each element, regardless of its expert rating, was assigned one point towards the total score. The highest possible quality score was 21.
After training on a collection of order sets from non-Washington State hospitals, the contents of the 51 hospital order sets were all independently abstracted by two researchers (CRD and SJH) There was initial disagreement on only 189 of the 1,224 total possible elements (85% agreement). We were able to come to consensus regarding 100% of the elements after discussion of each initial difference.
Analysis
The hospital characteristics were summarized using percentages or medians (interquartile range), and were compared between quartiles of order set quality score. Domains of the quality score were summarized using medians (interquartile range), and were compared along quartiles of number of acute care hospital days. The number of ICU beds, the number of ICU bed-days, the total hospital beds and the total hospital days were all highly correlated. The number of acute care bed-days was chosen to represent hospital volume, and the number of ICU bed-days was chosen to represent ICU volume [18, 19].
We used multivariable clustered linear regression to model the association between hospital-level factors and the order set quality score. We chose hospital-level factors a priori based on the literature and included the following: teaching hospital status, CPOE status, membership in a hospital network, number of acute care bed-days, number of ICU bed-days, hospital organizational structure, critical access status, and open versus closed ICU model. Our final model clustered on order sets with common elements within a hospital network. We observed collinearity between acute care bed-days and ICU bed-days as assessed by the variance inflation factor, and ultimately excluded ICU bed-days from the final model. Finally, we performed a number of sensitivity analyses, examining alternative definitions of hospital volume and the order set quality score to test the robustness of our findings. P < 0.05 was selected to denote statistical significance. All statistical tests were two-sided and performed using STATA version 11.1 (StataCorp, College Station, TX, USA).
Results
The results of the expert survey are summarized in Table 1. There were several elements about which there was consensus that they were very important elements of a high-quality order set, including assessing and documenting both pain and sedation and titrating analgesia and sedation medications based on a patient's goal (pain) or a defined endpoint (sedation). The experts rated the analgesia and delirium elements higher than the sedation ones, as indicated by a lower mean expert survey score for the sedation elements than the analgesia or delirium elements (P < 0.01 for both).
The characteristics of the 51 eligible hospitals are summarized in Table 2. Hospital bed-days per year ranged from 3,654 to 131,881 (median 31,011). We observed that higher volume hospitals were more likely to be members of a larger hospital network (P = 0.01) and more likely to be a teaching ICU (P < 0.01). Larger ICUs were less likely to be open (P = 0.01) and less likely to be a part of a critical access hospital (P = 0.02).
We present the distribution of the analgesia, sedation and delirium quality score by network status and quartile of hospital volume in Table 3. The median total quality score was 8 (interquartile range 6 to 14; range 0 to 19) and was approximately normally distributed. Higher hospital volume was associated with higher quality scores in bivariable analysis (P < 0.01). We also observed that the association between quartile of number of ICU beds and quality score was consistent across each of the separate analgesia, sedation and delirium domains (P < 0.01 for all; Table 3).
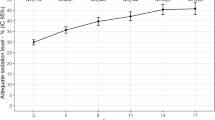
The results of the multivariable model are shown in Table 4. After adjusting for all of the a priori identified potential confounders - including critical access status, open ICU status, teaching ICU status, CPOE and organizational structure - an increased hospital volume and membership in a hospital network were both associated with a higher quality score. A 100,000 patient-day increase in hospital volume was associated with an adjusted average quality score more than seven points higher (P < 0.01). The predicted quality scores were plotted to show the association between hospital volume and adjusted quality score (Figure 2).
Predicted order set quality score across number of hospital days, adjusted for measured hospital characteristics. Predicted order set quality score across the number of hospital days for all hospitals (n = 51), adjusted for all measured hospital characteristics. Error bars correspond to 95% confidence intervals. The maximum possible score was 21.
We also observed that membership in a hospital network was independently associated with a higher order set quality score. Hospitals that were members of a hospital network had order set quality scores that were more than four points higher, on average, than hospitals who did not participate in a network (P < 0.01).
We performed several sensitivity analyses. First, to address the concern that a quality score of equally weighted elements might simply reward length, we recalculated the expert quality score, assigning a greater weight to those elements with a lower (better) mean expert score. We assigned two points to those elements with a mean score of 1.2 to 1.5, and three points to those elements with a mean score < 1.2. Assigning this greater weight did not change our results. Second, we looked at different ways to model hospital volume, including ICU bed-days, number of ICU beds and number of hospital beds and their log-transformation - the results were similar, although not all reached statistical significance in the model. Finally, we included the four hospitals without an order set, assigning them a quality score of zero, and our results were unchanged.
From a qualitative perspective, order sets varied considerably. For example, one extreme featured only limited information on propofol administration. The other extreme featured complex algorithms and if-then algorithmic statements with comprehensive pain, agitation and delirium assessment and treatment.
Discussion
We found among all Washington State hospitals that provide care for mechanically ventilated patients that greater hospital volume and membership in a hospital network were independently associated with higher quality scores for ICU analgesia, sedation and delirium order sets. To our knowledge this is the first rigorous assessment of the content of ICU analgesia, sedation and delirium order sets and the association between hospital-level factors and order set quality.
The development of order sets and their subsequent implementation is complex and poorly understood [3]. Landmark or significant clinical trials often form the foundation of clinical practice guidelines [25–28]. Ideally, hospitals incorporate the content of these guidelines or the results of the trials themselves into their routine patient care activities as a structure element of quality improvement. Yet this may not happen in a uniform manner at all hospitals. In fact, recent evidence suggests that the care provided by ICU practitioners may be less adherent to guidelines than the providers believe it to be and may lag significantly behind the publication of research findings and clinical guidelines [13, 29].
The guidelines upon which we based our order set quality score were published in 2002 and they may be outdated to some degree. However, there was expert consensus for our study in 2011 that all of the elements included in our score were at least, on average, more likely than not to be included in a high-quality ICU analgesia, sedation and delirium order set. We also included two elements (a daily spontaneous awakening trial for each eligible patient, and a paired daily spontaneous awakening trial and spontaneous breathing trial for all eligible patients) that were not included in the original guidelines but that we thought experts would probably agree ought to be included in a high-quality order set. Although new guidelines are forthcoming, our study demonstrates associations between order set quality and hospital characteristics based on currently available guidelines.
The broad distribution of the order set quality score is notable and represents a potential opportunity for quality improvement. Although we were not able to examine whether the order set quality score was associated with patient outcomes, the implementation of sedation, sepsis, ventilator-associated pneumonia and weaning protocols have all been associated with improved patient outcomes and decreased costs [30–39]. As such, we believe our findings are an important first step in improving the structure of the care environment, a step that could lead to improvements in both processes and outcomes.
There are several possible reasons why higher hospital volume was associated with higher-quality order set scores. First, there is an extensive body of work showing an association between volume and outcome in medicine [18–21]. Volume may be a proxy for resources to devote to structure and process quality improvement endeavors. Additionally, prior studies have shown that high-performing hospitals have a cooperative culture that works to improve the process of care delivery throughout the hospital [15, 40]. Cooperative culture and effective quality improvement efforts require the dedicated work of a multidisciplinary team that has the time and resources to engage in a resource-intensive enterprise [3, 14, 41]. High-volume hospitals may be more able to devote nursing, physician and pharmacy resources to foster a cooperative culture focused on quality improvement [42].
Membership in a hospital network was also associated with an increase in order set quality score. We hypothesize that hospital networks may be more likely to share protocols and order sets as well as be more likely to have the overall resources to devote to quality improvement activities, such as order set creation. Indeed, several of the hospital networks did have identical or nearly identical protocols in at least some of their hospitals. Hospital networks may also have more resources to devote to quality improvement across their broad population of hospitals, including the development and implementation of high-quality order sets. However, as the recent trial by Scales and colleagues showed, a network of hospitals for quality improvement purposes need not be constrained by common ownership, as we defined it in this study [41]. Furthermore, geographic networks, like the Keystone Project in Michigan, or participation in networks defined by common interest, like the Institute for Healthcare Improvement, have improved ICU outcomes [43, 44]. Taken together, sharing resources such as protocols and order sets across networks may represent an opportunity for maximizing quality improvement. The development of critical care networks might present an opportunity to improve structure quality elements [22, 23].
Interestingly, we did not observe an association between certain hospital characteristics and order set quality. Specifically, a hospital's ICU staffing model (open vs. closed) or the teaching status of the ICU were not independently associated with its order set quality score. This could partly be a function of our sample size of 51 hospitals or of the collinearity among these variables, as both had a bivariable association with the order set quality score.
Our study has some important limitations. First, we did not have access to patient-level or hospital-level process or outcome data and were unable to study the association between order set quality and clinical process or patient outcomes. Second, we used an expert-validated measure of order set quality, which will require external validation in future studies. Third, we weighted all elements in our quality score equally because our quality score was not designed to distinguish between the individual elements. However, specific elements (for example, a daily interruption of sedation) may be more strongly contributing to improved patient outcomes than others, and may be dependent upon other factors such as nurse-patient ratios or pharmacist staffing that we were not able to study [5, 11]. Future studies with larger sample sizes will be required to understand how alternative weighting of quality score elements affects score performance. Fourth, our study was not designed to assess the process of order set creation, a topic that merits further study. Finally, our results derive from a single state involving hospital data from 2009 and may not be generalizable to other regions. However, we did study the 13th most populated US state and included all hospitals that cared for mechanically ventilated patients.
Conclusions
Among hospitals that provide ongoing care to mechanically ventilated patients, a greater hospital volume and membership in a hospital network were both independently associated with a greater expert-validated order set quality score. Future research should focus on the relationship between order set quality scores and process and outcome measures of quality. Equally importantly, steps should be taken to improve the process of order set development and dissemination to help all hospitals obtain high-quality order sets. The development of regional critical care networks might be one way in which structure elements of quality could be improved.
Key messages
-
An expert-validated quality score was created to summarize the guideline concordance of all analgesia, sedation and delirium order sets in Washington State.
-
Order sets are a structure element of a structure-process-outcome quality improvement model.
-
Hospital volume and membership in a hospital network are both associated with a better analgesia, sedation and delirium order set quality score.
-
The creation of networks of hospitals might be one way to improve a structure element of a structure-process-outcome model of ICU quality improvement.
-
More research is needed to better understand the process of order set creation and dissemination and to better understand the relationship between order set quality scores and outcome measures of quality.
Abbreviations
- CPOE:
-
computerized physician order entry.
References
Halpern NA, Pastores SM, Greenstein RJ: Critical care medicine in the United States 1985-2000: an analysis of bed numbers, use, and costs. Crit Care Med 2004, 32: 1254-1259. 10.1097/01.CCM.0000128577.31689.4C
Jackson DL, Proudfoot CW, Cann KF, Walsh T: A systematic review of the impact of sedation practice in the ICU on resource use, costs and patient safety. Crit Care 2010, 14: R59. 10.1186/cc8956
Kollef MH, Micek ST: Using protocols to improve patient outcomes in the intensive care unit: focus on mechanical ventilation and sepsis. Semin Respir Crit Care Med 2010, 31: 19-30. 10.1055/s-0029-1246286
Girard TD, Kress JP, Fuchs BD, Thomason JW, Schweickert WD, Pun BT, Taichman DB, Dunn JG, Pohlman AS, Kinniry PA, Jackson JC: Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet 2008, 371: 126-134. 10.1016/S0140-6736(08)60105-1
Kress JP, Pohlman AS, O'Connor MF, Hall JB: Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000, 342: 1471-1477. 10.1056/NEJM200005183422002
Brook AD, Ahrens TS, Schaiff R, Prentice D, Sherman G, Shannon W, Kollef MH: Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation. Crit Care Med 1999, 27: 2609-2615. 10.1097/00003246-199912000-00001
Ely EW, Baker AM, Dunagan DP, Burke HL, Smith AC, Kelly PT, Johnson MM, Browder RW, Bowton DL, Haponik EF: Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med 1996, 335: 1864-1869. 10.1056/NEJM199612193352502
Prasad M, Christie JD, Bellamy SL, Rubenfeld GD, Kahn JM: The availability of clinical protocols in US teaching intensive care units. J Crit Care 2010, 25: 610-619. 10.1016/j.jcrc.2010.02.014
Mehta S, Burry L, Fischer S, Martinez-Motta JC, Hallett D, Bowman D, Wong C, Meade MO, Stewart TE, Cook DJ: Canadian survey of the use of sedatives, analgesics, and neuromuscular blocking agents in critically ill patients. Crit Care Med 2006, 34: 374-380. 10.1097/01.CCM.0000196830.61965.F1
Patel RP, Gambrell M, Speroff T, Scott TA, Pun BT, Okahashi J, Strength C, Pandharipande P, Girard TD, Burgess H, Dittus RS, Gordon R: Delirium and sedation in the intensive care unit: survey of behaviors and attitudes of 1384 healthcare professionals. Crit Care Med 2009, 37: 825-832. 10.1097/CCM.0b013e31819b8608
Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM, Crippen DW, Fuchs BD, Kelleher RM, Marik PE, Nasraway SA, Murray MJ, Peruzzi WT, Lumb PD: Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002, 30: 119-141. 10.1097/00003246-200201000-00020
Martin J, Heymann A, Basell K, Baron R, Biniek R, Burkle H, Dall P, Dictus C, Eggers V, Eichler I, Engelmann L, Garten L, Hartl W, Haase U, Huth R, Kessler P, Kleinschmidt S, Koppert W, Kretz FJ, Laubenthal H, Marggraf G, Meiser A, Neugebauer E, Neuhaus U, Putensen C, Quintel M, Reske A, Roth B, Scholz J, Schroder S et al: Evidence and consensus-based German guidelines for the management of analgesia, sedation and delirium in intensive care - short version. Ger Med Sci 2010, 8: Doc02.
Stoneking L, Denninghoff K, Deluca L, Keim SM, Munger B: Sepsis bundles and compliance with clinical guidelines. J Intensive Care Med 2011, 26: 172-182. 10.1177/0885066610387988
Amalberti R, Auroy Y, Berwick D, Barach P: Five system barriers to achieving ultrasafe health care. Ann Intern Med 2005, 142: 756-764.
Clemmer TP, Spuhler VJ, Berwick DM, Nolan TW: Cooperation: the foundation of improvement. Ann Intern Med 1998, 128: 1004-1009.
Morgenthaler TI, Lovely JK, Cima RR, Berardinelli CF, Fedraw LA, Wallerich TJ, Hinrichs DJ, Varkey P: Using a framework for spread of best practices to implement successful venous thromboembolism prophylaxis throughout a large hospital system. Am J Med Qual 2012, 27: 30-38. 10.1177/1062860611411518
Donabedian A: Evaluating the quality of medical care. Milbank Memorial Fund Q 1966, 33: 166-206.
Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O'Brien CR, Rubenfeld GD: Hospital volume and the outcomes of mechanical ventilation. N Engl J Med 2006, 355: 41-50. 10.1056/NEJMsa053993
Ross JS, Normand SLT, Wang Y, Ko DT, Chen J, Drye EE, Keenan PS, Lichtman JH, Bueno H, Schreiner GC: Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med 2010, 362: 1110-1118. 10.1056/NEJMsa0907130
Durairaj L, Torner JC, Chrischilles EA, Vaughan Sarrazin MS, Yankey J, Rosenthal GE: Hospital volume-outcome relationships among medical admissions to ICUs. Chest 2005, 128: 1682-1689. 10.1378/chest.128.3.1682
Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE: Hospital volume and surgical mortality in the United States. N Engl J Med 2002, 346: 1128-1137. 10.1056/NEJMsa012337
Kahn JM, Linde-Zwirble WT, Wunsch H, Barnato AE, Iwashyna TJ, Roberts MS, Lave JR, Angus DC: Potential value of regionalized intensive care for mechanically ventilated medical patients. Am J Respir Crit Care Med 2007, 177: 285-291. 10.1164/rccm.200708-1214OC
Iwashyna TJ, Christie JD, Kahn JM, Asch DA: Uncharted paths: hospital networks in critical care. Chest 2009, 135: 827-833. 10.1378/chest.08-1052
Treggiari MM, Martin DP, Yanez ND, Caldwell E, Hudson LD, Rubenfeld GD: Effect of intensive care unit organizational model and structure on outcomes in patients with acute lung injury. Am J Respir Crit Care Med 2007, 176: 685-690. 10.1164/rccm.200701-165OC
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ: Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 2001, 344: 699-709. 10.1056/NEJM200103083441001
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R: Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008, 36: 296-327. 10.1097/01.CCM.0000298158.12101.41
Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, Sexton B, Hyzy R, Welsh R, Roth G, Bander J, Kepros J, Goeschel C: An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2006, 355: 2725-2732. 10.1056/NEJMoa061115
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001, 345: 1368-1377. 10.1056/NEJMoa010307
Brunkhorst FM, Engel C, Ragaller M, Welte T, Rossaint R, Gerlach H, Mayer K, John S, Stuber F, Weiler N, Oppert M, Moerer O, Bogatsch H, Reinhart K, Loeffler M, Hartog C: Practice and perception - a nationwide survey of therapy habits in sepsis. Crit Care Med 2008, 36: 2719-2725. 10.1097/CCM.0b013e318186b6f3
Bird D, Zambuto A, O'Donnell C, Silva J, Korn C, Burke R, Burke P, Agarwal S: Adherence to ventilator-associated pneumonia bundle and incidence of ventilator-associated pneumonia in the surgical intensive care unit. Arch Surg 2010, 145: 465-470. 10.1001/archsurg.2010.69
Skrobik Y, Ahern S, Leblanc M, Marquis F, Awissi DK, Kavanagh BP: Protocolized intensive care unit management of analgesia, sedation, and delirium improves analgesia and subsyndromal delirium rates. Anesth Analg 2010, 111: 451-463. 10.1213/ANE.0b013e3181d7e1b8
Nachtigall I, Tamarkin A, Tafelski S, Deja M, Halle E, Gastmeier P, Wernecke KD, Bauer T, Kastrup M, Spies C: Impact of adherence to standard operating procedures for pneumonia on outcome of intensive care unit patients. Crit Care Med 2009, 37: 159-166. 10.1097/CCM.0b013e3181934f1b
Thiel SW, Asghar MF, Micek ST, Reichley RM, Doherty JA, Kollef MH: Hospital-wide impact of a standardized order set for the management of bacteremic severe sepsis. Crit Care Med 2009, 37: 819-824. 10.1097/CCM.0b013e318196206b
Weireter LJ Jr, Collins JN, Britt RC, Reed SF, Novosel TJ, Britt LD: Impact of a monitored program of care on incidence of ventilator-associated pneumonia: results of a longterm performance-improvement project. J Am Coll Surg 2009, 208: 700-705. 10.1016/j.jamcollsurg.2009.01.041
Afessa B, Gajic O, Keegan MT, Seferian EG, Hubmayr RD, Peters SG: Impact of introducing multiple evidence-based clinical practice protocols in a medical intensive care unit: a retrospective cohort study. BMC Emerg Med 2007, 7: 10-18. 10.1186/1471-227X-7-10
Nguyen HB, Corbett SW, Steele R, Banta J, Clark RT, Hayes SR, Edwards J, Cho TW, Wittlake WA: Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality. Crit Care Med 2007, 35: 1105-1112. 10.1097/01.CCM.0000259463.33848.3D
Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, Schorr C, Artigas A, Ramsay G, Beale R, Parker MM, Gerlach H, Reinhart K, Silva E, Harvey M, Regan S, Angus DC: The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med 2010, 38: 367-374. 10.1097/CCM.0b013e3181cb0cdc
Ferrer R, Artigas A, Levy MM, Blanco J, Gonzalez-Diaz G, Garnacho-Montero J, Ibanez J, Palencia E, Quintana M, de la Torre-Prados MV: Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA 2008, 299: 2294-2303. 10.1001/jama.299.19.2294
Devlin JW, Holbrook AM, Fuller HD: The effect of ICU sedation guidelines and pharmacist interventions on clinical outcomes and drug cost. Ann Pharmacother 1997, 31: 689-695.
Curry LA, Spatz E, Cherlin E, Thompson JW, Berg D, Ting HH, Decker C, Krumholz HM, Bradley EH: What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? Ann Intern Med 2011, 154: 384-390.
Scales DC, Dainty K, Hales B, Pinto R, Fowler RA, Adhikari NK, Zwarenstein M: A multifaceted intervention for quality improvement in a network of intensive care units: a cluster randomized trial. JAMA 2011, 305: 363-372. 10.1001/jama.2010.2000
Curtis JR, Cook DJ, Wall RJ, Angus DC, Bion J, Kacmarek R, Kane-Gill SL, Kirchhoff KT, Levy M, Mitchell PH, Moreno R, Pronovost P, Puntillo K: Intensive care unit quality improvement: a 'how-to' guide for the interdisciplinary team. Crit Care Med 2006, 34: 211-218. 10.1097/01.CCM.0000190617.76104.AC
Lipitz-Snyderman A, Steinwachs D, Needham DM, Colantuoni E, Morlock LL, Pronovost PJ: Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis. BMJ 2011, 342: d219. 10.1136/bmj.d219
Jain M, Miller L, Belt D, King D, Berwick DM: Decline in ICU adverse events, nosocomial infections and cost through a quality improvement initiative focusing on teamwork and culture change. Qual Saf Health Care 2006, 15: 235-239. 10.1136/qshc.2005.016576
Acknowledgements
The authors thank the nurses and staff of all the participating hospitals in Washington State, without whose support the study would not have been possible. This work was supported by the National Institutes of Health (Grant T32 HL07287). JRC received support through a K24 Award from the National Heart, Lung, and Blood Institute (NHLBI) (K24 HL68593).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
CRD served as the primary author, conceived and designed the study protocol, collected and analyzed all of the data, wrote the manuscript and its revisions, and approved the final version of the manuscript. SJH designed the study protocol, collected and analyzed the data, reviewed the manuscript and approved the final version of the manuscript. MMT designed the study protocol, analyzed study data, reviewed the manuscript and approved the final version of the manuscript. JRC designed the study protocol, collected and analyzed study data, reviewed the manuscript and approved the final version of the manuscript. CWS collected and analyzed the study data, reviewed the manuscript and approved the final version of the manuscript. NDY III analyzed the study data, reviewed the manuscript and approved the final version of the manuscript. VSF designed the study protocol, analyzed the data, reviewed the manuscript and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Dale, C.R., Hayden, S.J., Treggiari, M.M. et al. Association between hospital volume and network membership and an analgesia, sedation and delirium order set quality score: a cohort study. Crit Care 16, R106 (2012). https://doi.org/10.1186/cc11390
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc11390