Abstract
Introduction
Fluid overload is a clinical problem frequently related to cardiac and renal dysfunction. The aim of this study was to evaluate fluid overload and changes in serum creatinine as predictors of cardiovascular mortality and morbidity after cardiac surgery.
Methods
Patients submitted to heart surgery were prospectively enrolled in this study from September 2010 through August 2011. Clinical and laboratory data were collected from each patient at preoperative and trans-operative moments and fluid overload and creatinine levels were recorded daily after cardiac surgery during their ICU stay. Fluid overload was calculated according to the following formula: (Sum of daily fluid received (L) - total amount of fluid eliminated (L)/preoperative weight (kg) × 100). Preoperative demographic and risk indicators, intra-operative parameters and postoperative information were obtained from medical records. Patients were monitored from surgery until death or discharge from the ICU. We also evaluated the survival status at discharge from the ICU and the length of ICU stay (days) of each patient.
Results
A total of 502 patients were enrolled in this study. Both fluid overload and changes in serum creatinine correlated with mortality (odds ratio (OR) 1.59; confidence interval (CI): 95% 1.18 to 2.14, P = 0.002 and OR 2.91; CI: 95% 1.92 to 4.40, P <0.001, respectively). Fluid overload played a more important role in the length of intensive care stay than changes in serum creatinine. Fluid overload (%): b coefficient = 0.17; beta coefficient = 0.55, P <0.001); change in creatinine (mg/dL): b coefficient = 0.01; beta coefficient = 0.11, P = 0.003).
Conclusions
Although both fluid overload and changes in serum creatinine are prognostic markers after cardiac surgery, it seems that progressive fluid overload may be an earlier and more sensitive marker of renal dysfunction affecting heart function and, as such, it would allow earlier intervention and more effective control in post cardiac surgery patients.
Similar content being viewed by others
Introduction
Cardiac surgery is the surgical procedure most frequently associated with acute kidney injury (AKI) [1]. Kidney dysfunction during the perioperative period has also been associated with increased length of hospital stay [2] and with a mortality rate as high as 50% [3], regardless of the underlying disease [4]. Therefore, research has been carried out with various biomarkers in order to determine their prognostic value.
Creatinine is the most widely used marker of kidney function in patients undergoing cardiac surgery. According to Lassnigg, a small increase in serum creatinine (0 to 0.5 mg/dL) has been associated with 30-day mortality [5]. On the other hand, fluid overload has also been linked with worse prognosis in several situations, including heart failure [6, 7]. Due to this close interaction, fluid overload has been identified as a new biomarker of heart and renal function [8]. Cardio renal syndrome combines kidney dysfunction and heart failure in many clinical conditions. In kidney and in heart dysfunction, fluid overload is generally regarded as an important clinical condition [9, 10]. Fluid overload exerts greater venous pressure on the kidney, reducing kidney perfusion and glomerular filtration [11]. However, fluid overload often remains symptomless for several days until clinical symptoms set in, when treatment is usually initiated [12].
Classically, creatinine has been used to identify kidney dysfunction; however, serum creatinine may remain within the normal range until about half of the kidney function is lost [13]. Hence, clinical diagnosis of kidney dysfunction might be dangerously delayed, as might renal and heart protective procedures. Brain Natriuretic Peptide (BNP) and pro BNP are widely used biomarkers for heart failure, but when the glomerular filtration rate is less than 60 ml/minute their levels become very high, reducing their potential diagnostic accuracy [14]. However, there is no evidence of the relative importance of fluid overload detection and/or changes in serum creatinine in terms of their relative sensitivity as markers of the risk of early mortality in the postoperative period following cardiac surgery.
Materials and methods
Study design
We conducted a cohort study. This study was approved by the Ethics Committees of the Instituto de Cardiologia do Rio Grande do Sul/Fundação Universitária de Cardiologia (IC/FUC) , Porto Alegre, RS, Brazil and Universidade Federal de São Paulo (UNIFESP) , São Paulo, SP, Brazil, and registered under the numbers 4560/10 and 1781/107, respectively. Data were collected anonymously following the clinical routine, with a waiver for informed consent. We conducted a one year cohort prospective study of all patients from the Postoperative ICU who underwent surgery involving cardiopulmonary bypass (CPB) in a tertiary cardiac referral hospital, Instituto de Cardiologia do Rio Grande do Sul/Fundação Universitária de Cardiologia (IC/FUC) , beginning September 2010. Inclusion criteria were as follows: adult patients (>18 years old) submitted to the following elective surgical procedures: myocardial revascularization surgery, valve replacement surgery, valve replacement surgery plus myocardial revascularization, atrial septoplasty and ventricular septoplasty. The exclusion criteria were as follows: length of stay in the Postoperative ICU less than 24 hours, loss to follow-up and patients submitted to surgical re-intervention during the same hospital stay.
The hypothesis of this study was that fluid overload is independently related to mortality and length of stay in the ICU following cardiac surgery. Thus, the purpose of this study was to evaluate the effects of fluid overload and serum changes in serum creatinine on death and length of ICU stay and mortality in patients who underwent heart surgery, regardless of other perioperative risk factors.
We followed the STROBE statement of observational studies.
Data collection
Study population methodology
Preoperative demographic and risk indicators, intra-operative parameters and postoperative information were obtained from medical records. The preoperative variables were age (in full years), gender, weight (kg), serum creatinine (in mg/dL), EuroSCORE risk and related diseases. Serum creatinine was measured using the automated colorimetric method (Roche® Mannheim, Germany), reference values from 0.30 to 1.30 mg/dL. At our hospital, the routine creatinine analysis variation was 1.4%. Cardiac function was quantified using the ejection fraction (%) obtained by the echocardiogram. During the intra-operative period, fluid balance (fluid administered - fluid excreted - in mL) and CPB time (in minutes) were evaluated.
During postoperative follow up all available liquid intake and output data from surgery day until ICU discharge or death were included. Fluid balance (fluid administered - fluid excreted - in mL) and changes in serum creatinine were evaluated daily. Fluid management and all other interventions were determined by attending physicians and were not influenced by the study researchers. Patients were monitored from surgery until discharge or death during ICU stay period. We also evaluated the survival status and the total length of ICU stay (in days) of each patient.
To assess the impact of fluid accumulation and acute kidney dysfunction on mortality and length of ICU stay, percentage fluid accumulation and changes in serum creatinine were measured and analyzed.
For fluid accumulation, we considered the whole length of the ICU stay, including the day of surgery. We measured the 24-hour totals of fluid intake and output daily, including the trans-operative surgical period. In order to calculate daily fluid balance, the following formula was applied daily: Total fluid received (L) - Total amount of fluid eliminated (L).
In order to quantify fluid accumulation, the following formula was applied: Daily fluid accumulation sum = [Total quantity of fluid received (L) - total amount of fluid eliminated (L)]/Preoperative weight (kg) × 100. This percentage of fluid accumulation was calculated according to procedures found in previous studies [15, 16]. We used the term 'percentage of fluid accumulation' to define the percentage of cumulative fluid adjusted for body weight. We define fluid overload as ≥10% of fluid accumulation, following a previously applied classification [17, 18]. To measure changes in serum creatinine, for each patient we calculated the difference between the highest serum creatinine value observed in ICU and preoperative creatinine. To identify if the fluid accumulation might interfere with the dilution value of changes in creatinine, we used a correction factor, according to Macedo [19]: Adjusted creatinine = serum creatinine × correction factor.
We also evaluated age, EuroSCORE risk, preoperative creatinine, stratified changes in creatinine (≤0.3 mg/dL, 0.3 to 0.6mg/dL and ≥0.6 mg/dL), stratified volume accumulation (≤5%, 5% to 10%, ≥10%) and CPB time as potential confounding factors. We considered infection, pulmonary edema, bleeding, cardiac arrhythmia and death as combined events in the analysis of the study outcome. We did not analyze the temporal fluctuations of fluid overload in response to diuretics as a marker of mortality.
The study size was determined using the computer software Programs for Epidemiologists (PEPI version 4.04x). The program indicated a base of 480 patients for the 5% (α = 0.05) minimal error type I and a 20% probability error type II to estimate the OR value = 3, mortality incidence about 5% when comparing patients with the 0 to 0.5 creatinine change in relation to decreased -0.3 to 0 values, according to Lassnigg[5]. Data analysis was performed using Microsoft, Excel (Microsoft Corp, Redmond, WA, USA).
Statistical analysis
Quantitative data were described using mean and standard deviation or the median and interquartile range in the presence of skewness. Categorical data were expressed using counts and percentages. We excluded patients who died in the trans-operative period and in the first 24 hours after surgery.
Volume accumulation and changes in creatinine were transformed to Z scores to analyze the association of unit changes in both variables. We did individual Chi-square tests to identify the potential morbidities. Due to the limited number of deaths, we analyzed the combined morbidities, including mortality, and its association with potentially predictive factors using logistic regression to obtain ORs with their respective 95% CIs.
Due to the skewness, the length of ICU stay was log-transformed. For the association of volume accumulation and length of ICU stay we used a linear regression model (r Pearson coefficient). Length of ICU stay was modeled using multiple linear regression to evaluate its relationship to a number of independent factors. In this model, changes in serum creatinine were expressed as Δ creatinine, which was calculated as: Changes in creatinine = Highest serum creatinine value - Baseline creatinine. Standardized beta coefficients were used to obtain adjusted contributions of these factors in the model. Significance level was set at α = 0.05. Data were analyzed using SPSS version 18.0.
Results
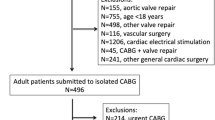
Five hundred and eighty-six patients were admitted to the postoperative ICU from September 2010 through September 2011. Eighty-four patients were excluded because they had undergone other surgical procedures, surgical reintervention or were lost to follow-up. Five hundred and two patients were prospectively studied (Figure 1).
Patients Characteristics
A total of 502 patients, with a mean age of 62.4 ± 13.3 years old, 61.4% men and 38.6% women were analyzed; baseline characteristics are shown in Table 1. We also observed that only 19.6% of the patients (96) had changes in creatinine >0.3 mg/dl during their entire length of ICU stay, and only seven patients needed dialysis; 12 patients had a neurologic disorder and 30 patients had an infection.
Death, percentage variation of fluid overload and serum changes in serum creatinine
Over the 12-month period, 17 patients died during their ICU stay in the postoperative period (3.38%). When we analyzed the association of fluid accumulation and changes in serum creatinine by Z score variables with mortality, we observed that fluid overload and changes in serum creatinine were significantly associated with mortality. For fluid overload, we found a significant increase of 1.59 in the OR (CI 1.18 to 2.14, P = 0.002) for death at each Z score in fluid overload. For creatinine, we found a significant increase of 2.91 in the OR for death (CI 1.92 to 4.40, P<0.001) at every creatinine Z score change (Table 2). We were unable to separately analyze the death event adjusted to confounding factors because the number of deaths was very small in this period of observation. Thus, we studied this relationship including combined events, such as death, infection, cardiac arrhythmia, bleeding and pulmonary edema. Logistic regression analysis of combined events and association variables revealed a significant increase in combined events when the change in serum creatinine was 0.3 to 0.6 mg/dl (OR 2.4; CI 1.24 to 4.65; P = 0.009), and ≥0.6 mg/dl (OR 6.17; CI 2.83 to 13.45;
P <0.001). We also found a significant and independent increase in combined events when the fluid accumulation increased 10% (OR 4.43; CI: 2.08 to 9.14; P <0.001) (Table 3). We also calculated this model with creatinine values adjusted to volume accumulation, as described by Macedo et al. [19] and found similar results for changes in creatinine (OR 2.5; CI 1.31 to 4.83, P = 0.005 to changes of 0.3 to 0.6 mg/dL and OR 6.30; CI 2.92 to 13.58, P <0.001 to changes in creatinine ≥0.6 mg/dL).
We have to emphasize that none of the patients who died had a decreased creatinine level. Considering this observation, we did not analyze the group separately. It was possible to demonstrate that of the 157 patients who had decreased creatinine levels, only four (2.5%) presented fluid overload ≥10%.
Length of ICU stay and percentage variation of fluid overload
We found a moderate to strong magnitude relationship between the length of ICU stay and fluid overload (r = 0.57, P <0.001). We also found that patients who survived after four days in the ICU had no fluid accumulation (Figure 2). After analyzing the independent contribution of all parameters, we observed that a 10% fluid overload was substantially greater than 0.1 mg/dL changes in serum creatinine, in accounting for ICU stay. In this analysis, time on CPB, EuroSCORE, preoperative creatinine and age were not found to be associated with length of ICU stay (Table 4).
Length of stay, fluid accumulation, changes in serum creatinine and mortality. Black circle: non-survival with changes in serum creatinine <0.6 mg/dL; White circle: survival with changes in serum creatinine <0.6mg/dL; Black square: non-survival with changes in serum creatinine ≥0.6 mg/dL; White square: survival with changes in serum creatinine ≥0.6 mg/dL.
Outcome of fluid overload, length of stay in ICU, change in serum creatinine and death
We found a moderate association between fluid accumulation and length of ICU stay (r = 0.57, P <0.001). As the majority of patients stayed only two days in the ICU, (median = 2, 1 to 3), we analyzed these patients in relation to the upper percentile (P75). We found that only 66 patients stayed more than four days in the ICU (P75). The outcome of fluid overload is time related (Figure 2). We found that ten patients died within the first four days in the ICU (P75), 71.4% with fluid accumulation ≥10%; we also found that all seven patients (100%) who died after four days in the ICU had fluid accumulation ≥10%. No patient with less than 10% fluid accumulation died during this period. When we considered the change in serum creatinine, we found that eight patients (75%) with creatinine variation ≥ 0.6mg/dL died in the first four days, and six patients (85.7%) died after a four-day stay in the ICU.
Discussion
Our analysis describes the importance of fluid overload and changes in serum creatinine during the perioperative period following cardiac surgery as early markers of intra-ICU mortality and longer ICU stay.
To our knowledge, this study is the first to evaluate systematically fluid overload after cardiac surgery. Our most interesting finding is that the 10% fluid overload also seemed to have a significant and independent effect on the combined events, including death. This 10% fluid overload effect was observed in another study that investigated acute kidney dysfunction [17]. Sutherland et al., in a recent pediatric study into acute kidney dysfunction, reported a 3% increase in mortality for each 1% increase in fluid accumulation [20].
An inverse relationship between fluid accumulation and survival has been reported in several other conditions, such as in the perioperative period [21–23], acute pulmonary edema [8, 24], pulmonary injury [25], sepsis [18, 23, 26] and acute kidney injury (AKI) [27], chronic renal failure [28, 29] and decompensated heart failure [30]. When we studied the impact of all the adjusted variables on combined events, we found that the changes in serum creatinine (≥0.3 mg/dL) and fluid accumulation (≥10%) were the variables most significantly associated with mortality (Table 2). The changes in serum creatinine values and the association with mortality seems to corroborate Lassnigg's findings [5]. These results were previously observed in the perioperative period as well as in critically ill populations, because fluid overload has been associated with impaired wound healing and prolonged mechanical ventilation [31, 32]. Hypervolemia also seems to be associated with cardiac edema, leading to myocyte injury [33] and malignant ventricular tachyarrhythmia [34].
We also found a significant and independent association between fluid overload and length of ICU stay, similar to those previously found in patients undergoing general surgery [35], with cardio renal syndrome and acute kidney diseases [7]. In our data, fluid overload seemed to play a much greater role than creatinine in the length of ICU stay (Table 4).
The association between classic risk factors, such as CPB [36], EuroSCORE [37] and preoperative renal dysfunction, and a higher rate of postoperative complications and longer length of hospital stay has been widely reported in the medical literature [38]. However, when we analyzed the independent contribution of variables to account for the length of ICU stay, we found that only fluid overload and changes in serum creatinine were related to length of ICU stay.
The early identification of fluid overload is essential to establish adequate management in cardiac patients, since this is regarded as the most important hemodynamic factor in the worsening of renal function in patients with congestive heart failure [39]. When cardiac dysfunction occurs, it is not unusual to find that renal function suddenly worsens [40] and that the adjustment of volume and sodium is out of control [41]. Fluid overload may be associated with myocardial edema, which, together with inflammatory changes and the activation of the renin-angiotensin system, increases the consumption of myocardial oxygen, leading to an unfavorable clinical situation [42]. It may also alter renal function due to diminished perfusion secondary to venous congestion [13, 43], so reducing glomerular filtration [44].
Once renal insufficiency occurs in the setting of heart failure, the prognosis becomes poor. There is a gap in the knowledge regarding the clear distinction between pre-renal and established acute renal failure associated with decreasing compensatory mechanisms and subclinical episodes of heart and kidney dysfunction. Filling this gap is critical for the adequate management of the afflicted patients [45].
Serum creatinine levels can also undergo changes during the postoperative period after cardiac surgery due to extracorporeal circulation and hemodilution [7]. However, in our data, we found no relationship between the decreased change in creatinine and mortality, because no patient in this group died, in contrast to what was observed by Lassnigg [5].
Due the fact that only 66 patients stayed more than four days in the ICU, in our data it was impossible to detect an expressive temporal profile. However, we found none of the surviving patients had fluid overload four days after cardiac surgery. Interaction between the heart and kidneys is intense. It is also well established that renal and cardiac function are closely related to fluid control and maladjustment in one of the organs may trigger an alteration in the other [46]. Fluid accumulation may have a bidirectional association with renal dysfunction [24] and may account for this rather direct relationship between heart and kidney, the cardio renal syndrome [24]. In order to establish adequate cross-talk between them, it is necessary to maintain an adequate blood volume and hemodynamic stability [30]. This is so important that several authors have identified fluid overload as a new biomarker of dysfunction of the cardio renal syndrome [41].
Study limitations
The present study has some limitations. This is a prospective and observational study, prone to bias of selection and residual confounding. Our population included patients with and without sepsis, the number of deaths was small (17 patients), and few patients required dialysis (seven patients). Also, the percentage time of the fluid overload was not considered in this study, a factor which, as is known, may interfere in the length of hospitalization and mortality [15]. Therefore, it is also difficult to distinguish precisely whether the excess of fluid balance is the cause or the result of postoperative complications. It also remains unclear whether fluid restriction or the use of diuretics after cardiac surgery reduces morbidity and mortality [23].
We did not analyze the mechanisms involved in the development of fluid overload, including the contribution of volume infusion of fluids, the particular type of fluid administered or the absence of response to diuretics. These points need to be addressed in further studies.
Other measurements associated with fluid overload, such as central venous pressure or pulmonary capillary pressure, and pro BNP measures could be performed. In fact, these parameters were obtained from several patients, but not in a systematic protocol. Therefore, we did not analyze and present the related data. However, our results strongly indicate that fluid accumulation control and changes in serum creatinine together may represent valuable tools to detect a population with a higher cardiovascular risk among patients treated in a 'real life' scenario.
Conclusions
In summary, we showed a significant and independent association between fluid overload and changes in serum creatinine in relation to combined events of death, infection, bleeding, arrhythmia and pulmonary edema in postoperative cardiac surgery. We also found that fluid overload was the variable most related to length of stay in postoperative care following cardiac surgery.
As such, our findings contribute towards expanding the knowledge regarding this still unclear field of the functional interaction between the kidneys and the heart. Further randomized and controlled studies are needed to define whether early fluid overload detection would be an unrecognized form of initial renal failure and a target treatment to lower mortality associated with cardiac surgery.
Fluid therapy is widely endorsed for the resuscitation of critically ill patients across a range of conditions. Yet, the approach to fluid therapy is subject to substantial variation in clinical practice. Emerging evidence shows that choice, timing and amount of fluid therapy affect outcome. Further studies would need to focus on these aspects of fluid therapy by means of larger, more rigorous and blinded controlled trials.
Key messages
-
Fluid overload is independently associated with combined events in post operative cardiac surgery.
-
Increase in serum creatinine is independently associated with combined events in post operative cardiac surgery.
-
Fluid overload is substantially more effective in accounting for ICU stay than 0.1mg/dL changes in serum creatinine.
-
The early identification of fluid overload is essential to establish adequate management in cardiac patients.
Abbreviations
- AKI:
-
acute kidney injury
- b:
-
angular coefficient obtained in a multiple linear regression model
- CI:
-
confidence interval
- CPB:
-
cardiopulmonary bypass
- Δ variation:
-
(final value - initial value)
- P25 to P75:
-
interquartile range.
References
Hoste EA, Kellum JA, Katz NM, Rosner MH, Haase M, Ronco C: Epidemiology of acute kidney injury. Contrib Nephrol 2010, 165: 1-8.
Mangano CM, Diamondstone LS, Ramsay JG, Aggarwal A, Herskowitz A, Mangano DT: Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. The Multicenter Study of Perioperative Ischemia Research Group. Ann Intern Med 1998, 128: 194-203.
Chertow GM, Lazarus JM, Christiansen CL, Cook EF, Hammermeister KE, Grover F, Daley J: Preoperative renal risk stratification. Circulation 1997, 95: 878-884. 10.1161/01.CIR.95.4.878
Loef BG, Epema AH, Smilde TD, Henning RH, Ebels T, Navis G, Stegeman CA: Immediate postoperative renal function deterioration in cardiac surgical patients predicts in-hospital mortality and long-term survival. J Am Soc Nephrol 2005, 16: 195-200.
Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, Hiesmayr M: Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol 2004, 15: 1597-1605. 10.1097/01.ASN.0000130340.93930.DD
Cotter G, Metra M, Milo-Cotter O, Dittrich HC, Gheorghiade M: Fluid overload in acute heart failure--re-distribution and other mechanisms beyond fluid accumulation. Eur J Heart Fail 2008, 10: 165-169. 10.1016/j.ejheart.2008.01.007
Cruz DN, Soni S, Slavin L, Ronco C, Maisel A: Biomarkers of cardiac and kidney dysfunction in cardiorenal syndromes. Contrib Nephrol 2010, 165: 83-92.
Bagshaw SM, Cruz DN: Fluid overload as a biomarker of heart failure and acute kidney injury. Contrib Nephrol 2010, 164: 54-68.
Hillege HL, Girbes AR, de Kam PJ, Boomsma F, de Zeeuw D, Charlesworth A, Hampton JR, van Veldhuisen DJ: Renal function, neurohormonal activation, and survival in patients with chronic heart failure. Circulation 2000, 102: 203-210. 10.1161/01.CIR.102.2.203
Bagshaw SM, Brophy PD, Cruz D, Ronco C: Fluid balance as a biomarker: impact of fluid overload on outcome in critically ill patients with acute kidney injury. Critical Care 2008, 12: 169. 10.1186/cc6948
Schrier RW: Water and sodium retention in edematous disorders: role of vasopressin and aldosterone. Am J Med 2006, 119: S47-53. 10.1016/j.amjmed.2006.05.007
Gheorghiade M, Follath F, Ponikowski P, Barsuk JH, Blair JE, Cleland JG, Dickstein K, Drazner MH, Fonarow GC, Jaarsma T, Jondeau G, Sendon JL, Mebazaa A, Metra M, Nieminen M, Pang PS, Seferovic P, Stevenson LW, van Veldhuisen DJ, Zannad F, Anker SD, Rhodes A, McMurray JJ, Filippatos G, European Society of Cardiology; European Society of Intensive Care Medicine: Assessing and grading congestion in acute heart failure: a scientific statement from the Acute Heart Failure Committee of the Heart Failure Association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. Eur J Heart Fail 2010, 12: 423-433. 10.1093/eurjhf/hfq045
Soni SS, Ronco C, Katz N, Cruz DN: Early diagnosis of acute kidney injury: the promise of novel biomarkers. Blood Purif 2009, 28: 165-174. 10.1159/000227785
Iwanaga Y, Miyazaki S: Heart failure, chronic kidney disease, and biomarkers--an integrated viewpoint. Circ J 2010, 74: 1274-1282. 10.1253/circj.CJ-10-0444
Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL: Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int 2009, 76: 422-427. 10.1038/ki.2009.159
Goldstein SL, Currier H, Graf C, Cosio CC, Brewer ED, Sachdeva R: Outcome in children receiving continuous venovenous hemofiltration. Pediatrics 2001, 107: 1309-1312. 10.1542/peds.107.6.1309
Gillespie RS, Seidel K, Symons JM: Effect of fluid overload and dose of replacement fluid on survival in hemofiltration. Pediatr Nephrol 2004, 19: 1394-1399. 10.1007/s00467-004-1655-1
Bouchard J, Mehta RL: Fluid balance issues in the critically ill patient. Contrib Nephrol 2010, 164: 69-78.
Macedo E, Bouchard J, Soroko SH, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL: Fluid accumulation, recognition and staging of acute kidney injury in critically-ill patients. Critical Care 2010, 14: R82. 10.1186/cc9004
Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, Hackbarth R, Somers MJ, Baum M, Symons JM, Flores FX, Benfield M, Askenazi D, Chand D, Fortenberry JD, Mahan JD, McBryde K, Blowey D, Goldstein SL: Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis 2010, 55: 316-325. 10.1053/j.ajkd.2009.10.048
Brandstrup B, Tonnesen H, Beier-Holgersen R, Hjortso E, Ording H, Lindorff-Larsen K, Rasmussen MS, Lanng C, Wallin L, Iversen LH Gramkow CS, Okholm M, Blemmer T, Svendsen PE, Rottensten HH, Thage B, Riis J, Jeppesen IS, Teilum D, Christensen AM, Graungaard B, Pott F, Danish Study Group on Perioperative Fluid Therapy: Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg 2003, 238: 641-648. 10.1097/01.sla.0000094387.50865.23
Kleespies A, Thiel M, Jauch KW, Hartl WH: Perioperative fluid retention and clinical outcome in elective, high-risk colorectal surgery. Int J Colorectal Dis 2009, 24: 699-709. 10.1007/s00384-009-0659-5
Wei S, Tian J, Song X, Chen Y: Association of perioperative fluid balance and adverse surgical outcomes in esophageal cancer and esophagogastric junction cancer. Ann Thorac Surg 2008, 86: 266-272. 10.1016/j.athoracsur.2008.03.017
Ronco C, Maisel A: Volume overload and cardiorenal syndromes. Congest Heart Fail 2010,16(Suppl 1):Si-iv. quiz Svi
Sakr Y, Vincent JL, Reinhart K, Groeneveld J, Michalopoulos A, Sprung CL, Artigas A, Ranieri VM: High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest 2005, 128: 3098-3108. 10.1378/chest.128.5.3098
Hilton AK, Bellomo R: Totem and taboo: fluids in sepsis. Crit Care 2011, 15: 164. 10.1186/cc10247
Selewski DT, Cornell TT, Lombel RM, Blatt NB, Han YY, Mottes T, Kommareddi M, Kershaw DB, Shanley TP, Heung M: Weight-based determination of fluid overload status and mortality in pediatric intensive care unit patients requiring continuous renal replacement therapy. Intensive Care Med 2011, 37: 1166-1173. 10.1007/s00134-011-2231-3
Uchino S, Bellomo R, Kellum JA, Morimatsu H, Morgera S, Schetz MR, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-Van Straaten HM, Ronco C, Beginning and Ending Supportive Therapy for the Kidney (B.E.S.T. Kidney) Investigators Writing Committee: Patient and kidney survival by dialysis modality in critically ill patients with acute kidney injury. Int J Artif Organs 2007, 30: 281-292.
Bonello M, House AA, Cruz D, Asuman Y, Andrikos E, Petras D, Strazzabosco M, Ronco F, Brendolan A, Crepaldi C, Nalesso F, Ronco C: Integration of blood volume, blood pressure, heart rate and bioimpedance monitoring for the achievement of optimal dry body weight during chronic hemodialysis. Int J Artif Organs 2007, 30: 1098-1108.
Damman K, Voors AA, Hillege HL, Navis G, Lechat P, van Veldhuisen DJ, Dargie HJ: Congestion in chronic systolic heart failure is related to renal dysfunction and increased mortality. Eur J Heart Fail 2010, 12: 974-982. 10.1093/eurjhf/hfq118
Bundgaard-Nielsen M, Secher NH, Kehlet H: 'Liberal' vs. 'restrictive' perioperative fluid therapy--a critical assessment of the evidence. Acta Anaesthesiol Scand 2009, 53: 843-851. 10.1111/j.1399-6576.2009.02029.x
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL: Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 2006, 354: 2564-2575.
Peacock WF 4th, De Marco T, Fonarow GC, Diercks D, Wynne J, Apple FS, Wu AH: Cardiac troponin and outcome in acute heart failure. N Engl J Med 2008, 358: 2117-2126. 10.1056/NEJMoa0706824
Ip JE, Cheung JW, Park D, Hellawell JL, Stein KM, Iwai S, Liu CF, Lerman BB, Markowitz SM: Temporal associations between thoracic volume overload and malignant ventricular arrhythmias: a study of intrathoracic impedance. J Cardiovasc Electrophysiol 2011, 22: 293-299. 10.1111/j.1540-8167.2010.01924.x
Cooperman LH, Price HL: Pulmonary edema in the operative and postoperative period: a review of 40 cases. Ann Surg 1970, 172: 883-891. 10.1097/00000658-197011000-00014
Swaminathan M, Phillips-Bute BG, Conlon PJ, Smith PK, Newman MF, Stafford-Smith M: The association of lowest hematocrit during cardiopulmonary bypass with acute renal injury after coronary artery bypass surgery. Ann Thorac Surg 2003, 76: 784-791. discussion 792 10.1016/S0003-4975(03)00558-7
Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, Cortina J, David M, Faichney A, Gabrielle F, Gams E, Harjula A, Jones MT, Pintor PP, Salamon R, Thulin L: Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg 1999, 15: 816-822. discussion 822-823 10.1016/S1010-7940(99)00106-2
Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW: Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 2005, 16: 3365-3370. 10.1681/ASN.2004090740
Ponikowski P, Ronco C, Anker SD: Cardiorenal syndromes--recommendations from clinical practice guidelines: the cardiologist's view. Contrib Nephrol 2010, 165: 145-152.
Metra M, Nodari S, Parrinello G, Bordonali T, Bugatti S, Danesi R, Fontanella B, Lombardi C, Milani P, Verzura G, Cotter G, Dittrich H, Massie BM, Dei Cas L: Worsening renal function in patients hospitalised for acute heart failure: clinical implications and prognostic significance. Eur J Heart Fail 2008, 10: 188-195. 10.1016/j.ejheart.2008.01.011
Mebazaa A: Congestion and cardiorenal syndromes. Contrib Nephrol 2010, 165: 140-144.
Jessup M, Costanzo MR: The cardiorenal syndrome: do we need a change of strategy or a change of tactics? J Am Coll Cardiol 2009, 53: 597-599. 10.1016/j.jacc.2008.11.012
Amann K, Wanner C, Ritz E: Cross-talk between the kidney and the cardiovascular system. J Am Soc Nephrol 2006, 17: 2112-2119. 10.1681/ASN.2006030204
Ljungman S, Laragh JH, Cody RJ: Role of the kidney in congestive heart failure. Relationship of cardiac index to kidney function. Drugs 1990, 39: 10-21. 10.2165/00003495-199000394-00004
Macedo E, Mehta R: Prerenal azotemia in congestive heart failure. Contrib Nephrol 2010, 164: 79-87.
Ronco C: Cardiorenal syndromes: definition and classification. Contrib Nephrol 2010, 164: 33-38.
Acknowledgements
This is an initial study on volume accumulation produced together at four research centers. The authors include cardiologists, nephrologists, intensivists, basic research doctors, students and nurses. The major subject of interest is the cardio renal syndrome, and its clinical and physiological understanding.
The authors would like to thank Fapesp and Procad/Capes as well as Vania Naomi Hirakata for her statistical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AS and MCI conceived the study, participated in study design, prepared data, performed statistical analysis and wrote the paper. LVS, CRB, WRM and JRV participated in study design, prepared data, collected data and wrote the paper. EMCP, RE, LA and FCC contributed in the writing and critical appraisal of the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Stein, A., de Souza, L.V., Belettini, C.R. et al. Fluid overload and changes in serum creatinine after cardiac surgery: predictors of mortality and longer intensive care stay. A prospective cohort study. Crit Care 16, R99 (2012). https://doi.org/10.1186/cc11368
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc11368