Abstract
Introduction
In the emergency setting, focused cardiac ultrasound has become a fundamental tool for diagnostic, initial emergency treatment and triage decisions. A new ultra-miniaturized pocket ultrasound device (PUD) may be suited to this specific setting. Therefore, we aimed to compare the diagnostic ability of an ultra-miniaturized ultrasound device (Vscan™, GE Healthcare, Wauwatosa, WI) and of a conventional high-quality echocardiography system (Vivid S5™, GE Healthcare) for a cardiac focused ultrasonography in patients admitted to the emergency department.
Methods
During 4 months, patients admitted to our emergency department and requiring transthoracic echocardiography (TTE) were included in this single-center, prospective and observational study. Patients underwent TTE using a PUD and a conventional echocardiography system. Each examination was performed independently by a physician experienced in echocardiography, unaware of the results found by the alternative device. During the focused cardiac echocardiography, the following parameters were assessed: global cardiac systolic function, identification of ventricular enlargement or hypertrophy, assessment for pericardial effusion and estimation of the size and the respiratory changes of the inferior vena cava (IVC) diameter.
Results
One hundred fifty-one (151) patients were analyzed. With the tested PUD, the image quality was sufficient to perform focused cardiac ultrasonography in all patients. Examination using PUD adequately qualified with a very good agreement global left ventricular systolic dysfunction (κ = 0.87; 95%CI: 0.76-0.97), severe right ventricular dilation (κ = 0.87; 95%CI: 0.71-1.00), inferior vena cava dilation (κ = 0.90; 95%CI: 0.80-1.00), respiratory-induced variations in inferior vena cava size in spontaneous breathing (κ = 0.84; 95%CI: 0.71-0.98), pericardial effusion (κ = 0.75; 95%CI: 0.55-0.95) and compressive pericardial effusion (κ = 1.00; 95%CI: 1.00-1.00).
Conclusions
In an emergency setting, this new ultraportable echoscope (PUD) was reliable for the real-time detection of focused cardiac abnormalities.
Similar content being viewed by others
Introduction
The widespread use of emergency echocardiography provides valuable assistance in the management of acutely ill patients, allowing fast and accurate assessment of cardiac function and the ability to determine the cause of hemodynamic disorders [1–4]. Because standard echocardiographic equipment may be heavy and difficult to handle, hand-carried ultrasound (US) devices have been developed for bedside use, facilitating the growth of point-of-care ultrasonography [5]. When used by adequately trained intensivists, these devices have a well-demonstrated reliability and a widespread availability and rapid diagnostic capability, ideally suited for the emergency setting [6–8]. However, confusion between focused and comprehensive US among the many types of hand-carried US devices must be avoided [9–11]. Pocket devices are not able to perform a complete echocardiographic examination but can provide accurate diagnoses based on two-dimensional imaging for effective bedside screening. They can be used as an extension of the physical examination in various clinical settings, underlining the concept of personal echoscope. They have been shown to directly guide and alter clinical management and have a therapeutic impact equivalent to that of standard echocardiography [12–15].
Recently, a new generation of ultra-miniaturized US devices - the Vscan™ (GE Healthcare, Wauwatosa, WI, USA) - has been developed. Its true portability, ease of use, and relative low cost make this device adequately suited for routine use in strategies of focused US examination. At present, only a few studies evaluating its feasibility and clinical usefulness have been published [16–20]. However, none of them has compared its diagnostic accuracy with that of standard echocardiography in emergency settings. Thus, the main purpose of this study was to evaluate the recently available pocket US device (PUD) in comparison with standard transthoracic echocardiography (TTE) for focused cardiac ultrasonography in the emergency setting.
Materials and methods
Patients
During a 4-month period (from February to May 2011), all patients who were admitted to our emergency department and who required a TTE were included, unless two investigators were both unavailable. The following variables were collected at enrolment: demographic data, reason for admission (medical or surgical), medical history, cardio-respiratory status, Simplified Acute Physiology Score II (SAPS II), and indication for performing the US exam. Indications for TTE were left to the discretion of the attending physician but should be focused on a clinical problem or evaluation of patients with cardiac history (Table 1). This prospective, single-center, and observational study was approved by the local ethics committee (Comité de Protection des Personnes Sud-Ouest et Outre Mer III, Bordeaux, France; protocol DC 2011/07), which waived the need for informed consent. Patients or next of kin were orally informed of the goal and design of the study.
Investigators and equipment
Each eligible patient was subsequently examined by two different echocardiography systems: the tested PUD (Vscan™; GE Healthcare) and a conventional echographic system (Vivid S5™; GE Healthcare). The new PUD, designed to be operated with one hand, consisted of a 135 × 73 × 28 mm unit connected to a 1.7 to 3.8 MHz phased array transducer (total weight of 390 g). Autonomy, battery fully charged, was 1 hour. The technical capabilities of the PUD allowed diagnosis based only on two-dimensional imaging and allowed possible adjustments of global gain and depth. Color flow mode was available, but there were no advanced features such as the M-mode or pulsed and continuous Doppler mode. Images could be frozen and stored for review.
Each examination was performed independently by two intensivists - MB and CC, who are experienced in echocardiography and have level II competence (as assessed by the European Association of Echocardiography) in general adult TTE - in random order within a 30-minute time frame. Both investigators were provided with medical history and clinical and paraclinical exams of the patient but were unaware of the results found by the alternative echocardiography device.
Data acquisition
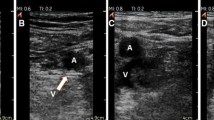
As recommended for focused cardiac examination in emergency patients [9], parameters recorded by using the PUD were the assessment of global cardiac systolic function, the identification of ventricular enlargement or hypertrophy, the assessment for a pericardial effusion, and the visual estimation of the size and respiratory changes of the inferior vena cava (IVC) diameter. Each clinical question was recorded by using a qualitative approach considered positive, negative, or undetermined (no response when the imaging quality or the device technology failed to provide a definite diagnosis). Only left ventricular ejection fraction (LVEF) was estimated by using a quantitative and visual approach.
For the purpose of this study, the systematic examination using conventional TTE was considered the reference diagnostic method to measure each variable, as recommended by the European Association of Echocardiography [21]. LVEF was calculated by the Simpson method unless it was impossible to obtain and then estimate the ejection fraction by visual approach. Hypertrophy was noticed when the thickness of the interventricular septum exceeded 13 mm, and dilation was noticed when the maximal end-diastolic antero-posterior diameter of the LV cavity was above 55 mm. Right ventricular (RV) dilation was defined by a diastolic ventricular ratio of greater than 0.6 when measured in the apical four-chamber view [22]. IVC diameter was measured proximally in the subcostal view between the right atrial junction and the superior hepatic vein, and a dilation corresponded to an end-expiratory diameter of greater than 23 mm [23]. IVC was considered collapsic if its diameter presented at least a 50% inspiratory decrease in patients with spontaneous ventilation [24]. Pericardial effusion, detected by an echo-free space, was considered compressive in the case of a collapse of the right cavities or respiratory variations of Doppler flow or both.
All echocardiography was interpreted online at bedside. For each US examination, the three standard transthoracic windows (parasternal, apical, and subcostal) were systematically screened. The examination was considered inconclusive when image quality was considered low, data were missing, or not accessible by the visual approach alone. In this case, the corresponding clinical question was not addressed. When all data were collected, duration of the study was measured for each method.
Statistical analysis
Results are expressed as mean ± standard deviation or median (25% to 75% interquartile range) as appropriate. The results of the PUD and conventional TTE were compared in each patient. Results obtained with the conventional TTE were considered the reference. LVEFs obtained with the two devices were compared by using linear correlation and Bland and Altman analysis [25]. The ability of the PUD to discriminate the severity of the global LV systolic dysfunction (normal was greater than 50%, moderately depressed was 30% to 50%, and severely depressed was less than 30%) was tested by using Cohen's κ coefficient, and 95% confidence intervals (CIs) were calculated [26]. For each other clinical question, data were recorded in order to calculate the sensitivity, specificity, and positive and negative predictive values. The agreement between the clinical responses provided by the two devices was assessed by using Cohen's κ coefficient, and 95% CIs were calculated [26]. Kappa values of less than 0.2 were interpreted as slight, 0.21 to 0.4 as fair, 0.41 to 0.6 as moderate, 0.61 to 0.8 as substantial, and 0.81 to 1.00 as very good agreement [27]. The duration of the exam using the PUD or the conventional approach was compared by using the Wilcoxon test. A P value of less than 0.05 was considered statistically significant.
Results
During the study period, 182 patients admitted to our department underwent a TTE. Among them, 31 patients were not enrolled in the study, because of the absence of at least one investigator. Finally, 151 patients were included. The main characteristics of these patients are shown in Table 1, and indications for TTE are shown in Table 2.
The ability of the PUD to diagnose clinical problems is shown in Table 3, and sensibility, specificity, positive and negative predictive values, and κ coefficient are compared with those of a standardized examination. LVEFs obtained with PUD and with conventional echocardiography were not significantly different (58% ± 13% versus 59% ± 13%, respectively, P > 0.05) and were correlated (r = 0.79, 95% CI 0.72 to 0.84, P < 0.0001) (Figure 1). Comparison between LVEFs obtained with PUD and with conventional TTE showed a mean bias of 1.4% and limits of agreement of -12.2% to 14.9% (Figure 1). The intra-observer reproducibility percentages were 6.6% ± 3.3% using the standard TTE and 2.6% ± 4.2% using the PUD. The inter-observer reproducibility percentages were 6.9% ± 4.3% using standard TTE and 5.5% ± 3.9% using the PUD. Furthermore, examination using PUD adequately qualified the severity of the global LV systolic dysfunction (normal, moderately depressed, or severely depressed) in 134 patients (κ = 0.87, 95% CI 0.76 to 0.97). The presence (or absence) of LV dilation or hypertrophy was adequately classified by PUD, and there was substantial agreement (κ > 0.60). Compared with conventional TTE, PUD adequately identified RV dilation, RV dysfunction, pericardium effusion, and tamponade with good to excellent agreement (range of κ values was 0.63 to 1). Examination using PUD adequately identified the IVC size: empty (κ = 0.86, 95% CI 0.77 to 0.94) or dilated (κ = 0.90, 95% CI 0.80 to 1.00). Respiratory-induced variations in IVC size were well evaluated in spontaneous breathing (κ = 0.84, 95% CI 0.71 to 0.98).
Comparison of left ventricular ejection fractions (LVEFs) obtained by two devices. LVEFs were compared by using (a) linear correlation and (b) Bland and Altman analysis. A conventional high-quality echocardiography system was considered the reference. PUD, pocket ultrasound device; SD, standard deviation.
Image quality was good enough to address all clinical questions estimated by visual approach alone without missing data. Compared with conventional TTE exam, the exam using PUD was significantly shorter: 420 seconds (300 to 600) versus 180 seconds (165 to 300), respectively (P < 0.0001).
Discussion
Our study suggested that, in an emergency setting, the new PUD was reliable for the detection of focused cardiac abnormalities with a good agreement when compared with a last-generation conventional US device. Our results are in accordance with those of previous studies evaluating the diagnostic capabilities of this PUD in other clinical situations. In 100 cardiologic patients in a cardiological setting, Lafitte and colleagues [19] demonstrated that PUD showed good concordance of diagnostic capability with that of standard full-feature echocardiographic instruments. Prinz and Voigt [28], who studied 349 consecutive patients from an echocardiography lab, showed a very high image quality, excellent LVEF and LV dimension evaluations, and a good detection of pericardial effusion. In a perioperative setting, Frederiksen and colleagues [18] confirmed that PUD was well suited for performing a focus-assessed TTE in a surgery setting with a good image quality. More recently, Amiel and colleagues [16] demonstrated that PUD was able to assess LVEF with a good agreement in 94 critically ill patients.
In emergency or critical care settings, focused US allows findings to be directly correlated with the clinical situation, thereby offsetting the inherent limitations of the physical exam with real-time cardiovascular imaging [29]. Moreover, limited TTE not only provides new information on cardiac function but also may change the initial management of intensive care patients with a similar therapeutic impact thanks to the use of a portable US system compared with a standard US, despite its lower overall diagnostic capacity [13, 15]. By increasing the number of clinical diagnoses, PUD could prove cost-effective by decreasing the number of medical errors, providing a more efficient real-time diagnosis, and reducing the use of unnecessary routine US examinations [17, 30]. The capability and simplicity of this new PUD make it ideally suited for bedside use in emergency settings, providing time-sensitive assessment to assist physicians in the diagnosis of cardiovascular diseases in addition to the physical examination [31, 32]. In fact, it embodies the concept of the visual stethoscope by Galderisi and colleagues [33], who demonstrated the relevant additional diagnostic power of pocket-size devices in addition to the physical examination. Thanks to a semi-quantitative approach, the device can be used as an echoscopic tool, differing from echocardiography in the lack of quantitative and dedicated measurement tools (that is, area and volume calculations), the absence of flow Doppler capacity, and the inability to provide an extensive report. Recently, a consensus statement by the American Society of Echocardiography/American College of Emergency Physicians emphasized the complementary role of focused cardiac US to that of a more comprehensive echocardiography [9]. The semi-quantitative evaluation of cardiac function by focused US cannot replace a more complete echocardiographic examination but, in some cases, may specify its indications without delaying the immediate management of severe cardiac dysfunction as suspected by the clinical examination.
The smallness of these devices does not preclude the need for full training. Ultrasonography is a user-dependent technology, and as usage spreads, clinicians' skills need to be ensured and the benefits of its appropriate use need to be defined. Most of the recommendations that define skills required in critical care or emergency US also insist on the necessary training required to perform an appropriate examination for a specific purpose [1, 4, 34]. Furthermore, to apply a systematic diagnostic and therapeutic protocol based on US, all emergency physicians have to be trained in echocardiography, and completing this training can be challenging.
The present study has several limitations. First, the way data were collected was different between the two techniques: we used quantitative measurements with classic US and qualitative assessment with PUD. Consequently, the difference in time consumption was probably explained by the realization of time-specific measures for the evaluation of diameters and ejection fractions with the reference device. Similarly, intra-observer variability assessment was biased by the visual approach, as illustrated by lower intra-observer but similar inter-observer variability. However, the systematic measures using the reference diagnostic method were necessary to confirm that a visual approach alone may be sufficient [35]. Second, we found that the image quality of PUD was sufficient for focused echocardiography, but this does not mean that image quality was similar between the two devices. Third, both PUD and classic TTE were performed by operators experienced in echocardiography and therefore sensitized to a visual assessment of semi-quantitative parameters. We cannot evaluate the relevance of this device if used by an examiner who received minimal training in US. Finally, we evaluated an ultra-miniaturized PUD for focused cardiac ultrasonography in emergency patients but did not assess the impact of this evaluation in terms of diagnostic strategy, treatment, or prognosis.
Conclusions
We showed that, in an emergency setting, a new PUD is reliable for the detection of focused cardiac abnormalities with a good agreement when compared with a last-generation conventional US device. The former device cannot replace a more comprehensive echocardiographic evaluation but can trigger a more precise request without delaying the management of acutely ill patients. However, further methodologically rigorous studies are needed to assess patient-centered outcomes for point-of-care US.
Key messages
-
The image quality of the tested pocket ultrasound device was sufficient to perform focused cardiac ultrasonography in an emergency setting.
-
This new pocket ultrasound device is reliable for the detection of focused cardiac abnormalities by a semi-quantitative visual analysis with good agreement.
-
Our results should not be extrapolated to comprehensive echocardiography.
-
The training necessary to achieve a sufficient level of competence remains to be determined.
Abbreviations
- CI:
-
confidence interval
- IVC:
-
inferior vena cava
- LV:
-
left ventricular
- LVEF:
-
left ventricular ejection fraction
- PUD:
-
pocket ultrasound device
- RV:
-
right ventricular
- TTE:
-
transthoracic echocardiography
- US:
-
ultrasound.
References
American College of Emergency Physicians: Emergency ultrasound guidelines. Ann Emerg Med 2009, 53: 550-570.
Beaulieu Y: Bedside echocardiography in the assessment of the critically ill. Crit Care Med 2007, 35: S235-249. 10.1097/01.CCM.0000260673.66681.AF
Nelson BP, Melnick ER, Li J: Portable ultrasound for remote environments, Part I: Feasibility of field deployment. J Emerg Med 2011, 40: 190-197. 10.1016/j.jemermed.2009.09.006
Price S, Via G, Sloth E, Guarracino F, Breitkreutz R, Catena E, Talmor D: Echocardiography practice, training and accreditation in the intensive care: document for the World Interactive Network Focused on Critical Ultrasound (WINFOCUS). Cardiovasc Ultrasound 2008, 6: 49. 10.1186/1476-7120-6-49
Moore CL, Copel JA: Point-of-care ultrasonography. N Engl J Med 2011, 364: 749-757. 10.1056/NEJMra0909487
Atar S, Feldman A, Darawshe A, Siegel RJ, Rosenfeld T: Utility and diagnostic accuracy of hand-carried ultrasound for emergency room evaluation of chest pain. Am J Cardiol 2004, 94: 408-409. 10.1016/j.amjcard.2004.04.052
Spevack DM, Spevack DM, Tunick PA, Kronzon I: Hand carried echocardiography in the critical care setting. Echocardiography 2003, 20: 455-461. 10.1046/j.1540-8175.2003.03083.x
Vignon P, Frank MB, Lesage J, Mucke F, Francois B, Normand S, Bonnivard M, Clavel M, Gastinne H: Hand-held echocardiography with Doppler capability for the assessment of critically-ill patients: is it reliable? Intensive Care Med 2004, 30: 718-723. 10.1007/s00134-003-2128-x
Labovitz AJ, Noble VE, Bierig M, Goldstein SA, Jones R, Kort S, Porter TR, Spencer KT, Tayal VS, Wei K: Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr 2010, 23: 1225-1230. 10.1016/j.echo.2010.10.005
Mondillo S, Giannotti G, Innelli P, Ballo PC, Galderisi M: Hand-held echocardiography: its use and usefulness. Int J Cardiol 2006, 111: 1-5. 10.1016/j.ijcard.2005.07.002
Seward JB, Douglas PS, Erbel R, Kerber RE, Kronzon I, Rakowski H, Sahn LD, Sisk EJ, Tajik AJ, Wann S: Hand-carried cardiac ultrasound (HCU) device: recommendations regarding new technology. A report from the Echocardiography Task Force on New Technology of the Nomenclature and Standards Committee of the American Society of Echocardiography. J Am Soc Echocardiogr 2002, 15: 369-373. 10.1067/mje.2002.123026
Egan M, Ionescu A: The pocket echocardiograph: a useful new tool? Eur J Echocardiogr 2008, 9: 721-725. 10.1093/ejechocard/jen177
Manasia AR, Nagaraj HM, Kodali RB, Croft LB, Oropello JM, Kohli-Seth R, Leibowitz AB, DelGiudice R, Hufanda JF, Benjamin E, Goldman ME: Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth 2005, 19: 155-159. 10.1053/j.jvca.2005.01.023
Scholten C, Rosenhek R, Binder T, Zehetgruber M, Maurer G, Baumgartner H: Hand-held miniaturized cardiac ultrasound instruments for rapid and effective bedside diagnosis and patient screening. J Eval Clin Pract 2005, 11: 67-72. 10.1111/j.1365-2753.2004.00506.x
Vignon P, Chastagner C, Francois B, Martaille JF, Normand S, Bonnivard M, Gastinne H: Diagnostic ability of hand-held echocardiography in ventilated critically ill patients. Crit Care 2003, 7: R84-91. 10.1186/cc2360
Amiel JB, Grumann A, Lheritier G, Clavel M, Francois B, Pichon N, Dugard A, Marin B, Vignon P: Assessment of left ventricular ejection fraction using an ultrasonic stethoscope in critically ill patients. Crit Care 2012, 16: R29. 10.1186/cc11198
Cardim N, Fernandez Golfin C, Ferreira D, Aubele A, Toste J, Cobos MA, Carmelo V, Nunes I, Oliveira AG, Zamorano J: Usefulness of a new miniaturized echocardiographic system in outpatient cardiology consultations as an extension of physical examination. J Am Soc Echocardiogr 2011, 24: 117-124. 10.1016/j.echo.2010.09.017
Frederiksen CA, Juhl-Olsen P, Larsen UT, Nielsen DG, Eika B, Sloth E: New pocket echocardiography device is interchangeable with high-end portable system when performed by experienced examiners. Acta Anaesthesiol Scand 2010, 54: 1217-1223. 10.1111/j.1399-6576.2010.02320.x
Lafitte S, Alimazighi N, Reant P, Dijos M, Zaroui A, Mignot A, Lafitte M, Pillois X, Roudaut R, DeMaria A: Validation of the smallest pocket echoscopic device's diagnostic capabilities in heart investigation. Ultrasound Med Biol 2011, 37: 798-804. 10.1016/j.ultrasmedbio.2011.02.010
Reant P, Dijos M, Arsac F, Mignot A, Cadenaule F, Aumiaux A, Jimenez C, Dufau M, Prevost A, Pillois X, Fort P, Roudaut R, Lafitte S: Validation of a new bedside echoscopic heart examination resulting in an improvement in echo-lab workflow. Arch Cardiovasc Dis 2011, 104: 171-177. 10.1016/j.acvd.2011.01.003
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S, Spencer KT, St John Sutton M, Stewart W: Recommendations for chamber quantification. Eur J Echocardiogr 2006, 7: 79-108. 10.1016/j.euje.2005.12.014
Jurcut R, Giusca S, La Gerche A, Vasile S, Ginghina C, Voigt JU: The echocardiographic assessment of the right ventricle: what to do in 2010? Eur J Echocardiogr 2010, 11: 81-96. 10.1093/ejechocard/jep234
Weyman A: Principles and Practice of Echocardiography. 2nd edition. Philadelphia, PA: Lea & Febiger; 1994.
Kircher BJ, Himelman RB, Schiller NB: Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol 1990, 66: 493-496. 10.1016/0002-9149(90)90711-9
Bland JM, Altman DG: Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1: 307-310.
Cohen J: A coefficient of agreement for nominal scales. Educational and Psychological Measurement 1960, 20: 37-46. 10.1177/001316446002000104
Landis JR, Koch GG: The measurement of observer agreement for categorical data. Biometrics 1977, 33: 159-174. 10.2307/2529310
Prinz C, Voigt JU: Diagnostic accuracy of a hand-held ultrasound scanner in routine patients referred for echocardiography. J Am Soc Echocardiogr 2011, 24: 111-116. 10.1016/j.echo.2010.10.017
Kobal SL, Tolstrup K, Luo H, Neuman Y, Miyamoto T, Mirocha J, Naqvi TZ, Siegel RJ: Usefulness of a hand-carried cardiac ultrasound device to detect clinically significant valvular regurgitation in hospitalized patients. Am J Cardiol 2004, 93: 1069-1072. 10.1016/j.amjcard.2003.12.066
Galasko GI, Henein M: Direct access echocardiography. Int J Cardiovasc Imaging 2006, 22: 29-31. 10.1007/s10554-005-0721-5
Filly RA: Is it time for the sonoscope? If so, then let's do it right! J Ultrasound Med 2003, 22: 323-325.
Roelandt JR: Ultrasound stethoscopy: a renaissance of the physical examination? Heart 2003, 89: 971-973. 10.1136/heart.89.9.971
Galderisi M, Santoro A, Versiero M, Lomoriello VS, Esposito R, Raia R, Farina F, Schiattarella PL, Bonito M, Olibet M, de Simone G: Improved cardiovascular diagnostic accuracy by pocket size imaging device in non-cardiologic outpatients: the NaUSiCa (Naples Ultrasound Stethoscope in Cardiology) study. Cardiovasc Ultrasound 2010, 8: 51. 10.1186/1476-7120-8-51
Expert Round Table on Ultrasound in ICU: International expert statement on training standards for critical care ultrasonography. Intensive Care Med 2011, 37: 1077-1083.
Sievers B, Kirchberg S, Franken U, Puthenveettil BJ, Bakan A, Trappe HJ: Visual estimation versus quantitative assessment of left ventricular ejection fraction: a comparison by cardiovascular magnetic resonance imaging. Am Heart J 2005, 150: 737-742. 10.1016/j.ahj.2004.11.017
Acknowledgements
The authors thank Ray Cooke for assistance with manuscript preparation. Only departmental funds were used for this study. No external funds were obtained.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MB helped to conceive the study and design the trial, supervised the conduct of the trial and data collection, and helped to perform all echocardiography, to provide statistical advice on study design, to analyze the data, and to draft the manuscript. CC helped to conceive the study and design the trial, to perform all echocardiography, to provide statistical advice on study design, to analyze the data, and to draft the manuscript. GJ helped to conceive the study and design the trial. NM, FD, and PR helped to undertake recruitment of participating patients. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Biais, M., Carrié, C., Delaunay, F. et al. Evaluation of a new pocket echoscopic device for focused cardiac ultrasonography in an emergency setting. Crit Care 16, R82 (2012). https://doi.org/10.1186/cc11340
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc11340