Abstract
Introduction
Recent data have suggested that patient admission during intensive care unit (ICU) morning bedside rounds is associated with less favorable outcome. We undertook the present study to explore the association between morning round-time ICU admissions and hospital mortality in a large Canadian health region.
Methods
A multi-center retrospective cohort study was performed at five hospitals in Edmonton, Canada, between July 2002 and December 2009. Round-time ICU admission was defined as occurring between 8 and 11:59 a.m. Multivariable logistic regression analysis was used to explore the association between round-time admission and outcome.
Results
Of 18,857 unique ICU admissions, 2,055 (10.9%) occurred during round time. Round-time admissions were more frequent in community hospitals compared with tertiary hospitals (12.0% vs. 10.5%; odds ratio [OR] 1.16; 95% CI, 1.05-1.29, P < 0.004) and from the ward compared with the emergency department (ED) or operating theater (17.5% vs. 9.2%; OR 2.1; 95% CI, 1.9-2.3, P < 0.0001). Round-time admissions were more often medical than surgical (12.6% vs. 6.6%; OR 2.06; 95% CI, 1.83-2.31, P < 0.0001), had more comorbid illness (11.9% vs. 10.5%; OR 1.15; 95% CI, 1.04-1.27, P < 0.008) and higher APACHE II score (22.2 vs. 21.3, P < 0.001), and were more likely to have a primary diagnosis of respiratory failure (37.0% vs. 31.3%, P < 0.001) or sepsis (11.1% vs. 9.0%, P = 0.002). Crude ICU mortality (15.3% vs. 11.6%; OR 1.38; 95% CI, 1.21-1.57, P < 0.0001) and hospital mortality (23.9% vs. 20.6%; OR 1.21; 95% CI, 1.09-1.35, P < 0.001) were higher for round-time compared with non-round-time admissions. In multi-variable analysis, round-time admission was associated with increased ICU mortality (OR 1.19, 95% CI, 1.03-1.38, P = 0.017) but was not significantly associated with hospital mortality (OR 1.02; 95% CI, 0.90-1.16, P = 0.700). In the subgroup admitted from the ED, round-time admission showed significantly higher ICU mortality (OR 1.54; 95% CI, 1.21-1.95; P < 0.001) and a trend for higher hospital mortality (OR 1.22; 95% CI, 0.99-1.51, P = 0.057).
Conclusions
Approximately 1 in 10 patients is admitted during morning rounds. These patients are more commonly admitted from the ward and are burdened by comorbidities, are non-operative, and have higher illness severity. These patients admitted during morning rounds have higher observed ICU mortality but no difference in hospital mortality.
Similar content being viewed by others
Introduction
Bedside clinical rounds are an integral component for both patient care and medical education. Intensivists in academic medical centers and many metropolitan/community-based hospitals often must balance evidence-based and high-quality patient care with appropriate supervision of trainees, including medical students, residents, and fellows.
The acuity of illness in the first few hours after patient admission to the intensive care unit (ICU) is most often used to prognosticate the clinical course on the basis of the premise that these patients are most physiologically unstable during this period [1]. This represents a crucial phase for resuscitation, often requiring active and diligent bedside multi-disciplinary care. The concept of early, prompt, and aggressive intervention to reverse physiologic instability has been shown to improve outcomes across a range of critically ill states, including sepsis [2], ischemic stroke [3], cardiac arrest [4, 5], and acute myocardial infarction [6]. However, in the morning, the ICU team is often focused on multi-disciplinary bedside clinical and teaching rounds. New ICU admissions occurring during this period may disrupt workflow and, in selected circumstances, negatively impact the care of other ICU patients. Likewise, patients admitted during morning rounds may have their transfer to the ICU or the initiation of timely diagnostic, supportive, and therapeutic measures (or both) delayed [7].
Recently, in a retrospective cohort study, Afessa and colleagues [8] found an increase in mortality for critically ill patients admitted to the ICU during morning bedside clinical rounds. These data imply that system-level factors, such as hospital/ICU organizational structure, have the potential to negatively impact patient outcome. This retrospective study, however, was performed at a single academic institution and may not be widely generalizable.
Accordingly, to further explore the hypothesis that ICU admission during morning rounds portends risk of worse clinical outcome, we performed a multi-center cohort study at five teaching hospitals in a large Canadian health region. The objective was to investigate the effect of round-time ICU admissions on ICU and hospital mortality in critically ill patients.
Materials and methods
The study was approved by the Health Research Ethics Board at the University of Alberta prior to commencement. The requirement for individual informed consent was waived. The reporting of this study follows the STROBE (strengthening the reporting of observational studies in epidemiology) guideline [9].
Study design and setting
This was a multi-center retrospective observational cohort study performed at five teaching-affiliated hospitals in Edmonton, Canada, between 1 July 2002 and 31 December 2009. Edmonton has an estimated population of 730,000 and a metropolitan population of 1,034,945. The three metropolitan/community hospitals are the Grey Nuns Community Hospital (GNH) (eight beds and one daytime/one night-time intensivist), Misericordia Community Hospital (six beds and one daytime/one night-time intensivist), and Sturgeon General Hospital (six beds and one daytime/one night-time intensivist). These three hospitals all have mixed medical/surgical ICUs. The GNH is the regional referral center for all major vascular surgery. The two tertiary hospitals are the Royal Alexandria Hospital (RAH) (22 beds and two daytime intensivist teams and one night-time intensivist) and University of Alberta Hospital (UAH) (30 beds and three daytime intensivist teams and one night-time intensivist). Both of these tertiary hospitals have mixed medical/surgical/trauma ICUs. The RAH is a level II trauma center, and the UAH is a level I trauma center and the regional referral center for all non-cardiac solid-organ transplantation. Bedside morning rounds in each ICU were attended to by one or more consultant intensivists, residents, and/or bedside clinicians and by a multi-disciplinary team consisting of registered nurses, respiratory therapists, pharmacists, dieticians, and physiotherapists. Critical care fellows rotate between the ICUs, and the majority of their rotations occur at the two tertiary hospital sites.
Study population
All consecutive adult (at least 18 years old) patients admitted to one of the five hospitals' participating ICUs were eligible. If a patient had multiple ICU admissions during a single hospitalization, only the first admission was included for analysis. Patients discharged from the ICU less than 24 hours after admission and those with missing data on vital status were excluded.
Study definitions
Round-time admission was defined as an ICU admission occurring between 8 and 11:59 a.m., corresponding to the routine time during which multi-disciplinary and teaching bedside clinical rounds are performed at all participating ICUs. Non-round-time admission was defined as an ICU admission occurring between noon and 7:59 a.m. ICU admission source was classified as emergency department (ED), operating room/emergency post-operative status, operating room/elective post-operative status, transfer from other institutions, or in-hospital ward transfer. Severity of illness was defined according to the Acute Physiology and Chronic Health Evaluation II (APACHE II) score [10]. Hepatic failure was defined as having documented cirrhosis by histology or elevated bilirubin and international normalized ratio attributed to liver disease. Immunosuppression was defined as having received cytotoxic medication or steroids or both within the 7 days preceding ICU admission. Chronic respiratory disease was defined as a documented need for home oxygen therapy or severe exercise restriction or both. Chronic kidney disease was defined as chronic dialysis therapy. Hematologic cancer was defined as having pathologically confirmed lymphoma, leukemia, or multiple myeloma. Congestive heart failure was defined as having symptoms at minimal exertion. Surgical status was defined as having had an operative procedure within 7 days of ICU admission.
Data sources
We used an ICU-specific clinical/administrative database maintained by the regional Division of Critical Care Medicine, termed the Minimal Data Set database, which routinely captures demographic, diagnostic, clinical, physiologic, and outcome data for all ICU admissions to the five participating hospitals. We extracted data on demographics, ICU admission source/time, post-operative status, comorbidities, admission diagnoses, necessity for invasive mechanical ventilation, APACHE II score, ICU and hospital duration of stay, and ICU and hospital mortality.
Statistical analysis
The primary exposure of interest was time of ICU admission (round-time versus non-round-time). The primary outcome measure was hospital mortality. The secondary outcome measures were ICU mortality and ICU and hospital lengths of stay. Continuous normally or near-normally distributed data are reported as means with standard deviations and compared by Student t test. Non-normally distributed continuous data are reported as medians and interquartile ranges and were compared by Mann-Whitney U test. Categorical variables were compared by using the chi-squared test. Separate customized multi-variable logistic regression models with ICU or hospital mortality as dependent variable and round-time admission as an independent variable were created and were adjusted for demographics, comorbidity, APACHE II score, use of mechanical ventilation, surgical status, admission source, and primary diagnostic category, study year, and center. Data are reported as odds ratios (ORs) with 95% confidence intervals (CIs). Data were evaluated for multi-colinearity. Model calibration and fit were assessed by the area under the receiver operating characteristic curve (AUR ROC) and the Pearson goodness-of-fit (GoF) test, respectively. All statistical analyses were two-sided, and a P value of less than 0.05 was considered significant. Statistical analyses were conducted by using Intercooled Stata Release 10 (StataCorp LP, College Station, TX, USA).
Results
There were 24,829 ICU admissions during the study period. After exclusion of 1,732 (7.0%) because of repeat admissions, 3,841 (15.5%) for an ICU stay of less than 24 hours, and 399 (1.6%) because of missing data on vital status, the study cohort consisted of 18,857 unique ICU admissions (75.9%). Of these, 2,055 (10.9%) occurred during round time, from 8 to 11:59 a.m., and 16,802 (89.1%) during non-round time, from noon to 7:59 p.m. The two tertiary hospitals accounted for the majority of admissions (73.4%) during the study period (Table 1). However, round-time admissions were more common in the community ICUs when compared with the tertiary ICUs (12.0% versus 10.5%, OR 1.16, 95% CI 1.05 to 1.29, P = 0.004).
Patient characteristics
Patients admitted at round time were more likely to be admitted from the hospital ward when compared with the ED or operating theater (17.5% versus 9.2%, OR 2.10, 95% CI 1.90 to 2.30, P < 0.0001) (Table 2). Round-time admissions were more often medical than surgical (12.6% versus 6.6%, OR 2.06, 95% CI 1.83 to 2.31, P < 0.0001). Round-time patients also had greater comorbid illness (11.9% versus 10.5%, OR 1.15, 95% CI 1.04 to 1.27, P < 0.008), and those with any comorbidity were more likely to have a higher number of conditions (4 versus 3, P = 0.01). Specifically, round-time patients had higher prevalences of hematologic malignancies (P = 0.005), chronic kidney disease (P = 0.04), and immunosuppression (P = 0.002) when compared with non-round-time admissions. Acuity of illness was higher for round-time admissions compared with non-round-time (APACHE II score of 22.2 versus 21.3, P < 0.001). Round-time admissions were more likely to have primary diagnoses of respiratory failure (37.0% versus 31.3%, P < 0.001) and sepsis (11.1% versus 9.0%, P = 0.002) and were less likely to have diagnoses of cardiovascular (11.5% versus 13.8%, P = 0.004) or gastrointestinal (12.1% versus 17.6%, P < 0.001) failure in comparison with non-round-time admissions, respectively.
Clinical outcomes
Crude ICU mortality (15.3% versus 11.6%, OR 1.38, 95% CI 1.21 to 1.57, P < 0.0001) and hospital mortality (23.9% versus 20.6%, OR 1.21, 95% CI 1.09 to 1.35, P < 0.001) were significantly greater for ICU admissions occurring during round time compared with non-round time (Table 3). There were no significant differences in ICU or hospital lengths of stay between round-time and non-round-time admissions.
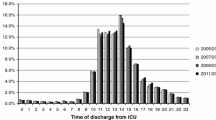
After covariate adjustment, round-time admission remained associated with higher odds of ICU death (OR 1.19, 95% CI 1.03 to 1.38, P = 0.017; AUC ROC 0.818, 95% CI 0.809 to 0.827, GoF, P = 0.260) but was not significantly associated with hospital mortality (OR 1.02, 95% CI 0.90 to 1.16, P = 0.700; AUC ROC 0.798, 95% CI 0.791 to 0.806, GoF, P = 0.996) (Tables 4 and 5). There was variability in the adjusted OR for ICU mortality when stratified by study year, and a significantly lower OR for death was observed during the period of 2006-2007 (OR 0.85, 95% CI 0.74 to 0.99, P = 0.035).
Sensitivity analysis
In a further exploratory analysis, higher adjusted ICU mortality for round-time compared with non-round-time admissions was seen among the community ICU (OR 1.43, 95% CI 1.09 to 1.89, P = 0.009) when compared with the tertiary ICU subgroup (Additional file 1). However, there remained no significant association between morning round admission and hospital mortality stratified by community or tertiary subgroups (Additional file 2). The subgroup referred from the ED for ICU admission showed a higher adjusted OR for ICU death (OR 1.54, 95% CI 1.21 to 1.95, P < 0.001) and a trend toward higher hospital death (OR 1.22, 95% CI 0.99 to 1.51, P = 0.057) for round-time admission compared with non-round-time admission (Additional file 3). The subgroup admitted during the years 2006/2007 showed a higher adjusted OR for ICU (OR 1.47, 95% CI 1.11 to 1.95, P = 0.008) and hospital death (OR 1.30, 95% CI 1.03 to 1.64, P = 0.028) relative to other years for round-time compared with non-round-time admission (Additional file 4).
Discussion
We performed a large, multi-center, retrospective cohort study to evaluate the association between admission to the ICU during morning bedside rounds and mortality.
Summary of major findings
We found that approximately 1 in 10 ICU admissions occurs during the period of morning bedside clinical rounds. We found that round-time admissions more commonly occurred in community compared with tertiary hospital ICUs. We also found that patients admitted during round time had higher likelihoods to be transferred from the ward and to be medical (non-operative) and were characterized by a higher burden of comorbid illness and greater illness severity. Likewise, we found that the distribution of admission diagnoses differed; patients arriving during morning rounds were more likely to have respiratory failure and septic diagnoses. Although we showed that patients admitted during morning rounds had higher crude ICU and hospital mortality, the association with ICU mortality remained after adjustment in multi-variable analysis; however, there was no significant association with hospital mortality. Finally, in additional sensitivity analyses, we found a higher mortality associated with admissions occurring during morning rounds for those occurring in community hospitals and for patients referred from the ED.
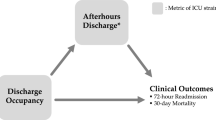
Comparison with previous studies
A number of observational studies have evaluated the association between time of ICU admission and hospital mortality and have shown inconsistent findings [11–17]. In data from a large Canadian health region, ICU admission 'after hours' was independently predictive of higher in-hospital mortality [11]. Alternatively, a recent systematic review suggested that weekend, but not night-time, ICU admissions were associated with an increased risk for death [18], implying that differences in ICU organizational structure on weekends and 'after hours' may negatively impact patient outcomes. In a recent French multi-center study, ICU admissions during the weekend or during 'after hours' were not associated with an increased risk of death, whereas ICU discharge 'after hours' independently predicted a worse clinical outcome [19].
To date, only one large retrospective study has investigated an association between ICU admission during morning rounds and mortality: Afessa and colleagues [8] examined 49,844 unique admissions to a single tertiary/academic center encompassing four closed ICUs (two surgical, one medical, and one multi-disciplinary) over the course of a 13-year period and used prospectively collected clinical/administrative data from a local quality/outcomes database. In that study, round-time admission was more narrowly defined (in comparison with our study) as occurring between 8 and 10:59 a.m.; patients admitted 2 hours before or after this time were excluded. Round-time admissions accounted for 7.2% of all ICU admissions; given that we used a slightly more liberal definition, this figure is similar to the 10.9% observed in our study. Patients admitted during round time were similarly characterized by higher illness severity and were more likely to be non-operative in comparison with non-round-time admissions. In that study, round-time admission was associated with a significantly higher hospital mortality (16.2% versus 8.8%, adjusted OR 1.32, 95% CI 1.18 to 1.48, P < 0.001). The investigators were also able to show significant declines in mortality for round-time admissions over the course of the study (21.3% in 1994/1995 to 13.6% in 2006/2007) and an association with modifications to the ICU organizational model (change from one- to two-intensivist team, P < 0.001; in-house intensivist coverage, P < 0.001; introduction of a rapid response team, P < 0.001; however, all of these changes occurred very late in the study).
We believe that our data extend the findings of this study, in particular by enabling the evaluation of multiple hospital ICUs, including community-based teaching hospitals, and more extensive covariate adjustment. Our data suggest that ICU admission during morning rounds portends an increased risk for ICU death, and while no statistical difference for in-hospital mortality, certainly fails to suggest that admission during this time leads to improved clinical outcomes, when theoretically all available staff (intensivists, trainees, full complement of multi-disciplinary team members) are present in the ICU.
We believe that the observed differences between community and tertiary hospital ICUs with respect to morning round-time admissions are novel. We observed the proportion of total ICU admissions during round time to be higher in the community as compared with those of tertiary hospital ICUs (12.0% versus 10.5%, P = 0.004). This was furthermore associated with an adjusted ICU mortality that was 44% higher and a non-significant increase in hospital mortality, despite comparable patient characteristics and illness severity.
In addition, we found that ICU admission from the ED during morning rounds was associated with greater ICU mortality and a trend for greater hospital mortality. This generates speculation about the influence of system-level factors associated with delays in transfer of critically ill patients from the ED, such as ICU capacity/bed availability, organizational structure, and/or personnel/staffing models, whereby selected patients may be 'held' in the ED during 'after hours' until an ICU bed is available the following morning. In a large observational study using the Project IMPACT database, Chalfin and colleagues [7] found that 2.1% of critically ill patients admitted from the ED to the ICU experienced delays in transfer, defined as a stay in the ED of more than 6 hours. Whereas patients with delayed ED transfer to the ICU had characteristics similar to those of patients without a delayed transfer, the former had a longer median hospital stay (7.0 versus 6.0 days, P < 0.001) and greater hospital mortality (17.4% versus 12.9%, P < 0.001).
Study limitations and strengths
Our study has several limitations. First, although our study is large and multi-centric and represents all ICUs in a large Canadian health region, it is a retrospective analysis of prospectively collected data and is observational and thus is potentially predisposed to bias and residual confounding. However, the evaluation of health services, such as how the timing of admission to the ICU impacts patient course and outcomes, cannot feasibly be evaluated in a clinical trial setting. Accordingly, we believe that there is value in replicating observational studies of this nature to assess for consistency and generalizability across studies. Second, despite our adjustment of those variables available, we recognize that we may have omitted additional variables of prognostic importance. Third, we estimated that the routine time during which morning bedside rounds occur at all sites was between 8 and 11:59 a.m. and further recognize that this may have varied at times between and within sites during the study period and depended on additional unrecorded intangible factors.
Areas of future research
We believe that these observations suggest that system-level factors (such as the relative timing of ICU admission and organizational structure) in addition to patient-level factors (such as comorbidity, illness severity, and admission diagnosis) can have an important modifying effect on the outcome for critically ill patients. However, although our study adds to our current understanding of these patient-system interactions, further confirmatory studies that focus on the relative timing of admission in community/metropolitan hospitals, the impact of delayed transfers from the ED to the ICU, and their interaction with ICU organizational structure and capacity are needed.
Conclusions
In summary, patients admitted during morning rounds have important differences in baseline characteristics, disposition, and illness severity in comparison with those admitted during other periods of the day. Moreover, in comparison with the latter, the former have a significantly higher ICU mortality but have similar hospital mortality. Importantly, ICU admission during morning rounds was associated with higher mortality in community hospitals and in patients referred from the ED. These data argue for a need to critically evaluate the patient-system factors associated with ICU admission, such as those that occur during morning bedside rounds and that have the potential to impact patient outcome.
Key messages
-
Approximately 1 in 10 intensive care unit (ICU) admissions occurs during morning bedside clinical rounds.
-
Patients admitted during morning rounds had higher likelihoods to be transferred from the ward and to be medical (non-operative) and were characterized by a higher burden of comorbid illness and greater illness severity.
-
Patients admitted during morning rounds had higher crude and adjusted ICU mortality.
-
There was no significant association between morning rounds and hospital mortality after adjustment in multi-variable analysis.
-
We found a higher mortality associated with admissions occurring during morning rounds for those occurring in community hospitals and for patients referred from the emergency department.
Abbreviations
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation II
- AUR ROC:
-
area under the receiver operating characteristic curve
- CI:
-
confidence interval
- ED:
-
emergency department
- GNH:
-
Grey Nuns Community Hospital
- GoF:
-
goodness-of-fit
- ICU:
-
intensive care unit
- OR:
-
odds ratio
- RAH:
-
Royal Alexandria Hospital
- UAH:
-
University of Alberta Hospital.
References
Moreno RP, Metnitz PG, Almeida E, Jordan B, Bauer P, Campos RA, Iapichino G, Edbrooke D, Capuzzo M, Le Gall JR, SAPS 3 Investigators: SAPS 3--from evaluation of the patient to evaluation of the intensive care unit. Part 2: development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med 2005, 31: 1345-1355. 10.1007/s00134-005-2763-5
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001, 345: 1368-1377. 10.1056/NEJMoa010307
Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, Albers GW, Kaste M, Marler JR, Hamilton SA, Tilley BC, Davis SM, Donnan GA, Hacke W, ECASS, ATLANTIS, NINDS and EPITHET rt-PA Study Group, Allen K, Mau J, Meier D, del Zoppo G, De Silva DA, Butcher KS, Parsons MW, Barber PA, Levi C, Bladin C, Byrnes G: Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 2010, 375: 1695-1703. 10.1016/S0140-6736(10)60491-6
Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K: Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 2002, 346: 557-563. 10.1056/NEJMoa003289
Hypothermia after Cardiac Arrest Study Group: Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002, 346: 549-556.
Nallamothu B, Fox KA, Kennelly BM, Van de Werf F, Gore JM, Steg PG, Granger CB, Dabbous OH, Kline-Rogers E, Eagle KA, GRACE Investigators: Relationship of treatment delays and mortality in patients undergoing fibrinolysis and primary percutaneous coronary intervention. The Global Registry of Acute Coronary Events. Heart 2007, 93: 1552-1555.
Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP, DELAY-ED study group: Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med 2007, 35: 1477-1483. 10.1097/01.CCM.0000266585.74905.5A
Afessa B, Gajic O, Morales IJ, Keegan MT, Peters SG, Hubmayr RD: Association between ICU admission during morning rounds and mortality. Chest 2009, 136: 1489-1495. 10.1378/chest.09-0529
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative: Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007, 335: 806-808. 10.1136/bmj.39335.541782.AD
Knaus WA, Draper EA, Wagner DP, Zimmerman JE: APACHE II: a severity of disease classification system. Crit Care Med 1985, 13: 818-829. 10.1097/00003246-198510000-00009
Laupland KB, Shahpori R, Kirkpatrick AW, Stelfox HT: Hospital mortality among adults admitted to and discharged from intensive care on weekends and evenings. J Crit Care 2008, 23: 317-324. 10.1016/j.jcrc.2007.09.001
Morales IJ, Peters SG, Afessa B: Hospital mortality rate and length of stay in patients admitted at night to the intensive care unit. Crit Care Med 2003, 31: 858-863. 10.1097/01.CCM.0000055378.31408.26
Luyt CE, Combes A, Aegerter P, Guidet B, Trouillet JL, Gibert C, Chastre J: Mortality among patients admitted to intensive care units during weekday day shifts compared with 'off' hours. Crit Care Med 2007, 35: 3-11. 10.1097/01.CCM.0000249832.36518.11
Sheu CC, Tsai JR, Hung JY, Yang CJ, Hung HC, Chong IW, Huang MS, Hwang JJ: Admission time and outcomes of patients in a medical intensive care unit. Kaohsiung J Med Sci 2007, 23: 395-404. 10.1016/S0257-5655(07)70003-2
Uusaro A, Kari A, Ruokonen E: The effects of ICU admission and discharge times on mortality in Finland. Intensive Care Med 2003, 29: 2144-2148. 10.1007/s00134-003-2035-1
Wunsch H, Mapstone J, Brady T, Hanks R, Rowan K: Hospital mortality associated with day and time of admission to intensive care units. Intensive Care Med 2004, 30: 895-901. 10.1007/s00134-004-2170-3
Meynaar IA, van der Spoel JI, Rommes JH, van Spreuwel-Verheijen M, Bosman RJ, Spronk PE: Off hour admission to an intensivist-led ICU is not associated with increased mortality. Crit Care 2009, 13: R84. 10.1186/cc7904
Cavallazzi R, Marik PE, Hirani A, Pachinburavan M, Vasu TS, Leiby BE: Association between time of admission to the ICU and mortality. A Systematic Review and Meta-analysis. Chest 2010, 138: 68-75. 10.1378/chest.10898
Laupland KB, Misset B, Souweine B, Tabah A, Azoulay E, Goldgran-Toledano D, Dumenil AS, Vésin A, Jamali S, Kallel H, Clec'h C, Darmon M, Schwebel C, Timsit JF: Mortality associated with timing of admission to and discharge from ICU: a retrospective cohort study. BMC Health Services Research 2011, 11: 321. 10.1186/1472-6963-11-321
Acknowledgements
SB is supported by a Canada Research Chair in Critical Care Nephrology and Clinical Investigator Award from Alberta Innovates - Health Solutions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
IS participated in the design of the study, performed statistical analysis, and drafted the manuscript. CK and RG participated in the design of the study and helped draft the manuscript. SB conceived the study, participated in its design and coordination, performed statistical analysis, and helped to draft the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
13054_2012_549_MOESM1_ESM.DOC
Additional file 1: Sensitivity Analysis. Multiple variable logistic regression analysis showing the association of ICU death with round-time/non-round-time admission, APACHE II score, age, burden of comorbidities, mechanical ventilation at admission, source of admission, study year and admission diagnosis stratified by study site. (DOC 84 KB)
13054_2012_549_MOESM2_ESM.DOC
Additional file 2: Sensitivity Analysis. Multiple variable logistic regression analysis showing the association of hospital death with round-time/non-round-time admission, APACHE II score, age, burden of comorbidities, mechanical ventilation at admission, source of admission, study year and admission diagnosis stratified by study site. (DOC 83 KB)
13054_2012_549_MOESM3_ESM.DOC
Additional file 3: Sensitivity Analysis. Multiple variable logistic regression analysis showing the association of ICU and hospital death with round-time/non-round-time admission, APACHE II score, age, burden of comorbidities, mechanical ventilation at admission, study year, study site and admission diagnosis among patients referred from the Emergency Department. (DOC 76 KB)
13054_2012_549_MOESM4_ESM.DOC
Additional file 4: Sensitivity Analysis. Multiple variable logistic regression analysis showing the association of ICU and hospital death with round-time/non-round-time admission, APACHE II score, age, burden of comorbidities, mechanical ventilation at admission, source of admission, study site and admission diagnosis among patients admitted during years 2006/2007. (DOC 78 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
de Souza, I.O., Karvellas, C.J., Gibney, R.N. et al. Impact of intensive care unit admission during morning bedside rounds and mortality: a multi-center retrospective cohort study. Crit Care 16, R72 (2012). https://doi.org/10.1186/cc11329
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc11329