Abstract
Introduction
Pleth Variability Index (PVI) is an automated and continuous calculation of respiratory variations in the perfusion index. PVI correlates well with respiratory variations in pulse pressure (ΔPP) and is able to predict fluid responsiveness in the operating room. ICU patients may receive vasopressive drugs, which modify vascular tone and could affect PVI assessment. We hypothesized that the correlation between PVI and ΔPP and the ability of PVI to identify patients with ΔPP > 13% is dependent on norepinephrine (NE) use.
Methods
67 consecutive mechanically ventilated patients in the ICU were prospectively included. Three were excluded. The administration and dosage of NE, heart rate, mean arterial pressure, PVI and ΔPP were measured simultaneously.
Results
In all patients, the correlation between PVI and ΔPP was weak (r2 = 0.21; p = 0.001). 23 patients exhibited a ΔPP > 13%. A PVI > 11% was able to identify patients with a ΔPP > 13% with a sensitivity of 70% (95% confidence interval: 47%-87%) and a specificity of 71% (95% confidence interval: 54%-84%). The area under the curve was 0.80 ± 0.06. 35 patients (53%) received norepinephrine (NE(+)). In NE(+) patients, PVI and ΔPP were not correlated (r2 = 0.04, p > 0.05) and a PVI > 10% was able to identify patients with a ΔPP > 13% with a sensitivity of 58% (95% confidence interval: 28%-85%) and a specificity of 61% (95% confidence interval:39%-80%). The area under the ROC (receiver operating characteristics) curve was 0.69 ± 0.01. In contrast, NE(-) patients exhibited a correlation between PVI and ΔPP (r2 = 0.52; p < 0.001) and a PVI > 10% was able to identify patients with a ΔPP > 13% with a sensitivity of 100% (95% confidence interval: 71%-100%) and a specificity of 72% (95% confidence interval: 49%-90%). The area under the ROC curve was 0.93 ± 0.06 for NE(-) patients and was significantly higher than the area under the ROC curve for NE(+) patients (p = 0.02).
Conclusions
Our results suggest that in mechanically ventilated adult patients, NE alters the correlation between PVI and ΔPP and the ability of PVI to predict ΔPP > 13% in ICU patients.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Fluid is administered to critically ill patients in order to increase cardiac preload and cardiac output (CO), yet studies have shown that about 50% of critically ill patients do not exhibit the desired effect [1, 2]. None of the routinely used static variables of cardiac preload such as filling pressures (central venous pressure (CVP) and pulmonary artery occlusion pressure) reliably predict fluid responsiveness [1, 3]. In contrast to static indices of preload, dynamic indices based on cardiopulmonary interactions and variations in left ventricular stroke volume are able to predict adequately the individual response to fluid loading [4–9] in specific settings (adult patients, tidal volume > 8 ml/kg, chest closed, heart rate/respiratory rate ratio > 3.6, absence of spontaneous breathing effort, arrhythmia, increase in intra-abdominal pressure or right ventricular dysfunction) [10–15]. However, these techniques are either invasive (respiratory variations in pulse pressure (ΔPP), stroke volume variations) with potential complications or are not continuous. The monitoring of the respiratory variations in pulse oximetry plethysmographic waveform amplitude (ΔPOP) has been proposed as a non-invasive method. Several studies have shown that ΔPOP correlates well with ΔPP and predicts fluid responsiveness in mechanically ventilated patients in the operating room and not in spontaneous breathing patients [16–19]. However, the agreement between ΔPOP and ΔPP and the ability of ΔPOP to predict fluid responsiveness in ICUs remains controversial [20, 21]. The difficulty in obtaining an interpretable pulse oximetry plethysmographic waveform signal could explain this controversy. Furthermore, ΔPOP is not easily measured at the bedside and cannot be continuously monitored. Recently, the Pleth Variability Index (PVI) (Masimo Corp., Irvine, CA, USA), a novel algorithm allowing automated and continuous calculation of the respiratory variations in the perfusion index (PI), was proposed. The pulse oximeter waveform uses the two components of light absorption. PI is defined as the ratio between constant absorption and pulsatile absorption. It has been demonstrated that PVI correlates well with ΔPOP and ΔPP and that it can predict fluid responsiveness and the hemodynamic effect of positive end-expiratory pressure in the operating room and in the immediate postoperative period [22–24]. In ICUs, some patients receive vasopressive drugs such as norepinephrine (NE), which modify vascular tone. PVI measurements are influenced by vascular tone that may affect its pulsatile absorption component [21, 25, 26]. In this way, NE may affect PVI assessment. We hypothesized that NE use may impact (i) the correlation between PVI and ΔPP and (ii) the ability of PVI to identify patients with a ΔPP above 13% (threshold often used in clinical practice in order to indicate volume expansion) [7]. To test this hypothesis, PVI and ΔPP were simultaneously measured in consecutive patients receiving or not receiving NE. This hypothesis was tested only in adult patients because ΔPP fails in predicting fluid responsiveness in children because arterial compliance and chest wall-to-lung elastance ratio differ from adults [15].
Materials and methods
Patients
After obtaining approval from the local ethics committee (Comité de Protection des Personnes Sud-Ouest et Outre Mer III, Bordeaux, France; protocol no. DC 2009/34) and informed consent from the patient's next of kin, 67 consecutive mechanically ventilated patients from our ICU were prospectively included in the study.
Inclusion criteria were the following: patients mechanically ventilated without spontaneous breathing effort (identified by clinical examination and visual examination of respiratory curves), tidal volume of 8 ml/kg or above, absence of arrhythmia, heart rate/respiratory rate ratio above 3.6, Motor Activity Assessment Scale below 1 [27], Ramsay score above 5, absence of hypothermia or hyperthermia, left ventricular ejection fraction above 50%, absence of right ventricular dysfunction (attested by a peak systolic velocity of tricuspid annular motion < 0.15 m/s), and absence of increase in intra-abdominal pressure suspected by clinical context and examination. Patients were excluded if hemodynamic instability occurred (defined by a variation in heart rate or blood pressure of ≥10% over the 15-minute period before starting and during the protocol).
Sedation and analgesia were provided by continuous infusion of midazolam or propofol with sufentanil or morphine. All patients were previously equipped with an arterial catheter (115.090, 20 gauges, 8 cm, Vygon, Ecouen, France) connected and stored to a bedside monitor (Ultraview SL2900, Spacelabs Healthcare, Issaquah, Washington, USA). A personal computer was connected to the monitor in order to record arterial curves. A pulse oximeter probe (LNOP® Adt, Masimo Corp., Irvine, CA, USA) was attached to the index finger of the controlateral hand and wrapped to prevent outside light from interfering with the signal. The pulse oximeter was connected to a Masimo Radical 7 monitor with PVI software (Masimo SET, Masimo Corp., Irvine, CA, USA).
Measurements
Echocardiographic measurements
Doppler echocardiography was performed using a standard transthoracic probe (P4-2, Siemens Medical, Malvern, PA, USA) and a dedicated unit (Acuson CV-70, Siemens Medical System, Malvern, PA, USA). The stroke volume was calculated as the product of the aortic valve area by the velocity time integral of aortic blood flow (VTIAo). Using the parasternal long-axis view, the diameter of the aortic cusp was measured and the aortic valve area (π(diameter2)/4) was calculated. Using the apical five-chamber view, the VTIAo was computed from the area under the envelope of the pulsed-wave Doppler signal obtained at the level of the aortic annulus. The VTIAo value was averaged over five consecutive measurements. CO was calculated as the product of heart rate and stroke volume. Left ventricular ejection fraction (LVEF) was measured using the biplane Simpson's method from the apical two- and four-chamber views. Respiratory variations in VTIAo were measured: the maximum and minimum VTIAo values were identified for one minute and averaged to obtain VTIAomax and VTIAomin. The mean VTIAo (VTIAomean) was calculated as (VTIAomax - VTIAomin)/2. Respiratory variations in VTIAo was calculated as (VTIAomax - VTIAomin)/VTIAomean × 100. Peak systolic velocity of tricuspid annular motion, a right ventricular function parameter, was assessed by tissue Doppler echocardiography. Patients with a peak systolic velocity of tricuspid annular motion below 0.15 m/s were not included because it has been shown that ΔPP may prove inaccurate in this case [12].
Calculation of ΔPP
Arterial waveforms were recorded using a personal computer. The computer images were analyzed using Image J software (National Institutes of Health, Bethesda, MD, USA). Pulse pressure was defined as the difference between systolic and diastolic arterial blood pressure. Maximal (Pulse Pressure max) and minimal (Pulse Pressure min) values were determined over the same respiratory cycle. ΔPP was then calculated as: ΔPP = (Pulse Pressure max - Pulse Pressure min)/((Pulse Pressure max + Pulse Pressure min)/2), as previously described [7]. ΔPP was evaluated in triplicate over each of three consecutive respiratory cycles. The mean values of the three determinations were used for statistical analysis. ΔPP was analyzed offline by a physician (MB) blinded to PVI values.
Pleth Variability Index
For the measurement of oxygen saturation via pulse oximetry, red and infrared lights are utilized. A constant amount of light (DC) from the signal of the pulse oximeter is absorbed by the skin, other tissues, and nonpulsatile blood, while a variable amount of light (AC) is absorbed by the pulsating arterial inflow. To calculate PI, the infrared pulsatile signal is indexed against the nonpulsatile infrared signal and expressed as a percentage (PI = (AC/DC) × 100). The infrared signal is used because it is less affected by changes in arterial saturation than the red signal. PVI is a measure of the dynamic changes in the PI that occur during the respiratory cycle (PVI = (PImax-PImin)/Pimax). It is calculated by measuring changes in PI over a defined time interval where one or more complete respiratory cycle occurred. PVI is therefore displayed continuously on the monitor as a percentage.
Other measurements
Temperature, mean arterial pressure, and heart rate were also recorded.
Study protocol
Immediately before and during the recording period, vasoactive drugs were not changed, and fluid expansion was not given. One set of simultaneous measurements was performed. PVI values were recorded by an observer blinded to ΔPP values. Measurements began after a stable PVI value (i.e., a value that remained unchanged or varied for a maximum of one point) was obtained for at least five minutes.
Statistical analysis
Results were expressed as mean ± standard deviation unless stated otherwise. ΔPP and PVI were compared using Student's t test and linear correlation. Characteristics of patients receiving NE (NE(+)) or not (NE(-)) were compared using Student's t test. Data were divided into two groups according to the value of ΔPP (> 13% or ≤13%); this threshold has been shown to be predictive of fluid responsiveness in mechanically ventilated patients [7]. Receiver operating characteristic (ROC) curves were generated for PVI in all patients, in NE(+) patients and in NE(-) patients, varying the discriminating threshold of this parameter. Area under the ROC curves generated for NE(+) and NE(-) patients were compared using a z test. A P value of less than 0.05 was considered to be statistically significant. Statistical analysis was performed using Statview for Windows, version 5 (SAS Institute, Cary, NC, USA), Medcalc (software 11.5.1.0; Mariakerke, Belgium) and Sigmaplot 11.0 (Systat Software, Inc. San Jose, CA, USA).
Results
Global analysis
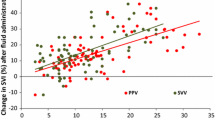
Sixty seven patients were initially included. Three patients were excluded for hemodynamic instability during the protocol (n = 3). Patients were included 3.8 ± 1.7 days after admission to the ICU. The main characteristics of the 64 patients are shown in Table 1. In all patients, PVI and ΔPP were not significantly different (P > 0.05). The correlation coefficient between PVI and ΔPP was 0.21 (P = 0.001; Figure 1). In all patients, respiratory variations in VTIAo correlated moderately with PVI (r2 = 0.19, P = 0.0003). Twenty-three patients exhibited a ΔPP above 13%. In all patients, a PVI threshold value above 11% was able to discriminate between ΔPP above 13% and ΔPP of 13% and below with a sensitivity of 70% (95% confidence interval: 47% to 87%) and a specificity of 71% (95% confidence interval: 54% to 84%). Positive and negative predictive values and positive and negative likelihood ratio are shown in Table 2. Area under the ROC curve for PVI to predict ΔPP above 13% was 0.80 ± 0.06.
Relation between Pleth Variabilty Index and respiratory-induced variations in pulse pressure in patients (a) receiving or (b) not receiving norepinephrine. clear circle, patients receiving norepinephrine (NE(+)); filled circle, patients not receiving norepinephrine (NE(-)); ΔPP, respiratory-induced variations in pulse pressure; PVI, Pleth Variabilty Index.
Impact of norepinephrine
Thirty five patients (53%) received NE since 3.6 ± 1.6 days (mean dosage = 0.36 ± 0.27 μg/kg/min). None of them received dobutamine, epinephrine or dopamine. Hemodynamic data, temperature, inspiratory oxygen fraction, tidal volume, respiratory rate, and heart rate were not different in NE(+) and NE(-) patients (Table 3).
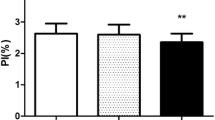
In NE(+) patients, PVI did not correlate with ΔPP (r2 = 0.04, P > 0.05; Figure 1) or with respiratory variations in VTIAo (r2 = 0.031, P > 0.05). Twelve patients (24%) exhibited a ΔPP above 13%. A PVI threshold value above 10% was able to discriminate between ΔPP above 13% and ΔPP of 13% or below with a sensitivity of 58% (95% confidence interval: 28% to 85%) and a specificity of 61% (95% confidence interval: 39% to 80%). Positive and negative predictive values and positive and negative likelihood ratio are shown in Table 2. Area under the curve for PVI to predict ΔPP above 13% in NE(+) patients was 0.69 ± 0.01 (Figure 2). The difference between ΔPP and PVI was not correlated with NE dosage (P > 0.05).
In NE(-) patients, PVI correlated with ΔPP (r2 = 0.52, P < 0.001; Figure 1) and with respiratory variations in VTIAO (r2 = 0.53, P < 0.0001). Eleven patients (38%) exhibited a ΔPP above 13%. A PVI threshold value above 10% was able to discriminate between ΔPP above 13% and ΔPP of 13% or below with a sensitivity of 100% (95% confidence interval: 71% to 100%) and a specificity of 72% (95% confidence interval: 49% to 90%). Positive and negative predictive values and positive and negative likelihood ratio are shown in Table 2. Area under the curve for PVI to predict ΔPP above 13% was 0.93 ± 0.06 (Figure 2).
The area under the ROC curves for NE(+) and NE(-) patients were significantly different (P = 0.02).
Impact of pulsatility index
PI values were not correlated with NE dosage (P > 0.05). The difference between PVI and ΔPP was not correlated with PI values (P > 0.05 in all patients, both in NE(+) patients and in NE(-) patients).
Discussion
Our data suggest that in the condition of the study, the relation between PVI and ΔPP in ICU patients is weak and that the ability of PVI to predict a ΔPP above 13% are negatively influenced by NE use. Further studies are needed to investigate the ability of PVI to predict fluid responsiveness in specific settings.
Mechanical ventilation induces cyclic changes in intrathoracic and transpulmonary pressures that transiently affect left ventricular preload, resulting in cyclic changes in stroke volume in preload-dependent, but not in preload-independent, patients [28, 29]. These cyclic changes in stroke volume can be evaluated by cyclic changes in arterial pulse pressure. Several studies have shown that ΔPP is able to predict fluid responsiveness in patients in the operating theatre and in ICUs [4, 30]. Even if most patients admitted to ICUs are instrumented with an intra-arterial catheter, it is well known that percutaneous arterial catheterization is associated with rare but serious complications (thrombosis, infections, pseudoaneurysm, hematoma, bleeding) [31–35]. Therefore, a non-invasive approach may be of value.
ΔPOP has been proposed as an alternative to ΔPP. In the operating room, it has been shown that ΔPOP correlates well with ΔPP and can predict fluid responsiveness [16, 17]. In ICUs, however, the results are controversial. Although some studies have found a strong correlation between ΔPOP and ΔPP and have shown that ΔPOP can be a good indicator of fluid responsiveness [20, 36], Landsverk et al. showed a poor agreement between ΔPOP and ΔPP [21]. This technique is not yet available in clinical practice because plethysmographic waveform processing and filtering requires specific tools and software that are not widely available. PVI has been proposed for the automated and continuous calculation of the respiratory variations in the pulse oximeter waveform amplitude [22]. It can also predict fluid responsiveness in the operating room [23].
In the present study, the correlation between PVI and ΔPP is weak in ICU patients. Our results are not in accordance with those of Loupec et al. [37]. Several reasons may explain these differences. First, the population studied by Loupec et al. is different from our patients. They included a majority of surgical and septic patients. In contrast, we included a majority of trauma patients. In patients with brain injury, NE is administered in order to increase cerebral perfusion pressure, whereas peripheral vasomotor tone is hardly affected. In contrast, in septic patients, vasoplegia induces an alteration in microvascular perfusion and NE is administered in order to improve or restore vasomotor tone. The amplitude of the pulse oximetry plethysmographic waveform is influenced by changes in vascular tone from all tissue compartments present in the fingertip, and vasoconstriction narrows the amplitude of the waveform. Thus, patients with brain injury who require NE had potentially a different vasomotor tone than patients with septic shock under NE and this may affect PVI in a different manner. Unfortunately, we did not explore skin microcirculation (e.g. using laser Doppler flowmetry) and we cannot make firm conclusions on this hypothesis. Second, in the present study the mean duration of NE infusion before starting protocol was rather long (3.6 ± 1.6 days) and all patients did not receive NE. This may impact the quality of the signal. Third, we did not perform fluid challenge or passive leg raising tests. Finally, we excluded patients with right ventricular dysfunction.
Mechanical ventilation induces cyclic changes in stroke volume. These variations may be measured ideally at the level of the heart (e.g. respiratory variations in VTIAo) or may be evaluated peripherally using surrogates (ΔPP, pulse contour analysis). As PVI and ΔPP are measured peripherally, NE infusion may alter the relation between these surrogates and the respiratory variations in stroke volume. In this way, the lack of correlation between ΔPP and PVI in NE(+) patients could be due to issues in PVI or ΔPP. However, the relation between PVI and respiratory variations in VTIAo was also altered in NE(+) patients. Thus, the lack of relation between PVI and ΔPP in NE(+) patients seems to be due to issues in PVI, and not in ΔPP.
Several mechanisms are known to interfere with ΔPOP and PVI calculations and could explain our results. PI depends on vasomotor tone, which may affect the pulsatile absorption component [25, 26]. For this reason, signal quality, body temperature, vasoactive drug infusion, level of sedation, presence of nociceptive input, and spontaneous movements may have an impact. Even if vasomotor tone is constant over a single respiratory cycle and does not alter the analysis of the relative change in PI induced by mechanical ventilation, it may be that vasoconstriction induced by NE narrows the amplitude of the pulse oximeter waveform and alters the PI analysis. We did not observe a dose-effect relation (the difference between ΔPP and PVI was not correlated with NE dosage). A recent study suggested that PI values may influence the ability of PVI to predict fluid responsiveness [38]. In our study, we did not find any relation between PI values and NE dosage or between PI values and the difference between PVI and ΔPP values. Pulse oximeter waveform may be influenced by outside light absorption and the pulse oximeter may have to be wrapped in order to prevent outside light from interfering with the signal. Furthermore, the site for measuring the effect of ventilation on pulse oximeter waveform (ear, finger, and forehead) is of major importance [39]. In order to avoid artefacts, all these parameters have been taken into account during the procedure.
Our study has some limitations. First, we focused on the relation between PVI and ΔPP and did not perform fluid challenge. We chose 13% as a cut-off value for ΔPP because this was the first value to be reported and because most of the studies focusing on this topic found similar values even in patients receiving NE [7, 40]. However, there is no firm data supporting any discriminant universal ΔPP threshold in clinical settings, especially in patients needing tight fluid titration. Second, as dynamic indices such as ΔPP or PVI are known to have some limitations, we made sure we were testing situations in which these indices are interpretable: no spontaneous breathing activity, no arrhythmia, tidal volume above 8 ml/kg, absence of right heart failure and heart rate/respiratory rate above 3.6 [10–12]. Finally, we did not measure intra-abdominal pressure in all patients whereas it is known that clinical context and evaluation may cause problems when diagnosing intra-abdominal hypertension [41, 42].
Conclusions
In the conditions of the study, our results suggest that: the correlation between PVI and ΔPP is weak; NE modifies the correlation between PVI and ΔPP; and NE alters the ability of PVI to predict ΔPP above 13% in ICU patients.
Key messages
-
The relation between PVI and ΔPP is weak in ICU patients.
-
The relation between PVI and ΔPP is negatively influenced by NE use.
-
The ability of PVI to predict a ΔPP above 13% is negatively influenced by NE use.
Abbreviations
- ΔPOP:
-
respiratory variations in pulse oximetry plethysmographic waveform amplitude
- ΔPP:
-
respiratory induced variations in pulse pressure
- CO:
-
cardiac output
- CVP:
-
central venous pressure
- LVEF:
-
left ventricular ejection fraction
- NE:
-
norepinephrine
- PI:
-
perfusion index
- PVI:
-
pleth variability index
- ROC:
-
receiver operating characteristics
- VTIAo:
-
velocity time integral of aortic blood flow.
References
Michard F: Changes in arterial pressure during mechanical ventilation. Anesthesiology 2005, 103: 419-428. 10.1097/00000542-200508000-00026
Michard F, Teboul JL: Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest 2002, 121: 2000-2008. 10.1378/chest.121.6.2000
Osman D, Ridel C, Ray P, Monnet X, Anguel N, Richard C, Teboul JL: Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Crit Care Med 2007, 35: 64-68. 10.1097/01.CCM.0000249851.94101.4F
Biais M, Nouette-Gaulain K, Cottenceau V, Revel P, Sztark F: Uncalibrated pulse contour-derived stroke volume variation predicts fluid responsiveness in mechanically ventilated patients undergoing liver transplantation. Br J Anaesth 2008, 101: 761-768. 10.1093/bja/aen277
Feissel M, Michard F, Faller JP, Teboul JL: The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med 2004, 30: 1834-1837.
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL: Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 2001, 119: 867-873. 10.1378/chest.119.3.867
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL: Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 2000, 162: 134-138.
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P: Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology 1998, 89: 1313-1321. 10.1097/00000542-199812000-00007
Cannesson M, Desebbe O, Lehot JJ: Fluid responsiveness assessment using the pulse oxymeter waveform: not yet ready for prime time. Anesth Analg 2007, 104: 1598-1599. 10.1213/01.ane.0000260463.40639.7f
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL: Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med 2005, 31: 517-523. 10.1007/s00134-005-2586-4
De Backer D, Taccone FS, Holsten R, Ibrahimi F, Vincent JL: Influence of respiratory rate on stroke volume variation in mechanically ventilated patients. Anesthesiology 2009, 110: 1092-1097. 10.1097/ALN.0b013e31819db2a1
Mahjoub Y, Pila C, Friggeri A, Zogheib E, Lobjoie E, Tinturier F, Galy C, Slama M, Dupont H: Assessing fluid responsiveness in critically ill patients: False-positive pulse pressure variation is detected by Doppler echocardiographic evaluation of the right ventricle. Crit Care Med 2009, 37: 2570-2575. 10.1097/CCM.0b013e3181a380a3
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL: Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 2006, 34: 1402-1407. 10.1097/01.CCM.0000215453.11735.06
Wyler von Ballmoos M, Takala J, Roeck M, Porta F, Tueller D, Ganter CC, Schroder R, Bracht H, Baenziger B, Jakob SM: Pulse-pressure variation and hemodynamic response in patients with elevated pulmonary artery pressure: a clinical study. Crit Care 2010, 14: R111. 10.1186/cc9060
Durand P, Chevret L, Essouri S, Haas V, Devictor D: Respiratory variations in aortic blood flow predict fluid responsiveness in ventilated children. Intensive Care Med 2008, 34: 888-894. 10.1007/s00134-008-1021-z
Cannesson M, Attof Y, Rosamel P, Desebbe O, Joseph P, Metton O, Bastien O, Lehot JJ: Respiratory variations in pulse oximetry plethysmographic waveform amplitude to predict fluid responsiveness in the operating room. Anesthesiology 2007, 106: 1105-1111. 10.1097/01.anes.0000267593.72744.20
Natalini G, Rosano A, Taranto M, Faggian B, Vittorielli E, Bernardini A: Arterial versus plethysmographic dynamic indices to test responsiveness for testing fluid administration in hypotensive patients: a clinical trial. Anesth Analg 2006, 103: 1478-1484. 10.1213/01.ane.0000246811.88524.75
Delerme S, Castro S, Freund Y, Nazeyrollas P, Josse MO, Madonna-Py B, Rouff E, Riou B, Ray P: Relation between pulse oximetry plethysmographic waveform amplitude induced by passive leg raising and cardiac index in spontaneously breathing subjects. Am J Emerg Med 2010, 28: 505-510. 10.1016/j.ajem.2009.03.023
Delerme S, Renault R, Le Manach Y, Lvovschi V, Bendahou M, Riou B, Ray P: Variations in pulse oximetry plethysmographic waveform amplitude induced by passive leg raising in spontaneously breathing volunteers. Am J Emerg Med 2007, 25: 637-642. 10.1016/j.ajem.2006.11.035
Feissel M, Teboul JL, Merlani P, Badie J, Faller JP, Bendjelid K: Plethysmographic dynamic indices predict fluid responsiveness in septic ventilated patients. Intensive Care Med 2007, 33: 993-999. 10.1007/s00134-007-0602-6
Landsverk SA, Hoiseth LO, Kvandal P, Hisdal J, Skare O, Kirkeboen KA: Poor agreement between respiratory variations in pulse oximetry photoplethysmographic waveform amplitude and pulse pressure in intensive care unit patients. Anesthesiology 2008, 109: 849-855. 10.1097/ALN.0b013e3181895f9f
Cannesson M, Delannoy B, Morand A, Rosamel P, Attof Y, Bastien O, Lehot JJ: Does the Pleth variability index indicate the respiratory-induced variation in the plethysmogram and arterial pressure waveforms? Anesth Analg 2008, 106: 1189-1194. 10.1213/ane.0b013e318167ab1f
Cannesson M, Desebbe O, Rosamel P, Delannoy B, Robin J, Bastien O, Lehot JJ: Pleth variability index to monitor the respiratory variations in the pulse oximeter plethysmographic waveform amplitude and predict fluid responsiveness in the operating theatre. Br J Anaesth 2008, 101: 200-206. 10.1093/bja/aen133
Desebbe O, Boucau C, Farhat F, Bastien O, Lehot JJ, Cannesson M: The ability of pleth variability index to predict the hemodynamic effects of positive end-expiratory pressure in mechanically ventilated patients under general anesthesia. Anesth Analg 2010, 110: 792-798. 10.1213/ANE.0b013e3181cd6d06
Lima A, Bakker J: Noninvasive monitoring of peripheral perfusion. Intensive Care Med 2005, 31: 1316-1326. 10.1007/s00134-005-2790-2
Lima AP, Beelen P, Bakker J: Use of a peripheral perfusion index derived from the pulse oximetry signal as a noninvasive indicator of perfusion. Crit Care Med 2002, 30: 1210-1213. 10.1097/00003246-200206000-00006
Devlin JW, Boleski G, Mlynarek M, Nerenz DR, Peterson E, Jankowski M, Horst HM, Zarowitz BJ: Motor Activity Assessment Scale: a valid and reliable sedation scale for use with mechanically ventilated patients in an adult surgical intensive care unit. Crit Care Med 1999, 27: 1271-1275. 10.1097/00003246-199907000-00008
Pinsky MR: Using ventilation-induced aortic pressure and flow variation to diagnose preload responsiveness. Intensive Care Med 2004, 30: 1008-1010. 10.1007/s00134-004-2208-6
Vieillard-Baron A, Chergui K, Augarde R, Prin S, Page B, Beauchet A, Jardin F: Cyclic changes in arterial pulse during respiratory support revisited by Doppler echocardiography. Am J Respir Crit Care Med 2003, 168: 671-676. 10.1164/rccm.200301-135OC
Michard F: Changes in arterial pressure during mechanical ventilation. Anesthesiology 2005, 103: 419-428. 10.1097/00000542-200508000-00026
Scheer B, Perel A, Pfeiffer UJ: Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care 2002, 6: 199-204. 10.1186/cc1489
Cohen A, Reyes R, Kirk M, Fulks RM: Osler's nodes, pseudoaneurysm formation, and sepsis complicating percutaneous radial artery cannulation. Crit Care Med 1984, 12: 1078-1079. 10.1097/00003246-198412000-00017
Evans PJ, Kerr JH: Arterial occlusion after cannulation. Br Med J 1975, 3: 197-199. 10.1136/bmj.3.5977.197
McEllistrem RF, O'Toole DP, Keane P: Post-cannulation radial artery aneurysm--a rare complication. Can J Anaesth 1990, 37: 907-909. 10.1007/BF03006633
Slogoff S, Keats AS, Arlund C: On the safety of radial artery cannulation. Anesthesiology 1983, 59: 42-47. 10.1097/00000542-198307000-00008
Cannesson M, Besnard C, Durand PG, Bohe J, Jacques D: Relation between respiratory variations in pulse oximetry plethysmographic waveform amplitude and arterial pulse pressure in ventilated patients. Crit Care 2005, 9: R562-568. 10.1186/cc3799
Loupec T, Nanadoumgar H, Frasca D, Petitpas F, Laksiri L, Baudouin D, Debaene B, Dahyot-Fizelier C, Mimoz O: Pleth variability index predicts fluid responsiveness in critically ill patients. Crit Care Med 2010, 39: 294-299.
Broch O, Bein B, Gruenewald M, Hocker J, Schottler J, Meybohm P, Steinfath M, Renner J: Accuracy of the pleth variability index to predict fluid responsiveness depends on the perfusion index. Acta Anaesthesiol Scand 2011, 55: 686-693. 10.1111/j.1399-6576.2011.02435.x
Shelley KH, Jablonka DH, Awad AA, Stout RG, Rezkanna H, Silverman DG: What is the best site for measuring the effect of ventilation on the pulse oximeter waveform? Anesth Analg 2006, 103: 372-377. 10.1213/01.ane.0000222477.67637.17
Marik PE, Cavallazzi R, Vasu T, Hirani A: Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med 2009, 37: 2642-2647. 10.1097/CCM.0b013e3181a590da
Cheatham ML, Malbrain ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppaniemi A, Olvera C, Ivatury R, D'Amours S, Wendon J, Hillman K, Wilmer A: Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. II. Recommendations. Intensive Care Med 2007, 33: 951-962. 10.1007/s00134-007-0592-4
Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppaniemi A, Olvera C, Ivatury R, D'Amours S, Wendon J, Hillman K, Johansson K, Kolkman K, Wilmer A: Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med 2006, 32: 1722-1732. 10.1007/s00134-006-0349-5
Acknowledgements
The authors thank Ray Cooke for assistance with manuscript preparation. Only departmental funds were used for this study. No external funds were obtained.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests. The manufacturers (Masimo Corp, Irvine, CA, USA) provided the material free of charge.
Authors' contributions
MB conceived and designed the study. MB, VC, LP, and JFC collected the data. MB and FM performed the statistical analysis and drafted the manuscript. MB and FS wrote the paper. All authors read and approved the final manuscript
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Biais, M., Cottenceau, V., Petit, L. et al. Impact of norepinephrine on the relationship between pleth variability index and pulse pressure variations in ICU adult patients. Crit Care 15, R168 (2011). https://doi.org/10.1186/cc10310
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc10310