Abstract
Introduction
Tidal volume and plateau pressure minimisation are the standard components of a protective lung ventilation strategy for patients with acute respiratory distress syndrome (ARDS). Open lung strategies, including higher positive end-expiratory pressure (PEEP) and recruitment manoeuvres to date have not proven efficacious. This study examines the effectiveness and safety of a novel open lung strategy, which includes permissive hypercapnia, staircase recruitment manoeuvres (SRM) and low airway pressure with PEEP titration.
Method
Twenty ARDS patients were randomised to treatment or ARDSnet control ventilation strategies. The treatment group received SRM with decremental PEEP titration and targeted plateau pressure < 30 cm H2O. Gas exchange and lung compliance were measured daily for 7 days and plasma cytokines in the first 24 hours and on days 1, 3, 5 and 7 (mean ± SE). Duration of ventilation, ICU stay and hospital stay (median and interquartile range) and hospital survival were determined.
Results
There were significant overall differences between groups when considering plasma IL-8 and TNF-α. For plasma IL-8, the control group was 41% higher than the treatment group over the seven-day period (ratio 1.41 (1.11 to 1.79), P = 0.01), while for TNF-α the control group was 20% higher over the seven-day period (ratio 1.20 (1.01 to 1.42) P = 0.05). PaO2/FIO2 (204 ± 9 versus 165 ± 9 mmHg, P = 0.005) and static lung compliance (49.1 ± 2.9 versus 33.7 ± 2.7 mls/cm H2O, P < 0.001) were higher in the treatment group than the control group over seven days. There was no difference in duration of ventilation (180 (87 to 298) versus 341 (131 to 351) hrs, P = 0.13), duration of ICU stay (9.9 (5.6 to 14.8) versus 16.0 (8.1 to 19.3) days, P = 0.19) and duration of hospital stay (17.9 (13.7 to 34.5) versus 24.7 (20.5 to 39.8) days, P = 0.16) between the treatment and control groups.
Conclusions
This open lung strategy was associated with greater amelioration in some systemic cytokines, improved oxygenation and lung compliance over seven days. A larger trial powered to examine clinically-meaningful outcomes is warranted.
Trial registration
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) is an inflammatory condition of the lungs that is associated with high mortality [1]. Mechanical ventilation is a life supporting intervention that aims to maintain gas exchange in these patients, but it can also augment or initiate lung injury [2]. Lung-protective mechanical ventilation strategies that aim to minimise tidal volume and plateau pressure have been the predominant intervention associated with improved patient survival [3, 4].
Clinicians frequently use high positive end-expiratory pressure (PEEP) to improve alveolar recruitment in patients with ARDS. PEEP aims to counter the pulmonary shunt due to increased lung collapse resulting from inflammation. High PEEP maintains functional residual capacity and improves oxygenation [5, 6] and may even have an effect on reducing mortality associated with ARDS [7, 8]. The best strategy to set optimal PEEP for an individual patient has not yet been established [9, 10].
It is unclear whether lung recruitment manoeuvres (LRM) add benefit to low tidal volume protective ventilation strategies in ARDS [11, 12]. The most commonly used LRM requires the application of sustained continuous positive airway pressure (CPAP) at 35 to 40 cm H2O for 40 seconds [2, 13, 14]. However, this LRM method can be uncomfortable, may induce circulatory depression and has not been associated with improved outcomes in patients with ARDS [13–15].
We previously demonstrated that a staircase recruitment manoeuvre (SRM) was safe and effective in improving oxygenation and lung compliance for up to one hour in patients with ARDS[16]. The SRM involves a progressive increase in PEEP (up to 40 cm H2O) over several minutes with mandatory pressure control ventilation, resulting in intermittent higher pressures (55 cm H2O) for longer duration and increased alveolar recruitment compared with static recruitment methods [16]. Borges and co-workers found that oxygenation benefits of the SRM can be maintained for up to six hours with the application of "optimal" PEEP using a PEEP titration manoeuvre [17]. To our knowledge the effect of an open lung strategy, which includes SRM and PEEP titration, on inflammatory markers or physiological indices has not been investigated beyond six hours in patients with ARDS.
The potentially deleterious higher airway pressures observed in previous strategies that incorporated high PEEP and LRMs may be avoided by reducing tidal volume, a practice that may require permissive hypercapnia. It has been demonstrated in animals and humans that the acidosis induced by this hypercapnia, independent of any changes in ventilator strategy, may also confer benefit in ARDS [18–20].
The aim of this pilot trial was to compare an open lung pressure control ventilation strategy that utilised SRM, high PEEP and permissive hypercapnia to limit airway pressures (PHARLAP; Permissive Hypercapnia, Alveolar Recruitment, Low Airway Pressures) with a control strategy (conventional ARDSnet 'protective' volume controlled ventilation [21]) in patients with ARDS to determine the effect on inflammatory cytokines, physiological lung injury (arterial oxygenation and lung compliance) and rates of barotrauma over a seven-day period.
Materials and methods
This pilot randomised, controlled, parallel-group study was conducted between January 2008 and October 2009. The Human Research Ethics Committees of The Alfred Hospital and Monash University approved the study protocol. Informed consent was obtained from each patient's next of kin.
Twenty mechanically ventilated patients with ARDS [22] in the Intensive Care Unit of the Alfred Hospital were enrolled. Patients were randomised to treatment (PHARLAP) or control groups using sequentially numbered sealed opaque envelopes, generated by computerised random block schedule. Patients were stratified by the diagnosis of severe sepsis according to ACCP/SCCM Consensus Conference guidelines [23–25].
Inclusion criteria were the diagnosis of ARDS [26, 27], age > 15 years, and the presence of both an intra-arterial line and central venous catheter. Patients were excluded if they had chest trauma, an intercostal catheter with air leak, a pneumothorax on chest x-ray, bronchospasm on auscultation, raised intracranial pressure, mean arterial pressure ≤60 mmHg, significant arrhythmias or were ventilated for longer than 72 hours.
Interventions
PHARLAP ventilation strategy
The PHARLAP strategy included pressure control ventilation (PCV), with plateau pressures < 30 cm H2O while delivering tidal volumes of less than 6 mls/kg ideal body weight (IBW) with patients in a supine position with 30 degrees head of bed elevation. The fraction of inspired oxygen (FIO2) was adjusted until the continuously monitored oxygen saturation was 90 to 92%. For the SRM, the high pressure was set to 15 cm H2O above the PEEP, which was increased in a stepwise manner to 20, then 30 and then 40 cm H2O every two minutes, and then reduced to 25, then 22.5, then 20, then 17.5 or then an absolute minimum of 15 cm H2O every three minutes until a decrease in SaO2 ≥ 1% from maximum SaO2 was observed. This was defined as the derecruitment point. PEEP was then increased to 40 cm H2O for one minute and returned to a PEEP level 2.5 cm H2O above the derecruitment point (which was then defined as optimal PEEP). Stepwise increases in PEEP did not continue if the patient became bradycardic or tachycardic (< 60 or > 140 beats per minute), developed a new arrhythmia, became hypotensive (systolic blood pressure < 80 mmHg) or became hypoxaemic (SaO2 < 85%). Following this SRM the tidal volume was adjusted to achieve a tidal volume ≤ 6 mls/kg IBW and a plateau pressure ≤ 30 cm H2O. Hypercapnia was tolerated and acidosis was only treated if the pH was less than 7.15 by increasing respiratory rate to a maximum of 38 breaths per minute. The PHARLAP group received one SRM daily (with decremental PEEP titration) until the patient was deemed ready for weaning. In addition, PEEP was transiently elevated to 40 cm H2O (with PCV at 15 cm H2O) for one minute if oxygen desaturation ≤ 90% occurred or after disconnection from the ventilator.
Patients were assessed daily for weaning readiness. Weaning was commenced in both groups when all of the following occurred: respiratory rate < 35 breaths per minute, PaO2 > 60 mm Hg, SpO2 > 90% with fraction of inspired oxygen < 0.4 and PEEP < 10 cm H2O, mean arterial pressure > 60 mm Hg without inotrope infusions or sedatives.
Control ventilation strategy
The control group was treated using the ARDSnet protocol, with assist control ventilation and FiO2/PEEP titration [21]. Tidal volumes were limited to 6 mls/kg, plateau pressures < 30 cm H2O. Acidosis (pH < 7.3) was actively managed by increasing minute ventilation. PCV was not used, and recruitment manoeuvres were only allowed if the patient met the criteria for use of a rescue therapy, which was when the patient was receiving FiO2 ≥ 0.9, and the treating clinicians considered one necessary.
Outcome measures
Plasma interleukin-6 (IL-6), interleukin-1β (IL-1β), interleukin-8 (IL-8) and TNF-α concentrations were measured from arterial blood samples taken at baseline, three hours after randomisation and then on days 1, 3, 5 and 7. Samples were immediately centrifuged at 1,500 g for 10 minutes and plasma aspirated and stored at -70°C. Cytokines were detected using commercially available enzyme-linked immune-absorbent assays (ELISA, R&D Systems, Inc., Minneapolis, MN, USA).
Peak and plateau pressure, tidal volume, respiratory rate, PEEP, heart rate and rhythm, central venous pressure, blood pressure, inotrope dosage and arterial blood gases were measured at baseline, 1, 3, 6 and 24 hours and then daily during the period of mechanical ventilation up to seven days. Derived variables were PaO2/FIO2 ratio and static lung compliance. Length of stay (in ICU and in hospital), length of mechanical ventilation and hospital survival for both groups were recorded.
Sample size
The sample size was one of convenience as this was a pilot study. We estimated that 10 patients per group would provide > 80% power to detect a difference of one standard deviation in cytokine levels, with a two-sided test for differences, a P-value of 0.01 whilst assuming an Intraclass Correlation of 0.2 between baseline level and Day 3. The intention to treat principle was utilised.
Statistical analysis
All outcomes were initially assessed for normality and log-transformed where appropriate. Group comparisons were made using chi-square tests for equal proportion, Student t-tests for normally distributed data and Wilcoxon rank sum tests otherwise, with normally distributed data reported as means ± standard errors and non-normal data reported as medians (interquartile range). Group comparisons over time were performed using repeated measures analysis of variance fitting an overall group effect, a time effect and a group by time interaction to ascertain if the groups behaved differently over time. As cytokine measurements were found to be well approximated by log-normal distributions, results have been graphed as geometric means (95% CI) with differences reported as ratios (95% CI). Where baseline differences were found to exist, results were analysed using analysis of covariance with baseline values as a covariate. All models were fitted using the PROC Mixed procedure in SAS (SAS Version 9.1 SAS Institute Inc., Cary, NC, USA). To account for possible bias arising from differing extubation or dropout rates between groups, additional sensitivity analyses were conducted for compliance and oxygenation with patients carrying their last observation forward. A two-sided P-value ≤0.05 was considered statistically significant.
Results
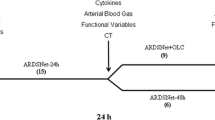
Twenty patients with ARDS were enrolled (Figure 1). Baseline demographic data of the control and PHARLAP groups are displayed in Table 1. There were no statistically significant differences between the groups at baseline.
In the PHARLAP group, all 10 patients received daily SRM with maximum PEEP of 40 cm H2O and a maximum plateau airway pressure of 55 cm H2O. Three patients transiently desaturated to < 90% at maximum PEEP of 40 cm H2O with no lasting adverse effects. There was no radiographic evidence of barotrauma during the seven day study period.
Two patients from the control group developed severe hypoxaemia (SaO2 ≤ 90% whilst receiving FiO2 0.9 and PEEP 18) and received rescue therapies (a static recruitment manoeuvre in one and inhaled nitric oxide in the other). One patient in the control group died during the seven-day intervention period. Five patients in the PHARLAP group were weaned from mechanical ventilation within the seven days compared to three in the control group. At Day 7, there were five PHARLAP group patients and six control group patients who remained on mechanical ventilation.
There was evidence to suggest that some cytokine values differed between groups with plasma IL-8 and TNF-α levels being significantly lower in the PHARLAP group (Figure 2). Using an analysis of covariance with baseline values as a covariate, the overall levels of IL-8 over all time points were 41% higher in the control group compared to the PHARLAP group (ratio 1.41 (1.11 to 1.79), P = 0.01). Similarly, overall levels of TNF-α over all time points were 20% higher in the control group compared to the PHARLAP group (ratio 1.20 (1.01 to 1.42), P = 0.05). There were no statistically significant differences in IL-6 or IL-1β between the treatment and control groups.
IL-8 and TNF-α measured over 168 hours (seven days) reported as geometric means (95% CI). There was a significant overall difference in interleukin-8 and serum tumour necrosis factor-alpha between the treatment group and the control group over the seven-day period (P = 0.01 and P = 0.05 respectively).
There was a significant overall improvement in static lung compliance in the PHARLAP group compared to the control group over seven days (49.1 ± 2.9 versus 33.7 ± 2.7 mls/cm H2O, P < 0.001, Figure 3). PaO2/FIO2 was higher in the PHARLAP group than the control group over the first 24 hours (Figure 4) and over 7 days (204 ± 9 versus 165 ± 9 cm H2O, P = 0.005, Figure 5).
Static lung compliance measured in ventilated patients for seven days (mean ± SE). There was a significant overall improvement in static lung compliance in the PHARLAP group compared to control group patients. A = missing data analysed as random P = 0.001, B = last observation carried forward P = 0.01.
The PEEP was higher in the PHARLAP group over the first 24 hours (Table 2) and throughout the 7 days (PHARLAP 12 ± 0.5 cm H2O, control 9.5 ± 0.5, P = 0.004, Table 3) than the control group.
There were no other significant differences between the groups (Table 3) in respiratory and haemodynamic variables, peak or plateau pressures, pH, PaCO2 or SOFA scores during the seven-day period. Of note, the mean plateau pressures were less than 30 cm H2O throughout the study in both groups and the plateau pressures were no higher in the PHARLAP group than the control group.
There were no differences in length of ventilation, length of stay in ICU and length of stay in hospital, or hospital survival (Table 4).
Discussion
This pilot, randomised controlled study examined the efficacy and safety of a multi-faceted open lung mechanical ventilation strategy that included permissive hypercapnia, staircase recruitment manoeuvres, decremental PEEP titration, low airway pressure and pressure control ventilation in patients with ARDS. The strategy appeared safe and was associated with ameliorations in plasma IL-8 and TNF-α levels, improved static lung compliance and improved oxygenation over a seven-day period. Although some cytokines were not significantly ameliorated (IL-6 and IL-1β) and unsurprisingly given the size of the study there were no significant differences in duration of mechanical ventilation, ICU stay and hospital stay.
Static lung compliance decreased by nearly 30% in the control strategy group over the first 24 hours and remained low for the duration of the study compared with the PHARLAP strategy, which actually resulted in an increase in compliance. These suggest a greater degree of lung recruitment was sustained throughout the study period in the PHARLAP group, an effect which may be important in ARDS to minimise the potential negative effects of ventilator induced lung injury.
Systemic arterial oxygenation, as measured by the PaO2/FIO2, was improved by the PHARLAP strategy and maintained for seven days. The beneficial effects of PEEP on oxygenation have been demonstrated by systematic review and include an association with improved survival in patients with ARDS [8]. It is unclear from our results whether the improved oxygenation was as a result of the increased PEEP, the SRM, both, or another aspect of our multi-pronged strategy. However, the results of this trial expand on the previous work by our group which demonstrated that the SRM with decremental optimal PEEP titration improved lung compliance and oxygenation over a one hour period in patients with ARDS [16].
The shorter duration of mechanical ventilation in the PHARLAP group resulted in smaller group size contributing to the mean values of PaO2/FIO2 and compliance as days progressed. This may have given the incorrect appearance of decreasing differences between the two groups especially considering that patients with better PaO2/FIO2 and compliance values are more likely to be extubated. We have attempted to correct for this by including a sensitivity analysis with last observation carried forward (Figures 3 and 5). In both analyses the differences between the PHARLAP and the control ventilation groups were statistically significant with the PHARLAP group having higher PaO2/FIO2 and static lung compliance over seven days.
It is as yet unclear if these physiological improvements would translate into clinically meaningful outcomes such as improved survival. However, in our study the use of rescue therapies for severe hypoxaemia was only required in the control group. Two of the patients in the control group required nitric oxide and the application PEEP levels higher than specified by the control group strategy protocol to maintain adequate oxygenation.
Although the study protocol advocated permissive hypercapnia and low airway pressures as components of the PHARLAP strategy, the mean PaCO2, pH and plateau pressure values were similar in both the PHARLAP and control groups. This suggests that these factors were less likely to have been responsible for the different outcomes between the groups. The primary differences in strategies were the application of the recruitment manoeuvre and the higher PEEP level with a lower driving pressure (a consequence of higher PEEP and unchanged plateau pressure) in the PHARLAP group. This is in contrast to several randomised trials [13, 14, 28], in all of which the treatment groups had a higher plateau pressure in association with a higher PEEP level, an important factor which may have confounded that ability of these high PEEP (± LRM) studies to detect a difference between groups. Importantly, our strategy achieved similar peak and plateau airway pressures in both groups despite increased levels of PEEP in the PHARLAP group.
Transient desaturation at maximum PEEP during SRMs with subsequent augmentation of oxygen saturation higher than baseline with PEEP reduction has previously been described by our group [16] and by others [17]. In this study, maximum PEEP was associated with transient desaturation in 3 of the 10 patients who received SRMs. There were no other adverse events reported. Transient desaturation does not indicate a failure of the lungs to respond to a recruitment manoeuvre [16]. The PHARLAP strategy improved lung compliance and oxygenation despite transient desaturation in these three patients.
Lung recruitment manoeuvres that involve high airway pressures to achieve and maintain lung recruitment have the potential to cause over-distension [29]. Plasma levels of IL-6, IL-1β, IL-8 and TNF-α were analysed to determine if the SRM caused an increase in inflammatory markers, which might reflect the systemic effects of over-distension lung injury. Our results showed that the PHARLAP strategy resulted in an overall reduction of plasma IL-8 and TNF-α over seven days that may have indicated a protective benefit associated with the treatment strategy. To ensure that observed differences between groups for IL-8 and TNF-α were not due to baseline imbalances, an analysis of covariance was conducted with baseline values used as covariates. There were no significant differences for IL-6 and IL-1β, which may reflect the large heterogeneity of the patient population, the small sample size, or that some cytokine levels are not affected by this mechanical ventilation strategy.
Although this study was not adequately powered to determine clinically-meaningful outcomes, it is interesting to note that the PHARLAP strategy was associated with what might be considered trends (P < 0.20) towards shorter duration of mechanical ventilation, ICU stay and hospital stay. We feel such pilot study results warrant investigation in a larger randomized trial. If the PHARLAP strategy is effective, it may be a safe and cost effective treatment strategy for patients with ARDS.
This study has a number of limitations. The unblinded nature of the study, coupled with the use of adjunctive interventions at the discretion of the intensive care physician in the case of severe hypoxaemia, may have confounded our results. There are several possible mechanisms for a decrease in SaO2 observed during the SRM other than atelectasis and increased shunt, which may lead to a false assumption of developing airway closure. It is possible that during the incremental pressure of the SRM there were reduced tidal volumes resulting in increased PaCO2 and arterial desaturation; however, in a previous study by our group the PaCO2 had returned to baseline levels at the point of determination of optimal PEEP [16]. We performed this study in a single-centre, which facilitated rigorous education and consistent implementation of the strategy, but may decrease the generalisability of the results to other populations. The small sample size meant the study was underpowered to determine differences in length of mechanical ventilation, ICU stay and hospital stay. It also meant that despite random allocation the static lung compliance at baseline was slightly higher and the PEEP was slightly lower in the PHARLAP group (Table 1). These differences were not statistically significant, but may have influenced our results.
Conclusions
This randomized controlled trial showed that a multi-faceted open lung strategy that was based on staircase recruitment manoeuvres and decremental PEEP titration improved plasma cytokines (IL-8 and TNF-α), static lung compliance and oxygenation over seven days. There were no differences in duration of mechanical ventilation, ICU stay or hospital stay; however, further investigation in a larger randomized trial is warranted.
Key messages
-
An open lung strategy including staircase recruitment and PEEP titration improved plasma cytokines, static lung compliance and oxygenation over seven days
-
An open lung strategy including staircase recruitment and PEEP titration was safe
-
Open lung ventilation was associated with a trend for reduced duration of ventilation that requires investigation in a larger trial
-
Open lung ventilation was associated with less use of rescue therapies
Abbreviations
- ARDS:
-
acute respiratory distress syndrome
- ARDSnet:
-
Acute Respiratory Distress Syndrome Network
- CI:
-
confidence interval
- FIO2:
-
fraction of inspired oxygen
- IBW:
-
ideal body weight
- ICU:
-
intensive care unit
- IL-6:
-
interleukin-6
- IL-8:
-
interleukin-8
- IL-1β:
-
interleukin-1β
- PaCO2:
-
partial pressure of carbon dioxide
- PaO2:
-
partial pressure of oxygen
- PaO2/FIO2:
-
ratio of partial pressure of oxygen to fraction of inspired oxygen
- PCV:
-
pressure control ventilation
- PEEP:
-
positive end expiratory pressure
- PHARLAP:
-
open lung ventilation strategy with Permissive Hypercapnia and Alveolar Recruitment and Low Airway Pressure
- SaO2:
-
arterial oxygen saturation
- SE:
-
standard error
- SRM:
-
staircase recruitment manoeuvre
- SOFA:
-
Sequential Organ Failure Assessment score
- TNF-α:
-
tumour necrosis factor-alpha
- VCV:
-
volume controlled ventilation.
References
Brower RG, Rubenfeld GD: Lung-protective ventilation strategies in acute lung injury. Crit Care Med. 2003, 31 (4 Suppl): S312-316.
Amato MBP, Barbas CSV, Medeiros DM, Magaldi RB, Schettino G, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR: Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. New Engl J Med. 1998, 338 (6): 347-354. 10.1056/NEJM199802053380602.
Brower RG, Matthay M, Schoenfeld D: Meta-analysis of acute lung injury and acute respiratory distress syndrome trials. Am J Respir Crit Care Med. 2002, 166 (11): 1515-1517.
Petrucci N, Iacovelli W: Lung protective ventilation strategy for the acute respiratory distress syndrome. Cochrane Database Syst Rev. 2007, CD003844-3
Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G: Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006, 354 (17): 1775-1786. 10.1056/NEJMoa052052.
Gernoth C, Wagner G, Pelosi P, Luecke T: Respiratory and haemodynamic changes during decremental open lung positive end-expiratory pressure titration in patients with acute respiratory distress syndrome. Crit Care. 2009, 13 (2): R59-10.1186/cc7786.
Phoenix SI, Paravastu S, Columb M, Vincent JL, Nirmalan M: Does a higher positive end expiratory pressure decrease mortality in acute respiratory distress syndrome? A systematic review and meta-analysis. Anesthesiology. 2009, 110 (5): 1098-1105. 10.1097/ALN.0b013e31819fae06.
Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, Slutsky AS, Pullenayegum E, Zhou Q, Cook D, Brochard L, Richard JC, Lamontagne F, Bhatnagar N, Stewart TE, Guyatt G: Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. Jama. 2010, 303 (9): 865-873. 10.1001/jama.2010.218.
Toth I, Leiner T, Mikor A, Szakmany T, Bogar L, Molnar Z: Hemodynamic and respiratory changes during lung recruitment and descending optimal positive end-expiratory pressure titration in patients with acute respiratory distress syndrome. Crit Care Med. 2007, 35 (3): 787-793. 10.1097/01.CCM.0000257330.54882.BE.
Badet M, Bayle F, Richard JC, Guerin C: Comparison of optimal positive end-expiratory pressure and recruitment maneuvers during lung-protective mechanical ventilation in patients with acute lung injury/acute respiratory distress syndrome. Respir Care. 2009, 54 (7): 847-854. 10.4187/002013209793800448.
Fan E, Wilcox ME, Brower RG, Stewart TE, Mehta S, Lapinsky SE, Meade MO, Ferguson ND: Recruitment maneuvers for acute lung injury: a systematic review. Am J Respir Crit Care Med. 2008, 178 (11): 1156-1163. 10.1164/rccm.200802-335OC.
Hodgson CL, Keating JL, Holland AE, Davies AR, Smirneos L, Bradley SJ, Tuxen D: Recruitment manoeuvres for adults with acute lung injury receiving mechanical ventilation. Cochrane Database Syst Rev. 2009, CD006667-2
Brower RG, Morris A, MacIntyre N, Matthay MA, Hayden D, Thompson T, Clemmer T, Lanken PN, Schoenfeld D: Effects of recruitment maneuvers in patients with acute lung injury and acute respiratory distress syndrome ventilated with high positive end-expiratory pressure. Crit Care Med. 2003, 31 (11): 2592-2597.
Meade MO, Cook DJ, Guyatt GH, Slutsky AS, Arabi YM, Cooper DJ, Davies AR, Hand LE, Zhou Q, Thabane L, Austin P, Lapinsky S, Baxter A, Russell J, Skrobik Y, Ronco JJ, Stewart TE, Lung Open Ventilation Study Investigators: Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008, 299 (6): 637-645. 10.1001/jama.299.6.637.
Lim S-C, Adams AB, Simonson DA, Dries DJ, Broccard AF, Hotchkiss JR, Marini JJ: Intercomparison of recruitment maneuver efficacy in three models of acute lung injury. Crit Care Med. 2004, 32 (12): 2371-2377. 10.1097/01.CCM.0000147445.73344.3A.
Hodgson CL, Tuxen DV, Holland AE, Pilcher D, Bailey M, Varma D, Thomson K, Keating JL: A positive response to a recruitment maneuver with PEEP titration in patients with ARDS, regardless of transient oxygen desaturation during the maneuver. JICM. 2011, 26: 41-49.
Borges JB, Okamoto VN, Matos GF, Caramez MP, Arantes PR, Barros F, Souza CE, Victorino JA, Kacmarek RM, Barbas CS, Carvalho CR, Amato MB: Reversibility of lung collapse and hypoxemia in early acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006, 174 (3): 268-278. 10.1164/rccm.200506-976OC.
Higgins BD, Costello J, Contreras M, Hassett P, D OT, Laffey JG: Differential effects of buffered hypercapnia versus hypercapnic acidosis on shock and lung injury induced by systemic sepsis. Anesthesiology. 2009, 111 (6): 1317-1326. 10.1097/ALN.0b013e3181ba3c11.
Laffey JG, Honan D, Hopkins N, Hyvelin JM, Boylan JF, McLoughlin P: Hypercapnic acidosis attenuates endotoxin-induced acute lung injury. Am J Respir Crit Care Med. 2004, 169 (1): 46-56.
Laffey JG, Tanaka M, Engelberts D, Luo X, Yuan S, Tanswell AK, Post M, Lindsay T, Kavanagh BP: Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Am J Respir Crit Care Med. 2000, 162 (6): 2287-2294.
The Acute Respiratory Distres Syndrome Network: Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lng injury and the acute respiratory distress syndrome. New Eng J of Med. 2002, 342: 1301-1309.
Artigas A, Bernard GR, Carlet J, Dreyfuss D, Gattinoni L, Hudson L, Lamy M, Marini JJ, Matthay MA, Pinsky MR, et al: The American-European Consensus Conference on ARDS. Am J Resp Crit Care Med. 1998, 157 (4 Pt 1): 1332-1347.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992, 101 (6): 1644-1655. 10.1378/chest.101.6.1644.
Bone RC, Sibbald WJ, Sprung CL: The ACCP-SCCM consensus conference on sepsis and organ failure. Chest. 1992, 101 (6): 1481-1483. 10.1378/chest.101.6.1481.
Bone RC, Sprung CL, Sibbald WJ: Definitions for sepsis and organ failure. Crit Care Med. 1992, 20 (6): 724-726.
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R: The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994, 149 (3 Pt 1): 818-824.
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, LeGall JR, Morris A, Spragg R: Report of the American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. The Consensus Committee. Intensive Care Med. 1994, 20 (3): 225-232. 10.1007/BF01704707.
Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, Lefrant JY, Prat G, Richecoeur J, Nieszkowska A, Gervais C, Baudot J, Bouadma L, Brochard L, Expiratory Pressure (Express) Study Group: Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008, 299 (6): 646-655. 10.1001/jama.299.6.646.
Kacmarek RM, Kallet RH: Respiratory controversies in the critical care setting. Should recruitment maneuvers be used in the management of ALI and ARDS?. Respir Care. 2007, 52 (5): 622-631.
Acknowledgements
We would like to thank the dedicated medical, nursing and physiotherapy staff in ICU at The Alfred Hospital, Melbourne, who kindly assisted with this study. We would also like to thank Shirley Vallance, Jasmin Board and Victoria Bennett for their assistance with patient screening and Cristina Morganti-Kossmann and Edwin Yan from the National Trauma Research Institute for their assistance with cytokine analysis. We appreciate the support of the Australian and New Zealand Intensive Care Society Clinical Trials Group, Australian and New Zealand College of Anaesthetists, The Intensive Care Foundation and The Alfred Hospital, Australia.
Support for this work was from the Alfred Hospital Research Trust, Intensive Care Foundation, Australian and New Zealand College of Anaesthetists, National Health and Medical Research Council (Scholarship).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
CH, AN and DT conceived and participated in the design of the study, collected the data, and drafted the manuscript. JC and AD conceived of the study, participated in its design and coordination, and manuscript preparation. AW and DP collected data and participated in the manuscript preparation. MB participated in the manuscript preparation and data analysis. JK and AEH and AMH participated in study design, and manuscript preparation. CH and AN coordinated the study. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hodgson, C.L., Tuxen, D.V., Davies, A.R. et al. A randomised controlled trial of an open lung strategy with staircase recruitment, titrated PEEP and targeted low airway pressures in patients with acute respiratory distress syndrome. Crit Care 15, R133 (2011). https://doi.org/10.1186/cc10249
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc10249