Statement of findings
We assessed the association between a glutamine repeat polymorphism in AIB1 and breast cancer risk in a case-control study (464 cases, 624 controls) nested within the Nurses' Health Study cohort. We observed no association between AIB1 genotype and breast cancer incidence, or specific tumor characteristics. These findings suggest that AIB1 repeat genotype does not influence postmenopausal breast cancer risk among Caucasian women in the general population.
Similar content being viewed by others
Synopsis
Introduction
A causal association between endogenous and exogenous estrogens and breast cancer has been established. Steroid hormones regulate the expression of proteins that are involved in breast cell proliferation and development after binding to their respective steroid hormone receptors. Coactivator and corepressor proteins have recently been identified that interact with steroid hormone receptors and modulate transcriptional activation [1]. AIB1 (amplified in breast 1) is a member of the steroid receptor coactivator (SRC) family that interacts with estrogen receptor (ER)α in a ligand-dependent manner, and increases estrogen-dependent transcription [2]. Amplification and overexpression of AIB1 has been observed in breast and ovarian cancer cell lines and in breast tumors [2,3]. A polymorphic stretch of glutamine amino acids, with unknown biologic function, has recently been described in the carboxyl-terminal region of AIB1 [4]. Among women with germline BRCA1 mutations, significant positive associations were observed between AIB1 alleles with 26 or fewer glutamine repeats and breast cancer risk [5]
Aim
To establish whether AIB1 repeat alleles are associated with breast cancer risk and specific tumor characteristics among Caucasian women.
Patients and methods
We evaluated associations prospectively between AIB1 alleles and breast cancer risk in the Nurses' Health Study using a nested case-control design. The Nurses' Health Study was initiated in 1976, when 121 700 US-registered nurses between the ages of 30 and 55 years returned an initial questionnaire reporting medical histories and baseline health-related exposures. Between 1989 and 1990 blood samples were collected from 32 826 women. Eligible cases in this study consisted of women with pathologically confirmed incident breast cancer from the subcohort who gave a blood specimen. Cases with a diagnosis anytime after blood collection up to June 1, 1994, with no previously diagnosed cancer except for nonmelanoma skin cancer were included. Controls were randomly selected participants who gave a blood sample and were free of diagnosed cancer (except nonmelanoma skin cancer) up to and including the interval in which the cases were diagnosed, and were matched to cases on year of birth, menopausal status, postmenopausal hormone use, and time of day, month and fasting status at blood sampling. The nested case-control study consisted of 464 incident breast cancer cases and 624 matched controls. The protocol was approved by the Committee on Human Subjects, Brigham and Womens' Hospital, Boston, Massachusetts USA. Information regarding breast cancer risk factors was obtained from the 1976 baseline questionnaire, subsequent biennial questionnaires, and a questionnaire that was completed at the time of blood sampling. Histopathologic characteristics, such as stage, tumor size and ER and progesterone receptor (PR) status, were ascertained from medical records when available and used in case subgroup analyses.
AIB1 repeat alleles were determined by automated fluorescence-based fragment detection from polymerase chain reaction (PCR)-amplified DNA extracted from peripheral blood lymphocytes. Fluorescent 5' -labeled primers were utilized for PCR amplification, and glutamine repeat number discrimination was performed using the ABI Prism 377 DNA Sequencer (Perkin-Elmer, Foster City, CA, USA). Genotyping was performed by laboratory personnel who were blinded to case-control status, and blinded quality control samples were inserted to validate genotyping identification procedures (n = 110); concordance for the blinded samples was 100%. Methods regarding plasma hormone assays have previously been reported [6]. Conditional and unconditional logistic regression models, including terms for the matching variables and other potential confounders, were used to assess the association of AIB1 alleles and breast cancer characterized by histologic subtype, stage of disease, and ER and PR status. We also evaluated whether breast cancer risk associated with AIB1 genotype differed within strata of established breast cancer risk factors, and whether repeat length in AIB1 indirectly influenced plasma hormone levels.
Results
The case-control comparisons of established breast cancer risk factors among these women have previously been reported [7], and are generally consistent with expectation. The mean age of the women was 58.3 (standard deviation [SD] 7.1) years, ranging from 43 to 69 years at blood sampling. There were 188 premenopausal and 810 postmenopausal women, with mean ages of 48.1 (SD 2.8) years and 61.4 (SD 5.0) years, respectively, at blood sampling. Women in this study were primarily white; Asians, African-Americans and Hispanics comprised less than 1% of cases or controls.
The distribution of AIB1 glutamine repeat alleles and AIB1 genotypes for cases and controls are presented in Table 1. Women with AIB1 alleles of 26 glutamine repeats or fewer were not at increased risk for breast cancer (odds ratio [OR] 1.01, 95% confidence interval [CI] 0.75-1.36; Table 2). Results were also similar by menopausal status and in analyses additionally adjusting for established breast cancer risk factors. Among premenopausal women, the OR for women with at least one allele with 26 glutamine repeats or fewer was 0.82 (95% Cl 0.37-1.81), and among postmenopausal women the OR was 1.09 (95% Cl 0.78-1.52; Table 2). We did not observe evidence of a positive association between shorter repeat length and advanced breast cancer, defined as women with breast cancer having one or more involved nodes (OR 1.07, 95% Cl 0.64-1.78), or with cancers with a hormone-dependent phenotype (ER-positive: OR 1.16, 95% Cl 0.81-1.65; Table 3). No associations were observed among women who had one or more alleles with 26 glutamine repeats or fewer, with or without a family history of breast cancer (family history: OR 1.09; 95% Cl 0.46-2.58; no family history: OR 0.94; 95% Cl 0.68-1.31; test for interaction P = 0.65). We also did not observe associations with breast cancer risk to be modified by other established breast cancer risk factors. Among postmenopausal controls not using postmenopausal hormones, geometric least-squared mean plasma levels of estrone sulfate and estrone were similar among carriers and noncarriers of AIB1 alleles with 26 glutamine repeats or fewer (both differences: ≤ +3.5%; P >0.50). Mean levels of estradiol were slightly, but nonsignificantly elevated among carriers of alleles with 26 glutamine repeats or fewer (+11.6%; P = 0.08).
Discussion
In this population-based nested case-control study, women with at most 26 repeating glutamine codons (CAG/CAA) within the carboxyl terminus of AIB1 were not at increased risk for breast cancer. We did not observe shorter repeat alleles to be positively associated with breast cancer grouped by histologic subtype, stage of disease, or by ER and PR status. These data suggest that AIB1 repeat length is not a strong independent risk factor for postmenopausal breast cancer, and does not modify the clinical presentation of the tumor among Caucasian women in the general population.
Introduction
A causal association between endogenous and exogenous estrogens and breast cancer development has been established [6,8,9]. Variant alleles of candidate genes involved in steroid hormone production (eg CYP17, CYP19 and 17β -HSD) [7,10,11,12,13] and polymorphic variants in steroid hormone receptors (eg ERα, PR and AR) [14,15,16,17] are currently being evaluated as potential high prevalence, low penetrance markers of breast cancer risk. Women with biologically functional polymorphisms in these genes may be exposed to increased levels of circulating steroid hormones or enhanced activity of hormone-responsive genes, and thus have altered susceptibility to steroid hormone-associated cancers.
Steroid hormones regulate the expression of proteins that are involved in breast cell proliferation and development after binding to their respective steroid hormone receptors. Coactivator and corepressor proteins have recently been identified that interact with steroid hormone receptors and modulate transcriptional activation [1]. AIB1 is a member of the SRC family that interacts with ERα in a ligand-dependent manner and increases estrogen-dependent transcription [2]. Amplification and over-expression of AIB1 has been observed in breast and ovarian cancer cell lines and in breast tumors [2,3]. A polymorphic stretch of glutamine amino acids, with unknown biologic function, has recently been described in the carboxyl-terminal region of AIB1 [4]. The androgen receptor has a similar polymorphic glutamine region, and shorter repeat lengths have been associated with increased risk of prostate cancer [18]. Among women with germline BRCA1 mutations, significant positive associations were observed between AIB1 alleles of 26 or fewer glutamine repeats and breast cancer risk [5].
The goal of the present study was to establish whether AIB1 repeat alleles are associated with breast cancer risk among Caucasian women. We evaluated associations prospectively between AIB1 alleles and breast cancer risk in the Nurses' Health Study using a nested case-control design. We investigated potential interactions between AIB1 alleles and established breast cancer risk factors, and whether specific repeat alleles may provide a growth advantage for the developing malignancy and thus be associated with histopathologic tumor characteristics. We also examined whether repeat length in AIB1 indirectly influences plasma hormone levels.
Patients and methods
Study population
The Nurses' Health Study was initiated in 1976, when 121 700 US-registered nurses between the ages of 30 and 55 years returned an initial questionnaire reporting medical histories and baseline health-related exposures. Updated information has been obtained by questionnaire every 2 years, including data on reproductive variables, and oral contraceptive and postmenopausal hormone use. Incident breast cancers are identified by self-report and confirmed by medical record review. Between 1989 and 1990, blood samples were collected from 32 826 women. Approximately 97% of the blood samples were returned within 26 h of being drawn, immediately centrifuged, aliquoted into plasma, red blood cells and buffy coat fractions, and stored in liquid nitrogen freezers. Subsequent follow up has been greater than 98% for this subcohort.
Eligible cases in this study consisted of women with pathologically confirmed incident breast cancer from the subcohort who gave a blood specimen. Cases with a diagnosis anytime after blood collection up to June 1, 1994, with no previously diagnosed cancer except for nonmelanoma skin cancer were included. Controls were randomly selected participants who gave a blood sample and were free of diagnosed cancer (except nonmelanoma skin cancer) up to and including the interval in which the cases were diagnosed. Controls were matched to cases on year of birth, menopausal status, postmenopausal hormone use, and time of day, month and fasting status at blood sampling. Women were defined as postmenopausal at the time of a bilateral oophorectomy or after having no menstrual cycle within the past 12 months before blood sampling. Women who had had a hysterectomy with one or both ovaries left intact were classified as pre-menopausal until the age at which 10% of the cohort had undergone natural menopause (46 years for smokers and 48 years for nonsmokers), and as postmenopausal at the age at which 90% of the cohort had undergone natural menopause (54 for smokers and 56 for nonsmokers). During the intervening years these women were classified as being of uncertain menopausal status.
For postmenopausal cases not using postmenopausal hormones within 3 months before blood sampling, we matched a second control to increase our statistical power in plasma steroid hormone analyses. The nested case-control study consisted of 464 incident breast cancer cases and 624 matched controls. The study sample for the plasma hormone analysis was comprised of 298 postmenopausal controls not using hormone replacement therapy within 3 months of blood sampling.
The protocol was approved by the Committee on Human Subjects, Brigham and Womens' Hospital, Boston, Massachusetts, USA.
Exposure data
Information regarding breast cancer risk factors was obtained from the 1976 baseline questionnaire, subsequent biennial questionnaires, and a questionnaire completed at the time of blood sampling. Menopausal status and use of postmenopausal hormones was assessed at blood sampling, and was updated until date of diagnosis for cases and the equivalent date for matched controls. Histopathologic characteristics such as stage, tumor size, and ER and PR status were ascertained from medical records when available, and used in case subgroup analyses.
Genotyping analysis
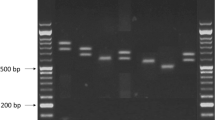
DNA was extracted from buffy coat fractions using the Qiagen QIAamp® Blood Kit (Qiagen Incorporated, Chatsworth, CA, USA). AIB1 genotyping was performed as follows. PCR amplification of the polymorphic fragment was generated using the following primers: 5'-TTCCGACAACAGAGGGTGG-3' (forward) and 5'-AGTCACATTAGGTGGGC-3' (reverse). Forty nanograms of genomic DNA was used per 22 μ l reaction with 1.7 μ l of each 10 μ mol/l primer, 4 μ l of 10 μ mol/l dNTPs, 2.2 μ l 10 × PCR buffer, 9.0 μ l water and 1.50 U Taq polymerase (Qiagen Incorporated). Amplification conditions were 2 min of initial denaturation at 94°C followed by 35 cycles of 30 s at 94°C, 90 s at 60°C and 30 s at 72°C, followed by a final extension at 72°C for 8 min. Two fluorescent 5' -labeled primers were utilized, allowing two samples per lane. A 5% Long Ranger/6 mol/l urea gel (Biowhittaker Molecular Applications, Rockland, ME, USA) was used for rapid fragment detection using the ABI Prism 377 DNA Sequencer (Perkin-Elmer, Foster City, CA, USA) at the Dana Farber Cancer Institute Molecular Biology Core Facility and the Harvard Center for Cancer Prevention, Boston, MA, USA. The size of the amplified products was determined relative to an internal size standard using Genescan and Genotyper Analysis software (Perkin-Elmer). Genotyping was performed by laboratory personnel who were blinded to case-control status, and blinded quality control samples were inserted to validate genotype identification procedures (n =110); concordance for the blinded samples was 100%.
Hormone analysis
Steroid hormone fractions of estrone sulfate, estrone and estradiol were assayed in up to three separate batches. Estrone sulfate from batches 1 and 2 were assayed in the laboratory of Dr C Longcope (University of Massachusetts Medical Center, Worcester, MA, USA). All other analyses were performed by at the Nichols Institute (San Juan Capistrano, CA, USA). Methods for plasma hormone assays and information regarding laboratory precision and reproducibility have previously been published [6,19]. Within-batch laboratory coefficients of variation were 13.6% or less.
Statistical analysis
A Mantel-Haenszel χ2-test across matched case-control sets was used to evaluate differences in the frequency of alleles with 26 repeats or fewer. ORs and 95% CIs were calculated using conditional and unconditional logistic regression. In addition to the matching variables, we adjusted for the following breast cancer risk factors: body mass index (kg/m2) at age 18 years (continuous); weight gain since age 18 years (< 5, 5-19.9, or ≥ 20 kg); age at menarche (< 12, 12, 13, or > 13 years); parity/age at first birth (nulliparous, one to two children/age at first birth ≤ 24 years, one to two children/age at first birth > 24 years, three or more children/age at first birth ≤ 24 years, three or more children/age at first birth > 24 years); first-degree family history of breast cancer (yes/no); history of benign breast disease (yes/no); and duration of postmenopausal hormone use (never; in the past for < 5 or ≥ 5 years; or current for < 5 years or ≥ 5 years). We also adjusted for age at menopause (years) in analyses limited to post-menopausal women.
To be consistent with prior studies [5], indicator variables for three AIB1 genotypes were created: two alleles with 26 repeats or fewer, one allele with 26 repeats or fewer, and two alleles with more than 26 repeats (reference group). We also evaluated breast cancer risk for specific AIB1 genotypes (28/29, 28/28, 26/29, 26/28 and 26/26) relative to 29/29 homozygotes. Unconditional logistic regression models, including terms for the matching variables and other potential confounders, were used to assess the association between AIB1 alleles and breast cancer characterized by histologic subtype, stage of disease, and ER and PR status. To increase statistical power, all controls were utilized when cases were limited to clinical parameters and histologic subtypes. We also evaluated whether breast cancer risk associated with AIB1 genotype differed between strata of established breast cancer risk factors. Because of the low prevalence of genotypes with both alleles with 26 glutamine repeats or fewer, in stratified analyses carriers of alleles with 26 repeats or fewer were compared with noncarriers. Multiplicative interactions were evaluated by including interaction terms between genotype and risk factor variables in logistic regression models. The likelihood ratio test was used to assess the statistical significance of these interactions.
Mixed regression models for clustered data were used to evaluate the association between genotype and circulating hormone levels among postmenopausal controls, controlling for body mass index at blood sampling and the matching variables [20]. The natural logarithms of the plasma hormone values were used in the analyses to reduce the skew of the regression residuals. Information regarding outlying values and exclusions were previously reported [7]. We used the Statistical Analysis System for all analyses [21].
Results
AIB1genotype and breast cancer risk
The case-control comparisons of established breast cancer risk factors among the women studied have previously been published [7], and are generally consistent with expectation. The mean age of the women was 58.3 (SD 7.1) years, ranging from 43 to 69 years at blood sampling. There were 188 premenopausal and 810 post-menopausal women, with mean ages of 48.1 (SD 2.8) years and 61.4 (SD 5.0) years, respectively, at blood sampling. Women in this study were primarily white; Asians, African-Americans and Hispanics comprised less than 1% of cases or controls.
The distribution of AIB1 glutamine repeat alleles and AIB1 genotypes for cases and controls are presented in Table 1. In this study we observed alleles of 19, 22, 25, 26, 27, 28, 29, 30, 31 and 34 repeats, and the expected genotype frequencies, based on the allele frequencies among the cases and controls, were similar to the observed distributions. The allele frequencies were nearly identical for cases and controls; the most prevalent alleles were of 29 (cases 46.4%, controls 47.8%), 28 (cases 40.4%, controls 38.9%), and 26 (cases 12.0%, controls 11.9%) repeats. Average repeat lengths were also the same for cases and controls (cases 28.2, controls 28.2). Twenty-six-repeat allele homozygotes and heterozygotes were evenly distributed among cases and controls (26/26 homozygotes: cases 1.9%, controls 1.6%; 26/X heterozygotes: cases 20.0%; controls 20.5%). A cutoff point of 26 repeats or fewer was used to allow comparison with previously published data [5]. Using this cutoff point, allele frequencies were almost identical for cases and controls (one or more alleles of 26 repeats or fewer: 12.1% versus 12.2%; P = 0.82).
Women with 26 repeats or fewer were not at increased risk for breast cancer; compared with noncarriers, the adjusted OR for carriers of alleles with 26 repeats or fewer was 1.01 (95% Cl 0.75-1.36; Table 2). Compared with noncarriers, the adjusted ORs for heterozygotes and homozygotes for alleles with 26 repeats or fewer were 0.99 (95% Cl 0.73-1.35) and 1.29 (95% Cl 0.52-3.23), respectively. Results were also similar by menopausal status and when adjusting for established breast cancer risk factors. Among premenopausal women, the OR for women with at least one allele with 26 repeats or fewer was 0.82 (95% Cl 0.37-1.81), and among post-menopausal women the corresponding OR was 1.09 (95% Cl 0.78-1.52). Compared with 29/29 homozygotes, no significant associations were observed for specific genotypes with alleles of 26 repeats (Table 2).
AIB1genotype and tumor characteristics
In analyses by histologic subtype, results were similar when limiting cases to those with invasive disease, or advanced stage of disease as characterized by number of involved lymph nodes, tumor size, and type of carcinoma (ductal versus lobular; Table 3). Results were also similar after adjustment for established breast cancer risk factors. A positive association was observed between short repeat alleles and poorly differentiated tumors, but this was not statistically significant (OR 1.54, 95% Cl 0.90-2.64). We did not observe evidence that shorter AIB1 alleles were associated with a hormone-dependent phenotype. In case-case analyses, alleles with 26 repeats or fewer were not over-represented among cases that were positive for the ER or PR (ER-positive versus ER-negative: 24% [61/250] versus 21% [12/58], two-tailed Fisher's Exact Test [FET] P = 0.61; PR-positive versus PR-negative: 24% [45/187] versus 22% [24/110], two-tailed FET P = 0.78).
AIB1genotype-breast cancer risk factor interactions
Because the data of Rebbeck et al [5] suggested that breast cancer risk associated with carrying a germline BRCA1 mutation may be modified by AIB1 allele status, we examined the potential interaction between genotype and a first-degree family history of breast cancer. In case-case analyses, women with at least one repeat allele of 26 repeats or fewer were nonsignificantly over-represented among cases with a family history of breast cancer (family history versus no family history: 23/83 [27.7%] versus 80/381 [21.0%]; two-tailed FET P = 0.19). However, in the nested case-control study there was no difference in association between women with one or more repeat alleles of 26 or fewer repeats with or without a family history of breast cancer (family history: OR 1.09, 95% Cl 0.46-2.58; no family history: OR 0.94, 95% Cl 0.68-1.31; test for interaction P = 0.58).
We evaluated other potential interactions between breast cancer risk factors and AIB1 alleles with 26 repeats or fewer. We observed no interactions between short repeat alleles and the following variables (P values represent tests for interaction): body mass index among post-menopausal women (P = 0.89), weight gain since age 18 years (P = 0.41), history of benign breast disease (P = 0.20), age at menarche (P = 0.24), age at first birth (P = 0.89) and parity (P = 0.18). We also stratified by oral contraceptive and postmenopausal hormone use status. The adjusted ORs for women who had ever and never used oral contraceptives were 0.75 (95% Cl 0.48-1.18) and 1.22 (95% Cl 0.79-1.89), respectively (test for interaction P = 0.14). No significant interaction was seen between carriers of alleles with 26 repeats or fewer and postmenopausal hormone use (test for interaction P = 0.41). The OR for alleles with 26 repeats or fewer among postmenopausal women who had never used hormones was 0.87 (95% Cl 0.45-1.66). Similar results were observed among past users (OR 1.18, 95% Cl 0.56-2.47) and current users of short duration (< 5 years; OR 1.16, 95% Cl 0.44-3.07). A borderline significant association was observed among current users who used postmenopausal hormones for 5 or more years (OR 1.98, 95% Cl 0.96-4.07).
AIB1genotype and hormone levels
Geometric least-squared mean plasma levels of estrone sulfate and estrone were similar among carriers and non-carriers of AIB1 alleles of 26 repeats or fewer (both differences ≤ +3.5%, P > 0.50). Mean levels of estradiol were slightly, but not significantly elevated among carriers of alleles with 26 repeats or fewer (+11.6%; P = 0.08). In analyses among cases the absolute differences were greater for carriers of alleles with 26 repeats or fewer (estrone sulfate: +18.5%, P = 0.21; estrone: +14.9%, P = 0.10; estradiol: +25.0%, P = 0.02).
Discussion
In the present population-based nested case-control study, women with 26 or fewer repeating glutamine codons (CAG/CAA) within the carboxyl terminus of AIB1 were not at increased risk for breast cancer. We did not observe shorter repeat alleles to be positively associated with breast cancer, as defined by histologic subtype or stage of disease, or by ER and PR status. We also did not observe evidence that risk associated with AIB1 allele status is modified by established breast cancer risk factors.
Coregulators of gene transcription modulate transactivation of hormone-responsive genes through interactions with transcription factors and steroid hormone receptors [1]. Members of the SRC family share similar functional domains, including a glutamine-rich domain within the carboxyl-terminus. Shorter CAG repeat lengths in the androgen receptor are associated with increased transcriptional activation of that receptor [22], and may be a model for the potential biologic significance of the polymorphic repeat in AIB1. The biologic function of this glutamine-rich region is currently unknown, however, and to our knowledge no studies have correlated this AIB1 repeat polymorphism with coactivator activity. Ainzick et al [2] first reported AIB1 gene amplification in 9.5% (10/105) of primary breast cancer specimens, and AIB1 mRNA over-expression in 58% of tumors without AIB1 gene amplification relative to normal mammary epithelium. AIB1 was also found to interact with ERα in a ligand-dependent manner, and transfection of AIB1 increased estrogen-dependent transcription. Bautista et al [3] also observed AIB1 gene amplification in 4.8% (56/1157) of breast and 7.4% (9/122) of ovarian tumors. In that study gene amplification was correlated with larger ER-positive and PR-positive tumors. In a relatively large case-control study (cases n = 581; controls n = 786), Platz et al [23] observed no association between germline AIB1 glutamine repeat length and prostate cancer incidence or stage.
To our knowledge, only one study has examined the association between AIB1 repeat alleles and breast cancer risk. Among a cohort of 366 BRCA1 mutation carriers, Rebbeck et al [5] observed a significant association between AIB1 alleles with 26 repeats or fewer and breast cancer risk (OR 1.9, 95% Cl 1.5-2.9). These results suggest that AIB1 genotypes may accentuate BRCA1-associated breast cancer risk through steroid hormone pathways. We were unable to examine this particular question because the study population we studied was not comprised of women with a high likelihood of carrying a highly penetrant mutation in BRCA1 (ie early-onset cases with an extensive family history of breast cancer - only 18 women had more than one first-degree relative with breast cancer). In the present study the majority of cases were postmenopausal at diagnosis (approximately 77%) and were diagnosed as having breast cancer at a later age (mean 62.7 years). However, the relative risk for shorter allele carriers was actually nonsignificantly reduced among premenopausal women (ie those more likely to carry a BRCA1 mutation). In addition, shorter repeat alleles were not associated with increased risk for breast cancer among women with a first-degree family history of breast cancer.
The strengths of the present study are the relatively large sample size and prospective design. We had high power (99.5% at the 0.05 significance level) to detect a significant relative risk of 2.0 among postmenopausal women, but we had low power (47.1%) to detect the same magnitude of association among premenopausal women. AIB1 genotype may be an important predictor of breast cancer risk among the small proportion of predisposed women with highly penetrant mutations in breast cancer susceptibility genes. However, the present data do not provide evidence to support the hypothesis that AIB1 genotype is involved in the development of postmenopausal breast cancer among Caucasian women in the general population.
References
Chen DJ, Li H: Coactivation and corepression in transcriptional regulation by steroid/nuclear hormone receptors. Crit Rev Eukaryot Gene Expr. 1998, 8: 169-190.
Anzick SL, Konen J, Walker RL, Azorsa DO, Tanner MM, Guan XY, Sauter G, Kallioniemi OP, Trent JM, Meltzer PS: AIB1, a steroid receptor coactivator amplified in breast and ovarian cancer. Science. 1997, 277: 965-968. 10.1126/science.277.5328.965.
Bautista S, Valles H, Walker RL, Anzick S, Zeillinger R, Meltzer P, Theiller C: In breast cancer, amplification of the steroid receptor coactivator gene AIB1 is correlated with estrogen and progesterone receptor positivity. Clin Cancer Res. 1998, 4: 2925-2929.
Shirazi SK, Bober MA, Coetzee GA: Polymorphic exonic CAG microsatellites in the gene amplified in breast cancer (AIB1 gene). Clin Genet. 1998, 54: 102-103.
Rebbeck TR, Kantoff PW, Krithivas K, Neuhausen SL, Blackwood MA, Godwin AK, Daly MB, Narod SA, Garber JE, Lynch HT, Weber BL, Brown MA: Modification of breast cancer risk in BRCA1 mutation carriers by the AIB1 gene [abstract]. Proc Am Assoc Cancer Res. 1999, 40: 194-
Hankinson SE, Willett WC, Manson JE, Colditz GA, Hunter DJ, Spiegelman D, Barbieri RL, Speizer FE: Plasma sex steroid hormone levels and risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 1998, 90: 1292-1299. 10.1093/jnci/90.17.1292.
Haiman CA, Hankinson SE, Spiegelman D, Colditz GA, Willett WC, Speizer FE, Kelsey KT, Hunter DJ: The relationship between a polymorphism in CYP17 with plasma hormone levels and breast cancer. Cancer Res. 1999, 59: 1015-1020.
Colditz GA: Relationship between estrogen levels, use of hormone replacement therapy, and breast cancer risk. J Natl Cancer Inst . 1998, 90: 814-823. 10.1093/jnci/90.11.814.
Bernstein L, Ross RK: Endogenous hormones and breast cancer. Epidemiol Rev. 1993, 15: 48-65.
Feigelson HS, Coetzee GA, Kolonel LN, Ross RK, Henderson BE: A polymorphism in the CYP17 gene increases breast cancer risk. Cancer Res. 1997, 57: 1063-1065.
Kristensen VN, Anderson TI, Linblom L, Erikstein B, Magnus P, Börrensen-Dale AL: A rare CYP19 (aromatase) variant may increase the risk of breast cancer. Pharmacogenetics. 1998, 8: 43-48.
Siegelmann-Danieli N, Buetow KH: Constitutional genetic variation at the human aromatase gene (CYP19) and breast cancer risk. Br J Cancer. 1999, 79: 456-463. 10.1038/sj.bjc.6690071.
Mannermaa A, Peltoketo H, Winqvist R, Ponder BA, Kiviniemi H, Easton DF, Poutanen M, Isomaa V, Vihko R: Human familial and sporadic breast cancer: analysis of the coding regions of the 17 β -hydroxysteroid dehydrogenase 2 gene (EDH17B2) using single-strand conformation polymorphism assay. Hum Genet. 1994, 93: 319-324.
Anderson TI, Heimdal KR, Skrede M, Tveit K, Berg K, Börrensen AL: Oestrogen receptor (ESR) polymorphisms and breast cancer susceptibility. Hum Genet. 1994, 94: 665-670.
Southey MC, Batten LE, McCredie MR, Giles GG, Dite G, Hopper JL, Venter DJ: Estrogen receptor polymorphism at codon 325 and risk of breast cancer in women before age forty. J Natl Cancer Inst. 1998, 90: 532-536. 10.1093/jnci/90.7.532.
Lancaster JM, Berchuck A, Carney ME, Wiseman R, Taylor JA: Progesterone receptor gene polymorphism and risk for breast and ovarian cancer [letter]. Br J Cancer. 1998, 78: 277-
Spurdle AB, Dite GS, Chen X, Mayne CJ, Southey MC, Batten LE, Chy H, Trute L, McCredie MR, Giles GG, Armes J, Venter DJ, Hopper JL, Chenevix-Trench G: Androgen receptor exon 1 CAG repeat length and breast cancer in women before age forty years. J Natl Cancer Inst . 1999, 91: 961-966. 10.1093/jnci/91.11.961.
Giovannucci E, Stampfer MJ, Krithivas K, Brown M, Dahl D, Brufsky A, Talcott J, Hennekens CH, Kantoff PW: The CAG repeat within the androgen receptor gene and its relationship to prostate cancer. Proc Natl Acad Sci USA. 1997, 94: 3320-3323. 10.1073/pnas.94.7.3320.
Hankinson SE, Manson JE, Spiegelson D, Willett WC, Longcope C, Speizer FE: Reproducibility of plasma hormone levels in post-menopausal women over a 2-3-year period. Cancer Epidemiol Bio-markers Prev . 1995, 4: 649-654.
Liang K-Y, Zeger SL: Regression analysis for correlated data. Annu Rev Public Health. 1993, 14: 43-68. 10.1146/annurev.pu.14.050193.000355.
SAS Institute, Incorporated : . SAS Technical Report p-229 SAS/STAT Software. Changes and Enhancements, Release 6.07. 1992
Chamberlain NL, Driver ED, Miesfeld RL: The length and location of CAG trinucleotide repeats in the androgen receptor N-terminal domain affect transactivation function. Nucleic Acids Res. 1994, 22: 3181-3186.
Platz EA, Giovannucci E, Brown M, Cieluch C, Shepard TF, Stampfer MJ, Kantoff PW: Amplified in breast cancer-1 (AIB1) glutamine repeat and prostate cancer risk. Prostate. 2000,
Acknowledgements
We thank Mr Robert O' Brien, Mrs Lisa Li, Mrs Barbara Egan, Mrs Jeanne Sparrow, Mr Tim Shepard and Dr Phillip Kantoff for their technical assistance. We are also indebted to the participants of the Nurses' Health Study for their dedication and commitment. This work is supported by NIH grants CA40356, CA49449 and CA65725. David Hunter is partially supported by an ACS Faculty Research Award, FRA-455, and Myles Brown by NIH grant CA57374.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haiman, C.A., Hankinson, S.E., Spiegelman, D. et al. Polymorphic repeat in AIB1 does not alter breast cancer risk. Breast Cancer Res 2, 378 (2000). https://doi.org/10.1186/bcr82
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/bcr82