Abstract
Introduction
While Cumulus – a semi-automated method for measuring breast density – is utilised extensively in research, it is labour-intensive and unsuitable for screening programmes that require an efficient and valid measure on which to base screening recommendations. We develop an automated method to measure breast density (AutoDensity) and compare it to Cumulus in terms of association with breast cancer risk and breast cancer screening outcomes.
Methods
AutoDensity automatically identifies the breast area in the mammogram and classifies breast density in a similar way to Cumulus, through a fast, stand-alone Windows or Linux program. Our sample comprised 985 women with screen-detected cancers, 367 women with interval cancers and 4,975 controls (women who did not have cancer), sampled from first and subsequent screening rounds of a film mammography screening programme. To test the validity of AutoDensity, we compared the effect estimates using AutoDensity with those using Cumulus from logistic regression models that tested the association between breast density and breast cancer risk, risk of small and large screen-detected cancers and interval cancers, and screening programme sensitivity (the proportion of cancers that are screen-detected). As a secondary analysis, we report on correlation between AutoDensity and Cumulus measures.
Results
AutoDensity performed similarly to Cumulus in all associations tested. For example, using AutoDensity, the odds ratios for women in the highest decile of breast density compared to women in the lowest quintile for invasive breast cancer, interval cancers, large and small screen-detected cancers were 3.2 (95% CI 2.5 to 4.1), 4.7 (95% CI 3.0 to 7.4), 6.4 (95% CI 3.7 to 11.1) and 2.2 (95% CI 1.6 to 3.0) respectively. For Cumulus the corresponding odds ratios were: 2.4 (95% CI 1.9 to 3.1), 4.1 (95% CI 2.6 to 6.3), 6.6 (95% CI 3.7 to 11.7) and 1.3 (95% CI 0.9 to 1.8). Correlation between Cumulus and AutoDensity measures was 0.63 (P < 0.001).
Conclusions
Based on the similarity of the effect estimates for AutoDensity and Cumulus in models of breast density and breast cancer risk and screening outcomes, we conclude that AutoDensity is a valid automated method for measuring breast density from digitised film mammograms.
Similar content being viewed by others
Introduction
Population mammographic screening might be more effective if screening strategies were tailored according to mammographic breast density [1, 2]. Women with high breast density are at higher risk of breast cancer [3] and in population mammographic breast cancer screening programmes they experience reduced screening programme sensitivity (the proportion of cancers that are screen-detected) [4, 5] and larger tumours at diagnosis [5, 6]. This is due to increased cancer risk and because dense areas on mammograms can obscure cancers [4–9].
Specific strategies for tailoring screening according to breast density include adding ultrasound to mammography [10–12], using magnetic resonance imaging (MRI) instead of mammography [13], or more frequent screening of women with high breast density potentially offset by less frequent screening of women with low breast density [2, 14]. Trials of MRI or adjunctive ultrasound for women with dense breasts suggest improvements in cancer detection but increases in false positive rates [10, 15].
Current methods of measuring breast density are not suitable for developing tailored screening strategies because they are manual methods that are time-consuming and have inadequate reliability. In the USA, radiologists routinely use the BI-RADS™ (Breast Imaging Reporting and Data System) visually estimated categories [16], however, this method has limited within-reader reliability (κ = 0.71) and between-reader reliability (κ = 0.54) [17], and it is not sufficiently discriminatory because it has only four categories of breast density and a majority of women (for example 81% [18], or 92% [19]) are classified in the middle two categories.
A widely used computer-assisted method is Cumulus[20]. It measures breast density on a continuous scale and has high between- and within-reader reliability in carefully monitored research settings [21], however, this may not be reliably realised in the routine screening context, and the method is time-consuming and costly in terms of staff time.
If breast density is to be routinely measured in screening programmes, an efficient and high-quality automated method is required. Ideally, trials of alternate screening strategies should be based on such a method so that the evidence can be easily translated into screening programmes.
Several automated measurement methods have recently been published [22–31]. All these methods offer perfect inter-read reliability. Some methods segment the distinctly white tissue (essentially automating the Cumulus approach) [25, 26] while others estimate the underlying volumes of dense and non-dense breast tissue by projecting two-dimensional information onto three-dimensional space [27–30]. Some automated methods have shown associations with breast cancer risk comparable to Cumulus and BI-RADS™ measures [25, 27] but none have yet been validated against important measures of the effectiveness of screening programmes such as programme sensitivity, interval cancer rates and tumour size at diagnosis. Validation of methods against screening outcomes is required because the way that breast density affects breast cancer risk is likely to differ from the way that it affects radiological reading of mammograms.
In this study, we describe an efficient, automated method for measuring breast density and compare it with Cumulus in terms of predicting breast cancer risk, screening programme sensitivity, risk of small and large screen-detected cancers and interval cancers, and tumour size at diagnosis. We utilise an existing study database of BreastScreen Australia film mammograms from screening episodes and their associated Cumulus breast density measurements and clinical and screening data [21, 32, 33].
Methods
Participants
BreastScreen Australia is a free population-based breast screening programme that offers biennial screening to women aged 40 years and above, specifically targeting women aged 50 to 69 years. For this study, the source population comprised all women who attended the BreastScreen Australia programme in the state of Victoria (BreastScreen Victoria), either for first round screening in 1994 or 1995 (and who reported no previous mammogram), or subsequent round screening in 1995 or 1996 (excluding women in the first round sample). Women were eligible for the study if they were 79 years or younger, had no self-reported history of breast cancer and no ‘significant’ breast cancer symptoms at the time of screening (breast lump not examined by a doctor or a blood-stained or watery nipple discharge). We included only women with a Cumulus breast density reading from our previous studies. Our database included updated BreastScreen Victoria data received in October 2005, which resulted in minor changes in the sample available for this analysis compared to our previous publications [21, 32, 33].
Selection of participants followed methods used previously [33], where cases were all eligible women with invasive screen-detected or interval breast cancers (675 screen-detected and 183 interval cancer cases at first round screening and 344 screen-detected and 198 interval cancer cases at subsequent rounds), women diagnosed with ductal carcinoma in situ (DCIS) were not included in the study, and controls consisted of a sample of screened women with no cancer diagnosis (either true-negative or false-positive screening outcomes) selected randomly from both first and subsequent screening rounds (2,051 women from first round screening and 3,267 women from subsequent rounds, corresponding to sampling fractions of 1.55% and 3.25% respectively).
Cancer ascertainment and classification
Screen-detected cancers were recorded by BreastScreen Victoria and interval cancers were identified by linking the population-based Victorian Cancer Registry to BreastScreen Victoria records, providing near-complete ascertainment of interval cancers [21, 34]. Tumour size was recorded as the widest cross-section of the largest lesion as reported in the pathology report. Consistent with national protocols, tumours coded as microinvasive were assigned a size of 0.1 mm and screen-detected cancers were categorised as small (≤15 mm) or large (>15 mm) [34].
Questionnaire data
Participants completed a questionnaire at the time of their screening appointment that included questions on family history of breast cancer (a first-degree relative versus no first-degree relative), current hormone therapy use (yes/no), country of birth and symptoms (none, or no ‘significant’ symptoms defined as any breast symptoms other than a breast lump or blood-stained or watery nipple discharge).
Digitised mammograms
Mammograms were originally taken on a range of analogue (film) mammography machines. Cranio-caudal (CC) views were scanned in the late 1990s using a single digitiser (digitiser specifications and settings not known). Each scanned image included various background artefacts such as tags indicating breast laterality and radiological view, nameplates, and bright borders generated during scanning.
Cumulusmeasurements
Cumulus was used previously to measure breast density from the digitised images, with measurements available for 93% of available cases included in previous analyses [24, 33]. We used measurements from the cancer-affected breast where possible for cases, and from a random side breast for women without cancer as done by others [35]. It is common practice in more recent studies to measure breast density from the contralateral (unaffected) breast for cases to avoid including the tumour in dense tissue estimation [36–39]; however, in practice breast density readings taken from ipsilateral and contralateral breasts have very similar distributions and similar estimates of breast cancer risk prediction [40], and Cumulus measures were highly correlated between breasts within this dataset [21]. Further, for this study we use the same mammogram for Cumulus and AutoDensity readings and so if there was bias in the measurement of exposure (breast density) it would affect both measures equally. The measurements were taken by one of four readers (a radiologist, a radiology registrar, and two research assistants), with high inter- and intra-reader reliability [21].
Automated measurement of breast density
We developed an executable program (‘AutoDensity’) which automatically identifies the breast area in the mammogram (breast segmentation) and then classifies breast density in a similar way to Cumulus by identifying distinctly white tissue to be classified as ‘dense’ (breast density segmentation).
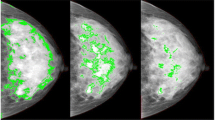
Our approach to dense tissue segmentation does not require standardisation across images; the method finds an optimal threshold for each mammogram independently from any other mammogram in a dataset. We first improved the contrast and reduced the noise of individual images by smoothing the breast area with the median filter of radius one and then applying histogram contrast stretching [41]. Then, to automatically segment dense tissue within the breast area, we modified a recently published method by Kim et al. that had been developed on digital mammograms [42]. This method computes an optimal intensity threshold between dense and fatty tissues, which outlines the dense area on the breast as shown in Figure 1. Our methods are described in more detail in Additional file 1.
Examples of the AutoDensity breast density segmentation process on three cranio-caudal-view digitised film mammograms. Examples shown are from three women with different breast densities, from each of the lowest quintile (Q1), third quintile (Q3) and upper decile (D10) of the population distribution of dense area. For each woman, the breast density segmentation process is illustrated using (A) the input mammogram, (B) the dense area outline, and (C) the dense area mask.
AutoDensity operates on Windows and Linux platforms and takes on average 2.9 seconds per image to produce measurements of breast density. AutoDensity outputs an indexed table of results along with images showing the original mammograms marked up with breast and breast density segmentations.
Statistical analysis
Women were excluded from the analysis if they had any missing data on hormone therapy use at the time of screening, personal history of breast cancer, breast symptoms and family history of breast cancer. Women for whom AutoDensity could not produce breast density readings due to failures in the breast segmentation algorithm to outline the breast area were also excluded.
For all analyses we assessed dense area and percent density measures of breast density. These produced similar associations with outcomes. Evidence is mixed about whether dense area or percent density are stronger predictors of risk [43–45]: we report on dense area as done in our more recent publications [32, 33] (results using percent density are available on request).
Statistical tests for interaction between screening round and breast density were performed for each screening outcome to determine whether the analyses should be conducted separately for first and subsequent screening rounds. There was no evidence of an interaction, therefore we categorised each breast density measure into whole-screened-population percentiles (weighting controls according to study sampling fractions to reproduce whole-population distributions). We then categorised breast density into the four lowest quintiles and the two upper deciles of their distributions (‘quintile-decile groups’) as done for our previous evaluations using Cumulus[32, 33]. Age was categorised into groups 40 to 49, 50 to 54, 55 to 59, 60 to 64, 65 to 69 and 70 to 79 years.
We examined associations of Cumulus and AutoDensity with factors known to be associated with breast density (age, hormone therapy use, region of birth (Australia, Europe/North America, Asia and other), family history of breast cancer, breast symptoms, screening round and clinical outcome (small or large screen-detected cancer, interval cancer, no cancer)). We applied the Cuzick non-parametric test for trends across ordinal categories and Kruskal-Wallis non-parametric tests for differences between nominal groups. To illustrate the observed characteristics of tumours diagnosed in different breast density groups, we plotted histograms of the relative frequency of quintiles of tumour size according to breast density quintiles (using quintile categories due to inadequate power to assess by decile) and mode of detection (screen-detected or interval cancers).
To compare how well Cumulus or AutoDensity could be used to discriminate women’s clinical outcomes based on information from their screening mammograms, we generated receiver operating characteristic (ROC) curves and calculated the area under the curves (AUC). We repeated this exercise for small screen-detected cancers, large screen-detected cancers and interval cancers versus controls, and for interval cancers versus screen-detected cancers.
To assess the association between breast density and clinical outcomes, we conducted a range of analyses including several previously published from this dataset using Cumulus measures [21, 32, 33]. We used unconditional logistic regression to estimate odds ratios of all invasive breast cancers, small screen-detected, large screen-detected and interval cancers (versus no cancer) for quintile-decile groups of breast density. We also modelled the relative odds of an interval cancer (versus a screen-detected cancer) in order to estimate programme sensitivity. All models were adjusted for age, hormone therapy use, family history of breast cancer, symptoms and screening round. Since there was no evidence of an interaction between screening round and breast density, all results are presented for combined screening rounds.
As a secondary analysis, we compared Cumulus and AutoDensity measures by examining pairwise correlation coefficients, scatterplots of percentiles, Bland-Altman plots of agreement and quantile-quantile (Q-Q) plots of a 20% random sample of breast density values, and cross-classification tables of quintile-decile groups (Q-Q plots compare two distributions by plotting their quantiles against each other). All analyses were conducted in Stata 12.1 [46].
Approvals and consent
This study was approved by the University of Melbourne Health Science Human Ethics Sub-Committee (Ethics ID 0932609) on 15 December 2009. All BreastScreen Victoria clients provide signed consent for use of their data for research purposes under the governance of the BreastScreen Victoria Board of Management, which approved this study on 22 September 2009.
Results
We excluded 161 women (2%) in the study group who had missing questionnaire data. A further 247 women (4%) were excluded because AutoDensity failed to segment the breast area of their mammograms. Compared to successful AutoDensity reads, failed AutoDensity reads had higher Cumulus values for breast area (median 260,990 versus 204,084 pixels, t test P < 0.001) and dense area (29,376 versus 26,446 pixels, t test P = 0.08), and lower Cumulus values for percent density (13% versus 15%, t test P = 0.03). There were no failures in the breast density segmentation step.
The final sample for analysis included 6,327 women, comprising 2,818 women from first-round screening (411 small screen-detected cancers, 247 large screen-detected cancers, 174 interval cancers and 1,986 controls) and 3,509 women from subsequent round screening (242 small screen-detected cancers, 85 large screen-detected cancers, 193 interval cancers and 2,989 controls).
Cumulus and AutoDensity were similarly distributed according to age, hormone therapy use, region of birth, breast symptoms, and screening test outcome (Table 1). Histograms of tumour characteristics (size and mode of detection) according to breast density highlighted the shift from predominantly small screen-detected tumours in women with low breast density to larger screen-detected and interval cancers in women with high breast density, for both Cumulus and AutoDensity classifications of breast density (Figure 2).
Distribution of tumour size and mode of detection according to dense area quintiles measured using (A) Cumulus and (B) AutoDensity . Screen-detected and interval cancers (marked as dark and light bars) are shown separately but stacked to indicate the size distribution of all cancers detected in each breast density quintile as well as the relative representation of screen-detected and interval cancers in this distribution. The dashed line represents the expected tumour size distribution within each breast density group if the distribution of tumour size did not vary according to breast density.
ROC curves and their AUCs (Figure 3) showed that Cumulus and AutoDensity had a similar ability to discriminate between women who developed breast cancer and women who did not. Discrimination was strongest between women with interval cancers and controls (for example AUC = 0.66 for AutoDensity) and lowest between small screen-detected cancers and controls (for example AUC = 0.52 for AutoDensity).
Receiver operating characteristic (ROC) curves and area under the curve (AUC) values to assess the discriminatory performance of Cumulus and AutoDensity dense area. ROC curves and AUC values are shown for various outcomes, including (A) all cancers versus controls, (B) small screen-detected cancers versus controls, (C) large screen-detected cancers versus controls, (D) interval cancers versus controls, (E) interval cancers versus screen-detected cancers for first round screening, and (F) interval cancers versus screen-detected cancers for subsequent round screening. Cumulus values are shown in black, AutoDensity values are shown in grey. The dashed line represents no predictive value.
Cumulus and AutoDensity breast density measures showed a similar association with the odds of invasive breast cancers, large-screen detected cancers and interval cancers (Figure 4).
Multivariate logistic regression of cancer risk and screening outcomes according to Cumulus and AutoDensity . Breast density was measured as dense area and categorised into quintile-decile groups. Regression models were adjusted for age, hormone therapy use, family history of breast cancer, symptoms and screening round.
From models of odds ratios of interval versus screen-detected cancers, we predicted similar, graded associations between breast density and screening programme sensitivity for both Cumulus and AutoDensity (Table 2), showing that AutoDensity could differentiate expected programme sensitivity. For example, for women aged 50 to 54 years attending their first screening appointment with no symptoms, hormone therapy or strong family history of breast cancer, a woman in the lowest quintile of AutoDensity had an expected programme sensitivity of 76% (95% confidence interval (CI) 57% to 89%) whereas a woman in the highest decile of AutoDensity had an expected programme sensitivity of 68% (95% CI 46% to 84%).
There was a strong correlation between Cumulus and AutoDensity segmentation of the breast area (r = 0.98, P < 0.001), however the correlation between measures of breast density was modest (r = 0.63, P < 0.001), with discordant values for both low and high values of breast density (Figure 5a). AutoDensity dense area tended to be higher than Cumulus (median 21,293 versus 18,400 pixels), particularly for more dense breasts (Figure 5b and c). Using quintile-decile groups, 41% of Cumulus and AutoDensity breast density measurements were in perfect agreement and 40% were in near agreement (within one neighbouring category) (Figure 5d).
Distribution and variation between Cumulus and AutoDensity . (A) Scatter plot of screened population percentiles of dense area for a 20% random sample of the study group. (B) Bland-Altman plot of agreement between Cumulus and AutoDensity dense area for a 20% random sample of the study group. The x-axis shows the mean value of the Cumulus and AutoDensity measurements for each image, on a log scale. (C) Quantile-quantile plot of dense area percentiles of Cumulus against percentiles of AutoDensity (a deviation from the diagonal indicates a difference in distributions). (D) Cross-classification of quintile-decile groups (%).
Discussion
Automated breast density measurements from film screening mammograms using AutoDensity were comparable to (and often better than) Cumulus in terms of predicting breast cancer risk and key screening programme outcomes (Figure 4).
These findings suggest that AutoDensity is a valid tool for identifying groups of women at increased risk of breast cancer and at high risk of large screen-detected cancers or interval cancers, and therefore most likely to benefit most from more intensive screening modalities such as MRI, adjunctive ultrasound or shorter screening intervals. Quite low AUC values (Figure 3) show that using AutoDensity alone to classify individual women’s risk of various clinical outcomes is of limited benefit (as for Cumulus). As noted in a review paper by Vachon et al. [47], efforts to incorporate breast density into existing breast cancer risk models modestly improve classification of women’s risk but the models remain better suited to identifying risk groups for targeted health services, rather than providing absolute risk estimates to individuals. Breast segmentation was highly correlated between Cumulus and AutoDensity measures (r = 0.98, P < 0.001), showing that AutoDensity can successfully delineate the breast area of interest even in images with complex background features.
As a limitation, automated breast segmentation failed for 4% of mammograms in the dataset; this tended to occur when breast images overlapped with background artefacts or the image border, which was more likely with larger breasts. We are continuing to develop our algorithm to reduce this failure rate.
The correlation between AutoDensity measures and Cumulus was moderate (r = 0.63, P < 0.001), despite each measure showing a similar distribution according to age, hormone therapy use, region of birth, family history of breast cancer, breast symptoms at screening and clinical outcomes (Table 1 and Figure 2). This finding does not reduce the validity of our primary finding that both measures predict breast cancer risk and breast cancer screening outcomes with a similar effect. While Cumulus is in common use, it is not the gold standard measure of breast density: both measures have error in terms of describing the breast composition of dense and fatty tissue. Indeed, further investigation of visual features that produced non-correlated measures may enable further improvement of AutoDensity; this will be the focus of future work.
This study has a number of strengths. We used a large, unique dataset from a well-organised population screening programme that includes interval cancers identified through linkage to the cancer registry and good information on tumour size as well as personal characteristics of screening participants, which enabled us to adjust our models for potential confounders. We assessed an automated method that does not require modifications at the time of image capture as required by some other methods, such as the collection of pre-processed (raw) images from mammography machines [29, 31] or the use of step wedges [27, 30, 31]. AutoDensity is not limited to specific machine brands and models of analogue mammogram machines because it flexibly identifies and removes the range of background artefacts generated by different film cassettes, and it replicates the Cumulus reader-driven approach of classifying as dense tissue the relatively bright components of the breast image. While Cumulus requires trained readers, is time-consuming and would have limited reliability in clinical practice, AutoDensity automatically completes readings in an average of 2.9 seconds, with perfect between-reader reliability (by definition, since it is fully automated). The program generates simple data tables of measurements and output images showing how the program has outlined the breast and the dense tissue.
The study did not include body mass index (BMI), which may modify the association between breast density measures and breast cancer risk [48]; our dataset was limited to information routinely collected by the BreastScreen programme, which does not include BMI; however, the primary aim of this study was to compare effect estimates from AutoDensity and Cumulus in the same models; and any bias in the model arising from excluding BMI should be the same for both breast density measures.
Our current analysis was confined to film mammograms taken during the period 1994 to 1996, utilising a large research dataset with existing Cumulus readings. AutoDensity is likely to be useful for research studies that require breast density estimation from older film mammograms, such as studies of long-term breast cancer risk. However, many screening services have adopted or will soon migrate to digital mammography. The breast density segmentation method implemented in this study was originally developed on digital mammograms and so it will need little modification for digital mammography; future work will aim to validate AutoDensity on data from BreastScreen Australia digital mammography services.
Conclusions
This study demonstrates that, despite only modest correlation with Cumulus measures, automated measurement of breast density from digitised screening mammograms using AutoDensity performs similarly to Cumulus in terms of helping to identify groups of screening participants known to be at higher risk of breast cancer, interval and large screen-detected cancers, lower programme sensitivity, and larger tumour size at diagnosis. AutoDensity is a fast, stand-alone Windows or Linux program that is a validated breast density measurement tool suitable for digitised film mammograms.
Abbreviations
- AUC:
-
Area under the curve
- BI-RADS:
-
Breast imaging reporting and data system™
- BMI:
-
Body mass index
- CC:
-
Cranio-caudal
- CI:
-
Confidence interval
- DCIS:
-
Ductal carcinoma in situ
- MRI:
-
Magnetic resonance imaging
- Q-Q plots:
-
Quantile-quantile plots
- ROC:
-
Receiver operating characteristic.
References
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, Jong RA, Hislop G, Chiarelli A, Minkin S, Yaffe MJ: Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007, 356: 227-236. 10.1056/NEJMoa062790.
BreastScreen Australia evaluation: mortality (ecological) study. Screening Monograph No 4/2009. Prepared by the National Breast and Ovarian Cancer Centre for the Australian Government Department of Health and Ageing. 2009, Canberra: Australian Government
McCormack VA, dos Santos Silva I: Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006, 15: 1159-1169. 10.1158/1055-9965.EPI-06-0034.
van Gils CH, Otten JD, Verbeek AL, Hendriks JH, Holland R: Effect of mammographic breast density on breast cancer screening performance: a study in Nijmegen, The Netherlands. J Epidemiol Community Health. 1998, 52: 267-271. 10.1136/jech.52.4.267.
Mandelson MT, Oestreicher N, Porter PL, White D, Finder CA, Taplin SH, White E: Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst. 2000, 92: 1081-1087. 10.1093/jnci/92.13.1081.
Sala E, Solomon L, Warren R, McCann J, Duffy S, Luben R, Day N: Size, node status and grade of breast tumours: association with mammographic parenchymal patterns. Eur Radiol. 2000, 10: 157-161. 10.1007/s003300050025.
Sala E, Warren R, McCann J, Duffy S, Day N, Luben R: Mammographic parenchymal patterns and mode of detection: implications for the breast screening programme. J Med Screen. 1998, 5: 207-212. 10.1136/jms.5.4.207.
Ma L, Fishell E, Wright B, Hanna W, Allan S, Boyd NF: Case–control study of factors associated with failure to detect breast cancer by mammography. J Natl Cancer Inst. 1992, 84: 781-785. 10.1093/jnci/84.10.781.
Kolb TM, Lichy J, Newhouse JH: Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: an analysis of 27,825 patient evaluations. Radiology. 2002, 225: 165-175. 10.1148/radiol.2251011667.
Corsetti V, Houssami N, Ghirardi M, Ferrari A, Speziani M, Bellarosa S, Remida G, Gasparotti C, Galligioni E, Ciatto S: Evidence of the effect of adjunct ultrasound screening in women with mammography-negative dense breasts: interval breast cancers at 1 year follow-up. Eur J Cancer. 2011, 47: 1021-1026. 10.1016/j.ejca.2010.12.002.
Nothacker M, Duda V, Hahn M, Warm M, Degenhardt F, Madjar H, Weinbrenner S, Albert US: Early detection of breast cancer: benefits and risks of supplemental breast ultrasound in asymptomatic women with mammographically dense breast tissue. A systematic review. BMC Cancer. 2009, 9: 335-10.1186/1471-2407-9-335.
Buchberger W, Niehoff A, Obrist P, DeKoekkoek-Doll P, Dunser M: Clinically and mammographically occult breast lesions: detection and classification with high-resolution sonography. Semin Ultrasound CT MR. 2000, 21: 325-336. 10.1016/S0887-2171(00)90027-1.
Benndorf M, Baltzer PA, Vag T, Gajda M, Runnebaum IB, Kaiser WA: Breast MRI as an adjunct to mammography: Does it really suffer from low specificity? A retrospective analysis stratified by mammographic BI-RADS classes. Acta Radiol. 2010, 51: 715-721. 10.3109/02841851.2010.497164.
Nickson C, Watson R, Kavanagh AM: A microsimulation model of the BreastScreen Australia program. Proceedings of the 18th World IMACS Congress and MODSIM09 International Congress on Modelling and Simulation Modelling and Simulation Society of Australia and New Zealand and International Association for Mathematics and Computers in Simulation: 13-17 July 2009; Cairns. Edited by: Anderssen RS, Braddock RD, Newham LTH. 2009, 164-170.
Berg WA, Zhang Z, Lehrer D, Jong RA, Pisano ED, Barr RG, Bohm-Velez M, Mahoney MC, Evans WP, Larsen LH, Narayanan D, Kalinyak JE: Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012, 307: 1394-1404. 10.1001/jama.2012.388.
American College of Radiology: Illustrated breast imaging reporting and data system (BI-RADS™). 1998, Reston, VA: American College of Radiology, 3
Ciatto S, Houssami N, Apruzzese A, Bassetti E, Brancato B, Carozzi F, Catarzi S, Lamberini MP, Marcelli G, Pellizzoni R, Pesce B, Risso G, Russo F, Scorsolini A: Categorizing breast mammographic density: intra- and interobserver reproducibility of BI-RADS density categories. Breast. 2005, 14: 269-275. 10.1016/j.breast.2004.12.004.
Kerlikowske K, Cook AJ, Buist DS, Cummings SR, Vachon C, Vacek P, Miglioretti DL: Breast cancer risk by breast density, menopause, and postmenopausal hormone therapy use. J Clin Oncol. 2010, 28: 3830-3837. 10.1200/JCO.2009.26.4770.
Venta LA, Hendrick RE, Adler YT, DeLeon P, Mengoni PM, Scharl AM, Comstock CE, Hansen L, Kay N, Coveler A, Cutter G: Rates and causes of disagreement in interpretation of full-field digital mammography and film-screen mammography in a diagnostic setting. AJR Am J Roentgenol. 2001, 176: 1241-1248. 10.2214/ajr.176.5.1761241.
Byng JW, Boyd NF, Fishell E, Jong RA, Yaffe MJ: The quantitative analysis of mammographic densities. Phys Med Biol. 1994, 39: 1629-1638. 10.1088/0031-9155/39/10/008.
Kavanagh AM, Cawson J, Byrnes GB, Giles GG, Marr G, Tong B, Gertig DM, Hopper JL: Hormone replacement therapy, percent mammographic density, and sensitivity of mammography. Cancer Epidemiol Biomarkers Prev. 2005, 14: 1060-1064. 10.1158/1055-9965.EPI-04-0165.
de Melo R, Vieira E, Conci A, Enyedi B, Reichardt A: Comparing two approaches to compute lacunarity of mammograms. Proceedings of the 13th International Workshop on Systems, Signals and Image Processing: 21-23 September 2006. 2006, Budapest, Hungary: , 299-302.
Keller B, Nathan D, Wang Y, Zheng Y, Gee J, Conant E, Kontos D: Adaptive multi-cluster fuzzy C-means segmentation of breast parenchymal tissue in digital mammography. Med Image Comput Comput Assist Interv. 2011, 14: 562-569.
Saha PK, Udupa JK, Conant EF, Chakraborty DP, Sullivan D: Breast tissue density quantification via digitized mammograms. IEEE Trans Med Imaging. 2001, 20: 792-803. 10.1109/42.938247.
Heine JJ, Carston MJ, Scott CG, Brandt KR, Wu FF, Pankratz VS, Sellers TA, Vachon CM: An automated approach for estimation of breast density. Cancer Epidemiol Biomarkers Prev. 2008, 17: 3090-3097. 10.1158/1055-9965.EPI-08-0170.
Li J, Szekely L, Eriksson L, Heddson B, Sundbom A, Czene K, Hall P, Humphreys K: High-throughput mammographic density measurement: a tool for risk prediction of breast cancer. Breast Cancer Res. 2012, 14: R114-10.1186/bcr3238.
Shepherd JA, Kerlikowske K, Ma L, Duewer F, Fan B, Wang J, Malkov S, Vittinghoff E, Cummings SR: Volume of mammographic density and risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2011, 20: 1473-1482. 10.1158/1055-9965.EPI-10-1150.
Highnam R, Brady M, Yaffe MJ, Karssemeijer N, Harvey J: Robust breast composition measurement - Volpara (TM). Digital Mammography. 2010, 6136: 342-349. 10.1007/978-3-642-13666-5_46.
Yaffe M, Alonze-Proulx O: Volumetric breast density and breast cancer risk from digital mammograms - preliminary results. Proceedings of the 5th International Workshop on Breast Densitometry and Breast Cancer Risk Assessment: June 9-10 2011; San Francisco. 2011, http://www.volparadensity.com/wp-content/uploads/Yaffe_VolparaRiskMeausres_5thWorkshopBreastDensity2011.pdf,
Pawluczyk O, Augustine BJ, Yaffe MJ, Rico D, Yang J, Mawdsley GE, Boyd NF: A volumetric method for estimation of breast density on digitized screen-film mammograms. Med Phys. 2003, 30: 352-364. 10.1118/1.1539038.
Shepherd JA, Herve L, Landau J, Fan B, Kerlikowske K, Cummings SR: Novel use of single X-ray absorptiometry for measuring breast density. Technol Cancer Res Treat. 2005, 4: 173-182.
Nickson C, Kavanagh AM: Tumour size at detection according to different measures of mammographic breast density. J Med Screen. 2009, 16: 140-146. 10.1258/jms.2009.009054.
Kavanagh AM, Byrnes GB, Nickson C, Cawson JN, Giles GG, Hopper JL, Gertig DM, English DR: Using mammographic density to improve breast cancer screening outcomes. Cancer Epidemiol Biomarkers Prev. 2008, 17: 2818-2824. 10.1158/1055-9965.EPI-07-2835.
Kavanagh AM, Amos AF, Marr GM: The ascertainment and reporting of interval cancers within the National BreastScreen Australia Program. 1999, Woolloomooloo, NSW, Australia: National Breast Cancer Centre
van Gils CH, Otten JD, Verbeek AL, Hendriks JH: Mammographic breast density and risk of breast cancer. Eur J Epi. 1998, 14: 315-320. 10.1023/A:1007423824675.
Heine JJ, Scott CG, Sellers TA, Brandt KR, Serie DJ, Wu FF, Morton MJ, Schueler BA, Couch FJ, Olson JE, Pankratz VS, Vachon CM: A novel automated mammographic density measure and breast cancer risk. J Natl Cancer Inst. 2012, 104: 1028-1037. 10.1093/jnci/djs254.
Aitken Z, McCormack VA, Highnam RP, Martin L, Gunasekara A, Melnichouk O, Mawdsley G, Peressotti C, Yaffe M, Boyd NF, dos Santos Silva I: Screen-film mammographic density and breast cancer risk: a comparison of the volumetric standard mammogram form and the interactive threshold measurement methods. Cancer Epidemiol Biomarkers Prev. 2010, 19: 418-428. 10.1158/1055-9965.EPI-09-1059.
Woolcott CG, Koga K, Conroy SM, Byrne C, Nagata C, Ursin G, Vachon CM, Yaffe MJ, Pagano I, Maskarinec G: Mammographic density, parity and age at first birth, and risk of breast cancer: an analysis of four case–control studies. Breast Cancer Res Treat. 2012, 132: 1163-1171. 10.1007/s10549-011-1929-9.
Martin LJ, Melnichouk O, Guo H, Chiarelli AM, Hislop TG, Yaffe MJ, Minkin S, Hopper JL, Boyd NF: Family history, mammographic density, and risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2010, 19: 456-463. 10.1158/1055-9965.EPI-09-0881.
Vachon CM, Brandt KR, Ghosh K, Scott CG, Maloney SD, Carston MJ, Pankratz VS, Sellers TA: Mammographic breast density as a general marker of breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2007, 16: 43-49. 10.1158/1055-9965.EPI-06-0738.
Sonka M, Hlavac B, Boyle R: Image Processing, Analysis, and Machine Vision. 2007, Toronto: Thomson Learning, 3
Kim Y, Kim C, Kim J-H: Automated estimation of breast density on mammogram using combined information of histogram statistics and boundary gradients. Proc SPIE Med Imaging. 2010, 7624: 76242F-
Stone J, Ding J, Warren RM, Duffy SW, Hopper JL: Using mammographic density to predict breast cancer risk: dense area or percentage dense area. Breast Cancer Res. 2010, 12: R97-10.1186/bcr2778.
Pettersson A, Hankinson SE, Willett WC, Lagiou P, Trichopoulos D, Tamimi RM: Nondense mammographic area and risk of breast cancer. Breast Cancer Res. 2011, 13: R100-10.1186/bcr3041.
Lokate M, Kallenberg MG, Karssemeijer N, Van den Bosch MA, Peeters PH, Van Gils CH: Volumetric breast density from full-field digital mammograms and its association with breast cancer risk factors: a comparison with a threshold method. Cancer Epidemiol Biomarkers Prev. 2010, 19: 3096-3105. 10.1158/1055-9965.EPI-10-0703.
Statacorp: Stata statistical software release 12.1. 2011, College Station, Texas: Statacorp, 121
Vachon CM, van Gils CH, Sellers TA, Ghosh K, Pruthi S, Brandt KR, Pankratz VS: Mammographic density, breast cancer risk and risk prediction. Breast Cancer Res. 2007, 9: 217-10.1186/bcr1829.
Boyd NF, Martin LJ, Sun L, Guo H, Chiarelli A, Hislop G, Yaffe M, Minkin S: Body size, mammographic density, and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2006, 15: 2086-2092. 10.1158/1055-9965.EPI-06-0345.
Acknowledgements
We thank BreastScreen Victoria for providing permission to use mammogram images and client data for the purpose of this study. At the Commonwealth Scientific and Industrial Research Organisation, we thank Ms Leanne Bischof of the Centre for Mathematics, Informatics and Statistics and Mr Jason Dowling of the Australian eHealth Research Centre for contributing to discussions on image processing, and Dr Olivier Salvado, Group Leader of Biomedical Imaging at the Australian eHealth Research Centre for supporting CSIRO involvement in this study, and Dr Pascal Vallotton, Group Leader of Quantitative Imaging at the Centre for Mathematics, Informatics and Statistics, for contributing staff time and existing image processing software resources to the study. This study was funded by the University of Melbourne Collaboration Grant ‘A software platform for comparing automated breast density measurement techniques’, the Victorian Breast Cancer Research Foundation Research Grant ‘Molecular Determinants of Mammographic Density’ and the National Breast Cancer Foundation Collaborative Grant ‘Integration of BreastScreen with epidemiological, molecular and translational research program’.
CN, ZA and ML were funded by the Victorian Breast Cancer Research Foundation Research Grant ‘Molecular Determinants of Mammographic Density’ and the National Breast Cancer Foundation Collaborative Grant ‘Integration of BreastScreen with epidemiological, molecular and translational research program’. YA, TE and MB were funded by the Commonwealth Scientific and Industrial Research Organisation. AK was funded by the University of Melbourne and DE by the University of Melbourne and Cancer Council Victoria.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Commonwealth Scientific and Industrial Research Organisation (CSIRO) has financially supported this study by contributing staff time for software development and manuscript writing. AutoDensity software may be commercialised in the future for use in research and clinical settings, with any financial gains to be shared equally between CSIRO and the University of Melbourne.
Authors’ contributions
CN conceived of and coordinated the study. AK originally collected the images for the study and led Cumulus measurement of those images. YA, TE, MB and ML developed the image processing algorithms. ZA and ML implemented the image processing and managed image and clinical data. ZA and CN performed the statistical analysis and DE and AK advised on analytic methods. CN, ZA, DE, YA and AK drafted the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Nickson, C., Arzhaeva, Y., Aitken, Z. et al. AutoDensity: an automated method to measure mammographic breast density that predicts breast cancer risk and screening outcomes. Breast Cancer Res 15, R80 (2013). https://doi.org/10.1186/bcr3474
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/bcr3474