Abstract
Introduction
In this study we aimed to validate the prognostic value of DC-SCRIPT mRNA expression in a large independent breast cancer cohort. In addition, since DC-SCRIPT is a transcriptional co-regulator of nuclear receptors, we explored its prognostic value in relation to estrogen-receptor-α (ESR1) and -β (ESR2) and evaluated its predictive value for response to tamoxifen treatment.
Methods
DC-SCRIPT mRNA levels were measured by real-time PCR in 1,505 primary invasive breast cancers and associated with outcome (disease-free survival (DFS), metastasis-free survival (MFS) and overall survival (OS)) using univariate and multivariable Cox regression analysis. Logistic and Cox regressions were used to associate DC-SCRIPT levels with clinical benefit and progression-free survival (PFS) for 296 patients treated with first-line systemic tamoxifen for advanced disease.
Results
In univariate and multivariable analysis higher DC-SCRIPT levels were associated with a favorable outcome for both the entire cohort and patients with lymph node-negative (LNN) disease that did not receive adjuvant therapy (DFS, MFS and OS; all, P < 0.001). This association was most pronounced in small (pT1) tumors, in ESR1-positive tumors and in tumors with low ESR2 expression. For first-line endocrine therapy for advanced disease no predictive association was seen with clinical benefit or PFS.
Conclusions
This study provides a higher level of evidence that DC-SCRIPT is indeed an independent, pure prognostic, factor for primary breast cancer and shows that DC-SCRIPT mRNA expression is most informative for either ESR1-positive and/or ESR2-low pT1 tumors.
Similar content being viewed by others
Introduction
Estrogens influence the aggressiveness of breast cancer through their cognate nuclear receptors. In particular, the estrogen receptor-alpha (ERα) (ESR1) - present in tumor cells of about 70% to 75% of all breast tumors - is considered crucial because of its proliferation-inducing actions and for that reason is an important target for therapy. Next to ESR1, a second ER exists, ERβ (ESR2). ESR2 counteracts the activity of ESR1 in many systems [1, 2] and is also expressed in the majority of breast cancers. Apart from breast epithelial tumor cells, ESR2 is also expressed in adjacent infiltrating lymphocytes, fibroblasts, and endothelial cells, all of which are known to influence tumor growth [3]. However, its precise role in breast cancer progression is less well defined.
DC-SCRIPT (zinc finger protein 366 [ZNF366]) is a recently identified nuclear receptor co-regulator first identified in immune cells [4–6]. Nuclear receptor co-regulators are proteins that can activate or repress the transcriptional activity of nuclear receptors. DC-SCRIPT is in this respect a unique co-regulator as we have shown that it enhances the activities of the nuclear retinoic acid receptor (RAR) and peroxisome proliferator-activated receptor (PPAR) heterodimers, RARα/RXRα and PPARγ/RXRα, but represses the activities of ESR1 and progesterone receptor (PGR) [7]. We also showed that DC-SCRIPT was an independent prognostic factor, particularly for hormone receptor-positive breast cancer. This led us to postulate that the anti-proliferative effect of DC-SCRIPT in breast cancer cells could be mediated by simultaneous modulation of the activity of multiple nuclear receptors.
To provide a higher level of evidence for DC-SCRIPT mRNA expression as a prognostic marker, we now report on DC-SCRIPT expression and its significance in a retrospective validation study of 1,505 breast cancer patients with known ESR1, ESR2, and PGR expression levels. The primary objective of this study was to confirm the relationship between DC-SCRIPT mRNA levels measured in primary breast cancers and tumor aggressiveness in a much larger, independent, breast cancer cohort. The main clinical endpoints for assessing the prognostic value of DC-SCRIPT expression were disease-free survival (DFS), metastasis-free survival (MFS), and overall survival (OS) in lymph node-negative (LNN) patients who had not received adjuvant systemic therapy; this approach allowed us to determine tumor aggressiveness during the natural course of the disease. As DC-SCRIPT modulates ER activity, we also analyzed the prognostic value of DC-SCRIPT separately in tumors stratified by ESR1 and ESR2 expression. Since several co-regulators of nuclear receptors also modulate response to therapy [8, 9], we also assessed, as a secondary aim of this study, the predictive value of DC-SCRIPT by using clinical benefit and progression-free survival (PFS) after first-line tamoxifen for advanced disease as the main endpoints.
Materials and methods
Patients
The protocol to study biological markers associated with disease outcome was approved by the medical ethics committee of the Erasmus Medical Center (Rotterdam, The Netherlands) (MEC 02.953). This retrospective study used 1,505 M0 (no metastasis) and 32 M1 (with metastasis) blind-coded freshly frozen primary tumor tissues of female patients with primary operable breast cancer from 1978 through 2000. The study was performed in accordance with the Code of Conduct of the Federation of Medical Scientific Societies in The Netherlands [10], and consent was not required. Wherever possible, the study has been reported in accordance with the Reporting Recommendations for Tumor Marker Prognostic Studies guidelines [11]. The primary breast tumors were from patients with detailed clinical follow-up as previously described [12–14]. ER protein status was determined by routine ligand-binding assays or enzyme immunoassays [15], and ESR1, ESR2, and PGR mRNA status was determined by real-time reverse transcriptase-polymerase chain reaction (RT-PCR) [14, 16, 17]. Follow-up, tumor staging, and response to therapy were defined by standard International Union Against Cancer (Geneva, Switzerland) classification criteria [18] and applied previously by Foekens and colleagues [19]. All 1,537 patients underwent breast-conserving lumpectomy (44%) or modified mastectomy (56%). Of the 1,505 patients included for the evaluation of tumor aggressiveness, 462 lymph node-positive patients (31%) were treated with adjuvant systemic therapy, 207 patients received hormonal therapy, 233 chemotherapy, and 22 combination therapy. Disease recurrence occurred in 836 patients, and 703 developed a distant metastasis. The median follow-up time of patients alive was 90 months (range of 4 to 260 months).
Eight hundred thirty-seven patients had no involved nodes and did not receive systemic adjuvant therapy. Of these 837 LNN patients, 383 had a disease relapse, 300 developed a distant metastasis, and 273 died during follow-up.
Of the 703 patients who developed a distant metastasis, 296 ER-positive patients, including the 32 M1 patients, received hormonal therapy as first-line therapy for advanced disease. Clinical benefit of first-line tamoxifen treatment was observed in 185 patients. Median follow-up time for treatment of advanced disease was 38 (4 to 120) months. Two hundred nineteen patients had died at the end of the follow-up. None of these patients had received prior adjuvant hormonal therapy, whereas 19% received prior adjuvant chemotherapy. A more detailed description of the patients and their therapy is given in the Supplementary materials and methods (Additional file 1). Patient and tumor characteristics combined with DC-SCRIPT mRNA expression and clinical outcome are listed in Table 1.
RNA isolation and quantitative RT-PCR
Tissue processing, RNA isolation, cDNA synthesis, and quantitative RT-PCR were performed as previously described [16]. Real-time quantitative PCRs were performed in a 25-μL reaction volume in an M×3000P™ Real-Time PCR System (Agilent, Amsterdam, The Netherlands). In addition to an SYBR-based assay to detect a 129-base pair (bp) DC-SCRIPT transcript covering exon 4 to 5 (forward primer: 5'-AAAGTCAAGCATGGAGTCATG-3'; reverse primer: 5'-GCTTCTGAGAGAGGTCAAAG-3'), a commercially available Taqman Gene Expression Assay from Applied Biosystems (Nieuwerkerk aan den IJssel, The Netherlands) covering exon 3 to 4 and generating a 62-bp product was used (Hs00403536_m1, RefSeq NM_152625.1). DC-SCRIPT levels were readily detected with both assays, and data generated with these assays correlated significantly (Spearman's rho = 0.87; P < 0.0001). We therefore performed our analyses on the real-time RT-PCR data generated with the Taqman assay, which is generally considered to be more specific. Intron-spanning primer sequences for the three reference genes - that is, hydroxymethylbilane synthase (HMBS), hypoxanthine-guanine phospho-ribosyltransferase (HPRT1), and β-2-microglobulin (B2M) - and for ESR1, ESR2, PGR, and real-time PCR conditions for these SYBR-based assays were as described previously [16, 17]. Forty rounds of amplification were performed, and fluorescent signals of the Taqman probe or SYBR green signal were used to generate cycle threshold (Ct) values from which mRNA expression levels were calculated. Ct values of HPRT1 and B2M were adjusted to the higher HMBS Ct values. Next, the expression levels of DC-SCRIPT were normalized against the average expression levels of the three reference genes as follows: mRNA target = 2(mean Ct reference genes - mean Ct target) [16].
Tissue processing
Primary tumor tissue was processed as described previously [16]. To assess the amount of invasive tumor cell nuclei relative to the amount of surrounding stromal cells, 5-μm sections were cut for hematoxylin-and-eosin staining before, during, and after the sections were cut for RNA isolation. Only specimens with at least 30% invasive tumor cell nuclei were included in this study.
Data analysis and statistics
The relationship between DC-SCRIPT and patient and tumor characteristics was investigated with the use of non-parametric methods (Spearman rank correlations for continuous variables and Wilcoxon rank-sum for dichotomized or Kruskal-Wallis test for ordered variables). To reduce skewness, DC-SCRIPT levels were transformed with the Box-Cox transformation. DC-SCRIPT levels were dichotomized with the previously identified 66.7% high versus 33.3% low cutoff for DC-SCRIPT [7]. To test for an association with tumor aggressiveness and the time to progression during first-line therapy, Cox regression analysis was applied on the Box-Cox-transformed and dichotomized DC-SCRIPT mRNA levels. The hazard ratio (HR) and its 95% confidence interval were computed to correlate the expression levels with DFS, MFS, OS, and PFS, respectively. In multivariable analysis, Cox proportional hazards models for DFS, MFS, OS, and PFS were applied to test DC-SCRIPT levels added to models with traditional factors. The proportional hazards assumptions were checked with Schoenfeld residuals. The analyses were stratified if necessary. The models for DFS, MFS, and OS for LNN patients who had not received adjuvant systemic therapy included age, menopausal status, tumor size, grade, and ESR1 and PGR mRNA levels. Survival curves were generated with the method of Kaplan and Meier. The log-rank test was used to test for differences between survival curves. Logistic regression was used for the association of DC-SCRIPT with clinical benefit. Computations were performed with the STATA statistical package, release 11.0 (STATA Corp., College Station, TX, USA) and SPSS 15.0 (SPSS Inc., Chicago, IL, USA). All P values are two-sided, and a P value of less than 0.05 was considered statistically significant.
Results
Associations of DC-SCRIPTwith clinicopathological factors and histological and intrinsic breast cancer subtypes
In analogy with our previous study, DC-SCRIPT mRNA expression was readily detected by quantitative RT-PCR in five normal breast tissues taken adjacent from tumor tissue and five prophylactic breast tissues (median [interquartile]: 0.063 [0.015] and 0.054 [0.035], respectively), whereas median levels were over 8-fold lower (P < 0.05) in 1,505 invasive breast tumors (0.0069 [0.0074]). Table 1 shows the median expression levels and interquartile ranges of DC-SCRIPT transcripts and relation with patient and tumor characteristics for these 1,505 patients who were evaluable for prognosis. DC-SCRIPT levels were positively associated with tumor grade and ESR1, PGR, and ESR2 steroid hormone receptor expression level and negatively associated with invasive epithelial tumor cell content and tumor size. In addition, ESR2 was more highly expressed in tumors with a higher percentage of stromal cells (786 tumors with 30% to 70% invasive epithelial cells), and ESR1 was more highly expressed in tumors with a high percentage of invasive epithelial cells (719 tumors with at least 70% invasive epithelial cells) (P < 0.001) (data not shown). High levels of DC-SCRIPT were found in breast tumors with a ductal carcinoma in situ (DCIS) component or infiltrating lobular carcinoma compared with infiltrating ductal carcinomas (both P < 0.01). Of 308 LNN tumors, intrinsic subtyping data were available [20]. In these tumors, basal-like tumors had the lowest levels and normal-like breast tumors expressed significantly higher levels of DC-SCRIPT compared with the other intrinsic subtypes (P < 0.001; Figure S1 in Additional file 2). Furthermore, luminal A tumors expressed higher levels of DC-SCRIPT and ESR2 but lower levels of ESR1 compared with luminal B tumors (median levels in luminal A versus luminal B: 0.0078 and 0.056 for DC-SCRIPT [P = 0.003], 0.0095 and 0.0023 for ESR2 [P < 0.001], and 6.1 and 13.6 for ESR1 [P < 0.001]). This may be explained at least partly by the fact that, in this cohort of 308 LNN tumors, the luminal B tumors contained a higher percentage of invasive epithelial cells (mean ± standard deviation [SD]: 77% ± 9% for the n = 64 luminal B tumors versus 67% ± 12% for the n = 71 luminal A tumors).
DC-SCRIPTand tumor aggressiveness in univariate and multivariable analyses
In the analyses including all 1,505 M0 patients, increasing levels of DC-SCRIPT mRNA were significantly associated with favorable DFS, MFS, and OS (HR 0.78, 0.74, and 0.77, respectively; all P < 0.001). To test for a relation between DC-SCRIPT mRNA levels and tumor aggressiveness (that is, the natural course of the disease without the confounding effect of systemic adjuvant therapy), we restricted our next analyses of MFS to those 837 LNN disease patients who had not received (neo)adjuvant systemic therapy. The significant relationships of DC-SCRIPT as a continuous variable in these univariate analyses justified the use of the previously identified cut point that dichotomized the cohort in 33.3% of the patients with low levels and 66.7% of patients with high levels of DC-SCRIPT mRNA in their primary tumors [7]. In univariate analysis, high levels of DC-SCRIPT were significantly associated with a favorable prognosis (HR 0.55; P < 0.001) (Table 2). When added to a multivariable base model for LNN disease - which included the traditional prognostic factors of age, menopausal status, grade, and PGR - stratified by ESR1 and tumor size to meet the proportional hazards assumption, the association of DC-SCRIPT with MFS remained highly significant (HR 0.60; P < 0.001) (Table 2). Adding ESR2 to the model did not significantly affect the prognostic value of DC-SCRIPT in these analyses (Table 2).
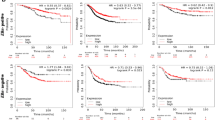
Because the proportional hazards assumptions were violated by ESR1 and tumor size and because DC-SCRIPT is a transcriptional co-regulator of nuclear receptors - including the, for breast cancer biologically relevant, steroid hormone receptors - we next explored its prognostic value as continuous variable in subgroups of tumors stratified by steroid hormone receptor status and tumor size (Table 3 and Figure 1). Subdividing the 837 primary LNN tumors into ESR1-positive and -negative [14] showed that increasing levels of DC-SCRIPT were, in univariate and multivariable analyses, associated with good prognosis only for the patients with ESR1-positive tumors. Subdividing these LNN tumors at the median level of ESR2 into high and low revealed that, in contrast to ESR1, increasing levels of DC-SCRIPT were, in both univariate and multivariable analyses, associated with good prognosis only for patients with primary tumors with low levels of ESR2. With respect to tumor size, in univariate and multivariable analyses, increasing levels of DC-SCRIPT were associated with good prognosis only for pT1 (small tumor without lymphatic/vascular invasion) tumors and not for larger tumors. These and additional exploratory Cox univariate analyses are summarized in Table 3. The prognostic value of DC-SCRIPT is visualized in Kaplan-Meier curves (Figure 1) as a dichotomized variable in these biologically relevant LNN ESR1-negative (Figure 1a) and -positive (Figure 1b) and LNN ESR2-high (Figure 1d) and -low (Figure 1e) subsets in combination with patients with pT1 primary tumors (Figure 1c, f).
Metastasis-free survival as a function of dichotomized DC-SCRIPT. Metastasis-free survival is shown as a function of dichotomized DC-SCRIPT in 837 lymph-node negative, primary breast cancer patients after subdividing them according high and low ESR1 and ESR2 in the primary tumor and tumor size. (a) ESR1 negative primary breast tumors, (b) ESR1 positive primary breast tumors, (c) ESR1 positive pT1 primary breast tumors, (d) ESR2 low primary breast tumors, (e) ESR2 high primary breast tumors, (f) ESR2 low pT1 primary breast tumors. Quantitative polymerase chain reaction cut points are shown for high versus low DC-SCRIPT (66.7% versus 33.3%) [7], for positive versus negative ESR1 (0.2) [14], and for ESR2-low versus -high at the median level of 0.005 (mRNA levels relative to reference gene set). Patients at risk are indicated. DC-SCRIPT, dendritic cell-specific transcript; ESR, estrogen receptor; pT1, small tumor without lymphatic/vascular invasion.
DC-SCRIPTand response to first-line endocrine therapy
DC-SCRIPT expression levels were evaluated in 296 hormone-naïve ER-positive primary breast tumors from patients whose relapse was treated with first-line tamoxifen monotherapy. These patients had not received (neo)adjuvant endocrine systemic treatment. In univariate analyses, no statistically significant associations were observed between DC-SCRIPT as transformed continuous variable and PFS or clinical benefit after start of first-line treatment with tamoxifen (HR = 1.08 [0.99 to 1.18], P = 0.07 and odds ratio = 0.88 [0.74 to 1.05], P = 0.16, respectively).
Discussion
DC-SCRIPT has been identified as a key modulator of nuclear receptor activity that has prognostic value in breast cancer [7]. The clinical conclusions about DC-SCRIPT mRNA expression as a prognostic marker in breast cancer were based on non-randomized retrospective analyses in three small, breast cancer cohorts from Nijmegen (The Netherlands) and still required independent validation. In this study, we provide a higher level of evidence as we confirm that mRNA expression values of DC-SCRIPT indicate outcome in an independent retrospective cohort of 1,505 primary breast cancers from Rotterdam. In addition, we confirm that DC-SCRIPT mRNA expression is a pure prognostic marker as it indicates - independently of current clinical prognostic markers such as age, menopausal status, grade, tumor size, and receptor status - the occurrence of distant metastasis in patients who did not receive any adjuvant systemic treatment. Because we used mRNA extracted from tumor tissue and a different mRNA isolation method (RNA-B versus column-based), an independent real-time PCR assay to detect DC-SCRIPT, a different type of machine to amplify the transcript, and personnel from another institute, we consider DC-SCRIPT a robust prognostic marker for patients with early breast cancer. The patients described in this retrospective study entered the clinic during 1978 to 2000. During this period, adjuvant therapy was not as widespread as it is nowadays; this circumstance was at the same time the strength of our cohort for the evaluation of a prognostic marker. The data that emerged from this study thus validate the hypothesis that DC-SCRIPT is associated with good prognosis in early disease and support the idea that DC-SCRIPT acts as a tumor suppressor in breast cancer progression [7].
Because of the size of this cohort and the biological function of DC-SCRIPT as a nuclear receptor co-regulator, we were able to include additional subgroup analyses to extend our insights into the clinical behavior and relevance of measuring DC-SCRIPT in primary breast cancers. High levels of DC-SCRIPT mRNA in primary tumors of breast cancer patients were significantly related with tumor characteristics that are associated with good prognosis, such as DCIS, infiltrating lobular carcinoma, breast tumors of the normal-like and luminal A subtype, and small (pT1), well-differentiated, steroid hormone receptor-positive tumors. While ESR1 is localized mainly in tumors with at least 70% invasive epithelial cells (P < 0.001), we showed for both ESR2 and DC-SCRIPT a positive correlation with tumors with less than 70% invasive epithelial cells (P < 0.001). As normal epithelial cells in tumors with less than 70% invasive epithelial cells express the highest levels of DC-SCRIPT, they could be responsible for this correlation. Furthermore, infiltrating leukocytes in the stroma might have contributed to the detected signal [4, 5]. Alternatively, or additionally, stromal cells may have played a role in the induction of DC-SCRIPT in the epithelial tumor cells. In analogy, ESR2 is - apart from breast cancer epithelial tumor cells - also expressed in adjacent infiltrating lymphocytes, fibroblasts, and endothelial cells [3].
Interestingly, in tumors that express relatively high ESR2 mRNA levels and that in general have a higher stromal content, DC-SCRIPT expression has little or no prognostic value. Thus, while in early ESR1-positive breast cancer DC-SCRIPT inhibits progression of breast cancer, this effect appears to be neutralized in tumors high in ESR2. Indeed, ESR2 has been reported to be dominant over ESR1 and able to counteract the proliferation-inducing activities of ESR1 [1, 2]. Unraveling the precise role of DC-SCRIPT in the complex genomic and non-genomic interplay between ESR1, ESR2, and their isoforms [21–23] might turn out to be rewarding for elucidating the 'yin-yang' role of these factors in breast cancer.
As DC-SCRIPT can inhibit ERα and PR activity, a second aim of the study was to address whether DC-SCRIPT affects the response to endocrine therapy. In our previous study, we had already explored the value of DC-SCRIPT mRNA expression to indicate outcome in a cohort of breast cancer patients who received adjuvant tamoxifen [7]. However, in the adjuvant setting - that, for ethical reasons, nowadays includes only non-randomly assigned patients among treated and untreated arms - one cannot discriminate between tumor aggressiveness and response to treatment [24]. The current retrospective study included hormone-naïve patients (that is, not having received any [neo]adjuvant endocrine treatment) who received first-line tamoxifen treatment for their advanced disease and therefore was better suited to study a putative relation of DC-SCRIPT and response to therapy. Despite the positive association of DC-SCRIPT with ESR1, DC-SCRIPT levels were unable to identify patients with ESR1-positive primary tumors at high or low risk to progress if treated with tamoxifen. Thus, although DC-SCRIPT can modulate the activity of ESR1, it does not affect the response to endocrine therapy with tamoxifen in advanced breast cancer. The early loss of DC-SCRIPT during cancer progression might explain this absence of a response in the metastatic disease setting.
Conclusions
This independent retrospective quantitative RT-PCR study validates that high levels of DC-SCRIPT are associated with reduced tumor aggressiveness. The association is particularly strong for small tumors with high ESR1 or low ESR2 mRNA levels or both. Finally, although DC-SCRIPT negatively regulates ESR1 and PGR activity, DC-SCRIPT levels measured in the primary tumors are not associated with response to first-line endocrine treatment for advanced disease. This finding is in line with DC-SCRIPT as an early marker for disease.
Abbreviations
- B2M :
-
beta-2-microglobulin gene
- bp:
-
base product
- Ct:
-
cycle threshold
- DCIS:
-
ductal carcinoma in situ
- DC-SCRIPT:
-
dendritic cell-specific transcript
- DFS:
-
disease-free survival
- ER:
-
estrogen receptor
- ESR :
-
estrogen receptor gene
- HMBS :
-
hydroxymethylbilane synthase gene
- HPRT1 :
-
hypoxanthine guanine phosphoribosyltransferase 1 gene
- HR:
-
hazard ratio
- LNN:
-
lymph node-negative
- M0:
-
no metastasis
- M1:
-
with metastasis
- MFS:
-
metastasis-free survival
- OS:
-
overall survival
- PCR:
-
polymerase chain reaction
- PFS:
-
progression-free survival
- PGR :
-
progesterone receptor gene
- PPAR:
-
peroxisome proliferator-activated receptor
- pT1:
-
small tumor without lymphatic/vascular invasion
- PR:
-
progesterone receptor
- RAR:
-
retinoic acid receptor
- RT-PCR:
-
reverse transcriptase polymerase chain reaction
- SYBR:
-
N',N'-dimethyl-N-[4-[(E)-(3-methyl-1,3-benzothiazol-2-ylidene)methyl]-1-phenylquinolin-1-ium-2-yl]-N-propylpropane-1,3-diamine.
References
Strom A, Hartman J, Foster JS, Kietz S, Wimalasena J, Gustafsson JA: Estrogen receptor beta inhibits 17beta-estradiol-stimulated proliferation of the breast cancer cell line T47D. Proc Natl Acad Sci USA. 2004, 101: 1566-1571. 10.1073/pnas.0308319100.
Liu MM, Albanese C, Anderson CM, Hilty K, Webb P, Uht RM, Price RH, Pestell RG, Kushner PJ: Opposing action of estrogen receptors alpha and beta on cyclin D1 gene expression. J Biol Chem. 2002, 277: 24353-24360. 10.1074/jbc.M201829200.
Hartman J, Strom A, Gustafsson JA: Estrogen receptor beta in breast cancer--diagnostic and therapeutic implications. Steroids. 2009, 74: 635-641. 10.1016/j.steroids.2009.02.005.
Triantis V, Moulin V, Looman MW, Hartgers FC, Janssen RA, Adema GJ: Molecular characterization of the murine homologue of the DC-derived protein DC-SCRIPT. J Leukoc Biol. 2006, 79: 1083-1091. 10.1189/jlb.1005588.
Triantis V, Trancikova DE, Looman MW, Hartgers FC, Janssen RA, Adema GJ: Identification and characterization of DC-SCRIPT, a novel dendritic cell-expressed member of the zinc finger family of transcriptional regulators. J Immunol. 2006, 176: 1081-1089.
Lopez-Garcia J, Periyasamy M, Thomas RS, Christian M, Leao M, Jat P, Kindle KB, Heery DM, Parker MG, Buluwela L, Kamalati T, Ali S: ZNF366 is an estrogen receptor corepressor that acts through CtBP and histone deacetylases. Nucleic Acids Res. 2006, 34: 6126-6136. 10.1093/nar/gkl875.
Ansems M, Hontelez S, Looman MW, Karthaus N, Bult P, Bonenkamp JJ, Jansen JH, Sweep FC, Span PN, Adema GJ: DC-SCRIPT: nuclear receptor modulation and prognostic significance in primary breast cancer. J Natl Cancer Inst. 2010, 102: 54-68. 10.1093/jnci/djp441.
Ramadoss P, Marcus C, Perdew GH: Role of the aryl hydrocarbon receptor in drug metabolism. Expert Opin Drug Metab Toxicol. 2005, 1: 9-21. 10.1517/17425255.1.1.9.
Osborne CK, Schiff R, Fuqua SA, Shou J: Estrogen receptor: current understanding of its activation and modulation. Clin Cancer Res. 2001, 7: 4338s-4342s. discussion 4411s-4412s
Code of Conduct of the Federation of Medical Scientific Societies in the Netherlands. [http://www.federa.org/?s=1&m=99]
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM: REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat. 2006, 100: 229-235. 10.1007/s10549-006-9242-8.
Jansen MP, Sieuwerts AM, Look MP, Ritstier K, Meijer-van Gelder ME, van Staveren IL, Klijn JG, Foekens JA, Berns EM: HOXB13-to-IL17BR expression ratio is related with tumor aggressiveness and response to tamoxifen of recurrent breast cancer: a retrospective study. J Clin Oncol. 2007, 25: 662-668. 10.1200/JCO.2006.07.3676.
Sieuwerts AM, Look MP, Meijer-van Gelder ME, Timmermans M, Trapman AM, Garcia RR, Arnold M, Goedheer AJ, de Weerd V, Portengen H, Klijn JG, Foekens JA: Which cyclin E prevails as prognostic marker for breast cancer? Results from a retrospective study involving 635 lymph node-negative breast cancer patients. Clin Cancer Res. 2006, 12: 3319-3328. 10.1158/1078-0432.CCR-06-0225.
Sieuwerts AM, Usher PA, Meijer-van Gelder ME, Timmermans M, Martens JW, Brunner N, Klijn JG, Offenberg H, Foekens JA: Concentrations of TIMP1 mRNA splice variants and TIMP-1 protein are differentially associated with prognosis in primary breast cancer. Clin Chem. 2007, 53: 1280-1288. 10.1373/clinchem.2006.082800.
Foekens JA, Portengen H, van Putten WL, Peters HA, Krijnen HL, Alexieva-Figusch J, Klijn JG: Prognostic value of estrogen and progesterone receptors measured by enzyme immunoassays in human breast tumor cytosols. Cancer Res. 1989, 49: 5823-5828.
Sieuwerts AM, Meijer-van Gelder ME, Timmermans M, Trapman AM, Garcia RR, Arnold M, Goedheer AJ, Portengen H, Klijn JG, Foekens JA: How ADAM-9 and ADAM-11 differentially from estrogen receptor predict response to tamoxifen treatment in patients with recurrent breast cancer: a retrospective study. Clin Cancer Res. 2005, 11: 7311-7321. 10.1158/1078-0432.CCR-05-0560.
Dorssers LC, van Agthoven T, Brinkman A, Veldscholte J, Smid M, Dechering KJ: Breast cancer oestrogen independence mediated by BCAR1 or BCAR3 genes is transmitted through mechanisms distinct from the oestrogen receptor signalling pathway or the epidermal growth factor receptor signalling pathway. Breast Cancer Res. 2005, 7: R82-92. 10.1186/bcr954.
Hayward JL, Carbone PP, Heuson JC, Kumaoka S, Segaloff A, Rubens RD: Assessment of response to therapy in advanced breast cancer: a project of the Programme on Clinical Oncology of the International Union Against Cancer, Geneva, Switzerland. Cancer. 1977, 39: 1289-1294. 10.1002/1097-0142(197703)39:3<1289::AID-CNCR2820390340>3.0.CO;2-F.
Foekens JA, Peters HA, Grebenchtchikov N, Look MP, Meijer-van Gelder ME, Geurts-Moespot A, van der Kwast TH, Sweep CG, Klijn JG: High tumor levels of vascular endothelial growth factor predict poor response to systemic therapy in advanced breast cancer. Cancer Res. 2001, 61: 5407-5414.
Smid M, Wang Y, Zhang Y, Sieuwerts AM, Yu J, Klijn JG, Foekens JA, Martens JW: Subtypes of breast cancer show preferential site of relapse. Cancer Res. 2008, 68: 3108-3114. 10.1158/0008-5472.CAN-07-5644.
Lee LM, Cao J, Deng H, Chen P, Gatalica Z, Wang ZY: ER-alpha36, a novel variant of ER-alpha, is expressed in ER-positive and -negative human breast carcinomas. Anticancer Res. 2008, 28: 479-483.
Chen JQ, Russo PA, Cooke C, Russo IH, Russo J: ERbeta shifts from mitochondria to nucleus during estrogen-induced neoplastic transformation of human breast epithelial cells and is involved in estrogen-induced synthesis of mitochondrial respiratory chain proteins. Biochim Biophys Acta. 2007, 1773: 1732-1746. 10.1016/j.bbamcr.2007.05.008.
Shaaban AM, Green AR, Karthik S, Alizadeh Y, Hughes TA, Harkins L, Ellis IO, Robertson JF, Paish EC, Saunders PT, Groome NP, Speirs V: Nuclear and cytoplasmic expression of ERbeta1, ERbeta2, and ERbeta5 identifies distinct prognostic outcome for breast cancer patients. Clin Cancer Res. 2008, 14: 5228-5235. 10.1158/1078-0432.CCR-07-4528.
Jansen MP, Foekens JA, Klijn JG, Berns EM: Re: Limits of predictive models using microarray data for breast cancer clinical treatment outcome. J Natl Cancer Inst. 2005, 97: 1851-1852. 10.1093/jnci/dji433. author reply 1852-1853
Foekens JA, Look MP, Bolt-de Vries J, Meijer-van Gelder ME, van Putten WL, Klijn JG: Cathepsin-D in primary breast cancer: prognostic evaluation involving 2810 patients. Br J Cancer. 1999, 79: 300-307. 10.1038/sj.bjc.6690048.
van Agthoven T, Sieuwerts AM, Meijer-van Gelder ME, Look MP, Smid M, Veldscholte J, Sleijfer S, Foekens JA, Dorssers LC: Relevance of breast cancer antiestrogen resistance genes in human breast cancer progression and tamoxifen resistance. J Clin Oncol. 2009, 27: 542-549. 10.1200/JCO.2008.17.1462.
Meijer-van Gelder ME, Look MP, Peters HA, Schmitt M, Brunner N, Harbeck N, Klijn JG, Foekens JA: Urokinase-type plasminogen activator system in breast cancer: association with tamoxifen therapy in recurrent disease. Cancer Res. 2004, 64: 4563-4568. 10.1158/0008-5472.CAN-03-3848.
Martens JW, Nimmrich I, Koenig T, Look MP, Harbeck N, Model F, Kluth A, Bolt-de Vries J, Sieuwerts AM, Portengen H, Meijer-Van Gelder ME, Piepenbrock C, Olek A, Höfler H, Kiechle M, Klijn JG, Schmitt M, Maier S, Foekens JA: Association of DNA methylation of phosphoserine aminotransferase with response to endocrine therapy in patients with recurrent breast cancer. Cancer Res. 2005, 65: 4101-4117. 10.1158/0008-5472.CAN-05-0064.
Acknowledgements
We especially thank the patients and surgeons, pathologists, and internists for their assistance in collecting tumor tissues and patients' clinical follow-up data. We thank Joan Bolt, Marion Meijer, Mieke Timmermans, Anita Trapman, and Wendy van der Smissen for their excellent technical support. This work was financially supported by VICI grant 918-66-615 (awarded to GJA) from the Netherlands Organization for Scientific Research (NWO).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AMS participated in the study design, collected laboratory data on the patients, performed laboratory work and statistical analyses, and wrote the manuscript. MA participated in the study design, performed laboratory work, and provided critical revision of the manuscript. MPL collected laboratory data on the patients, performed the clinical statistical analyses, and provided critical revision of the manuscript. PNS provided critical revision of the manuscript and participated in the study design. VdW and AvG performed the laboratory work and provided critical revision of the manuscript. JAF and JWMM participated in the study design, provided the study material and clinical information, and provided critical revision of the manuscript. GJA participated in the study design and provided critical revision of the manuscript. All authors read and approved the final manuscript.
Anieta M Sieuwerts, Marleen Ansems contributed equally to this work.
Electronic supplementary material
13058_2010_2765_MOESM2_ESM.TIFF
Additional file 2: Figure S1 - DC-SCRIPT mRNA expression in breast cancer subtypes. The box-plot shows the five statistics (lower whisker is 5% minimum, lower box part is 25th percentile, solid line in box presents the median, upper box part is 75th percentile and upper whisker is 95% maximum). Figure depicts P for Mann-Whitney U test to identify significantly different expression of DC-SCRIPT in between subtypes. (TIFF 216 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Sieuwerts, A.M., Ansems, M., Look, M.P. et al. Clinical significance of the nuclear receptor co-regulator DC-SCRIPT in breast cancer: an independent retrospective validation study. Breast Cancer Res 12, R103 (2010). https://doi.org/10.1186/bcr2786
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/bcr2786