Abstract
Introduction
Breast cancer comprises clinically distinct subtypes, but most risk statistics consider breast cancer only as a single entity. To estimate subtype-specific lifetime breast cancer risks, we took advantage of population-based data for which information regarding tumor expression of estrogen receptor (ER), progesterone receptor (PR) and HER2/neu (HER2) was newly available.
Methods
We included women whose breast cancer was diagnosed in the state of California from 2006 to 2007 and was reported to the National Cancer Institute's Surveillance, Epidemiology and End Results Program (N = 40,936). We calculated absolute lifetime and age-specific probabilities (percent, 95% confidence interval) of developing breast cancer subtypes defined by ER, PR, and HER2 status - luminal (ER and/or PR-positive, HER2-negative), HER2-positive (ER and PR-positive or negative, HER2-positive), and triple-negative (ER-negative, PR-negative, and HER2-negative) - separately for white, black, Hispanic, and Asian women.
Results
The luminal breast cancer subtype predominates across racial/ethnic groups, with lifetime risk lowest in Hispanic women (4.60%, 4.41-4.80%) and highest in white women (8.10%, 7.94-8.20%). HER2-positive breast cancer varies less by race (1.56-1.91%). Lifetime risk of triple-negative breast cancer is highest in black women (1.98%, 1.80-2.17%), compared to 0.77% (0.67-0.88%) for Asians, 1.04% (0.96-1.13%) for Hispanics and 1.25% (1.20-1.30%) for whites. Across racial/ethnic groups, nearly half of all luminal breast cancers occur after age 70.
Conclusions
These absolute risk estimates may inform health policy and resource planning across diverse populations, and can help patients and physicians weigh the probabilities of developing specific breast cancer subtypes against competing health risks.
Similar content being viewed by others
Introduction
Breast cancers are biologically heterogeneous. Gene expression profiling of breast tumor tissues has identified reliable patterns indicative of clinically distinct subtypes [1–4]. At this time, the subtype classifications most often used in clinical settings are based on the commonly measured tumor markers estrogen receptor (ER), progesterone receptor (PR), and HER2/neu (HER2), which offer imperfect but practical surrogates for genomic profiling [5]. It is increasingly recognized that breast cancer subtypes vary in occurrence (especially by race/ethnicity) [5–8], in their detection by screening mammography [9, 10], and in their risk associations with other factors [11–15]. Treatment options and prognosis also depend on breast cancer subtype [9, 16–18].
Despite accumulating evidence that breast cancer subtypes should be considered separately, it is still routine to present statistics that consider the disease as a single entity. Perhaps most commonly cited is the 12% lifetime probability statistic [19], prompting the widespread perception that 'one in eight' US women will develop the disease. This single estimate does not convey race-specific variation in breast cancer risks. Moreover, although some groups are reported to have greater relative risk of specific breast cancer subtypes, there are no data with which to counsel patients about the absolute magnitude of these risks in comparison with other threats to their health; one clinically important example is the ER-, PR-, and HER2-negative (triple-negative) breast cancer subtype among black women [5]. To provide estimates relevant to patient care and health policy, we took advantage of recent data on subtype-specific incidence patterns (collected in the large and diverse population of California) to calculate absolute lifetime risks of developing a first primary breast cancer according to breast cancer subtype and presented those calculations separately for women of four racial/ethnic groups.
Materials and methods
Study population
The California Cancer Registry (CCR), a contributor to the National Cancer Institute's Surveillance, Epidemiology and End Results (SEER) program, has ascertained all cancers diagnosed in the state of California since 1988, with estimated 99% completeness. In this analysis, we included all invasive breast cancers (International Classification of Disease for Oncology, Third Edition [ICD-O-3] sites 50.0 to 50.9; all histologies excluding sarcomas and lymphomas 9050 to 9055, 9140, and 9590 to 9989). The CCR has collected information on ER and PR since 1990 and on HER2 since 1999. Before the year 2006, 29% of cases lacked HER2 data; subsequently, HER2 data completeness increased to at least 85%, and thus we limited our assessment to the 40,936 women whose cancer was diagnosed between 1 January 2006 and 31 December 2007, comprising the most recent years for which data are available from the CCR. Each marker is reported as positive, negative, borderline, not tested, not recorded, or unknown. ER and PR were evaluated by dextran-coated charcoal assays or immunohistochemistry (IHC), with positive defined as greater than or equal to 5% nuclear staining; HER2 was tested by IHC (with 0 and 1+ defined as negative, 2+ as borderline, and 3+ as positive) or fluorescence in situ hybridization (with fewer than or equal to two gene copies defined as negative and greater than two copies defined as positive) [20]. Tumor size and stage at diagnosis, patient age at diagnosis, race, and ethnicity were abstracted directly from the medical record; in most cases (84%), race was derived from a patient self-report [21]. We categorized race/ethnicity as non-Hispanic (NH) white, NH black, Hispanic, and NH Asian or Pacific Islander (hereafter referred to as white, black, Hispanic, and Asian).
Categorization of breast cancer subtypes
We categorized breast cancer subtypes according to tumor expression of ER, PR, and HER2; we designated three subtype groupings, which are distinguished by their differences in clinical management (consisting of treatment with ER-, PR-, or HER2-targeted therapies) and by their prognosis. Similarly to previous investigators [22], we defined a 'luminal' category as ER- or PR-positive or both and HER2-negative (a category that overlaps, but does not concord completely, with the gene expression-based subtypes luminal A and luminal B) [3, 4]; other subtype categories were HER2-positive (ER- and PR-positive or -negative and HER2-positive) and triple-negative (ER-negative, PR-negative, and HER2-negative) [5–8, 17].
Statistical analysis
We used DevCan software (version 6.4.1), developed by the National Cancer Institute, to compute absolute probabilities that a specific breast cancer subtype will be diagnosed and the associated 95% confidence intervals (CIs) [23]. DevCan employs competing-risks methodology to estimate age-dependent probabilities of cancer occurrence and accounts for competing risks of death (specifically, all non-breast cancer causes of death) and is conditioned upon the patient's never having had breast cancer previously [24–27]. For each age group, DevCan calculates the probabilities of two mutually exclusive events: either developing the cancer of interest or dying from other causes without ever having developed the cancer of interest. Consequently, cause-specific mortality data are required to estimate incidence of the cancer of interest. The DevCan program uses data on cause-specific mortality for the US population; the data are specific to age, sex, race, and calendar year and are derived from the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention [23, 28]. Since NCHS does not provide subtype-specific breast cancer mortality data, we used overall breast cancer-specific mortality in place of breast cancer subtype-specific mortality and assumed that the difference in these mortality rates would be small at the population level. We limited our assessment to risks of developing a first breast cancer [23] and did not consider second primary breast cancer (a rare event affecting only 4% of breast cancer survivors) [29]. All analyses were conducted in accordance with the Institutional Review Board approval of the Cancer Prevention Institute of California (protocol number 2001-043).
Results and Discussion
Study participants
From the cohort of 40,936 women whose breast cancer was diagnosed in California in 2006-2007, we excluded 7,737 cases (18.9%) having any of the three markers ER, PR, or HER2 coded as borderline, not tested, not recorded, or unknown. This excluded group comprised 5,069 whites, 505 blacks, 1,262 Hispanics, and 901 Asians; there were no significant differences according to race/ethnicity or age between the cases excluded for missing ER, PR, or HER2 results and the included cases that had ER, PR, and HER data available (results not shown). We included a total of 33,199 women, for whom data on ER, PR, and HER2 were available, in our analyses. Table 1 presents demographic and clinical characteristics of the patient population derived from the CCR. Among breast cancer cases, 66.1% were white, 6.2% black, 16.6% Hispanic, and 11% Asian. Compared with other racial groups, white patients had a higher proportion of tumors that were luminal (71.6% versus 53% to 62.8%), that were diagnosed in local stage (64.5% versus 54.5% to 61.7%), and that were diagnosed at a size of 2 cm or less (61.7% versus 48.6% to 58.4%). Black women had the highest proportion of tumors that were triple-negative (24.6% versus 10% to 16.7%). A chi-square test of breast cancer subtypes by race yielded a P value of less than 0.0001, indicating a statistically significant difference in subtype distribution between racial groups.
Lifetime risks by racial/ethnic group
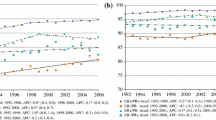
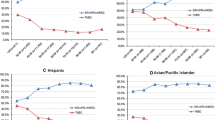
Table 2 presents absolute lifetime risks of developing specific breast cancer subtypes for white, black, Hispanic, and Asian women. All racial/ethnic groups have a higher lifetime risk of developing luminal breast cancer than any other subtype, but this luminal breast cancer risk varies significantly by race/ethnicity and ranges from 4.60% (95% CI 4.40% to 4.81%) for Hispanics to 8.10% (95% CI 7.94% to 8.20%) for whites. Although the 95% CIs around risks for HER2-positive breast cancer do not overlap between most racial/ethnic groups (for example, Hispanics 1.56%, 95% CI 1.46% to 1.68% and Asians 1.91%, 95% CI 1.78% to 2.07%), the risk differences are smaller in magnitude than for the luminal subtype. For triple-negative breast cancer, blacks have the highest lifetime risk at 1.98% (95% CI 1.80% to 2.17%), which is significantly greater than that of Asian (0.77%, 95% CI 0.67% to 0.88%), Hispanic (1.04%, 95% CI 0.96% to 1.13%), and white (1.25%, 95% CI 1.20% to 1.30%) women. For all races and all subtypes combined, overall absolute risk is 12.3% (95% CI 12.2% to 12.4%), which is consistent with 1 in 8 women developing breast cancer in her lifetime. Figure 1 presents race-specific incidence curves for each subtype.
Age-specific incidence of breast cancer. Incidence is expressed as rates per 100,000 by age (in years) for subtypes - luminal (ER- or PR-positive or both and HER2-negative), HER2-positive (ER- and PR-positive or -negative and HER2-positive), and triple-negative (ER-negative, PR-negative, and HER2-negative) - and for racial/ethnic groups: (a) whites, (b) blacks, (c) Hispanics, and (d) Asians. ER, estrogen receptor; HER2, Her2/neu; PR, progesterone receptor.
Absolute risks by age and racial/ethnic group
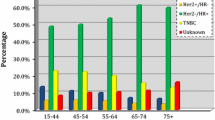
Table 3 presents age-specific risks for breast cancer subtypes for women who are unaffected by cancer at age 40. Between the ages of 40 and 49, white women have 0.87% (95% CI 0.84% to 0.90%) probability of developing luminal breast cancer, 0.27% (95% CI 0.25% to 0.29%) probability of developing HER2-positive breast cancer, and 0.17% (95% CI 0.16% to 0.19%) probability of developing triple-negative breast cancer; for blacks, corresponding probabilities are 0.59% (95% CI 0.52% to 0.66%), 0.31% (95% CI 0.26% to 0.37%), and 0.34% (95% CI 0.29% to 0.40%). For all races, nearly half the lifetime probability of developing luminal breast cancer occurs after age 70, whereas triple-negative breast cancer and HER2-positive breast cancer subtypes have an earlier age distribution, as shown in Figure 2. The Supplemental table (Additional file 1) presents age-specific risks in 10-, 20-, and 30-year intervals in addition to lifetime risks for women ages 20 to 80 by race/ethnicity and by breast cancer subtype.
Distribution of breast cancer subtypes by age. Distribution is expressed as a percentage, and age is expressed in years. Subtypes are defined as (a) luminal (ER- or PR-positive or both and HER2-negative), (b) HER2-positive (ER- and PR-positive or -negative and HER2-positive), and (c) triple-negative (ER-negative, PR-negative, and HER2-negative). ER, estrogen receptor; HER2, Her2/neu; PR, progesterone receptor.
Conclusions
We present lifetime and age-specific probabilities of developing luminal (ER- or PR-positive or both and HER2-negative), HER2-positive (ER- and PR-positive or -negative and HER2-positive), and triple-negative (ER-, PR-, and HER2-negative) subtypes of breast cancer for women from four racial/ethnic groups and use the most recently available data from the large and diverse population of California. These estimates refine the frequently cited 'one in eight' statistic [12], which fails to capture the substantial differences in epidemiology and prognosis among breast cancer subtypes [6–9, 16, 17]. Most importantly, these estimates facilitate clinically relevant discussion between patients and physicians. For women considering prevention strategies such as prophylactic tamoxifen or raloxifene, which reduce the incidence of only certain subtypes of breast cancer [30, 31], or screening methods such as magnetic resonance imaging (MRI), which may contribute more to the detection of triple-negative than luminal cancers [9, 10], our estimates may inform decisions about managing breast cancer risk. A woman at low risk for a specific subtype might choose to forego particular interventions and their side effects (for example, stroke and uterine cancer from tamoxifen or false-positive biopsies from screening mammogram or MRI) [30, 32], depending on the relative importance of such side effects and her competing health risks.
We present statistics separately for women in four major racial/ethnic groupings because lifetime risks for breast cancer as a whole vary substantially by these groups. Most notable were the significantly increased risks of luminal breast cancer among whites and of triple-negative breast cancer among black women. Our findings are consistent with studies reporting greater relative risks of triple-negative breast cancer among black women [5, 7, 8, 33] and strengthen the rationale for investigating genetic, reproductive, and lifestyle factors that may mediate this racial difference, such as age at menarche, family cancer history, breastfeeding, and abdominal adiposity [34, 35]. In all groups, the luminal subtype was the most common one. This universal predominance of luminal (ER- or PR-positive or both and HER2-negative) breast cancer, regardless of race, may be reassuring since this subtype has the best survival [5, 17], can be targeted by existing chemoprevention agents [30, 31], and may be most readily detectable by screening mammography [9, 10, 36, 37]. Although the disproportionately increased risk among black women of poor-prognosis triple-negative breast cancer warrants further study and targeted interventions, black women may be reassured to learn that they also have a high probability of avoiding this disease over their lifetimes.
It is essential to differentiate risks according to a woman's current age. A prior analysis using SEER data characterized qualitative patterns of breast cancer incidence according to ER status and reported an age-related crossover between black and white women [38]. We found that, for all races and for all subtypes, absolute breast cancer risks were low between ages 40 and 49 years: less than 1% per subtype and less than 2% for all subtypes combined. For women between ages 50 and 59, risks of each subtype increased substantially, and the greatest increase was for luminal breast cancers in white women. Nearly half the lifetime risk of luminal breast cancer, the dominant subtype for all racial/ethnic groups, occurred at or after age 70. These findings are important to the ongoing critical examination of mammographic screening guidelines [32, 36, 39] and may warrant extending recommendations for mammographic screening beyond the current upper limit of 69 years of age [32].
Our analyses have certain limitations, which should be considered in interpreting our results. Given the DevCan program's competing-risks methodology, cause-specific mortality is required to calculate incidence of the cancer in question [23, 25]; we used overall US breast cancer mortality rates to calculate subtype-specific incidence [28] because subtype-specific mortality rates are not available. However, since overall breast cancer mortality is low at the population level, this is unlikely to affect our risk estimates substantially. Racial misclassification might present another potential source of bias, but given that prior studies of the CCR found that race data derive from patient self-report in more than 80% of cases [21], it seems improbable that a large proportion were incorrectly classified. We excluded 7,737 cases (18.9%) from analysis because of missing ER, PR, or HER2 information; since there were no major differences in race or age distribution between the excluded and included cases, the lack of information on these cases seems unlikely to have biased our findings. Although defining subtypes by ER, PR, and HER2 expression does not entirely approximate results of genomic profiling, this classification offers a practical substitute that is increasingly well characterized in published literature [5, 7–9, 40–42] and that guides breast cancer treatment [43].
This study reports average lifetime risks at the population level; it does not address the urgent need for more accurate risk stratification of individual patients or the limitations of current breast cancer risk prediction models [44]. Genetic mutations such as BRCA1 convey dramatically increased risks of triple-negative breast cancer [45, 46], and the results of genome-wide association studies may eventually guide even more personalized risk prediction [47, 48]. Our estimates may inform health policy and resource planning across diverse populations and may help patients and clinicians to weigh the average probabilities of developing specific breast cancer subtypes against other competing health risks.
Abbreviations
- CCR:
-
California Cancer Registry
- CI:
-
confidence interval
- ER:
-
estrogen receptor
- HER2:
-
Her2/neu
- IHC:
-
immunohistochemistry
- MRI:
-
magnetic resonance imaging
- NCHS:
-
National Center for Health Statistics
- NH:
-
non-Hispanic
- PR:
-
progesterone receptor
- SEER:
-
Surveillance: Epidemiology and End Results.
References
Fan C, Oh DS, Wessels L, Weigelt B, Nuyten DS, Nobel AB, van't Veer LJ, Perou CM: Concordance among gene-expression-based predictors for breast cancer. N Engl J Med. 2006, 355: 560-569. 10.1056/NEJMoa052933.
Perou CM, Jeffrey SS, van de Rijn M, Rees CA, Eisen MB, Ross DT, Pergamenschikov A, Williams CF, Zhu SX, Lee JC, Lashkari D, Shalon D, Brown PO, Botstein D: Distinctive gene expression patterns in human mammary epithelial cells and breast cancers. Proc Natl Acad Sci USA. 1999, 96: 9212-9217. 10.1073/pnas.96.16.9212.
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lonning PE, Borresen-Dale AL, Brown PO, Botstein D: Molecular portraits of human breast tumours. Nature. 2000, 406: 747-752. 10.1038/35021093.
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, Deng S, Johnsen H, Pesich R, Geisler S, Demeter J, Perou CM, Lonning PE, Brown PO, Borresen-Dale AL, Botstein D: Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA. 2003, 100: 8418-8423. 10.1073/pnas.0932692100.
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S, Deming SL, Geradts J, Cheang MC, Nielsen TO, Moorman PG, Earp HS, Millikan RC: Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006, 295: 2492-2502. 10.1001/jama.295.21.2492.
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V: Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer. 2007, 109: 1721-1728. 10.1002/cncr.22618.
Lund MJ, Trivers KF, Porter PL, Coates RJ, Leyland-Jones B, Brawley OW, Flagg EW, O'Regan RM, Gabram SG, Eley JW: Race and triple negative threats to breast cancer survival: a population-based study in Atlanta, GA. Breast Cancer Res Treat. 2009, 113: 357-370. 10.1007/s10549-008-9926-3.
Stead LA, Lash TL, Sobieraj JE, Chi DD, Westrup JL, Charlot M, Blanchard RA, Lee JC, King TC, Rosenberg CL: Triple-negative breast cancers are increased in black women regardless of age or body mass index. Breast Cancer Res. 2009, 11: R18-10.1186/bcr2242.
Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, Lickley LA, Rawlinson E, Sun P, Narod SA: Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007, 13: 4429-4434. 10.1158/1078-0432.CCR-06-3045.
Yang WT, Dryden M, Broglio K, Gilcrease M, Dawood S, Dempsey PJ, Valero V, Hortobagyi G, Atchley D, Arun B: Mammographic features of triple receptor-negative primary breast cancers in young premenopausal women. Breast Cancer Res Treat. 2008, 111: 405-410. 10.1007/s10549-007-9810-6.
Li CI, Daling JR, Porter PL, Tang MT, Malone KE: Relationship between potentially modifiable lifestyle factors and risk of second primary contralateral breast cancer among women diagnosed with estrogen receptor-positive invasive breast cancer. J Clin Oncol. 2009, 27: 5312-5318. 10.1200/JCO.2009.23.1597.
Li CI, Mathes RW, Bluhm EC, Caan B, Cavanagh MF, Chlebowski RT, Michael Y, O'Sullivan MJ, Stefanick ML, Prentice R: Migraine history and breast cancer risk among postmenopausal women. J Clin Oncol. 2010, 28: 1005-1010. 10.1200/JCO.2009.25.0423.
Ma H, Luo J, Press MF, Wang Y, Bernstein L, Ursin G: Is there a difference in the association between percent mammographic density and subtypes of breast cancer? Luminal A and triple-negative breast cancer. Cancer Epidemiol Biomarkers Prev. 2009, 18: 479-485. 10.1158/1055-9965.EPI-08-0805.
Phipps AI, Malone KE, Porter PL, Daling JR, Li CI: Reproductive and hormonal risk factors for postmenopausal luminal, HER-2-overexpressing, and triple-negative breast cancer. Cancer. 2008, 113: 1521-1526. 10.1002/cncr.23786.
Phipps AI, Malone KE, Porter PL, Daling JR, Li CI: Body size and risk of luminal, HER2-overexpressing, and triple-negative breast cancer in postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2008, 17: 2078-2086. 10.1158/1055-9965.EPI-08-0206.
Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, Ollila DW, Sartor CI, Graham ML, Perou CM: The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007, 13: 2329-2334. 10.1158/1078-0432.CCR-06-1109.
Parise CA, Bauer KR, Brown MM, Caggiano V: Breast cancer subtypes as defined by the estrogen receptor (ER), progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2) among women with invasive breast cancer in California, 1999-2004. Breast J. 2009, 15: 593-602. 10.1111/j.1524-4741.2009.00822.x.
Liedtke C, Mazouni C, Hess KR, Andre F, Tordai A, Mejia JA, Symmans WF, Gonzalez-Angulo AM, Hennessy B, Green M, Cristofanilli M, Hortobagyi GN, Pusztai L: Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008, 26: 1275-1281. 10.1200/JCO.2007.14.4147.
Surveillance, Epidemiology and End Results. [http://seer.cancer.gov/]
California Cancer Reporting System Standards. Cancer Reporting in California, System Standards: Abstracting and Coding Procedures for Hospitals. 2008, Sacramento, CA: California Cancer Registry, Data Standards and Quality Control Unit, 1: 8
Gomez SL, Le GM, West DW, Satariano WA, O'Connor L: Hospital policy and practice regarding the collection of data on race, ethnicity, and birthplace. Am J Public Health. 2003, 93: 1685-1688. 10.2105/AJPH.93.10.1685.
Huober J, von Minckwitz G, Denkert C, Tesch H, Weiss E, Zahm DM, Belau A, Khandan F, Hauschild M, Thomssen C, Hogel B, Darb-Esfahani S, Mehta K, Loibl S: Effect of neoadjuvant anthracycline-taxane-based chemotherapy in different biological breast cancer phenotypes: overall results from the GeparTrio study. Breast Cancer Res Treat. 2010, 124: 133-140. 10.1007/s10549-010-1103-9.
DevCan - Probability of Developing or Dying of Cancer. [http://srab.cancer.gov/devcan/]
Fay MP: Estimating age conditional probability of developing disease from surveillance data. Popul Health Metr. 2004, 2: 6-10.1186/1478-7954-2-6.
Fay MP, Pfeiffer R, Cronin KA, Le C, Feuer EJ: Age-conditional probabilities of developing cancer. Stat Med. 2003, 22: 1837-1848. 10.1002/sim.1428.
Feuer EJ, Wun LM, Boring CC, Flanders WD, Timmel MJ, Tong T: The lifetime risk of developing breast cancer. J Natl Cancer Inst. 1993, 85: 892-897. 10.1093/jnci/85.11.892.
Wun LM, Merrill RM, Feuer EJ: Estimating lifetime and age-conditional probabilities of developing cancer. Lifetime Data Anal. 1998, 4: 169-186. 10.1023/A:1009685507602.
National Center for Health Statistics homepage. [http://www.cdc.gov/nchs/index.htm]
Bernstein JL, Lapinski RH, Thakore SS, Doucette JT, Thompson WD: The descriptive epidemiology of second primary breast cancer. Epidemiology. 2003, 14: 552-558. 10.1097/01.ede.0000072105.39021.6d.
Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, Bevers TB, Kavanah MT, Atkins JN, Margolese RG, Runowicz CD, James JM, Ford LG, Wolmark N: Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst. 2005, 97: 1652-1662. 10.1093/jnci/dji372.
Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, Bevers TB, Fehrenbacher L, Pajon ER, Wade JL, Robidoux A, Margolese RG, James J, Lippman SM, Runowicz CD, Ganz PA, Reis SE, McCaskill-Stevens W, Ford LG, Jordan VC, Wolmark N: Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006, 295: 2727-2741. 10.1001/jama.295.23.joc60074.
Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L: Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009, 151: 727-737. W237-742
Huo D, Ikpatt F, Khramtsov A, Dangou JM, Nanda R, Dignam J, Zhang B, Grushko T, Zhang C, Oluwasola O, Malaka D, Malami S, Odetunde A, Adeoye AO, Iyare F, Falusi A, Perou CM, Olopade OI: Population differences in breast cancer: survey in indigenous African women reveals over-representation of triple-negative breast cancer. J Clin Oncol. 2009, 27: 4515-4521. 10.1200/JCO.2008.19.6873.
Millikan RC, Newman B, Tse CK, Moorman PG, Conway K, Dressler LG, Smith LV, Labbok MH, Geradts J, Bensen JT, Jackson S, Nyante S, Livasy C, Carey L, Earp HS, Perou CM: Epidemiology of basal-like breast cancer. Breast Cancer Res Treat. 2008, 109: 123-139. 10.1007/s10549-007-9632-6.
Yang XR, Sherman ME, Rimm DL, Lissowska J, Brinton LA, Peplonska B, Hewitt SM, Anderson WF, Szeszenia-Dabrowska N, Bardin-Mikolajczak A, Zatonski W, Cartun R, Mandich D, Rymkiewicz G, Ligaj M, Lukaszek S, Kordek R, Garcia-Closas M: Differences in risk factors for breast cancer molecular subtypes in a population-based study. Cancer Epidemiol Biomarkers Prev. 2007, 16: 439-443. 10.1158/1055-9965.EPI-06-0806.
Esserman L, Shieh Y, Thompson I: Rethinking screening for breast cancer and prostate cancer. JAMA. 2009, 302: 1685-1692. 10.1001/jama.2009.1498.
Ikeda DM, Andersson I, Wattsgard C, Janzon L, Linell F: Interval carcinomas in the Malmo Mammographic Screening Trial: radiographic appearance and prognostic considerations. AJR Am J Roentgenol. 1992, 159: 287-294.
Anderson WF, Rosenberg PS, Menashe I, Mitani A, Pfeiffer RM: Age-related crossover in breast cancer incidence rates between black and white ethnic groups. J Natl Cancer Inst. 2008, 100: 1804-1814. 10.1093/jnci/djn411.
Partridge AH, Winer EP: On mammography--more agreement than disagreement. N Engl J Med. 2009, 361: 2499-2501. 10.1056/NEJMp0911288.
Dawood S, Broglio K, Kau SW, Green MC, Giordano SH, Meric-Bernstam F, Buchholz TA, Albarracin C, Yang WT, Hennessy BT, Hortobagyi GN, Gonzalez-Angulo AM: Triple receptor-negative breast cancer: the effect of race on response to primary systemic treatment and survival outcomes. J Clin Oncol. 2009, 27: 220-226. 10.1200/JCO.2008.17.9952.
Tan DS, Marchio C, Jones RL, Savage K, Smith IE, Dowsett M, Reis-Filho JS: Triple negative breast cancer: molecular profiling and prognostic impact in adjuvant anthracycline-treated patients. Breast Cancer Res Treat. 2008, 111: 27-44. 10.1007/s10549-007-9756-8.
Blows FM, Driver KE, Schmidt MK, Broeks A, van Leeuwen FE, Wesseling J, Cheang MC, Gelmon K, Nielsen TO, Blomqvist C, Heikkila P, Heikkinen T, Nevanlinna H, Akslen LA, Begin LR, Foulkes WD, Couch FJ, Wang X, Cafourek V, Olson JE, Baglietto L, Giles GG, Severi G, McLean CA, Southey MC, Rakha E, Green AR, Ellis IO, Sherman ME, Lissowska J, et al: Subtyping of breast cancer by immunohistochemistry to investigate a relationship between subtype and short and long term survival: a collaborative analysis of data for 10,159 cases from 12 studies. PLoS Med. 2010, 7: e1000279-10.1371/journal.pmed.1000279.
Carlson RW, Allred DC, Anderson BO, Burstein HJ, Carter WB, Edge SB, Erban JK, Farrar WB, Goldstein LJ, Gradishar WJ, Hayes DF, Hudis CA, Jahanzeb M, Kiel K, Ljung BM, Marcom PK, Mayer IA, McCormick B, Nabell LM, Pierce LJ, Reed EC, Smith ML, Somlo G, Theriault RL, Topham NS, Ward JH, Winer EP, Wolff AC: Breast cancer. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2009, 7: 122-192.
Amir E, Freedman OC, Seruga B, Evans DG: Assessing women at high risk of breast cancer: a review of risk assessment models. J Natl Cancer Inst. 2010, 102: 680-691. 10.1093/jnci/djq088.
Atchley DP, Albarracin CT, Lopez A, Valero V, Amos CI, Gonzalez-Angulo AM, Hortobagyi GN, Arun BK: Clinical and pathologic characteristics of patients with BRCA-positive and BRCA-negative breast cancer. J Clin Oncol. 2008, 26: 4282-4288. 10.1200/JCO.2008.16.6231.
Chen S, Parmigiani G: Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol. 2007, 25: 1329-1333. 10.1200/JCO.2006.09.1066.
Reeves GK, Travis RC, Green J, Bull D, Tipper S, Baker K, Beral V, Peto R, Bell J, Zelenika D, Lathrop M: Incidence of breast cancer and its subtypes in relation to individual and multiple low-penetrance genetic susceptibility loci. JAMA. 2010, 304: 426-434. 10.1001/jama.2010.1042.
Wacholder S, Hartge P, Prentice R, Garcia-Closas M, Feigelson HS, Diver WR, Thun MJ, Cox DG, Hankinson SE, Kraft P, Rosner B, Berg CD, Brinton LA, Lissowska J, Sherman ME, Chlebowski R, Kooperberg C, Jackson RD, Buckman DW, Hui P, Pfeiffer R, Jacobs KB, Thomas GD, Hoover RN, Gail MH, Chanock SJ, Hunter DJ: Performance of common genetic variants in breast-cancer risk models. N Engl J Med. 2010, 362: 986-993. 10.1056/NEJMoa0907727.
Acknowledgements
This study was supported by the National Cancer Institute (NCI) Surveillance, Epidemiology and End Results (SEER) program under contract N01-PC-35136. The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the NCI SEER program under contract N01-PC-35136 awarded to the Cancer Prevention Institute of California (formerly the Northern California Cancer Center), contract N01-PC-35139 awarded to the University of Southern California, and contract N01-PC-54404 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention's National Program of Cancer Registries, under agreement 1U58DP00807-01 awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the authors, and endorsement by the State of California, Department of Public Health, the NCI, or the Centers for Disease Control and Prevention or their contractors and subcontractors is not intended nor should it be inferred.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AWK conceived of the study, participated in study design and data interpretation, and drafted the manuscript. KF and SJS participated in study design and performed statistical analysis. CAC conceived of the study; participated in study design, analysis, and interpretation; and helped to draft the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
13058_2010_2759_MOESM1_ESM.PDF
Additional File 1: Supplemental table. Absolute risk (%) to develop breast cancer in specific age intervals, for cancer-free women by subtype and race/ethnicity. (PDF 22 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kurian, A.W., Fish, K., Shema, S.J. et al. Lifetime risks of specific breast cancer subtypes among women in four racial/ethnic groups. Breast Cancer Res 12, R99 (2010). https://doi.org/10.1186/bcr2780
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/bcr2780