Abstract
The widespread introduction of high throughput RNA interference screening technology has revealed tumour drug sensitivity pathways to common cytotoxics such as paclitaxel, doxorubicin and 5-fluorouracil, targeted agents such as trastuzumab and inhibitors of AKT and Poly(ADP-ribose) polymerase (PARP) as well as endocrine therapies such as tamoxifen. Given the limited power of microarray signatures to predict therapeutic response in associative studies of small clinical trial cohorts, the use of functional genomic data combined with expression or sequence analysis of genes and microRNAs implicated in drug response in human tumours may provide a more robust method to guide adjuvant treatment strategies in breast cancer that are transferable across different expression platforms and patient cohorts.
Similar content being viewed by others
Introduction
The fact that a large number of patients, who could otherwise be spared, are exposed to the severe side effects of chemotherapy necessitates an improved classification of breast cancer in the adjuvant setting in order to define patient groups who will benefit from the addition of adjuvant chemotherapy (and as a consequence, those patients who will not benefit from treatment). At the recent St Gallen conference it was recognised that: "perhaps the most difficult decision in current adjuvant therapy is selection of patients with highly or incompletely responsive disease for whom additional chemotherapy should be given."
Traditional clinical and pathological factors, based on several decades of clinical experience, guide this decision process. The introduction of genome-scale gene expression profiling has promised an improved understanding of breast cancer and identified distinct gene expression signatures that reflect prognosis in retrospective patient cohorts. However, conceptual and technical difficulties, such as tumour heterogeneity, the use of different array platforms and diverse statistical methods to analyse data, together with small sample sizes for each individual study, have caused serious concern [1]. While there are positive signs, such as that in independent datasets there is concordance amongst different gene expression signatures, it is not clear whether gene expression profiling simply captures already well known biological characteristics derived from careful phenotypic observations [2].
In this review, we present current evidence supporting the introduction of prognostic and chemosensitivity signatures into clinical practice and argue that uncertainties associated with these signatures may be resolved through the functional validation of genes involved in drug sensitivity and response.
Prognostic gene expression signatures
Considerable effort has been dedicated to establishing new prognostic strategies using genomic expression signatures in breast cancer, with the ultimate goal of optimising the stratification of patients into high and low risk groups to guide adjuvant decision-making [3–7]. The strategy is similar to the current adjuvant prescribing model in breast cancer that is focussed on administering chemotherapy to those most at risk whilst minimising harm by defining good prognostic cohorts who will not benefit from chemotherapy. However, it has been argued that the use of small number of patients with heterogeneous primary breast tumour types, often from retrospective cohorts, that these prognostic signatures were either derived or validated from should warrant caution [8, 9]. For example, the disproportion between the number of probe sets on microarray platforms (and hence the number of variables tested) and the number of tumour samples examined in each clinical study risks the 'overfitting' of data and a high false discovery rate.
There is limited evidence that prognostic signature sets predict chemosensitivity and long-term benefit from adjuvant chemotherapy or guide the choice of treatment regimen. It is also unclear to what extent these signatures are capturing traditional histopathological variables or substituting for the use of conventional prognostic strategies such as the Nottingham Prognostic Index or Adjuvant! Online. In this regard, Eden and colleagues [10] provide evidence that the NKI 70-gene prognostic signature [3] may not out-perform traditional breast cancer prognostic markers such as the Nottingham Prognostic Index.
Two ambitious adjuvant clinical trials in breast cancer aim to prospectively assess the utility of gene expression prognostic signatures through microarray or real-time PCR analyses and will compare these methods to conventional prognostic strategies. The MINDACT (Microarray In Node negative Disease may Avoid ChemoTherapy) multicentre clinical trial [11] is a prospective, randomised study that aims to compare the NKI 70-gene expression signature [3] with clinicalpathological criteria (Adjuvant! Online) commonly used in selecting patients for adjuvant chemotherapy in node-negative breast cancer (Table 1). The primary objective is to confirm that patients with low risk molecular prognosis but high risk clinical prognosis can be safely spared chemotherapy without affecting distant metastasis free survival. A second study, run by the NCI, will assess the utility of Oncotype DX, a 21-gene (16 genes and 5 control reference genes) RT-PCR assay developed from analysis of 3 breast cancer studies in 447 patients, to guide risk stratification for distant recurrence amongst patients with node negative, estrogen receptor (ER) positive breast cancer treated with tamoxifen [12]. The Trial Assigning IndividuaLized Options for Treatment (Rx) (TAILORx) [13] will examine the role of the recurrence score developed from this 21-gene assay in defining whether patients with ER or progesterone receptor positive and Her2 negative, node negative breast cancer can be safely spared chemotherapy. Secondary objectives aim to assess how the Genomic Health recurrence score compares against classical clinicopathological criteria.
Predictive genomic signatures of tumour drug sensitivity and response
The complexity of tumour cell cytotoxic response will involve the expression and post-translational modification of specific subsets of genes and microRNAs that may be distinct from those identified in prognostic signature sets. These cytotoxic response pathways exemplified by the Connectivity Map from the laboratories of Golub and colleagues [14] demonstrate that drugs with defined mechanisms of action share distinct molecular gene expression signatures. These data suggest that drug sensitivity pathways derived from such analyses are potentially exploitable in order to direct appropriate combination regimens to maximise tumour cytotoxicity or overcome drug resistance [14].
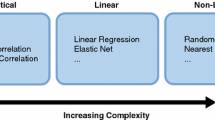
The concept of drug-specific response pathways that may be influenced by tumour genotype has led to efforts to identify predictive gene signatures of tumour drug sensitivity in order to individualise the choice of chemotherapy regimen and to achieve the goal of "personalised cancer medicine" [15]. Several groups have attempted to use breast cancer genomic signatures prior to treatment to predict short-term response to chemotherapy in the clinical setting in individual patient cohorts [16–20]. The unreliability and instability of gene expression signatures derived purely from associative studies is well documented [8, 9, 21, 22], contributing to failed attempts to define signatures predictive of response to common treatment regimens [23]. Such efforts have led to the conclusion that microarray analyses of small clinical trial cohorts may not yield a gene signature of sufficient power to predict drug sensitivity [23].
In order to improve the reliability of chemosensitivity predictive gene signatures, two laboratories have used cell line models to define gene expression signatures associated with drug response in vivo. Coexpression extrapolation (COXEN) is a recently reported method combining microarray expression data with NCI-60 drug sensitivity data to predict clinical response in human tumours [24]. The authors demonstrated that this approach could be used to predict drug sensitivity in cell lines derived from different primary tumours not included in the NCI-60. Next the authors tested the ability of COXEN to predict response to docetaxel monotherapy in a small breast cancer cohort of 24 patients. Although COXEN's accuracy was reduced compared to its ability to predict sensitivity of cell lines, its predictive power was still statistically significant. COXEN predicted 1 non-responder of the 11 patients sensitive to docetaxel and predicted 4 sensitive patients of 13 patients subsequently resistant to treatment. Of the non-responders, a further three patients with stable disease would have been predicted by COXEN to not respond to therapy.
In a similar approach, Nevins and colleagues [25] demonstrated that gene expression signatures deriving from the NCI-60 cell line set matched with cytotoxic sensitivity data could be used to predict response to chemotherapy in tumours from patients treated with the same drugs. Importantly, these signatures could be integrated to predict response to combined therapies. Recently, Bonnefoi and colleagues [26] presented data from the neoadjuvant phase III European Organisation for Research and Treatment of Cancer (EORTC) 10994/BIG 00-01 clinical trial comparing FEC to TET (docetaxel followed by epirupicin plus docetaxel) in an attempt to validate the Nevins and colleagues' data in a population of ER negative breast cancer patients. Their genomic signatures were the only independent variables predicting pathological complete response in 125 ER negative tumours. The authors conclude that selecting patients based on these regimen-specific signatures would increase the proportion of patients with pathological complete response from 44% to 70%. Furthermore, they contend that as the negative predictive value of each signature is so high, patients can now be excluded from conventional treatment regimens due to the ability to predict lack of benefit. These patients could in turn be prioritized for novel treatment strategies within the context of clinical trials.
This approach has been questioned by a bioinformatics team from the MD Anderson Cancer Center. Coombes and colleagues [27] argue that the NCI-60 cell line chemosensitivity data failed to predict patient response to chemotherapy when the authors attempted to replicate their analysis. The team were unable to reproduce the selection of cell lines used to establish the genomic signatures and noted methodological problems, including an "off-by-one" indexing error of probe set identification numbers, and the use of software that did not maintain independence of training and test sets. However, these arguments should be balanced against evidence published by the Nevins group providing confirmation of their datasets in the prediction of therapeutic response in breast cancer [26, 28].
These datasets await validation by independent groups in cohorts distinct from those used in the initial studies using alternative expression platforms. However, associative studies such as these provide minimal information regarding the contribution of individual genes to drug sensitivity, resistance and clinical response. Identifying core gene sets with a functional role in drug sensitivity may provide a more robust approach to the choice of therapeutic regimen and offer opportunities for therapeutic intervention in drug resistant disease.
Functional genomic approaches to predict chemosensitivity
The use of array-based datasets to predict prognosis in breast cancer and guide adjuvant decision-making provide an incomplete picture of a patient's likely benefit from chemotherapy. Even if prognostic signatures supplement traditional clinicopathological parameters in the stratification of risk in primary breast cancer, existing datasets provide little information guiding treatment regimen choice for individual patients. Conceivably, the future of adjuvant chemotherapy in breast cancer will rely not just on prognostic markers specific to the tumour/stroma environment but also on functional genomic markers of cytotoxic sensitivity and resistance to guide patient-specific adjuvant regimen decisions. For example, in patients at high risk of relapse, individuals may be identified who would be predicted to harbour multi-drug resistant micro-metastatic disease, who may not benefit from current combination regimens. In this regard, Bonnefoi, Nevins and colleagues [26] suggest their signatures can identify patients unlikely to benefit from chemotherapy who should be considered for phase I/II clinical trials using novel agents. The challenge is how to reliably identify and validate biomarkers of drug sensitivity and resistance and how to integrate these into future clinical strategies combined with optimal prognostic methods in order to stratify risk and guide regimen choice.
Identification of candidate biomarkers predictive of response to common cytotoxics
Following the widespread introduction of RNA interference (RNAi) technology, several methods have been developed to enable short or long term target gene silencing in cultured cells in the laboratory [29]. With such technology, it is now possible to systematically study the ability of individual genes to alter tumour cell sensitivity and resistance in a genome-wide manner. Using such methods, several laboratories have identified genes influencing resistance and sensitivity to diverse cytotoxics used in clinical practice.
Several RNAi functional genomic studies have identified drug-specific pathways of tumour cell resistance and sensitivity to diverse therapeutics. A kinome small interfering RNA (siRNA) screen performed in our laboratory to identify regulators of sensitivity and resistance to doxorubicin, cisplatin, 5-fluorouracil (5-FU) and paclitaxel revealed regulators of mitotic arrest and chromosomal instability as common mediators of resistance to paclitaxel in vitro [30–32]. White and colleagues [33] conducted a genome-wide siRNA screen in a human non-small cell lung cancer cell line with sub-lethal doses of paclitaxel. The silencing of 87 genes enhanced taxane-mediated cytotoxicity. The list included many proteosome components as synthetic enhancers of paclitaxel cytotoxicity, in keeping with the known efficacy of paclitaxel with proteosome inhibitors in cell culture model systems [34]. Four targets identified from their screen preferentially sensitised tumour cell lines in comparison to "normal" lines derived from the same patient.
A similar genome-wide study to identify enhancers of cisplatin cytotoxicity identified genes involved in the BRCA and DNA damage repair pathways (BARD1, BRCA1, BRCA2 and RAD51) that enhanced sensitivity to cisplatin following gene silencing [35]. This supports previous work demonstrating the association of the Fanconi Anemia/BRCA signalling pathway and cisplatin sensitivity [36].
Finally, cellular microRNAs are small non-coding RNAs with the capacity to coordinate the regulation of many genes simultaneously through mRNA degradation or translational silencing. Increasing evidence suggests that expression of distinct microRNAs in vitro and in vivo influences response and sensitivity to common chemotherapeutic agents [37–39].
Identification of candidate biomarkers predictive of response to targeted agents
Functional genomic RNAi analysis has provided novel insights into the mechanisms of action of established targeted therapies such as trastuzumab, or agents currently in phase I/II clinical trial development, such as Poly(ADP-ribose) polymerase (PARP) inhibitors.
Bernards and colleagues [40] recently presented data from a small hairpin RNA interference barcode screen targeting 8,000 genes in the Her2 positive BT-474 cell line. They identified that silencing the PTEN (Phosphatase and tensin homolog) tumour suppressor was the predominant regulator of trastuzumab resistance in this screen. Since PTEN inactivation is relatively infrequent in breast cancer and mutations of the upstream kinase PI3KCA (Phosphoinositide-3-kinase catalytic subunit alpha) occur in up to 25% of breast cancers [41], the authors examined the effects of PI3KCA activating mutations on trastuzumab sensitivity. They found that expression of both the activated mutant and wild-type PI3KCA subunits conferred trastuzumab resistance upon the Her2 positive, trastuzumab sensitive BT474 and SK-BR3 cell lines. Following examination of the effects of PI3K pathway activation on trastuzumab response in metastatic breast cancer, PI3KCA mutations alone (p = 0.052) or when combined with PTEN loss appeared to predict for worse outcome (p = 0.007) following trastuzumab monotherapy or in combination with chemotherapy. In a multivariate analysis, PI3K pathway activation appeared to be an independent prognostic predictor for progression on trastuzumab therapy. Studies in the adjuvant setting are now required to determine whether patients with Her2 positive disease with activation of the PI3K pathway derive limited benefit from trastuzumab therapy. In the future, perhaps, such patients would be optimally treated with AKT or mTOR/TORC1/TORC2 inhibitors, lying downstream of PI3K pathway activation, rather than trastuzumab.
Importantly, this study illustrates how the choice of the appropriate treatment regimen may never be entirely predictable from signatures of tumour gene expression since post-translational modifications or alterations in the coding sequence of components of the drug response pathway (such as PI3K) are not distinguished using these technologies. Therefore, for agents where the response pathways appear to be defined by a well categorised signal cascade, sequence and/or expression analysis of core components, such as EGFR, HER2, PI3KCA or PTEN, may provide more specific information to guide chemosensitivity than the analysis of PI3K/AKT pathway activation by gene expression profiling.
Turner and colleagues [42] recently reported an siRNA screen to identify regulators of sensitivity to a PARP inhibitor.
They identified several kinases, including CDK5, which promoted sensitivity to a PARP inhibitor when silenced in CAL51 cells. In elegant further experiments, the authors demonstrated the requirement for CDK5 in the DNA damage checkpoint activation and, specifically, the intra-S and G2M checkpoints in non-neuronal cells. The authors noted that CDK5 genomic loss occurred in approximately 5% of breast cancers studied, potentially identifying patients who may benefit from PARP inhibitor therapy. Prior to this study, CDK5 was thought to be a neuronal-specific kinase. This work demonstrates the power of RNAi to identify novel targets active in unexpected cell types.
Drug sensitivity prediction using functional genomics and array technology
There is accumulating evidence that RNAi functional data can be successfully combined with expression profiling data from human tumours to identify regulators of drug sensitivity. In our RNAi screen, we found that CERT, a ceramide transporter, sensitises multiple cancer cell types to diverse cytotoxics, and is over-expressed in multi-drug resistant and taxane-resistant cancer cell lines. Using expression profiling data from the CTCR-OV01 clinical trial, we identitifed that CERT is over-expressed in residual ovarian cancer tissue following paclitaxel therapy in vivo [30]. In a reverse approach, using expression profiling data to identify genes with a functional role in conferring drug resistance in vivo, we used a mixed effects model to identify individual genes correlating with carboplatin response using paired pre and post-treatment tumour biopsied. Importantly, many of these genes alter drug sensitivity in cultured cells in the laboratory (J Brenton and C Swanton, manuscript in preparation).
Ahmed and colleagues [43] presented data from an expression array-based approach to identify genes deregulated in matched paclitaxel-sensitive and -resistant ovarian cancer cell lines. They identified the extracellular matrix protein TGFBI as the most under-expressed gene in the paclitaxel-resistant cell line. Stable RNAi-mediated gene silencing of TGFBI promoted paclitaxel resistance and TGFBI was noted to be under-expressed in microarray expression data from taxane-resistant ovarian cancer from patients entered into the OV01 ovarian cancer clinical trial. The authors demonstrate the mechanism that TGFBI functions through an integrin-mediated signalling cascade to promote microtubule stabilisation. This work indicates that microarray expression profiling can be successfully combined with functional genomic validation to identify genes that may predict for resistance to common chemotherapeutic agents in vivo.
Ashworth and colleagues [44] recently reported an RNAi screen to identify regulators of resistance to tamoxifen in the MCF-7 cell line. They identified the cyclin dependent kinase CDK10, which promoted resistance to tamoxifen on gene silencing. Following an analysis of published microarray data, the authors demonstrated that tumours from patients treated with adjuvant tamoxifen with reduced CDK10 expression were at significantly higher risk of distant relapse. This work demonstrates the power of unbiased RNAi screens to identify candidate biomarkers of drug resistance in vivo.
In a focussed attempt to annotate drug response pathways and predict chemosensitivity in vivo, our laboratories are studying the functional consequences of consistent changes in gene expression following drug exposure. By silencing genes that are consistently repressed following drug exposure, we can mimic drug response and identify 'cytotoxic' genes within expression array datasets that may determine cell fate. Our data suggest that the expression of these 'cytotoxic' genes can identify tumours with intrinsic drug resistance in vivo (C Swanton and colleagues, submitted).
These studies suggest that the combination of unbiased genome-wide drug sensitivity analysis with array-based approaches may identify candidate genes with the capacity to influence cancer cell drug sensitivity in vivo. It is important to note, however, that candidate genes identified from these unbiased functional approaches still require extensive validation before they can be considered as putative biomarkers. It is also unclear whether these functional genomic approaches differentiate between intrinsic or acquired drug resistance pathways in tumour cells.
The next step will be to identify if these functional regulators of drug sensitivity can improve the prediction of chemosensitivity in prospective studies and whether they can be successfully combined with prognostic methods to guide the selection of appropriate chemotherapy regimens in a 'personalised' approach to improve patient outcome.
Functional genomic biomarker validation
Determining whether these functional regulators of drug sensitivity and resistance identified in laboratory studies can serve as putative biomarkers of clinical drug response to guide therapeutic decision-making remains a formidable challenge. Appropriate assays will have to be developed to quantify the expression of drug sensitivity regulators using array-based gene expression profiling, real-time PCR or immunohistochemistry in tumour samples prior to addressing their predictive value in prospective clinical trial cohorts. This should entail adherence to NCI-EORTC recommendations for biomarker validation [45], requiring the incorporation of stringent quality control procedures, accurate quantification and scoring methods and unbiased thresholding of expression values. The clinical validation of putative functional regulators of drug response will run the risk of failure similar to other biomarker development efforts unless strict reporting guidelines are adhered to, including the reporting of relationships to standard prognostic variables, often lacking from standard prognostic gene expression signature reports [45]. Finally, the NCI-EORTC recommend that predictive biomarker studies require even stricter considerations, requiring validation in large randomised trials with sufficient power to detect drug-specific differences in tumour response [45].
Conclusion
Optimising treatment strategies in primary breast cancer is of fundamental importance to reduce the risks of unnecessary treatment and to target adjuvant therapies to patients in a tumour-specific manner, utilising tumour biological characteristics to guide appropriate treatment decisions. There has been impressive progress in the last decade in deriving new prognostic strategies through the systematic analysis of whole genome mRNA expression changes in breast and other cancers. Although certain prognostic signatures may be potentially superior to clinical and histopathological criteria, they would still be predicted to lead to significant over-treatment of low-risk patients, indicating a need for alternative strategies to complement these signatures [46].
Further developments in functional genomic technologies are beginning to unravel the contribution of individual genes to intrinsic aspects of tumour biology, such as metastatic potential, uncontrolled cell proliferation, cellular invasion, migration and drug resistance. These efforts may help to identify tumours with multi-drug resistant phenotypes for which new treatment approaches are required. The complex integration of functional genomic drug response and sensitivity pathway analysis with tumour gene expression and sequencing data provides a promising strategy to optimise patient outcome in breast cancer and refine adjuvant and metastatic chemotherapy protocols on a patient-by-patient basis.
Abbreviations
- COXEN:
-
coexpression extrapolation
- EORTC:
-
European Organisation for Research and Treatment of Cancer
- ER:
-
estrogen receptor
- FU:
-
fluorouracil
- PARP:
-
Poly(ADP-ribose) polymerase
- RNAi:
-
RNA interference
- siRNA:
-
small interfering RNA.
References
Ein-Dor L, Kela I, Getz G, Givol D, Domany E: Outcome signature genes in breast cancer: is there a unique set?. Bioinformatics. 2005, 21: 171-178. 10.1093/bioinformatics/bth469.
Fan C, Oh DS, Wessels L, Weigelt B, Nuyten DS, Nobel AB, van't Veer LJ, Perou CM: Concordance among gene-expression-based predictors for breast cancer. N Engl J Med. 2006, 355: 560-569. 10.1056/NEJMoa052933.
van 't Veer LJ, Dai H, Vijver van de MJ, He YD, Hart AA, Mao M, Peterse HL, Kooy van der K, Marton MJ, Witteveen AT, Schreiber GJ, Kerkhoven RM, Roberts C, Linsley PS, Bernards R, Friend SH: Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002, 415: 530-536. 10.1038/415530a.
Vijver van de MJ, He YD, van't Veer LJ, Dai H, Hart AA, Voskuil DW, Schreiber GJ, Peterse JL, Roberts C, Marton MJ, Parrish M, Atsma D, Witteveen A, Glas A, Delahaye L, Velde van der T, Bartelink H, Rodenhuis S, Rutgers ET, Friend SH, Bernards R: A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002, 347: 1999-2009. 10.1056/NEJMoa021967.
Wang Y, Klijn JG, Zhang Y, Sieuwerts AM, Look MP, Yang F, Talantov D, Timmermans M, Meijer-van Gelder ME, Yu J, Jatkoe T, Berns EM, Atkins D, Foekens JA: Gene-expression profiles to predict distant metastasis of lymph-node-negative primary breast cancer. Lancet. 2005, 365: 671-679.
Naderi A, Teschendorff AE, Barbosa-Morais NL, Pinder SE, Green AR, Powe DG, Robertson JF, Aparicio S, Ellis IO, Brenton JD, Caldas C: A gene-expression signature to predict survival in breast cancer across independent data sets. Oncogene. 2007, 26: 1507-1516. 10.1038/sj.onc.1209920.
Carter SL, Eklund AC, Kohane IS, Harris LN, Szallasi Z: A signature of chromosomal instability inferred from gene expression profiles predicts clinical outcome in multiple human cancers. Nat Genet. 2006, 38: 1043-1048. 10.1038/ng1861.
Brenton JD, Carey LA, Ahmed AA, Caldas C: Molecular classification and molecular forecasting of breast cancer: ready for clinical application?. J Clin Oncol. 2005, 23: 7350-7360. 10.1200/JCO.2005.03.3845.
Ahmed AA, Brenton JD: Microarrays and breast cancer clinical studies: forgetting what we have not yet learnt. Breast Cancer Res. 2005, 7: 96-99. 10.1186/bcr1017.
Eden P, Ritz C, Rose C, Ferno M, Peterson C: "Good Old" clinical markers have similar power in breast cancer prognosis as microarray gene expression profilers. Eur J Cancer. 2004, 40: 1837-1841. 10.1016/j.ejca.2004.02.025.
MINDACT. [http://www.eortc.be/services/unit/mindact/documents/MINDACT_trial_outline.pdf]
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T, Hiller W, Fisher ER, Wickerham DL, Bryant J, Wolmark N: A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004, 351: 2817-2826. 10.1056/NEJMoa041588.
TAILORx. [http://www.cancer.gov/clinicaltrials/ECOG-PACCT-1]
Lamb J, Crawford ED, Peck D, Modell JW, Blat IC, Wrobel MJ, Lerner J, Brunet JP, Subramanian A, Ross KN, Reich M, Hieronymus H, Wei G, Armstrong SA, Haggarty SJ, Clemons PA, Wei R, Carr SA, Lander ES, Golub TR: The Connectivity Map: using gene-expression signatures to connect small molecules, genes, and disease. Science. 2006, 313: 1929-1935. 10.1126/science.1132939.
van't Veer LJ, Bernards R: Enabling personalized cancer medicine through analysis of gene-expression patterns. Nature. 2008, 452: 564-570. 10.1038/nature06915.
Chang JC, Wooten EC, Tsimelzon A, Hilsenbeck SG, Gutierrez MC, Elledge R, Mohsin S, Osborne CK, Chamness GC, Allred DC, O'Connell P: Gene expression profiling for the prediction of therapeutic response to docetaxel in patients with breast cancer. Lancet. 2003, 362: 362-369. 10.1016/S0140-6736(03)14023-8.
Hess KR, Anderson K, Symmans WF, Valero V, Ibrahim N, Mejia JA, Booser D, Theriault RL, Buzdar AU, Dempsey PJ, Rouzier R, Sneige N, Ross JS, Vidaurre T, Gomez HL, Hortobagyi GN, Pusztai L: Pharmacogenomic predictor of sensitivity to preoperative chemotherapy with paclitaxel and fluorouracil, doxorubicin, and cyclophosphamide in breast cancer. J Clin Oncol. 2006, 24: 4236-4244. 10.1200/JCO.2006.05.6861.
Iwao-Koizumi K, Matoba R, Ueno N, Kim SJ, Ando A, Miyoshi Y, Maeda E, Noguchi S, Kato K: Prediction of docetaxel response in human breast cancer by gene expression profiling. J Clin Oncol. 2005, 23: 422-431. 10.1200/JCO.2005.09.078.
Folgueira MA, Carraro DM, Brentani H, Patrão DF, Barbosa EM, Netto MM, Caldeira JR, Katayama ML, Soares FA, Oliveira CT, Reis LF, Kaiano JH, Camargo LP, Vêncio RZ, Snitcovsky IM, Makdissi FB, e Silva PJ, Góes JC, Brentani MM: Gene expression profile associated with response to doxorubicin-based therapy in breast cancer. Clin Cancer Res. 2005, 11: 7434-7443. 10.1158/1078-0432.CCR-04-0548.
Natowicz R, Incitti R, Horta EG, Charles B, Guinot P, Yan K, Coutant C, Andre F, Pusztai L, Rouzier R: Prediction of the outcome of preoperative chemotherapy in breast cancer by DNA probes that convey information on both complete and non complete responses. BMC bioinformatics. 2008, 9: 149-10.1186/1471-2105-9-149.
Michiels S, Koscielny S, Hill C: Prediction of cancer outcome with microarrays: a multiple random validation strategy. Lancet. 2005, 365: 488-492. 10.1016/S0140-6736(05)17866-0.
Ein-Dor L, Zuk O, Domany E: Thousands of samples are needed to generate a robust gene list for predicting outcome in cancer. Proc Natl Acad Sci USA. 2006, 103: 5923-5928. 10.1073/pnas.0601231103.
Sørlie T, Perou CM, Fan C, Geisler S, Aas T, Nobel A, Anker G, Akslen LA, Botstein D, Børresen-Dale AL, Lønning PE: Gene expression profiles do not consistently predict the clinical treatment response in locally advanced breast cancer. Mol Cancer Ther. 2006, 5: 2914-2918. 10.1158/1535-7163.MCT-06-0126.
Lee JK, Havaleshko DM, Cho H, Weinstein JN, Kaldjian EP, Karpovich J, Grimshaw A, Theodorescu D: A strategy for predicting the chemosensitivity of human cancers and its application to drug discovery. Proc Natl Acad Sci USA. 2007, 104: 13086-13091. 10.1073/pnas.0610292104.
Potti A, Dressman HK, Bild A, Riedel RF, Chan G, Sayer R, Cragun J, Cottrill H, Kelley MJ, Petersen R, Harpole D, Marks J, Berchuck A, Ginsburg GS, Febbo P, Lancaster J, Nevins JR: Genomic signatures to guide the use of chemotherapeutics. Nat Med. 2006, 12: 1294-1300. 10.1038/nm1491.
Bonnefoi H, Potti A, Delorenzi M, Mauriac L, Campone M, Tubiana-Hulin M, Petit T, Rouanet P, Jassem J, Blot E, Becette V, Farmer P, André S, Acharya CR, Mukherjee S, Cameron D, Bergh J, Nevins JR, Iggo RD: Validation of gene signatures that predict the response of breast cancer to neoadjuvant chemotherapy: a substudy of the EORTC 10994/BIG 00-01 clinical trial. Lancet Oncol. 2007, 8: 1071-1078. 10.1016/S1470-2045(07)70345-5.
Coombes KR, Wang J, Baggerly KA: Microarrays: retracing steps. Nat Med. 2007, 13: 1276-1277. 10.1038/nm1107-1276b.
Salter KH, Acharya CR, Walters KS, Redman R, Anguiano A, Garman KS, Anders CK, Mukherjee S, Dressman HK, Barry WT, Marcom KP, Olson J, Nevins JR, Potti A: An integrated approach to the prediction of chemotherapeutic response in patients with breast cancer. PLoS ONE. 2008, 3: e1908-10.1371/journal.pone.0001908.
Downward J: Use of RNA interference libraries to investigate oncogenic signalling in mammalian cells. Oncogene. 2004, 23: 8376-8383. 10.1038/sj.onc.1208073.
Swanton C, Marani M, Pardo O, Warne PH, Kelly G, Sahai E, Elustondo F, Chang J, Temple J, Ahmed AA, Brenton JD, Downward J, Nicke B: Regulators of mitotic arrest and ceramide metabolism are determinants of sensitivity to paclitaxel and other chemotherapeutic drugs. Cancer Cell. 2007, 11: 498-512. 10.1016/j.ccr.2007.04.011.
Swanton C, Nicke B, Marani M, Kelly G, Downward J: Initiation of high frequency multi-drug resistance following kinase targeting by siRNAs. Cell Cycle. 2007, 6: 2001-2004.
Harrison M, Swanton C: Epothilones and new analogues of the microtubule modulators in taxane-resistant disease. Expert Opin Investig Drugs. 2008, 17: 523-546. 10.1517/13543784.17.4.523.
Whitehurst AW, Bodemann BO, Cardenas J, Ferguson D, Girard L, Peyton M, Minna JD, Michnoff C, Hao W, Roth MG, Xie XJ, White MA: Synthetic lethal screen identification of chemosensitizer loci in cancer cells. Nature. 2007, 446: 815-819. 10.1038/nature05697.
Hernandez-Vargas H, von Kobbe C, Sanchez-Estevez C, Julian-Tendero M, Palacios J, Moreno-Bueno G: Inhibition of pacli-taxel-induced proteasome activation influences paclitaxel cytotoxicity in breast cancer cells in a sequence-dependent manner. Cell Cycle. 2007, 6: 2662-2668.
Bartz SR, Zhang Z, Burchard J, Imakura M, Martin M, Palmieri A, Needham R, Guo J, Gordon M, Chung N, Warrener P, Jackson AL, Carleton M, Oatley M, Locco L, Santini F, Smith T, Kunapuli P, Ferrer M, Strulovici B, Friend SH, Linsley PS: Small interfering RNA screens reveal enhanced cisplatin cytotoxicity in tumor cells having both BRCA network and TP53 disruptions. Mol Cell Biol. 2006, 26: 9377-9386. 10.1128/MCB.01229-06.
D'Andrea AD: The Fanconi Anemia/BRCA signaling pathway: disruption in cisplatin-sensitive ovarian cancers. Cell Cycle. 2003, 2: 290-292.
Nakajima G, Hayashi K, Xi Y, Kudo K, Uchida K, Takasaki K, Yamamoto M, Ju J: Non-coding microRNAs hsa-let-7g and hsa-miR-181b are associated with chemoresponse to S-1 in colon cancer. Cancer Genomics Proteomics. 2006, 3: 317-324.
Blower PE, Chung JH, Verducci JS, Lin S, Park JK, Dai Z, Liu CG, Schmittgen TD, Reinhold WC, Croce CM, Weinstein JN, Sadee W: MicroRNAs modulate the chemosensitivity of tumor cells. Mol Cancer Ther. 2008, 7: 1-9. 10.1158/1535-7163.MCT-07-0573.
Schetter AJ, Leung SY, Sohn JJ, Zanetti KA, Bowman ED, Yanaihara N, Yuen ST, Chan TL, Kwong DL, Au GK, Liu CG, Calin GA, Croce CM, Harris CC: MicroRNA expression profiles associated with prognosis and therapeutic outcome in colon adenocarcinoma. JAMA. 2008, 299: 425-436. 10.1001/jama.299.4.425.
Berns K, Horlings HM, Hennessy BT, Madiredjo M, Hijmans EM, Beelen K, Linn SC, Gonzalez-Angulo AM, Stemke-Hale K, Hauptmann M, Beijersbergen RL, Mills GB, Vijver van de MJ, Bernards R: A functional genetic approach identifies the PI3K pathway as a major determinant of trastuzumab resistance in breast cancer. Cancer Cell. 2007, 12: 395-402. 10.1016/j.ccr.2007.08.030.
Saal LH, Holm K, Maurer M, Memeo L, Su T, Wang X, Yu JS, Malmstrom PO, Mansukhani M, Enoksson J: PIK3CA mutations correlate with hormone receptors, node metastasis and ERBB2, and are mutually exclusive with PTEN loss in human breast carcinoma. Cancer Res. 2005, 65: 2554-2559. 10.1158/0008-5472-CAN-04-3913.
Turner NC, Lord CJ, Iorns E, Brough R, Swift S, Elliott R, Rayter S, Tutt AN, Ashworth A: A synthetic lethal siRNA screen identifying genes mediating sensitivity to a PARP inhibitor. EMBO J. 2008, 27: 1368-1377. 10.1038/emboj.2008.61.
Ahmed AA, Mills AD, Ibrahim AE, Temple J, Blenkiron C, Vias M, Massie CE, Iyer NG, McGeoch A, Crawford R, Nicke B, Downward J, Swanton C, Bell SD, Earl HM, Laskey RA, Caldas C, Brenton JD: The extracellular matrix protein TGFBI induces microtubule stabilization and sensitizes ovarian cancers to paclitaxel. Cancer Cell. 2007, 12: 514-527. 10.1016/j.ccr.2007.11.014.
Iorns E, Turner NC, Elliott R, Syed N, Garrone O, Gasco M, Tutt AN, Crook T, Lord CJ, Ashworth A: Identification of CDK10 as an important determinant of resistance to endocrine therapy for breast cancer. Cancer Cell. 2008, 13: 91-104. 10.1016/j.ccr.2008.01.001.
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM: REporting recommendations for tumour MARKer prognostic studies (REMARK). Br J Cancer. 2005, 93: 387-391. 10.1038/sj.bjc.6602678.
Piccart-Gebhart MJ, Sotiriou C: Adjuvant chemotherapy – yes or no? Prognostic markers in early breast cancer. Ann Oncol. 2007, 18 (Suppl 12): xii2-7. 10.1093/annonc/mdm532.
Acknowledgements
We would like to acknowledge the support of the University of Cambridge, Cancer Research UK and Hutchison Whampoa Limited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Swanton, C., Szallasi, Z., Brenton, J.D. et al. Functional genomic analysis of drug sensitivity pathways to guide adjuvant strategies in breast cancer. Breast Cancer Res 10, 214 (2008). https://doi.org/10.1186/bcr2159
Published:
DOI: https://doi.org/10.1186/bcr2159