Abstract
Changes in serum cartilage oligomeric matrix protein (COMP) were studied during a 6-month period from initiation of treatment of rheumatoid arthritis patients with either infliximab or etanercept, to elucidate whether the favourable results of tissue protection reported in clinical trials are corroborated by changing levels of circulating COMP. Rheumatoid arthritis patients commencing treatment with infliximab (N = 32) or etanercept (N = 17) were monitored in accordance with a structured protocol. Only patients who were not receiving glucocorticoids or who were on a stable dose of oral prednisolone (<10 mg daily) were included. Serum COMP was measured by a sandwich immunoassay based on two monoclonal antibodies against human COMP in samples obtained at treatment initiation and at 3 and 6 months. Serum COMP decreased at 3 months in both infliximab- and etanercept-treated patients (P < 0.001 and <0.005, respectively) and remained low at 6 months. There was no significant correlation between changes in or concentrations of serum COMP and serum C-reactive protein at any time point. A decrease in serum COMP was seen both in ACR20 responders (patients meeting the American College of Rheumatology criteria for 20% improvement) and in nonresponders. The pattern of changes of serum COMP, a marker for cartilage turnover, in these patient groups supports the interpretation that infliximab and etanercept have a joint protective effect. Serum COMP has potential as a useful marker for evaluating tissue effects of novel treatment modalities in rheumatoid arthritis.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic condition, which leads to varying degrees of functional impairment and disability. In early stages, symptoms reflecting the inflammatory process often predominate, whereas later the symptoms and consequences related to the extent of joint destruction increase [1]. Traditionally, treatment has focused on ameliorating the inflammation. Although rather effectively alleviating the symptoms related to the inflammatory process, most disease-modifying antirheumatic drugs used until very recently have been less effective in retarding the progressive joint destruction. The coupling between inflammation and subsequent joint destruction has thus been questioned [2].
A new era in antirheumatic therapy began when biologic agents that target specific cells or mediators in the disease process were developed and their feasibility was investigated in clinical trials. The first biologic principle tested in RA patients and shown to be dramatically effective in reducing the signs and symptoms of inflammation was blocking of tumour necrosis factor α (TNF-α) [3]. This was accomplished either by a monoclonal antibody, infliximab, or by a soluble receptor binding both TNF-α and TNF-β, etanercept [4–6]. Another principle tested was blocking of the effects of interleukin-1 using a receptor antagonist, which seemed somewhat less efficient in ameliorating inflammation [7]. In subsequent trials, the effect of blocking these cytokines on the progression of joint destruction has been tested. With radiography of hands and feet used as an end point, these treatment modalities show promise in retarding the destructive process [8–10].
Several drawbacks of clinical trials focusing on prevention of joint destruction can be identified. Since the rate of progression is slow, the trials must be conducted over a long period, preferably more than one year, to be able to detect changes. Furthermore, evaluation relies on radiographic assessment, which is time-consuming and, despite improvements during recent years, remains a subject of controversy regarding technical details [11]. Also, radiography is impractical in early stages of drug development, i.e. for proof of drug efficacy in small groups of patients or animals.
Alternative or complementary tools to assess progression of tissue damage should therefore facilitate the evaluation of treatments with the potential to modify structural joint damage. Molecular-marker technology is a tool that may aid in evaluating tissue effects of antirheumatic therapy [12]. One promising candidate is COMP (cartilage oligomeric matrix protein, also called thrombospondin-5), originally isolated and characterized in cartilage [13]. The first assay suitable for its measurement in serum and synovial fluid was described in 1992 and was based on a polyclonal antiserum and performed as an inhibition ELISA [14].
In this communication, we report the use of a novel sandwich ELISA using a combination of two monoclonal antibodies for the detection of COMP in serum. The purpose of the study was to monitor serum COMP changes during a 6-month period from initiation of treatment of RA patients with either infliximab or etanercept. By monitoring serum COMP, we wanted to elucidate whether the favourable results of tissue protection reported for the TNF-blockers could be corroborated by changing levels of a primarily cartilage-derived marker during treatment.
Materials and methods
Patients
Patients with RA who are treated with infliximab or etanercept at our unit are monitored in accordance with a structured clinical protocol [15]. All patients have consented to be included in the protocol. No formal approval by the ethics committe is required for this protocol, which is an integrated part of the routine management of these patients. The protocol includes repeated serum sampling. The sera are stored at -80°C [14]. The patients included in the present study were those who at a given time point were included in the protocol and had been treated for at least 6 months. They all fulfilled the American College of Rheumatology criteria for RA [16]. Only patients who were not receiving glucocorticoids or who were on a stable dose of prednisolone (<10 mg daily) were included in the study. Furthermore, no intra-articular glucocorticoid injections were given during the study period or 3 months prior to enrolment. The reason for the rigorous control of glucocorticoid administration was that previous studies had indicated that glucocorticoid treatment, whether oral or intra-articular, may modify serum COMP levels [12]. Infliximab and etanercept were given in accordance with the standard recommendations, i.e., for infliximab, infusion intravenously of 3 mg/kg body weight at baseline, week 2, and week 6 and then every 8 weeks, and, for etanercept, 25 mg subcutaneously twice weekly.
Quantification of serum COMP
Serum COMP was measured by a sandwich ELISA utilising two monoclonal antibodies directed against separate antigenic determinants on the human COMP molecule (AnaMar Medical, Lund, Sweden). The detection limit is <0.1 u/l and the intra-assay and inter-assay coefficient of variation is <5%. The assay is not influenced by rheumatoid factors. The serum concentrations of COMP obtained by this assay are highly correlated with serum levels obtained by the original inhibition assay (r values >0.9 in RA samples) (T Saxne and D Heinegård, unpublished). Samples obtained at baseline and after 3 and 6 months of therapy if available were analysed.
Statistical analyses
Comparisons were done by Wilcoxon's matched-pairs test, the Mann-Whitney U-test, or the chi-square test, where appropriate and correlations were calculated using Spearman's rank correlation coefficient. A P value of < 0.05 was considered significant.
Results
Some characteristics of the two groups of patients are shown in Table 1. There were no significant differences between the groups in the examined variables.
Serum concentrations of COMP decreased in patients treated with infliximab or etanercept (Figs 1 and 2). The decrease was apparent at the 3-month follow-up (P < 0.001 and < 0.005, respectively) and levels remained low after 6 months compared with baseline values, though not significant for etanercept. In the etanercept-treated group, serum COMP decreased in 15 of the 17 patients, whereas in the infliximab group, serum COMP decreased in 23 patients and remained unchanged or increased in 9 patients (no significant difference between the groups). The reason why some of the patients were not included after 6 months was in most cases that the prednisolone dosage had been changed and according to the inclusion criteria these patients were then not eligible for follow-up. Three patients had stopped taking TNF-blockers after the 3-month follow-up. The serum sample from the 3-month follow-up was missing for one patient taking etanercept, and sera from the 6-month follow-up were missing for two infliximab-treated patients.
Serum COMP (S-COMP) at baseline and after 3 and 6 months in rheumatoid arthritis patients treated with etanercept. Serum COMP was lower than at baseline after 3 months (P < 0.005). The levels remained low after 6 months, although not significantly lower than at baseline (P = 0.07). See text for details. COMP = cartilage oligomeric matrix protein (thrombospondin-5).
Serum COMP (S-COMP) at baseline and after 3 and 6 months in rheumatoid arthritis patients treated with infliximab. Serum COMP was lower than at baseline after 3 months (P < 0.001). The levels remained low after 6 months (P < 0.001 compared with baseline). For details, see text. COMP = cartilage oligomeric matrix protein (thrombospondin-5).
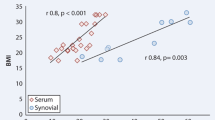
The most marked reduction in serum COMP was seen in the patients with the highest baseline values. The decrease was significant both in ACR20 responders (patients meeting the American College of Rheumatology criteria for 20% improvement) at 3 months and in nonresponders for both drugs (P < 0.05 or better) (Fig. 3). The COMP values did not correlate significantly with the C-reactive protein (CRP) values at any time point, nor did the changes (δ values) in CRP between time points correlate with those in COMP. The CRP values decreased significantly in the ACR20 responders in both infliximab- and etanercept-treated patients (P < 0.001 and P < 0.03, respectively), whereas in the nonresponders, no significant difference in CRP values between baseline and the 3-month follow-up was found. The baseline serum COMP levels did not differ between patients with or without prednisolone treatment.
Serum COMP (S-COMP) at baseline and after 3 months in rheumatoid arthritis patients treated with etanercept (a) or infliximab (b), grouped according to whether they were ACR20 responders (i.e., met the American College of Rheumatology criteria for 20% improvement) or nonresponders. Serum COMP was lower than at baseline after 3 months in all groups (P < 0.05 or better). For details, see text and Table 1.
Discussion
The COMP levels decreased in both treatment groups during the initial 3 months of therapy. This suggests that TNF blockade modifies the release of COMP from the tissue and supports the interpretation that this treatment modality retards the development of joint destruction, as previously indicated [8, 10]. Importantly, levels of COMP decreased both in responders and nonresponders. These observations taken together are consistent with the hypothesis that inflammation and tissue destruction are not directly linked, thus corroborating earlier published radiographic data on TNF blockade in RA [10]. This interpretation is further supported by the lack of correlation between CRP levels and between changes in CRP levels and changes in COMP levels. Although COMP is not unique to cartilage [17–19], the observations in this study clearly support a role for serum COMP as a marker reflecting processes not directly linked to the inflammation in RA. Having this characteristic, COMP adds to the variables that should be useful to include in the evaluation of potentially tissue-protective antirheumatic drugs. A recently published study in which the original inhibition assay was used for detection of serum COMP supports this conclusion [20]. In this study of adalimumab, a fully human anti-TNF-α monoclonal antibody, in RA, it was shown that baseline serum COMP was higher in the patient group whose disease progressed radiographically during a 2-year period. The COMP levels decreased during treatment in patients with radiographic progression but remained low and unchanged in patients with no progression.
We chose to include only patients without glucocorticoid treatment or with stable, low-dose prednisolone treatment, which considerably reduced the number of patients eligible. The reason for this action was, as pointed out above, that glucocorticoids tend to lower serum COMP levels. However, this effect does not seem to be due to the anti-inflammatory effect of glucocorticoids, since the lowering of serum COMP by glucocorticoids does not correspond to a decrease in inflammation, e.g. as measured by CRP or erythrocyte sedimentation rate (ESR) [12]. Instead, it could be hypothesized that the effect might be due to the joint protective effect suggested for glucocorticoids [21, 22]. Somewhat in contrast to previous findings, we did not in this study find any difference in baseline levels of COMP between low-dose prednisolone users and patients not taking prednisolone. We have no explanation for this. However, the possible effect of glucocorticoids on serum COMP needs to be considered when it is used as a biomarker, e.g. in drug trials or for clinical purposes.
A drawback of this study is the lack of radiographs for comparison with the changes in serum COMP levels. When we started to include patients in the protocol, we did not include radiographic follow-up, because we did not anticipate that treatment of patients with advanced RA with TNF blockers could substantially alter the radiographic appearance of the joints. It turns out that we were wrong. Furthermore, because of the observational nature of our protocol, no suitable group for comparison was available. Since our clinical results accord with the results of the pivotal trials of infliximab and etanercept that included radiographs, we believe that our study corroborates the results of these trials and that the findings support the use of COMP as a marker of cartilage processes in RA.
Conclusion
Serum COMP decreases during the first 3 months of treatment with etanercept or infliximab in patients with RA in a manner different from changes in symptoms and in levels of CRP. Thus, COMP shows promise as a non-inflammation-related marker of the disease process in RA, which should be useful for evaluating novel treatment modalities in the disease.
Abbreviations
- COMP:
-
cartilage oligomeric matrix protein (thrombospondin-5)
- CRP:
-
C-reactive protein
- ELISA:
-
enzyme-linked immunosorbent assay
- RA:
-
rheumatoid arthritis
- TNF-α:
-
tumour necrosis factor α.
References
Welsing PM, van Gestel AM, Swinkels HL, Kiemeney LA, van Riel PL: The relationship between disease activity, joint destruction, and functional capacity over the course of rheumatoid arthritis. Arthritis Rheum. 2001, 44: 2009-2017. 10.1002/1529-0131(200109)44:9<2009::AID-ART349>3.0.CO;2-L.
van den Berg WB: Uncoupling of inflammatory and destructive mechanisms in arthritis. Semin Arthritis Rheum. 2001, 30: 7-16. 10.1053/sarh.2001.23704.
Feldmann M, Maini RN: Discovery of TNF-alpha as a therapeutic target in rheumatoid arthritis: preclinical and clinical studies. Joint Bone Spine. 2002, 69: 12-18. 10.1016/S1297-319X(01)00335-9.
Elliott MJ, Maini RN, Feldmann M, Long-Fox A, Charles P, Katsikis P, Brennan FM, Walker J, Bijl H, Ghrayeb J, Woody JN: Treatment of rheumatoid arthritis with chimeric monoclonal antibodies to tumor necrosis factor alpha. Arthritis Rheum. 1993, 36: 1681-1690.
Elliott MJ, Maini RN, Feldmann M, Kalden JR, Antoni C, Smolen JS, Leeb B, Breedveld FC, Macfarlane JD, Bijl H, Woody JN: Randomised double-blind comparison of chimeric monoclonal antibody to tumour necrosis factor alpha (cA2) versus placebo in rheumatoid arthritis. Lancet. 1994, 344: 1105-1110. 10.1016/S0140-6736(94)90628-9.
Moreland LW, Baumgartner SW, Schiff MH, Tindall EA, Fleischmann RM, Weaver AL, Ettlinger RE, Cohen S, Koopman WJ, Mohler K, Widmer MB, Blosch CM: Treatment of rheumatoid arthritis with a recombinant human tumor necrosis factor receptor (p75)-Fc fusion protein. N Engl J Med. 1997, 337: 141-147. 10.1056/NEJM199707173370301.
Bresnihan B, Alvaro-Gracia JM, Cobby M, Doherty M, Domljan Z, Emery P, Nuki G, Pavelka K, Rau R, Rozman B, Watt I, Williams B, Aitchison R, McCabe D, Musikic P: Treatment of rheumatoid arthritis with recombinant human interleukin-1 receptor antagonist. Arthritis Rheum. 1998, 41: 2196-2204. 10.1002/1529-0131(199812)41:12<2196::AID-ART15>3.3.CO;2-U.
Bathon JM, Martin RW, Fleischmann RM, Tesser JR, Schiff MH, Keystone EC, Genovese MC, Wasko MC, Moreland LW, Weaver AL, Markenson J, Finck BK: A comparison of etanercept and methotrexate in patients with early rheumatoid arthritis. N Engl J Med. 2000, 343: 1586-1593. 10.1056/NEJM200011303432201.
Jiang Y, Genant HK, Watt I, Cobby M, Bresnihan B, Aitchison R, McCabe D: A multicenter, double-blind, dose-ranging, randomized, placebo-controlled study of recombinant human interleukin-1 receptor antagonist in patients with rheumatoid arthritis: radiologic progression and correlation of Genant and Larsen scores. Arthritis Rheum. 2000, 43: 1001-1009. 10.1002/1529-0131(200005)43:5<1001::AID-ANR7>3.0.CO;2-P.
Lipsky PE, van der Heijde DM, St Clair EW, Furst DE, Breedveld FC, Kalden JR, Smolen JS, Weisman M, Emery P, Feldmann M, Harriman GR, Maini RN: Infliximab and methotrexate in the treatment of rheumatoid arthritis. Anti-Tumor Necrosis Factor Trial in Rheumatoid Arthritis with Concomitant Therapy Study Group. N Engl J Med. 2000, 343: 1594-1602. 10.1056/NEJM200011303432202.
van der Heijde D, Simon L, Smolen J, Strand V, Sharp J, Boers M, Breedveld F, Weisman M, Weinblatt M, Rau R, Lipsky P: How to report radiographic data in randomized clinical trials in rheumatoid arthritis: guidelines from a roundtable discussion. Arthritis Rheum. 2002, 47: 215-218. 10.1002/art.10181.
Saxne T, Månsson B: Molecular markers for assessment of cartilage damage in rheumatoid arthritis. In Rheumatoid Arthritis: New Frontiers in Pathogenesis and Treatment. Edited by: Firestein G, Panayi GS, Wollheim FA. 2000, Oxford: Oxford University Press, 291-304.
Hedbom E, Antonsson P, Hjerpe A, Aeschlimann D, Paulsson M, Rosa-Pimentel E, Sommarin Y, Wendel M, Oldberg A, Heinegård D: Cartilage matrix proteins. An acidic oligomeric protein (COMP) detected only in cartilage. Biol Chem. 1992, 267: 6132-6136.
Saxne T, Heinegård D: Cartilage oligomeric matrix protein: a novel marker of cartilage turnover detectable in synovial fluid and blood. Br J Rheumatol. 1992, 31: 583-591.
Geborek P, Crnkic M, Petersson IF, Saxne T: Etanercept, infliximab, and leflunomide in established rheumatoid arthritis: clinical experience using a structured follow up programme in southern Sweden. Ann Rheum Dis. 2002, 61: 793-798. 10.1136/ard.61.9.793.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, Medsger TA, Mitchell DM, Neustadt DH, Pinals RS, Schaller JG, Sharp JT, Wilder RL, Hunder GG: The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-324.
DiCesare P, Hauser N, Lehman D, Pasumarti S, Paulsson M: Cartilage oligomeric matrix protein (COMP) is an abundant component of tendon. FEBS Lett. 1994, 354: 237-240. 10.1016/0014-5793(94)01134-6.
Smith RK, Zunino L, Webbon PM, Heinegård D: The distribution of cartilage oligomeric matrix protein (COMP) in tendon and its variation with tendon site, age and load. Matrix Biol. 1997, 16: 255-271. 10.1016/S0945-053X(97)90014-7.
Recklies AD, Baillargeon L, White C: Regulation of cartilage oligomeric matrix protein synthesis in human synovial cells and articular chondrocytes. Arthritis Rheum. 1998, 41: 997-1006. 10.1002/1529-0131(199806)41:6<997::AID-ART6>3.0.CO;2-G.
den Broeder AA, Joosten LA, Saxne T, Heinegård D, Fenner H, Miltenburg AM, Frasa WL, van Tits LJ, Buurman WA, van Riel PL, van de Putte LB, Barrera P: Long term anti-tumour necrosis factor alpha monotherapy in rheumatoid arthritis: effect on radiological course and prognostic value of markers of cartilage turnover and endothelial activation. Ann Rheum Dis. 2002, 61: 311-318. 10.1136/ard.61.4.311.
Kirwan JR: The effect of glucocorticoids on joint destruction in rheumatoid arthritis. The Arthritis and Rheumatism Council Low-Dose Glucocorticoid Study Group. N Engl J Med. 1995, 333: 142-146. 10.1056/NEJM199507203330302.
van Everdingen AA, Jacobs JW, Siewertsz Van Reesema DR, Bijlsma JW: Low-dose prednisone therapy for patients with early active rheumatoid arthritis: clinical efficacy, disease-modifying properties, and side effects: a randomized, double-blind, placebo-controlled clinical trial. Ann Intern Med. 2002, 136: 1-12.
Acknowledgements
Grants were obtained from the Swedish Medical Research Council, the Gustaf V 80-Year Foundation, the Greta and Johan Kock Foundation, Riksförbundet mot Reumatism, the Crafoord Foundation, the Nanna Svartz foundation, and the Medical Faculty of Lund University. The skilful technical assistance of Mrs Mette Lindell is appreciated.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
TS and DH are share-holders in AnaMar Medical.
Rights and permissions
About this article
Cite this article
Crnkic, M., Månsson, B., Larsson, L. et al. Serum cartilage oligomeric matrix protein (COMP) decreases in rheumatoid arthritis patients treated with infliximab or etanercept. Arthritis Res Ther 5, R181 (2003). https://doi.org/10.1186/ar760
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar760