Abstract
IFN-β treatment is emerging as a potentially effective form of therapy in various immune-mediated conditions. The present review addresses the possible role of IFN-β in immune-mediated diseases such as multiple sclerosis and rheumatoid arthritis. Several placebo-controlled trials are discussed, as are the available immunological data that are relevant to this field. Review of these data provides evidence that IFN-β has some beneficial therapeutic effect in patients with relapsing-remitting multiple sclerosis and might also have antirheumatic potential. This notion is supported by recent studies showing a critical role for IFN-β in bone homeostasis.
Similar content being viewed by others
Introduction
IFNs are a family of naturally secreted proteins with immunomodulatory functions. They enhance the ability of macrophages to destroy tumour cells, viruses and bacteria. The IFNs are divided into two types. Type 1 IFNs comprise IFN-α and IFN-β [1], and type 2 IFNs consist of IFN-γ alone. All type 1 IFNs probably originate from one common ancestral gene and are secreted in humans [2].
Under normal physiological conditions, type 1 IFNs are secreted endogenously by most human cells at low levels [3]. IFN-γ has a structure different from that of IFN-α and IFN-β, and acts through a unique receptor complex. IFN-β and IFN-γ appear to have opposing effects. IFN-γ promotes inflammatory responses whereas IFN-β has anti-inflammatory properties. IFN-γ can stimulate the production of chemokines, and is a powerful activator of mononuclear phagocytes, increasing their ability to destroy intracellular micro-organisms and tumour cells. Therefore, recombinant IFN-γ has been used clinically for the treatment of a variety of conditions, including chronic lymphocytic leukaemia, Hodgkin's disease and other disorders. IFN-γ has also been tried in immune-mediated diseases such as rheumatoid arthritis (RA) and multiple sclerosis (MS). IFN-γ was used in a multicentre, randomized, double-blind trial in 197 patients with active RA [4], which compared recombinant IFN-γ and placebo subcutaneously for a period of 24 weeks. However, it appeared to have no more therapeutic value than placebo. In MS patients, IFN-γ provoked disease exacerbation [5].
In contrast, IFN-β given to MS patients during clinical trials has been shown to reduce the relapse rate, to decrease disease activity on magnetic resonance imaging scans, and to delay disability progression [6–10]. The exact mechanism of action of IFN-β therapy is not precisely known at present. However, it has been shown that IFN-β downregulates the proinflammatory cytokines IL-1β and tumour necrosis factor (TNF)-α in vitro, and it enhances IL-10 and IL-1 receptor antagonist production [11–13]. Other possible effects of IFN-β treatment include the following (Fig. 1) [14]: enhancement of T-cell cytotoxity; regulation of antibody production; inhibition of T-cell proliferation and migration; enhancement of IL-2 production by Th1 cells; upregulation of transforming growth factor (TGF)-β1 and TGF-β-receptor 2 expression on peripheral blood mononuclear cells; downregulation of major histocompatibility complex class II expression on virus-infected cells and tumour cells; activation of natural killer cells; downregulation of several adhesion molecules; and enhancement of soluble adhesion molecules in serum.
Type 1 IFNs have also been found to be effective in antiangiogenic therapy for tumours such as haemangiomas [15, 16] and Kaposi's sarcoma [17]. The systemic administration of IFN-α and IFN-β can induce regression of vascularized tumours through a mechanism associated with endothelial cell damage, which leads to necrosis [18, 19]. Two pathways of angiogenesis have recently been identified, based on their dependence on the related but distinct integrins αvβ3 and αvβ5. Basic fibroblast growth factor enhanced angiogenesis is dependent on integrin αvβ3, whereas vascular endothelial growth factor enhanced angiogenesis requires αvβ5. IFN-β has been shown to downregulate basic fibroblast growth factor at mRNA and protein levels [20].
This antiangiogenic capacity of IFN-β may also be of relevance for the treatment of RA. The importance of angiogenesis in the maintenance of arthritis has been demonstrated in studies in which angiogenesis inhibitors were found to prevent onset of collagen-induced arthritis in rodents, and significantly suppressed established disease [21–23]. Furthermore, intra-articular administration of a cyclic peptide antagonist of αvβ3 in rabbits resulted in inhibition of synovial angiogenesis, as well as a reduction in joint swelling, synovial infiltrate and pannus formation, in both early and well established arthritis [24]. Importantly, in that study the αvβ3 antagonist provided significant protection against the development of cartilage erosions.
The present review addresses the possible role of IFN-β in immune-mediated diseases such as MS and RA.
Rationale for the use of IFN-β in multiple sclerosis
Because IFNs possess antiviral properties, the rationale for the use of IFN-β in MS in the past was based on the belief that viruses may play a role in causing MS, as well as triggering relapses of disease. At present MS is considered an autoimmune disease, associated with immune activity directed against an antigen derived from the central nervous system (CNS). It is known that macrophages, which express major histocompatibility complex class II molecules, present non-self antigens to T-cell receptors on Th1 cells. These activated T cells increase the expression of adhesion molecules such as intercellular adhesion molecule (ICAM)-1 and vascular cell adhesion molecule (VCAM)-1 on blood–brain barrier (BBB) endothelial cells. By this mechanism activated T-cells can cross the BBB. The activated T cells then activate macrophages, which in turn produce TNF-α, nitric oxide, free radicals and proteases, causing myelin damage.
In experimental autoimmune encephalomyelitis (EAE; a well known animal model of MS) demyelination is associated with a Th1 response (IFN-γ, IL-2 and TNF-α production), whereas Th2 cytokines (e.g. IL-4 and IL-10) tend to ameliorate the clinical signs of disease in mice and Lewis rats [25]. In MS, autoimmune T-cell responses to myelin antigens, particularly myelin basic protein, may contribute to the inflammatory processes in the CNS [26]. IFN-β has been shown to suppress myelin basic protein reactive T cells, to enhance the production of anti-inflammatory IL-4 and IL-10, and to decrease TNF-α and IFN-γ production [27–30]. Thus, IFN-β may induce immune deviation toward the production of Th2 cytokines, which may contribute to its therapeutic benefit in MS [27].
Extravasation of T cells across the BBB into the CNS is considered a major event in the pathogenesis of MS and EAE. In EAE, kinetic studies have demonstrated that antigen-specific T cells migrate to the CNS early in the immune response, which is followed by enhanced recruitment of a large number of non-antigen-specific T cells that traverse into the CNS parenchyma. The majority of these Tcells are in an activated state [31]. Adhesion molecules on the BBB, such as ICAM-1 and VCAM-1, play important roles and may enhance T-cell trafficking into the CNS. The effect of IFN-β could be caused in part through affecting these adhesion molecules.
In EAE, expression of ICAM-1 and VCAM-1 correlates with disease phase, specifically upregulation during the initial phase and decreased expression during disease remission [32]. Calabresi et al. [33] found increased levels of soluble VCAM-1 in the sera of MS patients, which correlated with a decrease in the number of contrast-enhancing lesions on magnetic resonance imaging during IFN-β treatment. Because soluble VCAM-1 results from the cleavage of its bound form, increased serum levels of soluble VCAM-1 might reflect a decrease in VCAM-1 expression on endothelium in MS patients treated with IFN-β. This suggests that IFN-β may downregulate expression of adhesion molecules on the BBB, which inhibits T-cell trafficking into the CNS.
The effects of IFN-β on cytokine profile and cell trafficking in the MS models and patients described above have stimulated studies on its potential for treatment of RA patients.
Innovative treatment of rheumatoid arthritis patients
RA is a chronic inflammatory disease that affects the synovial tissue in multiple joints. In most patients the disease leads to joint destruction and disability. Inflammation in RA is believed to be mediated by activation of T cells, leading to activation of macrophages and fibroblast-like synoviocytes. The latter produce a variety of proinflammatory cytokines, which results in proliferation of synovial tissue associated with destruction of cartilage and bone. Tissue destruction in RA is closely related to the production of matrix metalloproteinases (MMPs) and other proteinases, which are able to degrade collagen and proteoglycans. Macrophages play a central role in the amplification of stimulatory signals and tissue destruction. Macrophages are found in the synovial lining layer, where they may be involved in protection against infection. In RA they are activated and mediate inflammation by the production of cytokines such as TNF-α, IL-1β, IL-6, IL-12, IL-15, IL-18, platelet derived growth factor and TGF. These cytokines activate fibroblast-like synoviocytes, which maintain macrophage activation by secretion of granulocyte–macrophage colony-stimulating factor, IL-8 and other soluble mediators. Fibroblast-like synoviocytes and osteoclasts invade bone and cartilage, where chondrocytes are activated to produce further proinflammatory cytokines. It is believed that TNF-α is a key cytokine controlling the production of other proinflammatory cytokines.
As a consequence various anticytokine therapies for RA have been tried in the clinic. IL-1 and TNF-α are present in relatively high amounts in synovial fluid and synovial tissue of RA patients [34–36] and, as major contributors to the inflammatory and destructive manifestations of RA, they were the first cytokines to be targeted for treatment of RA. Although the natural inhibitors of IL-1 and TNF-α, namely IL-1 receptor antagonist and soluble TNF receptor, are present in rheumatoid synovium, there might not be enough to neutralize the proinflammatory actions of IL-1 and TNF-α. There appears to be an imbalance between proinflammatory and anti-inflammatory molecules in RA joints.
Following animal studies, two forms of TNF inhibitors have been used in clinical trials in RA: anti-TNF-α antibodies and soluble receptors, which bind with high affinity to TNF. A multicenter, placebo-controlled, double-blind trial in 73 patients was performed in 1994 [37]. Patients were followed over 4 weeks. A single infusion of TNF inhibitor induced significant improvement in arthritis activity. All other clinical trials performed with agents that block TNF-α revealed significant improvement in arthritis and protection against joint destruction [38–42].
The efficacy of recombinant human IL-1 receptor antagonist in RA patients was investigated in a 6-month, placebo-controlled, double-blind, randomized trial [43]. A group of 472 patients with active RA received daily, subcutaneous injections of placebo or one of three doses of recombinant human IL-1 receptor antagonist. After 6 months, the patients who received the highest dose of the active treatment exhibited significant clinical improvement, and X-ray films from those patients showed fewer bone erosions as compared with patients who received placebo.
Other therapeutic targets in RA include MMPs, to prevent the destruction of cartilage and bone. Collagenase (MMP-1), stromelysin-1 (MMP-3) and MMP-13 play important roles in RA [44–46]. Normal fibroblasts produce very low levels of MMP-1 and MMP-3. However, levels increase markedly in response to a variety of stimuli, such as cytokines, crystals and phagocytosis of debris [44, 47]. Increased amounts of MMPs are present in cartilage from patients with RA, and the level of enzyme activity correlates with the severity of the lesion. Similarly, synovial fluid from patients with RA exhibits an increase in MMP levels [48, 49]. Natural inhibitors that are specific for MMPs exist; they are produced locally by chondrocytes and fibroblast-like synoviocytes, and are termed 'tissue inhibitors of metalloproteinases' (TIMPs). It is likely that joint destruction is in part due to a local imbalance between activated MMPs and TIMPs [44, 50]. One study investigated intraperitoneal administration of TIMP-1 in the collagen-induced arthritis mouse model [51] and showed a significant reduction in the severity of disease as compared with untreated control aminals. Several chemotherapeutic agents, antibiotics and synthetic peptides can inhibit the activity of MMPs. Despite promising preclinical data, MMP inhibitors have not been used extensively in the clinic [46]. Minocycline – an antibiotic that can inhibit MMP activity – has been evaluated in three well controlled trials in RA [52–54]. All trials showed some improvement in the patient groups treated with minocycline as compared with placebo.
IFN-β therapy in animal models of rheumatoid arthritis
An alternative approach could be administration of IFN-β because IFN-β has been shown to downregulate the proinflammatory cytokines IL-1β and TNF-α in vitro, while possibly protecting against cartilage destruction by inhibition of IL-1β and MMP activity [55]. Increased production of IL-10 and IL-1 receptor antagonist also suggests that IFN-β therapy has potential as an antirheumatic strategy.
The effect of IFN-β in collagen-induced arthritis in mice was investigated by means of IFN-β gene therapy [56]. Fibroblasts from DBA/1 mice were infected with a retrovirus expressing murine IFN-β and were injected intraperitoneally into DBA/1 mice. This procedure has the advantage of a constant level of expression of IFN-β by syngeneic fibroblasts. Mice were injected with IFN-β-expressing fibroblasts before the onset of arthritis, and paw swelling, arthritic score and histological joint damage were assessed. The animals injected with the IFN-β-expressing fibroblasts developed less severe disease as compared with the control group, and there was a significant decrease in paw swelling.
The effect of treatment on established disease has also been studied. A single intraperitoneal injection of IFN-β-expressing fibroblasts was given in different dosages of cells after the onset of arthritis, again with significant improvement in clinical scores and decreased paw swelling as compared with untreated animals [56]. Histology revealed significant reductions in joint destruction in all groups of mice treated with IFN-β, indicating that constitutive expression of IFN-β has chondroprotective properties. In the same study, total level of type II collagen specific IgG and the levels of IgG1 and IgG2a were measured in order to investigate the effects of IFN-β treatment on the immune response to type II collagen. A modest decrease in total anticollagen IgG levels was observed. Anticollagen IgG2a (regarded as a marker for a Th1 response) was reduced, and there was an increase in IgG1 (regarded as a marker for a Th2 response). Taken together, an increase in the IgG1:IgG2a ratio was observed, which may indicate a modulation of a Th1 to a Th2 immune response. Furthermore, IFN-β could inhibit production of TNF-α, IL-12 and IFN-γ production in vitro in a dose-dependent manner. These effects were reversed by anti-IFN-β antibodies, giving further support to the hypothesis that IFN-β is able to downregulating Th1 responses.
A study in which mice with collagen-induced arthritis received daily intraperitoneal injections (up to 2.5 μg/mouse per day) of exogenous IFN-β yielded similar results [57]. A significant decrease in inflammation, and more importantly a statistically significant decrease in cartilage and bone destruction was observed in the IFN-β treated group as compared with control mice. Of importance, the protection of joint integrity appeared to be the most important effect of IFN-β.
Consistent with these observations, Takayanagi et al. [58] recently demonstrated the critical role of IFN-β in bone homeostasis. Those investigators observed that mice lacking IFN-β exhibited severe osteopenia, probably by downregulating osteoclastogenesis. Bone-resorbing osteoclasts and bone-forming osteoblasts are essential to maintenance a balance between bone resorption and bone formation. When this balance is disrupted in favour of the osteoclasts, bone destruction (as observed in RA) may follow. Osteoclast numbers and activity are dependent on the balance between the osteoclast-promoting receptor activator of nuclear factor-κB ligand (RANKL) and osteoclast-inhibiting osteoprotegerin. In addition, there is a negative feedback mechanism by which osteoclasts can control their own differentiation. RANKL induces the expression of IFN-β in osteoclast precursor cells via the transcription factor c-Fos (an essential transcription factor for the formation of osteoclasts). IFN-β is then released from these cells, and binds to and activates its own cell surface receptor system on osteoclast precursors, leading to a decrease in c-Fos levels. Lack of c-Fos leads to inhibition of osteoclast differentiation [59]. Thus, the IFN-β regulatory mechanism is important to maintenance of bone homeostasis, supporting the view that IFN-β therapy may be used to inhibit bone destruction [58, 59].
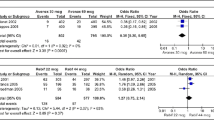
In addition to studies conducted in mouse models, IFN-β therapy has been evaluated in collagen-induced arthritis in rhesus monkeys [14]. The monkeys were susceptible to collagen type II induced arthritis because of lack of the major histocompatibility complex class I allele A-26. Three out of four monkeys had active polyarthritis at the time of treatment initiation. The fourth monkey was in a preclinical phase of the disease, as shown by elevation in serum acute phase reactants and synovial inflammation by arthroscopy. The monkeys were treated with a high dosage of 37 μg/kg mammalian cell-derived recombinant IFN-β1a subcutaneously each day for 1 week. Two monkeys with established arthritis exhibited clear clinical improvement after treatment, and the monkey with preclinical synovitis never developed signs of arthritis. During IFN-β treatment all four monkeys had a marked decrease in serum C-reactive protein levels. Thus, that study confirmed previous work in mouse collagen-induced arthritis, indicating that continous production of IFN-β by transfected cells or daily IFN-β injections has potential as an antirheumatic strategy.
IFN-β therapy in patients with arthritis
The preclinical studies encouraged us to perform an open phase I study in 12 patients with active RA [14]. They were treated with IFN-β subcutaneously three times a week, which is the schedule used in MS patients but differs from the treatment schedule used in the collagen-induced arthritis models described above. We chose not to use daily injections because it was anticipated that this would be less tolerable to the patients. Three different doses of IFN-β were used: 22 μg, 44 μg and 66 μg. Treatment was in general well tolerated. Although there was gradual and significant improvement in tender joint count, swollen joint count, patient's assessment of pain, and patient's and doctor's global assessment, the effects appeared to be limited. Conceivably, the clinical effects could have been more pronounced after treatment with daily injections. It should be noted, however, that this uncontrolled pilot study was not designed to demonstrate a clinical effect.
Arthroscopy was performed in these patients and synovial biopsies were taken before study entry, after 1 month and after 3 months of IFN-β treatment [55]. A statistically significant reduction in the mean immunohistological scores for expression of IL-1β, IL-6, MMP-1 and TIMP was observed in synovial tissue from RA patients after IFN-β therapy, suggesting a biological effect of the treatment.
Another pilot study was recently performed [60]. Six children with juvenile rheumatoid arthritis were treated for 16 weeks with weekly intramuscular injections of 10 or 20 μg/m2 IFN-β. All patients tolerated the treatment well and all six patients met criteria for a 30% response after treatment. Three of the six children even improved by at least 50% [60]. It should be stressed, however, that this study was not placebo controlled.
There are two case reports claiming the development of RA after the onset of IFN-β treatment. One report describes a patient who developed a seropositive polyarthritis, which fulfilled the American Colllege of Rheumatology criteria for RA, after 1.5 years of IFN-β treatment for MS [61]. In that case it appears that IFN-β was at least unable to prevent the onset of RA. Another case report describes a patient with the HLA-DRB1*0404 allele who developed a seronegative symmetric polyarthritis of the wrists and hand joints after 8 weeks of IFN-β treatment for MS [62]. Eight months after the IFN-β treatment ended, symptoms of arthritis subsided, with resolution of the synovitis. That patient did not fulfill the American College of Rheumatology criteria for RA. Taken together, these case reports show that IFN-β therapy does not prevent the development of arthritis in all patients.
Conclusion
In conclusion, IFN-β therapy has been shown to slow down the progression of disability in patients with relapsing-remitting MS, and might also have antirheumatic potential. It remains to be shown whether these exciting biological effects can translate into clinically meaningful improvement if the cytokine is administered only three times weekly or if more continous levels of IFN-β are required.
Abbreviations
- BBB:
-
= blood–brain barrier
- CNS:
-
= central nervous system
- EAE:
-
= experimental autoimmune encephalomyelitis
- IFN:
-
= interferon
- ICAM:
-
= intercellular adhesion molecule
- IL:
-
= interleukin
- MMP:
-
= matrix metalloproteinase
- MS:
-
= multiple sclerosis
- RA:
-
= rheumatoid arthritis
- RANKL:
-
= receptor activator of nuclear factor-κB ligand
- TGF:
-
= transforming growth factor
- Th:
-
= T-helper (cell)
- TIMP:
-
= tissue inhibitor of metalloproteinase
- TNF:
-
= tumour necrosis factor
- VCAM:
-
= vascular cell adhesion molecule.
References
Akbar AN, Lord JM, Salmon M: IFN-alpha and IFN-beta: a link between immune memory and chronic inflammation. Immunol Today. 2000, 21: 337-342. 10.1016/S0167-5699(00)01652-2.
De Maeyer E, De Maeyer-Guignard J: Type I interferons. Int Rev Immunol. 1998, 17: 53-73.
Stark GR, Kerr IM, Williams BR, Silverman RH, Schreiber RD: How cells respond to interferons. Annu Rev Biochem. 1998, 67: 227-264. 10.1146/annurev.biochem.67.1.227.
Veys EM, Menkes CJ, Emery P: A randomized, double-blind study comparing twenty-four-week treatment with recombinant interferon-gamma versus placebo in the treatment of rheumatoid arthritis. Arthritis Rheum. 1997, 40: 62-68.
Panitch HS, Hirsch RL, Haley AS, Johnson KP: Exacerbations of multiple sclerosis in patients treated with gamma interferon. Lancet. 1987, 1: 893-895. 10.1016/S0140-6736(87)92863-7.
Chofflon M: Recombinant human interferon beta in relapsing-remitting multiple sclerosis: a review of the major clinical trials. Eur J Neurol. 2000, 7: 369-380. 10.1046/j.1468-1331.2000.00057.x.
Comi G, Colombo B, Martinelli V: Prognosis-modifying therapy in multiple sclerosis. Neurol Sci. 2000, 21 (suppl 2): S893-S899. 10.1007/s100720070033.
Anonymous: Interferon beta-1b is effective in relapsing-remitting multiple sclerosis. I. Clinical results of a multicenter, randomized, double-blind, placebo-controlled trial. The IFNB Multiple Sclerosis Study Group. Neurology. 1993, 43: 655-661.
Anonymous: Randomised double-blind placebo-controlled study of interferon beta-1a in relapsing/remitting multiple sclerosis. PRISMS (Prevention of Relapses and Disability by Interferon beta-1a Subcutaneously in Multiple Sclerosis) Study Group. Lancet. 1998, 352: 1498-1504. 10.1016/S0140-6736(98)03334-0.
Jacobs LD, Cookfair DL, Rudick RA, Herndon RM, Richert JR, Salazar AM, Fischer JS, Goodkin DE, Granger CV, Simon JH, Alam JJ, Bartoszak DM, Bourdette DN, Braiman J, Brownscheidle CM, Coats ME, Cohan SL, Dougherty DS, Kinkel RP, Mass MK, Munschauer FE, Priore RL, Pullicino PM, Scherokman BJ, Whitham RH: Intramuscular interferon beta-1a for disease progression in relapsing multiple sclerosis. The Multiple Sclerosis Collaborative Research Group (MSCRG). Ann Neurol. 1996, 39: 285-294.
Coclet-Ninin J, Dayer JM, Burger D: Interferon-beta not only inhibits interleukin-1beta and tumor necrosis factor-alpha but stimulates interleukin-1 receptor antagonist production in human peripheral blood mononuclear cells. Eur Cytokine Netw. 1997, 8: 345-349.
Rep MH, Schrijver HM, van Lopik T, Hintzen RQ, Roos MT, Ader HJ, Polman CH, van Lier RA: Interferon (IFN)-beta treatment enhances CD95 and interleukin 10 expression but reduces interferon-gamma producing T cells in MS patients. J Neuroimmunol. 1999, 96: 92-100. 10.1016/S0165-5728(98)00271-9.
Rep MH, Hintzen RQ, Polman CH, van Lier RA: Recombinant interferon-beta blocks proliferation but enhances interleukin-10 secretion by activated human T-cells. J Neuroimmunol. 1996, 67: 111-118.
Tak PP, Hart BA, Kraan MC, Jonker M, Smeets TJ, Breedveld FC: The effects of interferon beta treatment on arthritis. Rheumatology (Oxford). 1999, 38: 362-369. 10.1093/rheumatology/38.4.362.
Bielenberg DR, Bucana CD, Sanchez R, Mulliken JB, Folkman J, Fidler IJ: Progressive growth of infantile cutaneous hemangiomas is directly correlated with hyperplasia and angiogenesis of adjacent epidermis and inversely correlated with expression of the endogenous angiogenesis inhibitor, IFN-beta. Int J Oncol. 1999, 14: 401-408.
Folkman J, Ingber D: Inhibition of angiogenesis. Semin Cancer Biol. 1992, 3: 89-96.
Marchisone C, Benelli R, Albini A, Santi L, Noonan DM: Inhibition of angiogenesis by type I interferons in models of Kaposi's sarcoma. Int J Biol Markers. 1999, 14: 257-262.
Dvorak HF, Gresser I: Microvascular injury in pathogenesis of interferon-induced necrosis of subcutaneous tumors in mice. J Natl Cancer Inst. 1989, 81: 497-502.
Wadler S, Schwartz EL: Antineoplastic activity of the combination of interferon and cytotoxic agents against experimental and human malignancies: a review. Cancer Res. 1990, 50: 3473-3486.
Singh RK, Gutman M, Bucana CD, Sanchez R, Llansa N, Fidler IJ: Interferons alpha and beta down-regulate the expression of basic fibroblast growth factor in human carcinomas. Proc Natl Acad Sci USA. 1995, 92: 4562-4566.
Peacock DJ, Banquerigo ML, Brahn E: Angiogenesis inhibition suppresses collagen arthritis. J Exp Med. 1992, 175: 1135-1138.
Gerlag DM, Borges E, Tak PP, Ellerby HM, Bredesen DE, Pasqualini R, Ruoslahti E, Firestein GS: Suppression of murine collagen-induced arthritis by targeted apoptosis of synovial neovasculature. Arthritis Res. 2001, 3: 357-361. 10.1186/ar327.
Oliver SJ, Banquerigo ML, Brahn E: Suppression of collagen-induced arthritis using an angiogenesis inhibitor, AGM- and a microtubule stabilizer, taxol. Cell Immunol. 1470, 157: 291-299. 10.1006/cimm.1994.1223.
Storgard CM, Stupack DG, Jonczyk A, Goodman SL, Fox RI, Cheresh DA: Decreased angiogenesis and arthritic disease in rabbits treated with an alphavbeta3 antagonist. J Clin Invest. 1999, 103: 47-54.
Diab A, Zhu J, Xiao BG, Mustafa M, Link H: High IL-6 and low IL-10 in the central nervous system are associated with protracted relapsing EAE in DA rats. J Neuropathol Exp Neurol. 1997, 56: 641-650.
Stinissen P, Raus J, Zhang J: Autoimmune pathogenesis of multiple sclerosis: role of autoreactive T lymphocytes and new immunotherapeutic strategies. Crit Rev Immunol. 1997, 17: 33-75.
Kozovska ME, Hong J, Zang YC, Li S, Rivera VM, Killian JM, Zhang JZ: Interferon beta induces T-helper 2 immune deviation in MS. Neurology. 1999, 53: 1692-1697.
Rieckmann P, Albrecht M, Kitze B, Weber T, Tumani H, Broocks A, Luer W, Poser S: Cytokine mRNA levels in mononuclear blood cells from patients with multiple sclerosis. Neurology. 1994, 44: 1523-1526.
Ozenci V, Kouwenhoven M, Huang YM, Kivisakk P, Link H: Multiple sclerosis is associated with an imbalance between tumour necrosis factor-alpha (TNF-alpha)- and IL-10-secreting blood cells that is corrected by interferon-beta (IFN-beta) treatment. Clin Exp Immunol. 2000, 120: 147-153. 10.1046/j.1365-2249.2000.01175.x.
Noronha A, Toscas A, Jensen MA: Interferon beta decreases T cell activation and interferon gamma production in multiple sclerosis. J Neuroimmunol. 1993, 46: 145-153. 10.1016/0165-5728(93)90244-S.
Yong VW, Chabot S, Stuve O, Williams G: Interferon beta in the treatment of multiple sclerosis: mechanisms of action. Neurology. 1998, 51: 682-689.
Cannella B, Cross AH, Raine CS: Adhesion-related molecules in the central nervous system. Upregulation correlates with inflammatory cell influx during relapsing experimental autoimmune encephalomyelitis. Lab Invest. 1991, 65: 23-31.
Calabresi PA, Tranquill LR, Dambrosia JM, Stone LA, Maloni H, Bash CN, Frank JA, McFarland HF: Increases in soluble VCAM-1 correlate with a decrease in MRI lesions in multiple sclerosis treated with interferon beta-1b. Ann Neurol. 1997, 41: 669-674.
Feldmann M, Brennan FM, Maini RN: Role of cytokines in rheumatoid arthritis. Annu Rev Immunol. 1996, 14: 397-440. 10.1146/annurev.immunol.14.1.397.
Tak PP, Smeets TJ, Daha MR, Kluin PM, Meijers KA, Brand R, Meinders AE, Breedveld FC: Analysis of the synovial cell infiltrate in early rheumatoid synovial tissue in relation to local disease activity. Arthritis Rheum. 1997, 40: 217-225.
Firestein GS: Cytokine networks in rheumatoid arthritis: implications for therapy. Agents Actions Suppl. 1995, 47: 37-51.
Elliott MJ, Maini RN, Feldmann M, Kalden JR, Antoni C, Smolen JS, Leeb B, Breedveld FC, Macfarlane JD, Bijl H: Randomised double-blind comparison of chimeric monoclonal antibody to tumour necrosis factor alpha (cA2) versus placebo in rheumatoid arthritis. Lancet. 1994, 344: 1105-1110. 10.1016/S0140-6736(94)90628-9.
Maini RN, Breedveld FC, Kalden JR, Smolen JS, Davis D, Macfar-lane JD, Antoni C, Leeb B, Elliott MJ, Woody JN, Schaible TF, Feldmann M: Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum. 1998, 41: 1552-1563. 10.1002/1529-0131(199803)41:3<565::AID-ART28>3.3.CO;2-#.
Maini R, St Clair EW, Breedveld F, Furst D, Kalden J, Weisman M, Smolen J, Emery P, Harriman G, Feldmann M, Lipsky P: Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial. ATTRACT Study Group. Lancet. 1999, 354: 1932-1939. 10.1016/S0140-6736(99)05246-0.
Moreland LW, Baumgartner SW, Schiff MH, Tindall EA, Fleischmann RM, Weaver AL, Ettlinger RE, Cohen S, Koopman WJ, Mohler K, Widmer MB, Blosch CM: Treatment of rheumatoid arthritis with a recombinant human tumor necrosis factor receptor (p75)-Fc fusion protein. N Engl J Med. 1997, 337: 141-147. 10.1056/NEJM199707173370301.
Moreland LW, Schiff MH, Baumgartner SW, Tindall EA, Fleischmann RM, Bulpitt KJ, Weaver AL, Keystone EC, Furst DE, Mease PJ, Ruderman EM, Horwitz DA, Arkfeld DG, Garrison L, Burge DJ, Blosch CM, Lange ML, McDonnell ND, Weinblatt ME: Etanercept therapy in rheumatoid arthritis. A randomized, controlled trial. Ann Intern Med. 1999, 130: 478-486.
Weinblatt ME, Kremer JM, Bankhurst AD, Bulpitt KJ, Fleischmann RM, Fox RI, Jackson CG, Lange M, Burge DJ: A trial of etanercept, a recombinant tumor necrosis factor receptor:Fc fusion protein, in patients with rheumatoid arthritis receiving methotrexate. N Engl J Med. 1999, 340: 253-259. 10.1056/NEJM199901283400401.
Bresnihan B, Alvaro-Gracia JM, Cobby M, Doherty M, Domljan Z, Emery P, Nuki G, Pavelka K, Rau R, Rozman B, Watt I, Williams B, Aitchison R, McCabe D, Musikic P: Treatment of rheumatoid arthritis with recombinant human interleukin-1 receptor antagonist. Arthritis Rheum. 1998, 41: 2196-2204. 10.1002/1529-0131(199812)41:12<2196::AID-ART15>3.3.CO;2-U.
Vincenti MP, Clark IM, Brinckerhoff CE: Using inhibitors of metalloproteinases to treat arthritis. Easier said than done?. Arthritis Rheum. 1994, 37: 1115-1126.
Harris ED: Rheumatoid arthritis. Pathophysiology and implications for therapy. N Engl J Med. 1990, 322: 1277-1289.
Furst DE: Leflunomide, mycophenolic acid and matrix metalloproteinase inhibitors. Rheumatology (Oxford). 1999, 38 (suppl 2): 14-18.
Brinckerhoff CE, Auble DT: Regulation of collagenase gene expression in synovial fibroblasts. Ann N Y Acad Sci. 1990, 580: 355-74.
Walakovits LA, Moore VL, Bhardwaj N, Gallick GS, Lark MW: Detection of stromelysin and collagenase in synovial fluid from patients with rheumatoid arthritis and posttraumatic knee injury. Arthritis Rheum. 1992, 35: 35-42.
Clark IM, Powell LK, Ramsey S, Hazleman BL, Cawston TE: The measurement of collagenase, tissue inhibitor of metalloproteinases (TIMP), and collagenase-TIMP complex in synovial fluids from patients with osteoarthritis and rheumatoid arthritis. Arthritis Rheum. 1993, 36: 372-379.
Tak PP, Bresnihan B: The pathogenesis and prevention of joint damage in rheumatoid arthritis: advances from synovial biopsy and tissue analysis. Arthritis Rheum. 2000, 43: 2619-2633. 10.1002/1529-0131(200012)43:12<2619::AID-ANR1>3.0.CO;2-V.
Carmichael DF, Stricklin GP, Stuart JM: Systemic administration of TIMP in the treatment of collagen-induced arthritis in mice. Agents Actions. 1989, 27: 378-379.
Kloppenburg M, Breedveld FC, Terwiel JP, Mallee C, Dijkmans BA: Minocycline in active rheumatoid arthritis. A double-blind, placebo-controlled trial. Arthritis Rheum. 1994, 37: 629-636.
Tilley BC, Alarcon GS, Heyse SP, Trentham DE, Neuner R, Kaplan DA, Clegg DO, Leisen JC, Buckley L, Cooper SM: Minocycline in rheumatoid arthritis. A 48-week, double-blind, placebo-controlled trial. MIRA Trial Group. Ann Intern Med. 1995, 122: 81-89.
O'Dell JR, Paulsen G, Haire CE, Blakely K, Palmer W, Wees S, Eckhoff PJ, Klassen LW, Churchill M, Doud D, Weaver A, Moore GF: Treatment of early seropositive rheumatoid arthritis with minocycline: four-year followup of a double-blind, placebo-controlled trial. Arthritis Rheum. 1999, 42: 1691-1695. 10.1002/1529-0131(199908)42:8<1691::AID-ANR18>3.0.CO;2-S.
Smeets TJ, Dayer JM, Kraan MC, Versendaal J, Chicheportiche R, Breedveld FC, Tak PP: The effects of interferon-beta treatment of synovial inflammation and expression of metalloproteinases in patients with rheumatoid arthritis. Arthritis Rheum. 2000, 43: 270-274. 10.1002/1529-0131(200002)43:2<270::AID-ANR5>3.0.CO;2-H.
Triantaphyllopoulos KA, Williams RO, Tailor H, Chernajovsky Y: Amelioration of collagen-induced arthritis and suppression of interferon-gamma, interleukin-12, and tumor necrosis factor alpha production by interferon-beta gene therapy. Arthritis Rheum. 1999, 42: 90-99. 10.1002/1529-0131(199901)42:1<90::AID-ANR12>3.0.CO;2-A.
Holten VJ, Sattonet-Roche P, Siegfried C, Graber P, Tak PP, Plater-Zyberk C: Treatment with recombinant interferon beta slows artilage destruction and reduces inflammation in the collagen-induced arthritis model of rheumatoid arthritis [abstract]. Arthritis Rheum. 2000, 43: s231-
Takayanagi H, Kim S, Matsuo K, Suzuki H, Suzuki T, Sato K, Yokochi T, Oda H, Nakamura K, Ida N, Wagner EF, Taniguchi T: RANKL maintains bone homeostasis through c-Fos-dependent induction of interferon-beta. Nature. 2002, 416: 744-749. 10.1038/416744a.
Alliston T, Derynck R: Medicine: interfering with bone remodelling. Nature. 2002, 416: 686-687. 10.1038/416686a.
Sundel RP, Wallace CA, Zurakowski Boston D: Pilot trial of interferon beta-1a in JRA [abstract]. Arthritis Rheum. 2001, 44: s272-
Alsalameh S, Manger B, Kern P, Kalden J: New onset of rheumatoid arthritis during interferon beta-1B treatment in a patient with multiple sclerosis: comment on the case report by Jabaily and Thompson [letter]. Arthritis Rheum. 1998, 41: 754-10.1002/1529-0131(199804)41:4<754::AID-ART33>3.0.CO;2-K.
Levesque MC, Ward FE, Jeffery DR, Weinberg JB: Interferon-beta1A-induced polyarthritis in a patient with the HLA-DRB1*0404 allele. Arthritis Rheum. 1999, 42: 569-573. 10.1002/1529-0131(199904)42:3<569::AID-ANR23>3.0.CO;2-M.
Acknowledgement
CP-Z was employed by Serono Pharmaceutical Research Institute, Geneva, Switzerland, at the time of writing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Holten, J., Plater-Zyberk, C. & Tak, P.P. Interferon-β for treatment of rheumatoid arthritis?. Arthritis Res Ther 4, 346 (2002). https://doi.org/10.1186/ar598
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar598